What is ectopia lentis
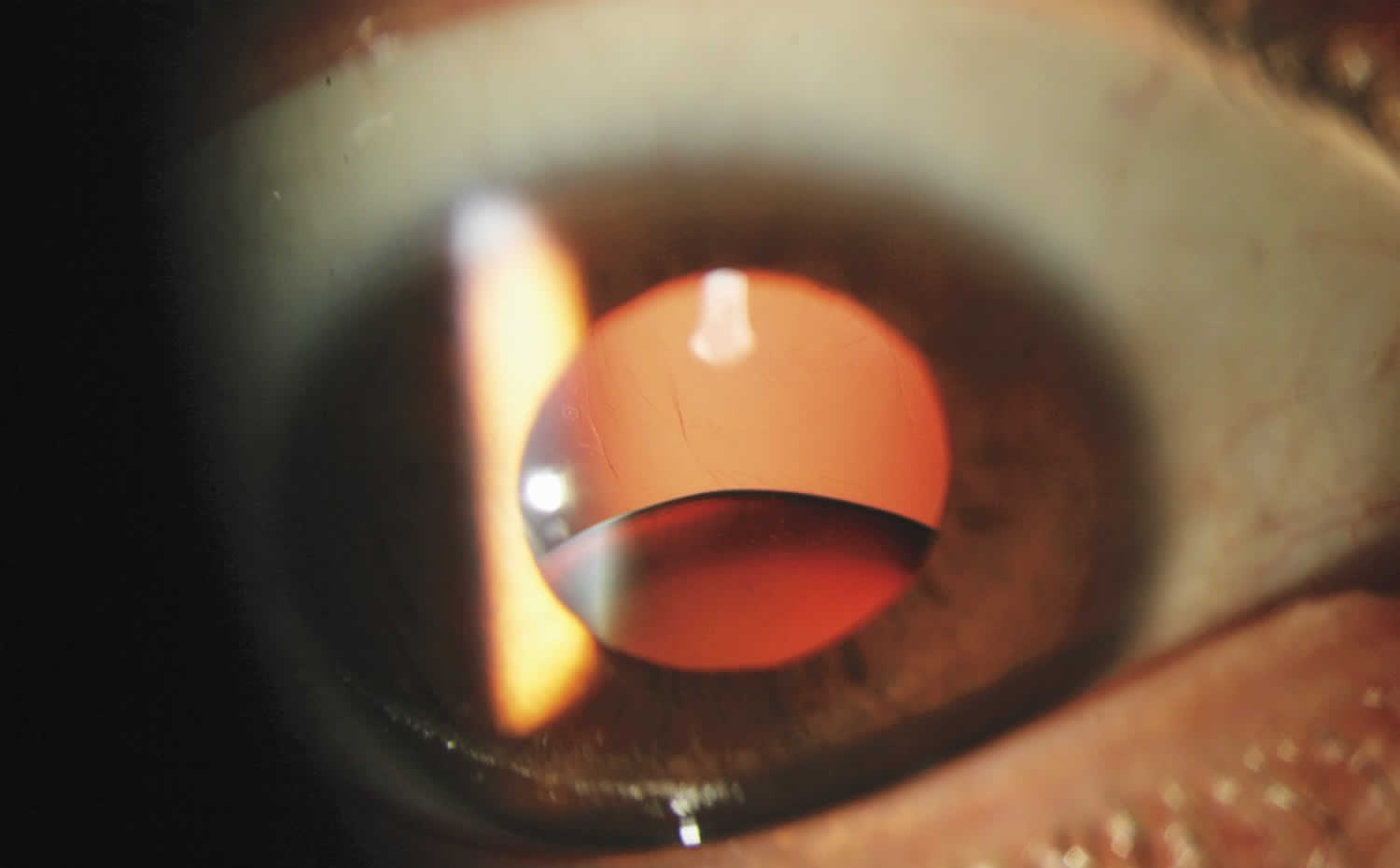
Ectopia lentis is defined as dislocation or displacement of the natural crystalline lens of the eye 1. The lens is defined as luxated (dislocated) when it lies completely outside of the hyaloid fossa, is free-floating in the vitreous, is in the anterior chamber, or lies directly on the retina. The lens is considered subluxed when it is partially displaced but remains within the lens space 2.
Ectopia lentis may occur after trauma or may be associated with ocular or systemic disease. As ectopia lentis may be the first sign of a more serious systemic disease, it is important to determine the etiology for appropriate patient management. Additionally, ectopic lentis can cause major complications within the eye, including significant refractive shifts, pupillary block glaucoma, retinal damage, and blindness.
Ectopia lentis causes
Ectopia lentis can occur due to trauma, ocular disease, or systemic disease. Trauma is the most common cause of ectopia lentis. Ectopia lentis may be present at birth or occur at any age. Traumatic ectopia lentis is most often the result of a direct blow to the eye, such as from a baseball or golf ball, but can also occur after blunt trauma to the head or orbit 3. Though trauma is the most common cause of ectopia lentis, if the trauma is minor, one should consider other underlying diseases that could predispose the patient to lens dislocation 4.
Ocular diseases associated with ectopia lentis:
- Simple ectopia lentis – simple ectopia lentis can occur as a congenital disorder or as a spontaneous disorder later in life. Both are hereditary and can be inherited in an autosomal dominant or recessive pattern. Mutations resulting in simple ectopia lentis include mutations to the ADAMTSL4 gene located on chromosome 1 (recessive inheritance pattern) and the FBN1 gene located on chromosome 15 (dominant inheritance pattern) 5. These mutations often result in irregularity and degeneration of the zonular fibers, leading to lens dislocation. Significant overlap exists between the genetics of simple ectopia lentis and the systemic diseases associated with ectopia lentis (e.g. mutations to the FBN1 gene can also result in Marfan syndrome) 6. In simple ectopia lentis, the lens dislocation is usually bilateral and occurs most often in the superotemporal direction 7.
- Ectopia lentis et pupillae – ectopia lentis et pupillae is a rare congenital disorder in which there is asymmetric eccentric pupils that are displaced in the opposite direction of a lens dislocation. The pupils are characteristically oval and ectopic, and often dilate poorly 8. The irides often appear atrophic with marked transillumination of the periphery on slit lamp examination 9. The lens dislocation is usually bilateral and commonly not symmetrical 7.
Other ocular disorders associated with ectopia lentis 7:
- Aniridia
- Congenital glaucoma
- Pseudoexfoliation syndrome
- Syphillis
- Retinitis pigmentosa
- Intraocular tumor
- Axenfeld Rieger syndrome
- Megalocornea
- Hypermature cataract
Systemic diseases associated with ectopia lentis:
- Marfan syndrome – Marfan syndrome is the most common cause of heritable ectopia lentis, and ectopia lentis is the most frequent ocular manifestation of Marfan syndrome, occurring in approximately 75% of patients 10. Marfan syndrome is an autosomal dominant disease resulting from various mutations to the fibrillin-1 gene located on chromosome 15. It is thought that the increased incidence of ectopia lentis with Marfan syndrome is due to altered fibrillin microfibrils leading to incompetent zonular fibers and structural abnormalities of the lens capsule 11. Lens dislocation in Marfan syndrome is usually bilateral and occurs most often in the superotemporal direction, though other directions are not uncommon 12.
- Homocystinuria – Homocystinuria is the second most common cause of heritable ectopia lentis. Homocystinuria is an autosomal recessive metabolic disorder most often caused by a near absence of cystathionine b-synthetase. It is associated with intellectual disability, osteoporosis, chest deformities, and increased risk of thrombotic episodes. Lens dislocation occurs in 90% of patients, and is thought to be due to decreased zonular integrity due to the enzymatic defect. Lens dislocation in homocystinuria is usually bilateral and in 60% of cases occurs in the inferior or nasal direction 13.
Other systemic diseases associated with ectopia lentis 6:
- Weill-Marchesani syndrome
- Sulfite oxidase deficiency
- Hyperlysinemia
- Ehlers-Danlos syndrome
- Sturge-Weber syndrome
- Mandibulofacial dysostosis
- Wildervanck syndrome
- Conradi syndrome
- Pfaundler syndrome
- Crouzon syndrome
- Pierre Robin syndrome
- Sprengel deformity
Ectopia lentis symptoms
Common presenting symptoms (visual disturbance) include the following:
- Red painful eye (secondary to trauma)
- Decreased distance visual acuity (secondary to astigmatism or myopia)
- Poor near vision (loss of accommodative power)
- Monocular diplopia
Determine if there is a history of ocular trauma.
Obtain a detailed history investigating possible systemic disease associations, as follows:
- Cardiovascular disease (eg, Marfan syndrome)
- Skeletal problems -Marfan syndrome, Weil-Marchesani syndrome, or homocystinuria
- Pertinent family history – Consanguinity, mental retardation, or unexplained deaths at young age (eg, autosomal recessive conditions, including homocystinuria, hyperlysinemia, ectopia lentis et pupillae 14 or sulfite oxidase deficiency)
Ectopia lentis complications
The most common ocular complications of ectopia lentis include amblyopia, uveitis, glaucoma, and retinal detachment; appropriate treatment for these specific entities should be implemented.
Ectopia lentis diagnosis
A history of any recent trauma is of principal importance. Traumatic ectopia lentis generally presents with a red, painful eye secondary to trauma. A detailed family history is required for atraumatic and mildly traumatic presentations. One should specifically ask about visual disturbances, cardiovascular disease, or skeletal abnormalities in the patient or patient’s family.
The most significant symptom of ectopia lentis is reduced visual acuity. Common visual disturbances include poor near vision due to loss of accommodation, poor distant vision due to astigmatism or myopia, and monocular diplopia. The degree of visual acuity reduction will vary with the degree of dislocation, the type of dislocation, and any other concurrent ocular defects. Minimal subluxation may lead to little or no loss of visual acuity, while disruption of the zonules, leading to increased curvature of the lens, may result in lenticular myopia and astigmatism 7.
Physical examination
Due to the association with multiple ocular and systemic diseases, a complete physical examination should be performed on any patient with ectopia lentis of undetermined etiology.
The ocular examination for ectopia lentis should consist of checking visual acuity, an external ocular exam, a slit lamp exam, retinoscopy and refraction, and a dilated fundus examination. Corneal diameter should be measured, as megalocornea is associated with Marfan syndrome. If astigmatism is present, keratometry may help determine whether the astigmatism is primarily corneal or if it is the result of altered lens location. Intraocular pressure may be elevated due to pupillary block or posttraumatic angle recession. Dilated fundus examination is necessary as retinal detachment is a possible consequence of ectopia lentis 7.
In younger children less cooperative with a slit lamp examination, examination with a penlight may demonstrate tremulousness of the iris (iridodonesis) 15.
Grading systems for ectopia lentis have been proposed to facilitate and standardize studies, as well as enable communication between clinicians managing these patients, but no specific grading system is widely accepted 16.
Laboratory tests
If a hereditary condition is suspected, perform appropriate diagnostic and laboratory evaluation (e.g. total plasma homocysteine concentration for homocystinuria, cardiac evaluation for Marfan syndrome).
Ectopia lentis treatment
Medical management
Medical management involves refractive correction as well as co-management of any associated systemic disease with the patient’s internist or pediatrician. As many predisposing diseases are hereditary, genetic counseling may be indicated. Treatment of ectopia lentis itself depends on where and how far the lens moves, as well as any resulting complications. In all cases, timely optical correction is important for prevention of amblyopia. If the dislocated lens migrates into the anterior chamber, treatment is initially pharmacological with mydriasis to permit posterior migration of the lens behind the iris. Pupillary block glaucoma should be treated with laser peripheral iridotomy, and elevations in intraocular pressure should be treated medically.
Progressive lens dislocation without major complications has been traditionally managed conservatively; however, some studies suggest that surgical intervention could lead to improved visual acuity 7. The decision to operate depends on many factors, including visual acuity, lens location, progressive subluxation of the lens, imminent total dislocation, and others.
Close follow-up care with a full ocular examination, including tonometry (intraocular pressure check) and dilated fundus examination, is important.
Ectopia lentis surgery
Surgical management of ectopia lentis remains a challenge, as inherent defects in the lens capsule makes implantation of an intraocular lens difficult. As a result, many patients are managed with lensectomy/vitrectomy with optical rehabilitation with a contact lens. Indications for lensectomy include, but are not limited to 15:
- Lens-induced glaucoma
- Lens in the anterior chamber, especially if the lens is touching the corneal endothelium
- Lens opacity that is mature or hypermature
- Evidence of lens-induced uveitis
- Inadequate visual acuity not correctable by refraction
- Imminent complete luxation of the lens
- Retinal detachment
Multiple surgical techniques exist for surgical correction of ectopia lentis, each with its own limitations and associated complications. Techniques include 17:
- Lensectomy/vitrectomy with a contact lens or spectacles
- Artisan iris clip lens
- Scleral-sutured posterior intraocular lens
- Implantation of in-the-bag intraocular lens with a capsular tension ring
Ectopia lentis prognosis
An individual’s prognosis depends on any underlying ocular or systemic disease, the degree of subluxation, and the management strategy pursued. Large prospective randomized clinical trials are needed to determine the long-term visual outcomes in specific patient populations affected by ectopia lentis. Fortunately, the majority of patients with ectopia lentis achieve a best-corrected visual acuity of 20/40 or better 18.
References- Nelson LB, Maumenee IH. Ectopia lentis. Surv Ophthalmol. 1982 Nov-Dec. 27(3):143-60.
- Clarke, Clement C. “Ectopia lentis: a pathologic and clinical study.” Archives of Ophthalmology 21.1 (1939): 124- 153.
- Harley, Robison D., Leonard B. Nelson, and Scott E. Olitsky, eds. Harley’s Pediatric Ophthalmology. Lippincott Williams & Wilkins, 2005. p.225.
- Jarrett, William H. “Dislocation of the lens: a study of 166 hospitalized cases.” Archives of ophthalmology 78.3 (1967): 289-296.
- Chandra, Aman, et al. “A genotype-phenotype comparison of ADAMTSL4 and FBN1 in isolated ectopia lentis.” Investigative ophthalmology & visual science53.8 (2012): 4889-4896.
- Sadiq, Mohammad Ali, and Deborah Vanderveen. “Genetics of ectopia lentis.” Seminars in ophthalmology. Vol. 28. No. 5-6. New York: Informa Healthcare USA, Inc., 2013.
- Nelson, Leonard B., and Irene H. Maumenee. “Ectopia lentis.” Survey of ophthalmology 27.3 (1982): 143-160.
- Cross, Harold E. “Ectopia lentis et pupillae.” American journal of ophthalmology 88.3 (1979): 381-384.
- Omulecki, Wojciech, Michal Wilczynski, and Marek Gerkowicz. “Management of bilateral ectopia lentis et pupillae syndrome.” Ophthalmic surgery, lasers & imaging: the official journal of the International Society for Imaging in the Eye37.1 (2005): 68-71.
- Wakita, M., et al. “[Statistical analysis of Marfan’s syndrome].” Nippon Ganka Gakkai Zasshi 93.6 (1989): 682- 690.
- Traboulsi, Elias I., et al. “Microfibril abnormalities of the lens capsule in patients with Marfan syndrome and ectopia lentis.” Ophthalmic genetics 21.1 (2000): 9-15.
- Maumenee, Irene Hussels. “The eye in the Marfan syndrome.” Transactions of the American Ophthalmological Society 79 (1981): 684.
- Neely, Daniel E., and David A. Plager. “Management of ectopia lentis in children.” Ophthalmology clinics of North America 14.3 (2001): 493-499.
- Omulecki W, Wilczynski M, Gerkowicz M. Management of bilateral ectopia lentis et pupillae syndrome. Ophthalmic Surg Lasers Imaging. 2006 Jan-Feb. 37(1):68-71.
- Singh, Daljit, et al. “P Dislocated Crystalline Lenses.” Pediatric Cataract Surgery: Techniques, Complications, and Management (2005): 205.
- Chandra, Aman, Philip J. Banerjee, and David G. Charteris. “Grading in ectopia lentis (GEL): a novel classification system.” British Journal of Ophthalmology97.7 (2013): 942-943.
- Hoffman, Richard S., et al. “Management of the subluxated crystalline lens.”Journal of Cataract & Refractive Surgery 39.12 (2013): 1904-1915.
- Chandra, A., and D. Charteris. “Molecular pathogenesis and management strategies of ectopia lentis.” Eye 28.2 (2014): 162-168.