Femoroacetabular impingement
Femoroacetabular impingement (FAI) is a condition in which extra bone grows along one or both of the bones that form the hip joint — giving the bones an irregular shape. A normally developed hip joint is formed by the end of the thigh bone (technically called the femoral head) that normally is shaped as a ball or sphere and the socket (also referred to as the acetabulum) on either side of the pelvic bone. FAI involves abnormal contact between the end of the thigh bone and neck against the frontal part of the hip socket. In FAI, bone overgrowth — called bone spurs — develop around the femoral head and/or along the acetabulum. This extra bone causes abnormal contact between the hip bones, and prevents them from moving smoothly during activity. Because they do not fit together perfectly, the bones rub against each other during movement. Over time this friction can damage the joint this can result in tears of the labrum and breakdown of articular cartilage (osteoarthritis), causing pain and limiting activity. FAI may occur from deformities of the femur, which is called cam impingement, or from deformities of the socket which is called pincer impingement. It can also occur in children who suffer from deformities of both the thigh bone and the hip socket simultaneously. The bony morphologies of femoroacetabular impingement, classified as pincer-, cam-, or combined-type deformities, are often accompanied by chondrolabral abnormalities 1.
Femoroacetabular impingement (FAI) is increasingly recognized as a cause for hip and groin pain in the young, active patient 2. The prevalence of femoroacetabular impingement in the general adult population is between 10 to 15% 3. Based on clinical diagnosis, femoroacetabular impingement affects adolescents and the young adult population before radiographic signs of arthritis manifest 4. The prevalence of symptomatic athletes has been reported to be higher than the general population at 55% 5. There is also literature that has examined the prevalence of anatomic morphology consistent with this condition but in asymptomatic individuals; therefore, patients can have bony features of femoroacetabular impingement and not manifest with symptoms. A meta-analysis by Frank et al. reports a prevalence of 37% for cam deformity and 67% for pincer deformity in asymptomatic volunteers 6. When accounting for the athletic population, cam deformity prevalence was 54.8% for athletes and 23.1% for non-athletes. The pincer lesion was present in 49.5% of the athletic population. Cam deformity is more prevalent in men than women, with a reported prevalence of 9 to 25% men versus 3 to 10% in women. Pincer lesions are more common in women than men, with reports of 19.6% versus 15.2% 7.
Hip arthroscopic surgery is indicated to treat femoroacetabular impingement and related defects including labral lesions, ligamentum teres injuries, and articular cartilage delamination 8. Compared with open approaches, hip arthroscopic surgery may result in faster recovery, lower complication rates, less pain, and less morbidity 9. Over the past decade, hip arthroscopic surgery rates have risen exponentially 10. Hip arthroscopic surgery has reduced pain and improved function in patients in most age groups, body mass indices (BMIs), sexes, income levels, and activity levels 11.
Negative outcomes after hip arthroscopic surgery for femoroacetabular impingement may be defined as persistent pain, looseness, and stiffness with reduced range of motion, refractory to nonsurgical treatment or reoperation 12. Furthermore, dissatisfaction can result from an inability to return to desired activities. Failure rates for hip arthroscopic surgery range from 2.9% to 13.2% 13. Residual or unaddressed femoroacetabular impingement is the most common cause of negative outcomes in hip arthroscopic surgery 14. Other potential causes of negative outcomes include unrecognized acetabular dysplasia, soft tissue laxity, and osteoarthritis. Positive outcomes after hip arthroscopic surgery usually involve achieving the minimal clinically important difference or substantial clinical benefit on patient-reported outcome measures 15. Negative outcomes after hip arthroscopic surgery for femoroacetabular impingement are typically managed with revision arthroscopic surgery or open surgical hip dislocation but sometimes require total hip arthroplasty 14.
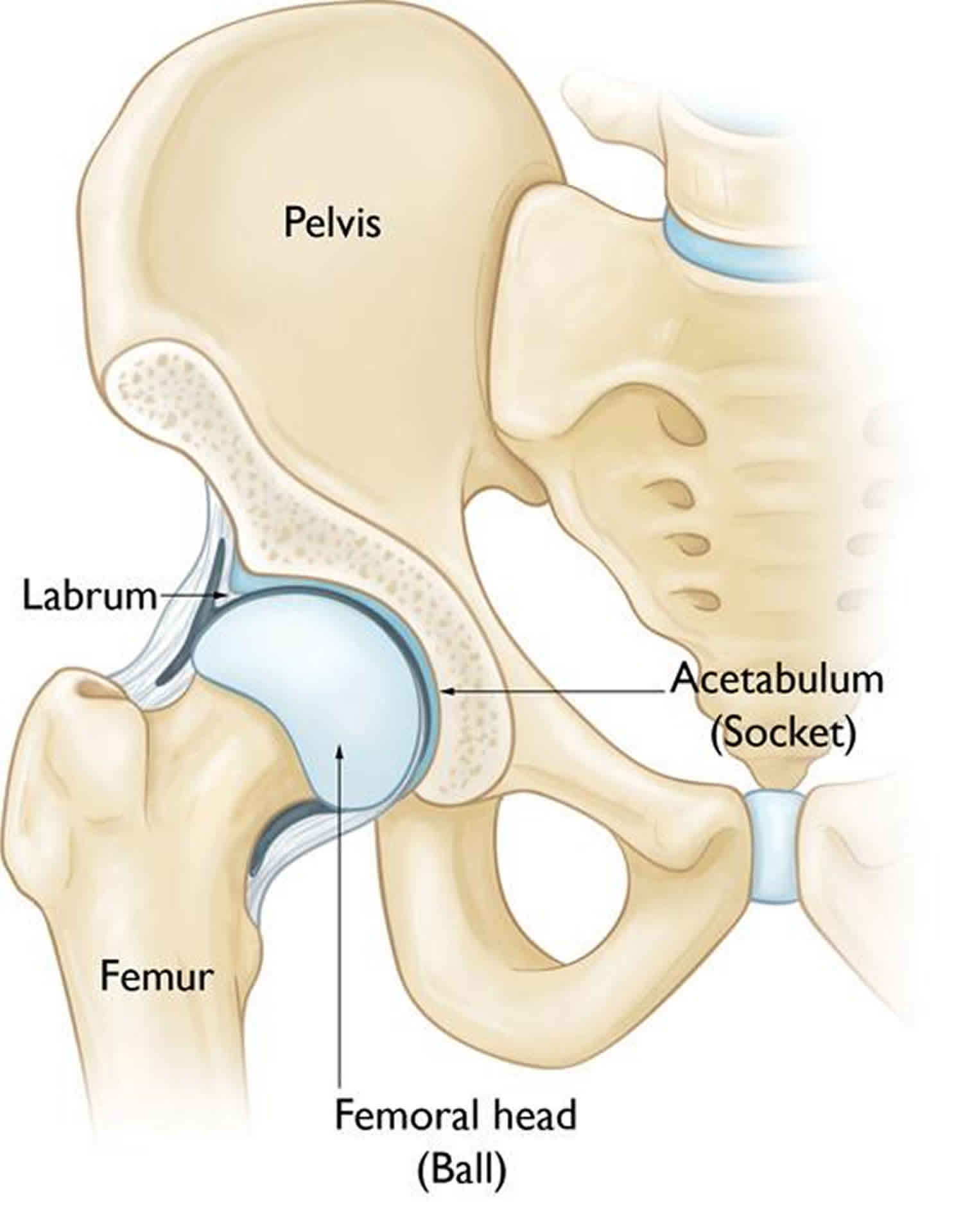
Hip joint anatomy
The hip is a ball-and-socket joint. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
A slippery tissue called articular cartilage covers the surface of the ball and the socket. It creates a smooth, low friction surface that helps the bones glide easily across each other during movement.
The acetabulum is ringed by strong fibrocartilage called the labrum. The labrum forms a gasket around the socket, creating a tight seal and helping to provide stability to the joint.
Figure 1. Hip joint anatomy (in a healthy hip, the femoral head fits perfectly into the acetabulum)
Types of FAI
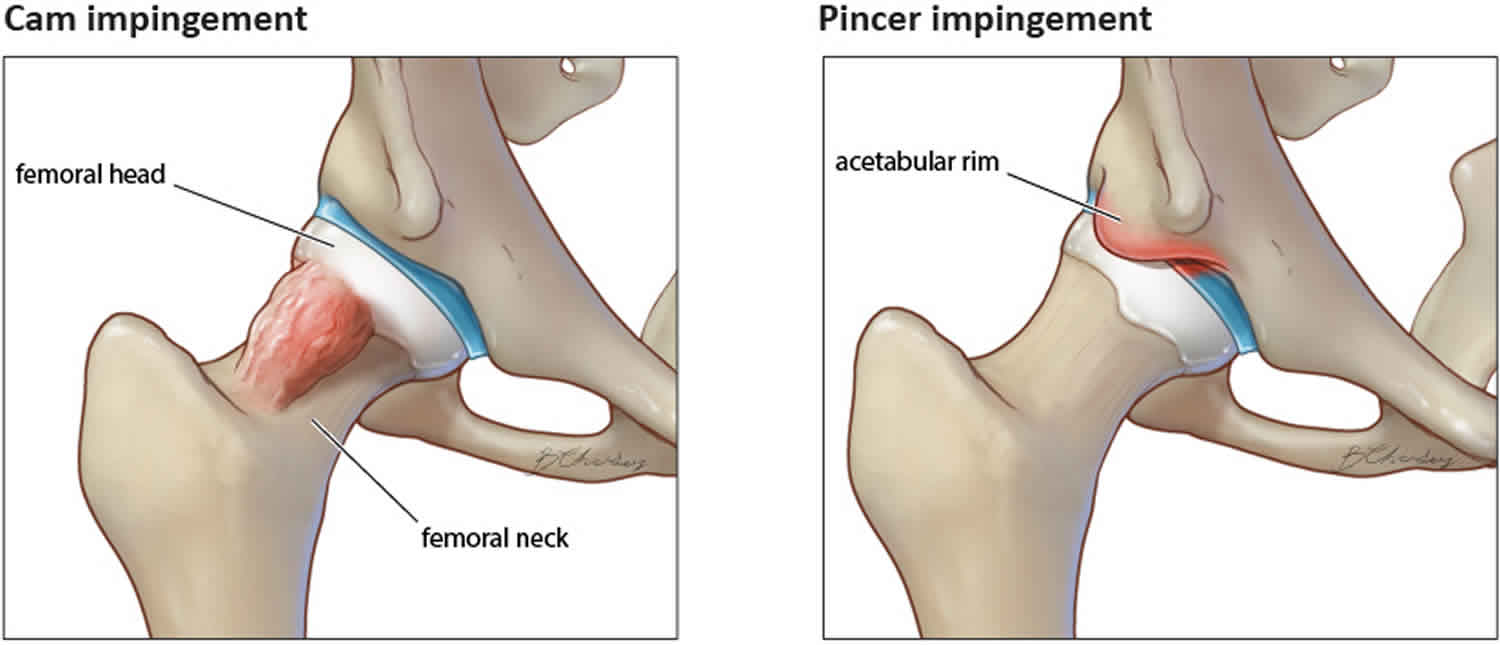
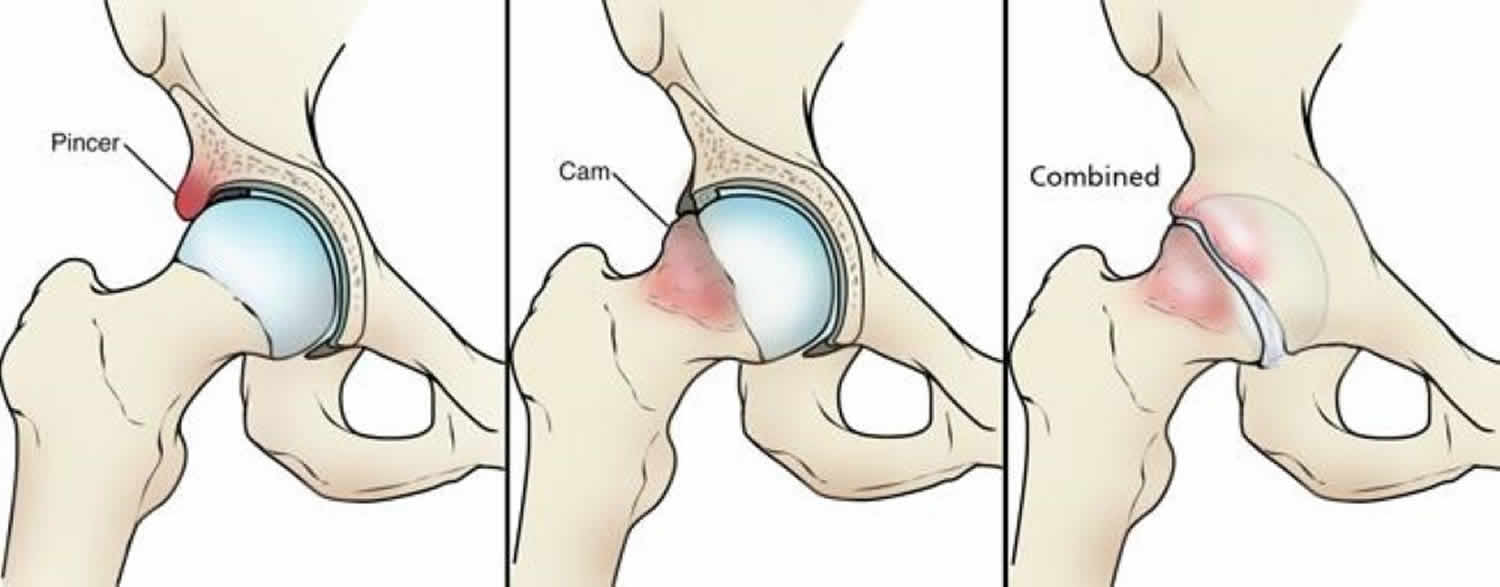
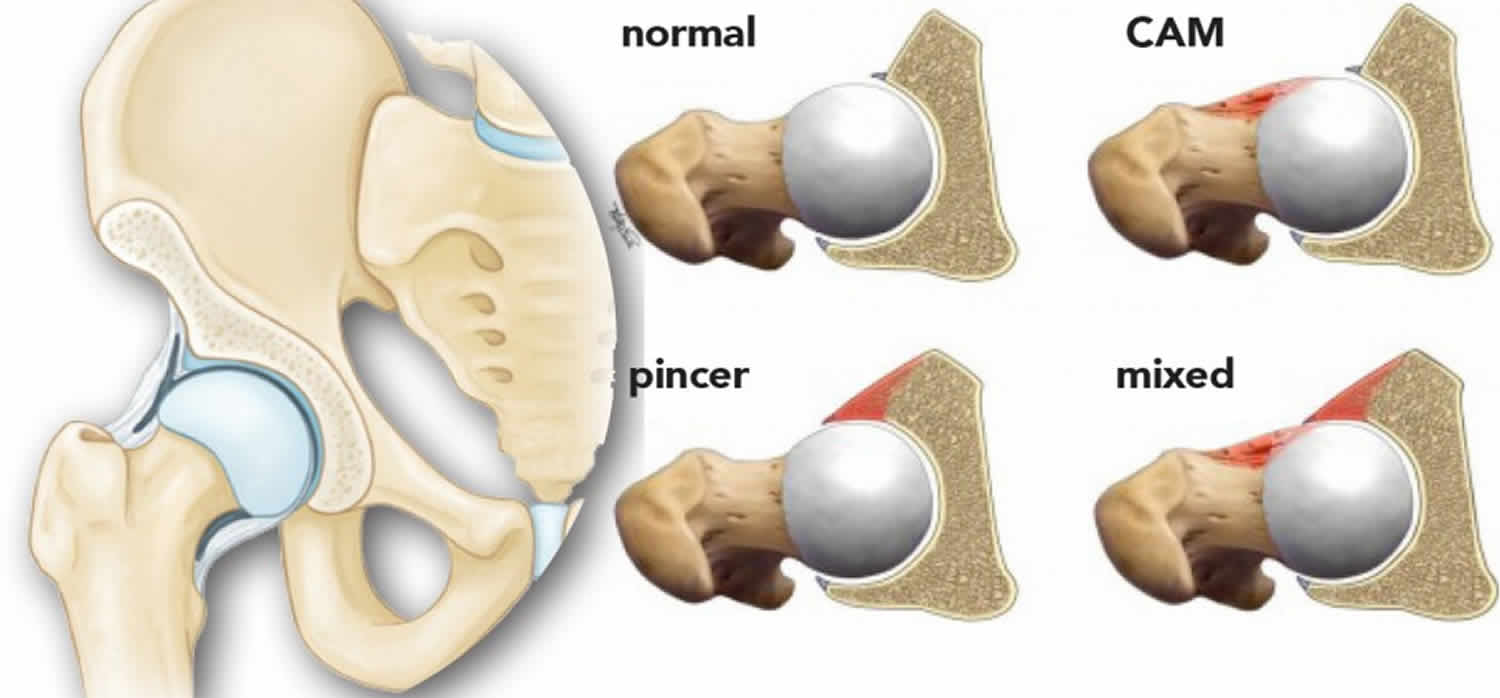
There are three types of femoroacetabular impingement (FAI): pincer, cam, and combined impingement.
- Pincer impingement. This type of impingement occurs because extra bone extends out over the normal rim of the acetabulum. The labrum can be crushed under the prominent rim of the acetabulum.
- Cam impingement. In cam impingement the femoral head is not round and cannot rotate smoothly inside the acetabulum. A bump forms on the edge of the femoral head that grinds the cartilage inside the acetabulum.
- Combined impingement. Combined impingement just means that both the pincer and cam types are present.
Figure 2. Femoroacetabular impingement
Footnote: (Left) Pincer impingement. (Center) Cam impingement. (Right) Combined impingement.
Figure 3. Femoroacetabular impingement types
Femoral acetabular impingement causes
The cause of femoroacetabular impingement is still under investigation; however, studies suggest that genetic factors may contribute to the abnormal hip pathology. Multiple studies have investigated single nucleotide polymorphisms such as GDF5, FRZB, DIO2, and HOX9 16. FRZB has been found by one study to contribute to a specific shape of proximal femur morphology on X-ray and increased development of osteoarthritis of the hip 17. DIO2 has also correlated with specific proximal femur morphology and the increased development of hip osteoarthritis 18. HOX9 was looked at in a Japanese population and found to contribute to pincer lesion formation of the acetabulum 18.
There is also evidence to suggest an increased incidence of femoroacetabular impingement in athletes due to cam deformity formation 18. More specifically, adolescents engaged in high-intensity sports were found to be ten times more likely to have a cam deformity and impingement than age-matched adolescents not participating in high-intensity sports 18. There is a theory that increased stress along the growth plate of the hip leads to increased stress reaction bone formation resulting in cam deformity and subsequent impingement.
The formation of femoroacetabular impingement has also occurred in patients with a history of slipped capital femoral epiphysis (SCFE). When this primary insult happens during childhood, the epiphysis of the femoral head slips posterior and medial respective to the metaphysis, leading to a prominent metaphysis anterior and laterally. Even after surgical in situ fixation of a slipped capital femoral epiphysis, there is residual deformity, and this can cause impingement 19.
FAI occurs because the hip bones do not form normally during the childhood growing years. It is the deformity of a cam bone spur, pincer bone spur, or both, that leads to joint damage and pain.
- Cam impingement (deformity of the thigh bone) occurs when the abnormally shaped femoral head (ball) and head-neck junction jam, or run into, the hip socket during certain activities like bending over, sitting for long periods of time, or riding a bike.
- Pincer impingement is caused by direct contact between the femoral head-neck junction and the acetabular rim in conditions where the coverage of the femoral head in the anterior region is excessive (acetabular retroversion, protrusion acetabulum etc.). Impingement of a child’s hip can also be caused due to pediatric hip disorders such as Legg-Calvé-Perthes disease, slipped capital femoral epiphysis or post-traumatic deformities.
When the hip bones are shaped abnormally, there is little that can be done to prevent femoroacetabular impingement. Femoroacetabular impingement (FAI) syndrome is caused by a prominent femoral head-neck junction (ie, cam morphology) or a prominent acetabular rim (ie, pincer morphology). Patients may also present a combination of the 2 deviations, where they have both cam and pincer morphology 20. At motion, these morphologies have the potential to cause abnormal mechanical stresses within the hip joint, which may cause subsequent soft tissue damage 21.
Activities such as running, hockey, dancing, and gymnastics are not causes of FAI, but because of the increased demand these activities place on the hips, the symptoms of FAI may occur earlier than in less active children.
It is not known how many people have femoroacetabular impingement. Some people may live long, active lives with femoroacetabular impingement and never have problems. When symptoms develop, however, it usually indicates that there is damage to the cartilage or labrum and the disease is likely to progress.
Because athletic people may work the hip joint more vigorously, they may begin to experience pain earlier than those who are less active. However, exercise does not cause femoroacetabular impingement.
Risk factors for developing femoro acetabular impingement
Risk factors for developing femoro acetabular impingement:
- Consequence of Legg-Calvé-Perthes altering the shape of the ball and socket of the hip joint
- Consequence of Slipped Capital Femoral Epiphysis altering the shape of the femoral head and acetabulum
- Activities involving repetitive motion of the hip (running, weight lifting, ice skating)
- Activities involving extreme flexion of the hip (dance, gymnastics)
- Trauma to the hip
Femoroacetabular impingement symptoms
Some people with FAI can live active lives and never experience pain or hip problems. Others, especially athletic and active people, may develop pain in the hip or thigh that is usually worse in a seated position. Clicking, popping or a pinching sensation may be felt deep in the hip joint.
Pain often occurs in the groin area or hip (front, side, and/or back) aggravated by activity and/or prolonged sitting is the most common symptom of femoroacetabular impingement (FAI). Other signs or symptoms include difficulty flexing the hip and popping or clicking of the hip. Turning, twisting, and squatting may cause a sharp, stabbing pain. Sometimes, the pain is just a dull ache.
The most common symptoms of FAI include:
- Pain
- Stiffness
- Limping
Femoroacetabular impingement diagnosis
A diagnosis of femoroacetabular impingement may be suspected after a detailed history and physical examination. X-rays can help evaluate the shape of the ball and socket to look for possible causes of impingement. The findings on X-ray are often subtle, however, and may be missed by practitioners who are unfamiliar with the condition.
During your first appointment, your doctor will discuss your general health and your hip symptoms. He or she will also examine your hip.
Impingement test
As part of the physical examination, your doctor will likely conduct the impingement test. For this test, your doctor will bring your knee up towards your chest and then rotate it inward towards your opposite shoulder. If this recreates your hip pain, the test result is positive for impingement.
Imaging tests
Your doctor may order imaging tests to help determine whether you have FAI.
- X-rays. These provide good images of bone, and will show whether your hip has abnormally shaped bones of FAI. X-rays can also show signs of arthritis.
- Computed tomography (CT) scans. More detailed than a plain x-ray, CT scans help your doctor see the exact abnormal shape of your hip.
- Magnetic resonance imaging (MRI) scans. These studies can create better images of soft tissue. They will help your doctor find damage to the labrum and articular cartilage. Injecting dye into the joint during the MRI may make the damage show up more clearly.
- Local anesthetic. Your doctor may also inject a numbing medicine into the hip joint as a diagnostic test. If the numbing medicine provides temporary pain relief, it confirms that FAI is the problem.
Femoroacetabular impingement treatment
Treatment may include non-surgical options such as activity modification, physical therapy, injections and anti-inflammatory medications. For those patients that don’t respond to non-operative treatment, hip arthroscopy or a surgical dislocation of the hip may be recommended.
When symptoms first occur, it is helpful to try and identify an activity or something you may have done that could have caused the pain. Sometimes, you can just back off on your activities, let your hip rest, and see if the pain will settle down. Over-the-counter anti-inflammatory medicines, such as ibuprofen and naproxen, may help.
If your symptoms persist, you will need to see a doctor to determine the exact cause of your pain and provide treatment options. The longer painful symptoms go untreated, the more damage FAI can cause in the hip.
Nonsurgical treatment
- Activity changes. Your doctor may first recommend simply changing your daily routine and avoiding activities that cause symptoms.
- Non-steroidal anti-inflammatory medications. Drugs like ibuprofen can be provided in a prescription-strength form to help reduce pain and inflammation.
- Physical therapy. Specific exercises can improve the range of motion in your hip and strengthen the muscles that support the joint. This can relieve some stress on the injured labrum or cartilage.
If your pain continues after a period of rest and therapy, an intra-articular injection (shot inside the joint) of numbing medication (local anesthetic) and a steroid is sometimes recommended. An injection helps clarify if the pain is coming from the joint or the surrounding muscle.
Surgical treatment
If tests show joint damage caused by FAI and your pain is not relieved by nonsurgical treatment, your doctor may recommend surgery. The surgical treatment of FAI aims to correct cam and/or pincer morphologies and repair damaged soft tissue 22. Initially, this was performed with an open surgical approach 23, but arthroscopic management has now emerged as the treatment of choice 24.
Arthroscopy
Many FAI problems can be treated with arthroscopic surgery. Arthroscopic procedures are done with small incisions and thin instruments. The surgeon uses a small camera, called an arthroscope, to view inside the hip.
During arthroscopy, your doctor can repair or clean out any damage to the labrum and articular cartilage. He or she can correct the FAI by trimming the bony rim of the acetabulum and also shaving down the bump on the femoral head.
Some severe cases may require an open operation with a larger incision to accomplish this.
Femoroacetabular impingement prognosis
Surgery can successfully reduce symptoms caused by impingement. Correcting the impingement can prevent future damage to the hip joint. However, not all of the damage can be completely fixed by surgery, especially if treatment has been put off and the damage is severe. It is possible that more problems may develop in the future.
While there is a small chance that surgery might not help, it is currently the best way to treat painful FAI.
References- Sogbein OA, Shah A, Kay J, et al. Predictors of Outcomes After Hip Arthroscopic Surgery for Femoroacetabular Impingement: A Systematic Review. Orthop J Sports Med. 2019;7(6):2325967119848982. Published 2019 Jun 19. doi:10.1177/2325967119848982 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6585257
- Frank RM, Walker G, Hellman MD, McCormick FM, Nho SJ. Evaluation of hip pain in young adults. Phys Sportsmed. 2014;42(2):38–47.
- O’Rourke RJ, El Bitar Y. Femoroacetabular Impingement. [Updated 2019 Oct 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547699
- Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin. Orthop. Relat. Res. 2004 Dec;(429):170-7.
- Lee WY, Kang C, Hwang DS, Jeon JH, Zheng L. Descriptive Epidemiology of Symptomatic Femoroacetabular Impingement in Young Athlete: Single Center Study. Hip Pelvis. 2016 Mar;28(1):29-34.
- Frank JM, Harris JD, Erickson BJ, Slikker W, Bush-Joseph CA, Salata MJ, Nho SJ. Prevalence of Femoroacetabular Impingement Imaging Findings in Asymptomatic Volunteers: A Systematic Review. Arthroscopy. 2015 Jun;31(6):1199-204.
- Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010 May;92(5):1162-9.
- Lynch TS, Terry MA, Bedi A, Kelly BT. Hip arthroscopic surgery: patient evaluation, current indications, and outcomes. Am J Sports Med. 2013;41(5):1174–1189.
- Botser IB, Jackson TJ, Smith TW, Leonard JP, Stake CE, Domb BG. Open surgical dislocation versus arthroscopic treatment of femoroacetabular impingement. Am J Orthop (Belle Mead NJ). 2014;43(5):209–214.
- Khan M, Ayeni OR, Madden K, et al. Femoroacetabular impingement: have we hit a global tipping point in diagnosis and treatment? Results from the InterNational Femoroacetabular Impingement Optimal Care Update Survey (IN FOCUS). Arthroscopy. 2016;32(5):779–787.
- Minkara AA, Westermann RW, Rosneck J, Lynch TS. Systematic review and meta-analysis of outcomes after hip arthroscopy in femoroacetabular impingement. Am J Sports Med. 2019;47(2):488–500.
- de Sa D, Phillips M, Catapano M, et al. Adhesive capsulitis of the hip: a review addressing diagnosis, treatment and outcomes. J Hip Preserv Surg. 2016;3(1):43–55.
- Cvetanovich GL, Weber AE, Kuhns BD, et al. Hip arthroscopic surgery for femoroacetabular impingement with capsular management: factors associated with achieving clinically significant outcomes. Am J Sports Med. 2018;46(2):288–296.
- Bogunovic L, Gottlieb M, Pashos G, Baca G, Clohisy JC. Why do hip arthroscopy procedures fail? Clin Orthop Relat Res. 2013;471(8):2523–2529.
- Nwachukwu BU, Chang B, Fields K, et al. Defining the “substantial clinical benefit” after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(6):1297–1303.
- Sekimoto T, Kurogi S, Funamoto T, Ota T, Watanabe S, Sakamoto T, Hamada H, Chosa E. Possible association of single nucleotide polymorphisms in the 3′ untranslated region of HOXB9 with acetabular overcoverage. Bone Joint Res. 2015 Apr;4(4):50-5.
- Baker-Lepain JC, Lynch JA, Parimi N, McCulloch CE, Nevitt MC, Corr M, Lane NE. Variant alleles of the Wnt antagonist FRZB are determinants of hip shape and modify the relationship between hip shape and osteoarthritis. Arthritis Rheum. 2012 May;64(5):1457-65.
- Packer JD, Safran MR. The etiology of primary femoroacetabular impingement: genetics or acquired deformity? J Hip Preserv Surg. 2015 Oct;2(3):249-57.
- Klit J, Gosvig K, Magnussen E, Gelineck J, Kallemose T, Søballe K, Troelsen A. Cam deformity and hip degeneration are common after fixation of a slipped capital femoral epiphysis. Acta Orthop. 2014 Dec;85(6):585-91.
- Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120.
- Beck M, Kalhor M, Leunig M, Ganz K. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018.
- Sansone M, Ahlden M, Jonasson P, et al. A Swedish hip arthroscopy registry: demographics and development. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):774–780.
- Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124.
- Khan M, Ayeni OR, Madden K, et al. Femoroacetabular impingement: have we hit a global tipping point in diagnosis and treatment? Results from the International Femoroacetabular Impingement Optimal Care Update Survey (IN FOCUS). Arthroscopy. 2016;32(5):779–787.