Fetor hepaticus
Fetor hepaticus is a late sign of liver failure and is one of the clinical features of hepatic encephalopathy where portal hypertension with portosystemic shunting allows thiols to pass directly into your lungs causing sweet, musty aroma of the breath or even slightly fecal aroma 1. Other possible causes are the presence of ammonia and ketones in the breath. Chronic liver disease and cirrhosis affect more than 5.5 million people in the United States and hundreds of millions all over the world 2.
The compound dimethyl sulfide and to a lower extent by ketones (acetone) have been associated with fetor hepaticus 1, raising the possibility of an objective noninvasive measure of liver failure. Furthermore, the volatile dimethyl sulfide is thought by some researchers to be the main contributor to the odor of fetor hepaticus 3. A secondary form of trimethylaminuria is also associated with liver failure, and it has been suggested that that trimethylamine is also a contributor to the odor of fetor hepaticus 3. Excessive amounts of trimethylamine may well contribute to the overall body odor problems encountered among patients with severe hepatic disease, precipitating in these individuals a secondary form of the ‘fish-odor syndrome’ 4.
Fetor hepaticus causes
Fetor hepaticus is a late sign of liver failure and is one of the clinical features of hepatic encephalopathy where portal hypertension with portosystemic shunting allows thiols to pass directly into your lungs causing sweet, musty aroma of the breath or even slightly fecal aroma 1. Other possible causes are the presence of ammonia and ketones in the breath.
Fetor hepaticus is associated with severe liver disease, which causes scarring and poor functioning of your liver. This can result in portal hypertension, which refers to increased blood pressure in the veins of your liver. Portal hypertension makes it hard for blood to flow through your liver, so it gets backed up in the veins surrounding your liver.
When blood doesn’t pass easily through your liver, the toxic substances that would usually be filtered out by your liver make their way to other parts of your body, including your lungs. When this happens, you might smell traces of these substances when you exhale. Dimethylsulfide is likely responsible for the distinct smell of fetor hepaticus.
Fetor hepaticus symptoms
The main symptom of fetor hepaticus is breath that smells like a combination of rotten eggs and garlic or even slightly fecal aroma 5.
Signs and symptoms of liver failure may include:
- Yellowing of your skin and eyeballs (jaundice)
- Pain in your upper right abdomen
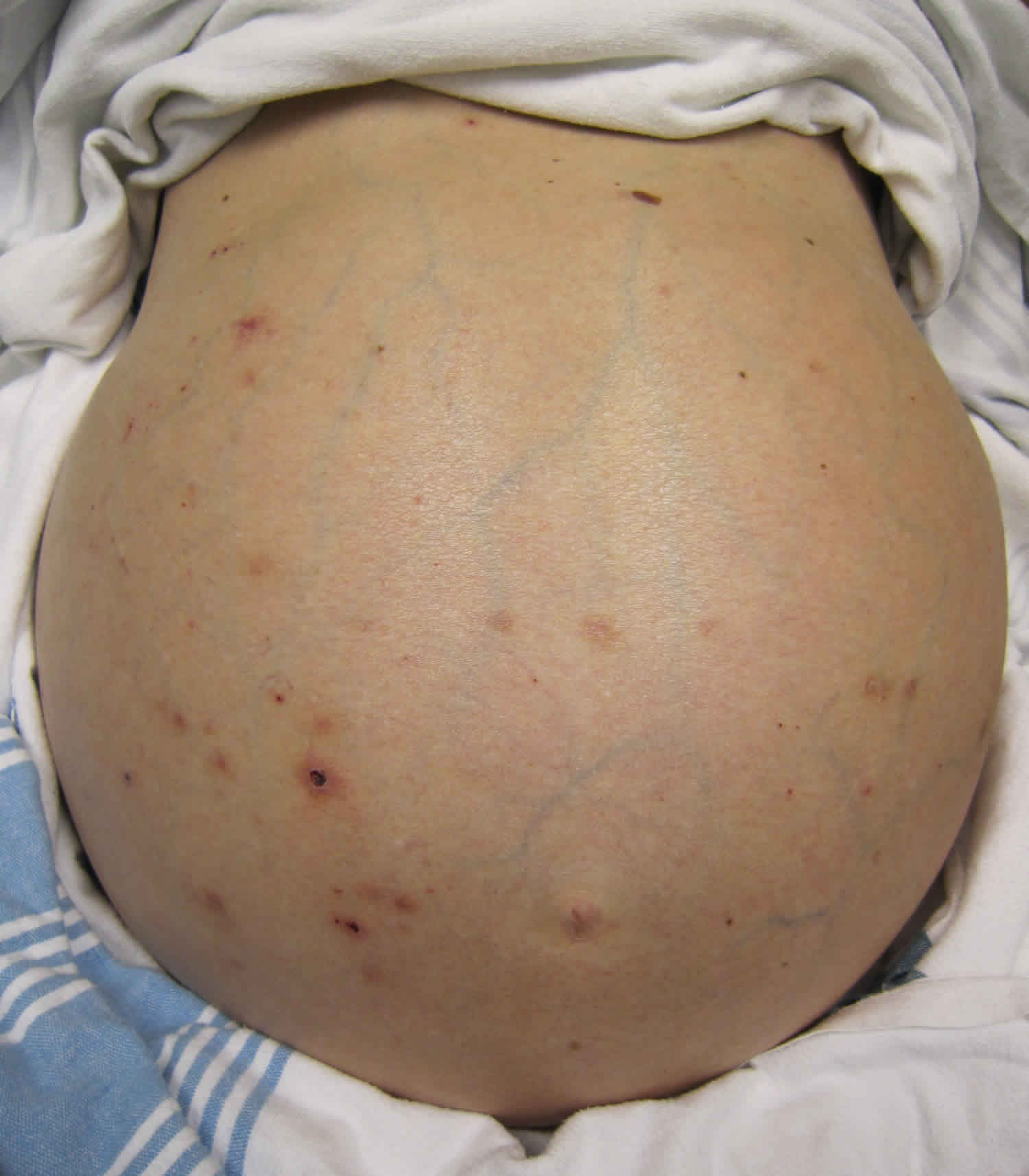
- Abdominal swelling
- Nausea
- Vomiting
- A general sense of feeling unwell (malaise)
- Disorientation or confusion
- Sleepiness
Fetor hepaticus treatment
Hepatic encephalopathy treatment
Hepatic encephalopathy also known as portosystemic encephalopathy, is a syndrome of largely reversible impairment of brain function occurring in patients with acute or chronic liver failure or when the liver is bypassed by portosystemic shunts 2. This leads to a spectrum of neurological impairments ranging from subclinical brain dysfunction to coma. The mechanisms causing this brain dysfunction are still largely unclear 6. Hepatic encephalopathy is classified into three types based on the underlying liver disease 2:
- Type A: Hepatic encephalopathy associated with acute liver failure
- Type B: Hepatic encephalopathy associated with porto-systemic shunts and no intrinsic hepatocellular disease
- Type C: Hepatic encephalopathy associated with cirrhosis and portal hypertension or porto-systemic shunts
The approach to a patient with hepatic encephalopathy depends upon the severity of mental status changes and upon the certainty of the diagnosis. As an example, a patient with known cirrhosis and mild complaints of decreased concentration might be served best by an empiric trial of rifaximin or lactulose and a follow-up office visit to check its effect. However, a patient presenting to the emergency department with severe hepatic encephalopathy requires a different approach. General management recommendations include the following 7:
- Exclude nonhepatic causes of altered mental function.
- Consider checking an arterial ammonia level in the initial assessment of a hospitalized patient with cirrhosis and with impaired mental function. Ammonia levels have less use in a stable outpatient.
- Precipitants of hepatic encephalopathy, such as hypovolemia, metabolic disturbances, gastrointestinal bleeding, infection, and constipation, should be corrected.
- Avoid medications that depress central nervous system function, especially benzodiazepines. Patients with severe agitation and hepatic encephalopathy may receive haloperidol as a sedative. Treating patients who present with coexisting alcohol withdrawal and hepatic encephalopathy is particularly challenging. These patients may require therapy with benzodiazepines in conjunction with lactulose and other medical therapies for hepatic encephalopathy.
- Patients with severe encephalopathy (ie, grade 3 or 4) who are at risk for aspiration should undergo prophylactic endotracheal intubation. They are optimally managed in the intensive care unit.
Most current therapies are designed to treat hyperammonemia that is a hallmark of most cases of hepatic encephalopathy.
Treatments to decrease intestinal ammonia production
Diet
In the late 19th century, it was recognized that the feeding of a high-protein diet to dogs that had undergone portosystemic shunt surgery could produce symptoms of abnormal coordination and stupor in the treated animals.
In the 20th century, low-protein diets were routinely recommended for patients with cirrhosis, in the hope of decreasing intestinal ammonia production and in preventing exacerbations of hepatic encephalopathy. An obvious consequence was the worsening of preexisting protein-energy malnutrition. Protein restriction may be appropriate in some patients immediately following a severe flare of symptoms (ie, episodic hepatic encephalopathy). However, protein restriction is rarely justified in patients with cirrhosis and persistent hepatic encephalopathy. Indeed, malnutrition is a more serious clinical problem than hepatic encephalopathy for many of these patients.
In the author’s experience, it is an infrequent patient who is intolerant of a diet high in protein 7. Most patients with mild chronic hepatic encephalopathy tolerate more than 60-80 g of protein per day. Furthermore, one study administered a protein-rich diet (>1.2 g/kg/day) to patients with advanced disease awaiting liver transplantation, without inducing a flare of encephalopathy symptoms 8. Another study randomized patients with severe episodic encephalopathy to either a low-protein diet or a high-protein diet, administered via nasogastric tube 9. All patients received the same regimen of neomycin per nasogastric tube. Mental function improved at the same rate in both treatment groups. Importantly, patients receiving the low-protein diet had evidence of increased protein breakdown during the duration of the study.
Diets containing vegetable proteins appear to be better tolerated than diets rich in animal protein, especially proteins derived from red meats. This may be because of increased content of dietary fiber, a natural cathartic, and decreased levels of aromatic amino acids. Aromatic amino acids, as precursors of the false neurotransmitters tyramine and octopamine, are thought to inhibit dopaminergic neurotransmission and worsen hepatic encephalopathy.
The author recommends that patients consume well-cooked chicken and fish in addition to vegetable proteins 7. Malnourished patients are encouraged to add commercially available liquid nutritional supplements to their diet. Patients rarely require specialized treatment with oral or enteral supplements rich in branched-chain amino acids.
To evaluate the beneficial and harmful effects of branched-chain amino acids (BCAA) versus any control intervention for people with hepatic encephalopathy, Gluud and colleagues 10 conducted a systematic review involving 16 randomized clinical trials that included 827 participants with hepatic encephalopathy. Primary outcomes included mortality (all cause), hepatic encephalopathy (number of people without improved manifestations of hepatic encephalopathy), and adverse events. The control groups received placebo/no intervention, diets, lactulose, or neomycin. In 15 trials, all participants had cirrhosis. Analyses showed that BCAA had a beneficial effect on hepatic encephalopathy. The authors found no effect of BCAA on mortality, quality of life, or nutritional parameters, but they recommended additional trials to evaluate these outcomes 10.
Cathartics
Lactulose (beta-galactosidofructose) and lactilol (beta-galactosidosorbitol) are nonabsorbable disaccharides that have been in common clinical use since the early 1970s (the latter is not available in the United States). They are degraded by intestinal bacteria to lactic acid and other organic acids.
Lactulose appears to inhibit intestinal ammonia production by a number of mechanisms. The conversion of lactulose to lactic acid and acetic acid results in the acidification of the gut lumen 11. This favors conversion of ammonia (NH3) to ammonium (NH4+); owing to the resultant relative impermeability of the membrane, the NH4+ ions are not easily absorbed, thereby remaining trapped in the colonic lumen, and there is a reduction in plasma NH3 12. Gut acidification inhibits ammoniagenic coliform bacteria, leading to increased levels of nonammoniagenic lactobacilli 11. Lactulose also works as a cathartic, reducing colonic bacterial load.
Initial lactulose dosing is 30 mL orally, daily or twice daily. The dose may be increased as tolerated. Patients should be instructed to reduce lactulose dosing in the event of diarrhea, abdominal cramping, or bloating. Patients should take sufficient lactulose as to have 2-4 loose stools per day.
Great care must be taken when prescribing lactulose. Overdosage can result in ileus, severe diarrhea, electrolyte disturbances, and hypovolemia. Hypovolemia may be sufficiently severe as to actually induce a flare of encephalopathy symptoms.
High doses of lactulose (e.g., 30 mL every 2-4 hours) may be administered orally or by nasogastric tube to patients hospitalized with severe hepatic encephalopathy. Lactulose may be administered as an enema to patients who are comatose and unable to take the medication by mouth. The recommended dosing is 300 mL lactulose plus 700 mL water, administered as a retention enema every 4 hours as needed.
Lactulose has been the subject of dozens of clinical trials over almost four decades. Many small trials demonstrated the medication’s efficacy in the treatment of hepatic encephalopathy. A controversial meta-analysis published in 2004 contradicted these trials and most physicians’ clinical experiences 13. When assessing high-quality randomized trials, lactulose was no more effective than placebo at improving encephalopathy symptoms. In trials comparing lactulose to an antibiotic (eg, neomycin, rifaximin), lactulose was actually inferior to antibiotic therapy.
In subsequent years, multiple randomized trials have reinvestigated the efficacy of lactulose.
In patients with minimal hepatic encephalopathy, lactulose was more effective than placebo in terms of improving patient performance on psychometric testing 14.
Lactulose was studied in large randomized trials as secondary prevention against recurrent overt encephalopathy 15. In the study by Sharma et al. 16, patients who were recovering from hepatic encephalopathy were randomized to receive lactulose (n = 61) or placebo (n = 64). Over a median follow-up of 14 months, 12 patients (19.6%) in the lactulose group developed overt hepatic encephalopathy as compared with 30 patients (46.8%) in the placebo group. The authors concluded that lactulose effectively prevented the recurrence of overt hepatic encephalopathy in patients with cirrhosis 16.
Lactulose also appeared to be effective as primary prophylaxis against the development of overt hepatic encephalopathy 17, although few physicians in the United States would advocate the use of lactulose for this indication.
An updated meta-analysis published in 2013 included these studies and affirmed the utility of lactulose in the management of hepatic encephalopathy 18,
Antibiotics
Neomycin and other antibiotics, such as metronidazole, oral vancomycin, paromomycin, and oral quinolones, are administered in an effort to decrease the colonic concentration of ammoniagenic bacteria. Initial neomycin dosing is 250 mg orally 2-4 times a day. Doses as high as 4000 mg/day may be administered. Neomycin is usually reserved as a second-line agent, after initiation of treatment with lactulose. Long-term treatment with this oral aminoglycoside runs the risks of inducing ototoxicity and nephrotoxicity because of some systemic absorption.
Rifaximin (Xifaxan), a nonabsorbable derivative of rifampin, has been used in Europe for more than 20 years for a wide variety of gastrointestinal indications. Multiple clinical trials have demonstrated that rifaximin at a dose of 400 mg taken orally 3 times a day was as effective as lactulose or lactitol at improving hepatic encephalopathy symptoms 19. Similarly, rifaximin was as effective as neomycin and paromomycin. Rifaximin had a tolerability profile comparable to placebo. It was better tolerated than both the cathartics and the other nonabsorbable antibiotics. A potential mechanism for rifaximin’s clinical activity is its effects on the metabolic function of the gut microbiota, rather than a change in the relative bacterial abundance 20.
In 2004, rifaximin received approval by the FDA in the United States for the treatment of travelers’ diarrhea. In 2005, it received orphan drug status as a treatment for hepatic encephalopathy. In March 2010, rifaximin was approved by the FDA to reduce recurrence of hepatic encephalopathy. The approval was based on a phase 3 clinical trial conducted by Bass et al. 21.
Bass et al evaluated rifaximin’s ability to reduce the risk of recurrent hepatic encephalopathy 21. In this double-blind, placebo-controlled, multinational, phase 3 clinical trial, 299 patients received either rifaximin 550 mg or placebo twice daily. Each group also received lactulose. Breakthrough episodes of hepatic encephalopathy occurred in 22% of patients treated with rifaximin and 46% of patients with placebo. Hepatic encephalopathy-related hospitalization occurred in 14% of patients treated with rifaximin and 23% of patients treated with placebo.
Peripheral edema and nausea are described in some rifaximin-treated patients. There are also questions whether long-term treatment with rifaximin can induce microbial resistance. Thus far, microbial resistance has not been reported in patients using the medication. It remains unclear whether diarrhea caused by Clostridium difficile occurs at a higher rate in rifaximin-treated patients than untreated patients. In the study by Bass et al, two rifaximin-treated patients and no placebo-treated patients developed Clostridium difficile infection 21.
Rifaximin was also examined in patients with minimal hepatic encephalopathy. In a large study by Sidhu et al, rifaximin was more effective than placebo in terms of improving patient performance on psychometric testing and in terms of improving health-related quality of life 22.
Treatments to increase ammonia clearance
L-ornithine L-aspartate
L-ornithine L-aspartate (LOLA) (Hepa-Merz) is available in Europe in both intravenous formulations and oral formulations. It is not available in the United States. L-ornithine L-aspartate (LOLA) is a stable salt of the two constituent amino acids. L-ornithine stimulates the urea cycle, with resulting loss of ammonia. Both l-ornithine and l-aspartate are substrates for glutamate transaminase. Their administration results in increased glutamate levels. Ammonia is subsequently used in the conversion of glutamate to glutamine by glutamine synthetase. L-ornithine L-aspartate (LOLA) was found to be effective in treating hepatic encephalopathy in a number of European trials 23.
Zinc
Zinc deficiency is common in cirrhosis. Even in patients who are not zinc deficient, zinc administration has the potential to improve hyperammonemia by increasing the activity of ornithine transcarbamylase, an enzyme in the urea cycle. The subsequent increase in ureagenesis results in the loss of ammonia ions.
Zinc sulfate and zinc acetate have been used at a dose of 600 mg orally every day in clinical trials. Hepatic encephalopathy improved in two studies 24; there was no improvement in mental function in two other studies 25.
Meena et al 26 evaluated the correlation between low serum zinc levels in 75 patients with decompensated chronic liver disease and various stages of hepatic encephalopathy. There was a statistically significant association between low serum zinc level and grade of hepatic encephalopathy or class of liver cirrhosis. Additional studies are needed to establish the role of correcting hypozincemia to prevent worsening of cirrhosis and development of encephalopathy 26.
Sodium benzoate, sodium phenylbutyrate, sodium phenylacetate, glycerol phenylbutyrate
Sodium benzoate interacts with glycine to form hippurate. The subsequent renal excretion of hippurate results in the loss of ammonia ions. Dosing of sodium benzoate at 5 g orally twice a day can effectively control hepatic encephalopathy 27. Use of the medication is limited by the risk of salt overload and by its unpleasant taste. The medication, also used as a food preservative, is available through many specialty chemical manufacturers throughout the United States. The author has limited its use to patients with severe encephalopathy symptoms. However, in the author’s opinion, doses of sodium benzoate as low as 2.5 g orally three times per week significantly improved mental function in outpatients who had persistent encephalopathy symptoms despite cotherapy with lactulose and rifaximin.
Sodium phenylbutyrate is converted to phenylacetate. Phenylacetate, in turn, reacts with glutamine to form phenylacetylglutamine. This chemical is subsequently excreted in the urine, with the loss of ammonia ions. Sodium phenylbutyrate (Buphenyl), intravenous sodium phenylacetate in combination with sodium benzoate (Ammonul), and glycerol phenylbutyrate (Ravicti) are approved by the FDA for the treatment of hyperammonemia associated with urea cycle disorders 28. The latter is currently in clinical trials in cirrhotic patients with hepatic encephalopathy 29.
In a phase II trial involving 178 patients with cirrhosis (including 59 already taking rifaximin) who had experienced two or more hepatic encephalopathy events in the previous 6 months, glycerol phenylbutyrate, at a dose of 6 mL orally twice-daily, significantly reduced the proportion of patients who experienced an hepatic encephalopathy event, time to first event, and total events 30. In addition, glycerol phenylbutyrate was associated with fewer hepatic encephalopathy hospitalizations. For patients not on rifaximin at enrollment, glycerol phenylbutyrate reduced the proportion of patients with an hepatic encephalopathy event, time to first event, and total events. Plasma ammonia was significantly lower in patients on glycerol phenylbutyrate than in patients on placebo. Adverse events occurred in a similar proportion of patients in the glycerol phenylbutyrate and placebo groups. The authors concluded that the results implicated ammonia in the pathogenesis of hepatic encephalopathy and suggested that glycerol phenylbutyrate had therapeutic potential in this patient population 30.
L-carnitine
L-carnitine improved hepatic encephalopathy symptoms in several small studies of patients with cirrhosis 31. Whether the medication works by improving blood ammonia levels or whether it works centrally perhaps by decreasing brain ammonia uptake remains unclear 32.
Treatments to improve sleep disturbances
Sleep disturbances are more common in patients with cirrhosis than in control subjects. Whether or not this relates to hepatic encephalopathy is unclear. A trial compared the histamine H1 blocker hydroxyzine with placebo in patients with cirrhosis and minimal hepatic encephalopathy 33. Sleep efficiency and the patients’ subjective quality of sleep improved in patients receiving hydroxyzine (25 mg) at bedtime. However, there was no accompanying improvement in cognition, as measured by neurophysiologic tests. The authors urged caution when prescribing hydroxyzine, on account of the risk of worsening encephalopathy in some patients.
Post-TIPS hepatic encephalopathy
Hepatic encephalopathy is seen in about 1 in 3 patients who undergo the creation of a transjugular intrahepatic portosystemic shunt (TIPS). Typically, post-TIPS encephalopathy symptoms are well controlled with the use of rifaximin or lactulose. However, post-TIPS encephalopathy symptoms can be profound in some instances. In a study by Fanelli et al. 34, 12 of 189 patients undergoing TIPS developed encephalopathy that was refractory to conventional therapy with lactulose. These patients subsequently underwent placement of an hourglass-shaped balloon-expandable polytetrafluoroethylene (ePTFE) stent-graft inside the original shunt. Encephalopathy symptoms resolved in all of the patients over the next 18-26 hours 34. Such a procedure is not expected to improve a patient’s overall condition. At the end of a mean of 74 weeks of follow-up, only 5 of the 12 patients remained alive and in good clinical condition.
Trebicka et al 35 studied the outcomes of diameter of covered, self-expandable nitinol stents in patients with a TIPS. Of 185 patients, 53 received 8 mm stents and the remaining received 10 mm stents. Patients who received 8 mm stents survived significantly longer than patients who received 10 mm stents, regardless whether they were fully dilated or underdilated. The authors concluded that the 8 mm stent is associated with a prolonged survival compared to 10 mm stents, independent of liver specific prognostic criteria 35.
Portal hypertension treatment
Portal hypertension is assumed to be present when a patient with chronic liver disease has collateral circulation, splenomegaly, ascites, or portosystemic encephalopathy. Proof requires measurement of the hepatic venous pressure gradient, which approximates portal pressure, by a transjugular catheter; however, this procedure is invasive and usually not done. Imaging may help when cirrhosis is suspected. Ultrasonography or CT often reveals dilated intra-abdominal collaterals, and Doppler ultrasonography can determine portal vein patency and flow.
Esophagogastric varices and portal hypertensive gastropathy are best diagnosed by endoscopy, which may also identify predictors of esophagogastric variceal bleeding (eg, red markings on a varix).
Mortality during acute variceal hemorrhage may exceed 50%. Prognosis is predicted by the degree of hepatic reserve and the degree of bleeding. For survivors, the bleeding risk within the next 1 to 2 years is 50 to 75%. Ongoing endoscopic or drug therapy lowers the bleeding risk but decreases long-term mortality only marginally.
When possible, the underlying disorder is treated.
In patients with esophagogastric varices that have bled, combined endoscopic and drug treatment decreases mortality and reduces risk of rebleeding better than either therapy used alone. A series of endoscopic banding sessions are done to obliterate residual varices, then periodic endoscopic surveillance is done to identify and treat recurrent varices. Long-term drug therapy usually involves nonselective beta-blockers; these drugs lower portal pressure primarily by diminishing portal flow, although the effects vary. Agents include propranolol (40 to 80 mg orally twice a day), nadolol (40 to 160 mg orally once a day), timolol (10 to 20 mg orally twice a day), and carvedilol (6.25 to 12.5 mg orally twice a day), with dosage titrated to decrease heart rate by about 25%. Adding isosorbide mononitrate 10 to 20 mg orally twice a day may further reduce portal pressure 36.
In patients with esophagogastric varices that have not yet bled (ie, for primary prophylaxis), outcomes are similar with beta blocker therapy or endoscopic therapy.
Patients who do not adequately respond to either treatment should be considered for transjugular intrahepatic portosystemic shunting (TIPS) or, less frequently, a surgical portacaval shunt. In TIPS, the shunt is created by placing a stent between the portal and hepatic venous circulation within the liver. Although TIPS may result in fewer immediate deaths than surgical shunting, particularly during acute bleeding, maintenance of patency may require repeat procedures because the stent may become stenosed or occluded over time. Long-term benefits are unknown. Liver transplantation may be indicated for some patients.
For bleeding due to portal hypertensive gastropathy, drugs can be used to decrease portal pressure. A shunt should be considered if drugs are ineffective, but results may be less successful than for esophagogastric variceal bleeding.
Because it rarely causes clinical problems, hypersplenism requires no specific treatment, and splenectomy should be avoided.
References- Van den Velde S, Nevens F, Van Hee P, van Steenberghe D, Quirynen M (November 2008). “GC-MS analysis of breath odor compounds in liver patients”. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 875 (2): 344–8. doi:10.1016/j.jchromb.2008.08.031 https://doi.org/10.1016/j.jchromb.2008.08.031
- Bleibel W, Al-Osaimi AM. Hepatic encephalopathy. Saudi J Gastroenterol. 2012;18(5):301–309. doi:10.4103/1319-3767.101123 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3500018
- Tangerman, A (Feb 19, 1994). “Cause and composition of foetor hepaticus”. Lancet. 343 (8895): 483. doi:10.1016/s0140-6736(94)92729-4 https://doi.org/10.1016/S0140-6736(94)92729-4
- Trimethylamine and foetor hepaticus. Scand J Gastroenterol. 1999 May;34(5):524-8. DOI:10.1080/003655299750026281 https://doi.org/10.1080/003655299750026281
- Trimethylamine and foetor hepaticus. Scand J Gastroenterol. 1999 May;34(5):524-8. https://doi.org/10.1080/003655299750026281
- Seyan AS, Hughes RD, Shawcross DL. Changing face of hepatic encephalopathy: Role of inflammation and oxidative stress. World J Gastroenterol. 2010;16:3347–57
- Hepatic Encephalopathy. https://emedicine.medscape.com/article/186101-overview
- Guy S, Tanzer-Torres G, Palese M, et al. Does nasoenteral nutritional support reduce mortality after liver transplant?. Hepatology. 1995. 22:144A.
- Cordoba J, Lopez-Hellin J, Planas M, et al. Normal protein diet for episodic hepatic encephalopathy: results of a randomized study. J Hepatol. 2004 Jul. 41(1):38-43.
- Gluud LL, Dam G, Les I, et al. Branched-chain amino acids for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2015 Sep 17. 9:CD001939
- Sharma P, Agrawal A, Sharma BC, Sarin SK. Prophylaxis of hepatic encephalopathy in acute variceal bleed: a randomized controlled trial of lactulose versus no lactulose. J Gastroenterol Hepatol. 2011 Jun. 26(6):996-1003.
- Satyanarayana U, Chakrapani U. Carbohydrates. Biochemistry. 4th ed. New Delhi, India: Elsevier; 2013. Chapter 2.
- Als-Nielsen B, Gluud LL, Gluud C. Non-absorbable disaccharides for hepatic encephalopathy: systematic review of randomised trials. BMJ. 2004 May 1. 328(7447):1046.
- Mittal VV, Sharma BC, Sharma P, Sarin SK. A randomized controlled trial comparing lactulose, probiotics, and L-ornithine L-aspartate in treatment of minimal hepatic encephalopathy. Eur J Gastroenterol Hepatol. 2011 Aug. 23(8):725-32.
- Agrawal A, Sharma BC, Sharma P, Sarin SK. Secondary prophylaxis of hepatic encephalopathy in cirrhosis: an open-label, randomized controlled trial of lactulose, probiotics, and no therapy. Am J Gastroenterol. 2012 Jul. 107(7):1043-50.
- Sharma BC, Sharma P, Agrawal A, Sarin SK. Secondary prophylaxis of hepatic encephalopathy: an open-label randomized controlled trial of lactulose versus placebo. Gastroenterology. 2009 Sep. 137(3):885-91, 891.e1.
- Sharma P, Sharma BC, Agrawal A, Sarin SK. Primary prophylaxis of overt hepatic encephalopathy in patients with cirrhosis: an open labeled randomized controlled trial of lactulose versus no lactulose. J Gastroenterol Hepatol. 2012 Aug. 27(8):1329-35.
- Gluud LL, Dam G, Borre M, et al. Lactulose, rifaximin or branched chain amino acids for hepatic encephalopathy: what is the evidence?. Metab Brain Dis. 2013 Jun. 28(2):221-5.
- Mas A, Rodes J, Sunyer L, et al. Comparison of rifaximin and lactitol in the treatment of acute hepatic encephalopathy: results of a randomized, double-blind, double-dummy, controlled clinical trial. J Hepatol. 2003 Jan. 38(1):51-8.
- Bajaj JS. Review article: potential mechanisms of action of rifaximin in the management of hepatic encephalopathy and other complications of cirrhosis. Aliment Pharmacol Ther. 2016 Jan. 43 suppl 1:11-26.
- Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010 Mar 25. 362(12):1071-81.
- Sidhu SS, Goyal O, Mishra BP, Sood A, Chhina RS, Soni RK. Rifaximin improves psychometric performance and health-related quality of life in patients with minimal hepatic encephalopathy (the RIME Trial). Am J Gastroenterol. 2011 Feb. 106(2):307-16.
- Delcker AM, Jalan R, Comes G. L-ornithine-l-aspartate vs. placebo in the treatment of hepatic encephalopathy: a meta-analysis of randomised placebo-controlled trials using individual data. Hepatology. 2000. 32:310A.
- Marchesini G, Fabbri A, Bianchi G, et al. Zinc supplementation and amino acid-nitrogen metabolism in patients with advanced cirrhosis. Hepatology. 1996 May. 23(5):1084-92.
- Bresci G, Parisi G, Banti S. Management of hepatic encephalopathy with oral zinc supplementation: a long-term treatment. Eur J Med. 1993 Aug-Sep. 2(7):414-6.
- Meena RK, G S, Saravanan P, P K, Ramadoss K, A V. Serum zinc level in decompensated liver disease and its correlation with stage of hepatic encephalopathy. J Assoc Physicians India. 2019 Jan. 67(1):30-2.
- Sushma S, Dasarathy S, Tandon RK, et al. Sodium benzoate in the treatment of acute hepatic encephalopathy: a double-blind randomized trial. Hepatology. 1992 Jul. 16(1):138-44.
- Batshaw ML, MacArthur RB, Tuchman M. Alternative pathway therapy for urea cycle disorders: twenty years later. J Pediatr. 2001 Jan. 138(1 Suppl):S46-54; discussion S54-5.
- Ghabril M, Zupanets IA, Vierling J, et al. Glycerol phenylbutyrate in patients with cirrhosis and episodic hepatic encephalopathy: A pilot study of safety and effect on venous ammonia concentration. Clin Pharmacol Drug Dev. 2013 Jul. 2(3):278-84.
- Rockey DC, Vierling JM, Mantry P, et al, for the HALT-HE Study Group. Randomized, double-blind, controlled study of glycerol phenylbutyrate in hepatic encephalopathy. Hepatology. 2014 Mar. 59(3):1073-83.
- Malaguarnera M, Pistone G, Elvira R, et al. Effects of L-carnitine in patients with hepatic encephalopathy. World J Gastroenterol. 2005 Dec 7. 11(45):7197-202.
- Therrien G, Rose C, Butterworth J, et al. Protective effect of L-carnitine in ammonia-precipitated encephalopathy in the portacaval shunted rat. Hepatology. 1997 Mar. 25(3):551-6.
- Spahr L, Coeytaux A, Giostra E, et al. Histamine H1 blocker hydroxyzine improves sleep in patients with cirrhosis and minimal hepatic encephalopathy: a randomized controlled pilot trial. Am J Gastroenterol. 2007 Apr. 102(4):744-53.
- Fanelli F, Salvatori FM, Rabuffi P, et al. Management of refractory hepatic encephalopathy after insertion of TIPS: long-term results of shunt reduction with hourglass-shaped balloon-expandable stent-graft. AJR Am J Roentgenol. 2009 Dec. 193(6):1696-702.
- Trebicka J, Bastgen D, Byrtus J, et al. Smaller diameter covered transjugular intrahepatic portosystemic shunt stents are associated with increased survival. Clin Gastroenterol Hepatol. 2019 Mar 30.
- Albillos A, Zamora J, Martínez J, et al: Stratifying risk in the prevention of recurrent variceal hemorrhage: Results of an individual patient meta-analysis. Hepatology 66:1219-1231, 2017.