What is fibrodysplasia ossificans progressiva
Fibrodysplasia ossificans progressiva is also called stone man syndrome, is a disorder in which muscle tissue and connective tissue such as tendons and ligaments are gradually replaced by bone (ossified), forming bone outside the skeleton (extra-skeletal or heterotopic bone) that constrains movement. This process generally becomes noticeable in early childhood, starting with the neck and shoulders and proceeding down the body and into the limbs. Fibrodysplasia ossificans progressiva has an extremely variable and episodic course and can be induced by trauma, infections, iatrogenic harms, immunization or can occur in an unpredictable way, without any recognizable trigger 1.
Extra-skeletal bone formation causes progressive loss of mobility as the joints become affected. Inability to fully open the mouth may cause difficulty in speaking and eating. Over time, people with this disorder may experience malnutrition due to their eating problems. They may also have breathing difficulties as a result of extra bone formation around the rib cage that restricts expansion of the lungs.
Any trauma to the muscles of an individual with fibrodysplasia ossificans progressiva, such as a fall or invasive medical procedures, may trigger episodes of muscle swelling and inflammation (myositis) followed by more rapid ossification in the injured area. Flare-ups may also be caused by viral illnesses such as influenza.
People with fibrodysplasia ossificans progressiva are generally born with malformed big toes. This abnormality of the big toes is a characteristic feature that helps to distinguish this disorder from other bone and muscle problems. Affected individuals may also have short thumbs and other skeletal abnormalities.
Fibrodysplasia ossificans progressiva is a very rare disorder, believed to occur in approximately 1 in 2 million people worldwide. Several hundred cases have been reported.
Fibrodysplasia ossificans progressiva key facts:
- Genetic disease affecting 1 in 2 million people
- No ethnic, racial, or gender patterns
- 800 confirmed cases across the globe
- 285 known cases in the United States
- Malformation of the great toes is visible at birth
- Flare-ups that worsen the connection occur spontaneously or following physical trauma such as: childhood immunizations, falls, surgery, biopsy or viral illnesses
- Fibrodysplasia ossificans progressiva is accelerated by trauma (including intra muscular injections), but venipuncture, subcutaneous and intravenous meds are okay
- Rogue bone growth progressively restricts movement
- Often misdiagnosed as cancer
- The exact rate of progression is unpredictable, although there appears to be a pattern to the progression (e.g., upper body in childhood and lower body in adolescence)
- No treatment exists, but four clinical trials are currently underway
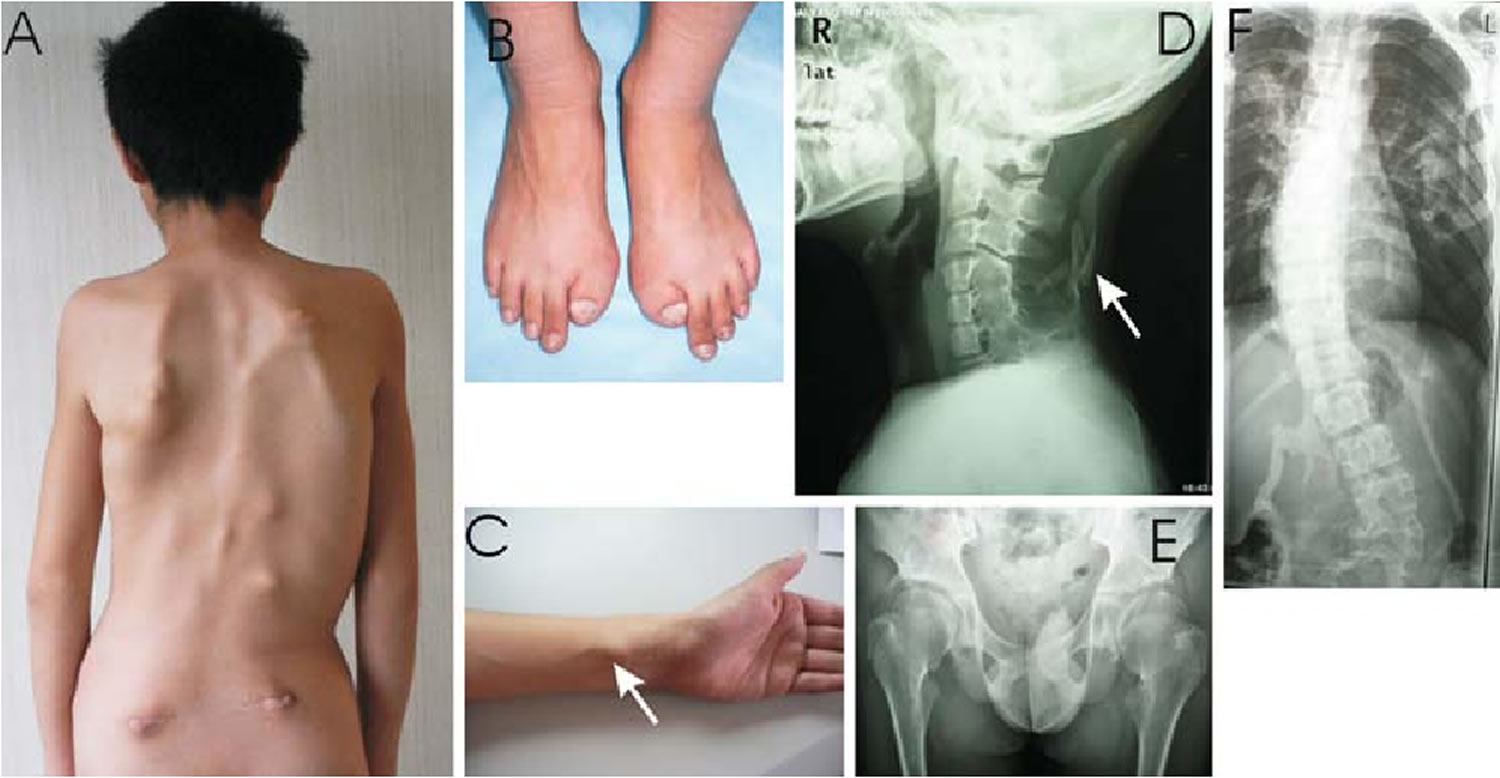
Figure 1. Fibrodysplasia ossificans progressiva
Footnote: (A) Typical heterotopic ossification of the dorsal and lumbar paravertebral muscles. (B) Symmetrical great toe malformations. (C) The arrow indicates an ossified lesion on the left forearm following a carpal fracture at the age of 17 years. (D) X-ray evidence of ossified soft tissue in its
[Source 2 ]Figure 2. Fibrodysplasia ossificans progressiva big toes
Is there cure for fibrodysplasia ossificans progressiva?
At this time, there is no cure nor treatment for fibrodysplasia ossificans progressiva. For now, medication is only helpful to manage the symptoms of fibrodysplasia ossificans progressiva (pain, inflammation, etc.)
How is the extra bone in fibrodysplasia ossificans progressiva different from normal bone?
The extra bone in fibrodysplasia ossificans progressiva forms by a progressive transformation of soft tissue into cartilage and bone. This is the same process by which bone regenerates (heals) after a fracture (break) occurs and is nearly identical to the process by which bone forms normally in an embryo. The abnormality in fibrodysplasia ossificans progressiva occurs not in the manner of bone formation but rather in its timing and location.
What is a flare-up and is it painful?
A flare-up occurs when the body starts to generate new bone. No one knows what initiates this process, but once it begins, it leads to tissue swelling and much discomfort. Sometimes the individual will not feel well and may develop a low-grade fever. While there is no medication or therapy that can stop the process of bone formation once it has begun, a physician can prescribe medicine to help relieve the pain. A single flare-up may continue for as long as 6-8 weeks. Multiple flare-ups may also occur during an active period of fibrodysplasia ossificans progressiva. When a flare-up is in progress, joint stiffness may occur overnight. The stiffness comes from swelling and pressure inside the muscle during the earliest stages of new bone formation. While flare-ups are usually painful, the degree of pain can vary. Most people find that the pain subsides when a flare-up is over; it appears that it is the process of extra bone formation, rather than the extra bone itself, that usually leads to pain.
What parts of the body are involved in fibrodysplasia ossificans progressiva?
Fibrodysplasia ossificans progressiva affects the neck, spine, chest, shoulders, elbows, wrists, hips, knees, ankles, jaw, and many areas in between. The progression of ossification follows a characteristic pattern. Usually extra bone forms in the neck, spine, and shoulders before developing in the elbows, hips and knees. The muscles of the diaphragm, tongue, eyes, face, and heart are characteristically spared. The well-documented and characteristic progression of fibrodysplasia ossificans progressiva, as well as the regions not affected, likely hold important clues to the cause and development of the disease.
Fibrodysplasia ossificans progressiva affects mobility because the body’s joints, such as the knees or the elbows, connect the bones and aid in movement. In fibrodysplasia ossificans progressiva, extra bone replaces the ligaments (which cover the joints), as well as muscles and tendons (which move the joints). Consequently, movement in areas affected by fibrodysplasia ossificans progressiva becomes difficult or impossible.
What physical variations are seen from person to person?
The largest variation seen is the timing and rate of extra bone formation. Another common variation includes the severity of movement restriction. For example, an elbow could be fixed in a closed position, putting the hand permanently across the chest, or the elbow may be left with some range of motion.
How does fibrodysplasia ossificans progressiva affect a child’s school life?
Fibrodysplasia ossificans progressiva does not affect a person’s intelligence or cognitive abilities. It does, however, negatively impact the child’s ability to safely access the school premises, use and manipulate the school’s materials, and function academically in a typical way.
Fibrodysplasia ossificans progressiva causes
Mutations in the ACVR1 (activin A receptor type 1) gene cause fibrodysplasia ossificans progressiva 3. The ACVR1 gene provides instructions for producing a member of a protein family called bone morphogenetic protein (BMP) type 1 receptors. The ACVR1 protein is found in many tissues of the body including skeletal muscle and cartilage. It helps to control the growth and development of the bones and muscles, including the gradual replacement of cartilage by bone (ossification) that occurs in normal skeletal maturation from birth to young adulthood.
Researchers believe that a mutation in the ACVR1 gene may change the shape of the receptor under certain conditions and disrupt mechanisms that control the receptor’s activity. As a result, the receptor may be constantly turned on (constitutive activation). Constitutive activation of the receptor causes overgrowth of bone and cartilage and fusion of joints, resulting in the signs and symptoms of fibrodysplasia ossificans progressiva.
Fibrodysplasia ossificans progressiva inheritance pattern
Fibrodysplasia ossificans progressiva is inherited in an autosomal dominant pattern, which means one copy of the altered gene in each cell is sufficient to cause the disorder. However, most cases of fibrodysplasia ossificans progressiva result from new mutations in the gene. These cases occur in people with no history of the disorder in their family. In a small number of cases, an affected person has inherited the mutation from one affected parent. When one parent has the abnormal gene, they will pass on either their normal gene or their abnormal gene to their child. Each of their children therefore has a 50% (1 in 2) chance of inheriting the changed gene and being affected by the condition.
Figure 3. Fibrodysplasia ossificans progressiva autosomal dominant inheritance pattern
Fibrodysplasia ossificans progressiva symptoms
Fibrodysplasia ossificans progressiva is characterized by the gradual replacement of muscle tissue and connective tissue (such as tendons and ligaments) by bone, restricting movement. This process generally becomes noticeable in early childhood, starting with the neck and shoulders and proceeding down the body and into the limbs.
Individuals with fibrodysplasia ossificans progressiva appear normal at birth except for characteristic malformed big toes, which are present in all classically affected individuals 4. This abnormality of the big toes is a characteristic feature that helps to distinguish this disorder from other bone and muscle problems. Affected individuals may also have short thumbs and other skeletal abnormalities.
The formation of extra-skeletal bone causes progressive loss of mobility as the joints become affected. Speaking and eating may also become difficult as the mouth becomes affected. Over time, people with fibrodysplasia ossificans progressiva may become malnourished because of the inability to eat. They may also develop breathing difficulties as a result of extra bone formation around the rib cage that restricts expansion of the lungs.
Malformed big toes are present at birth:
- Short, bent, and sometimes curved inward
- Important early sign of fibrodysplasia ossificans progressiva before the onset of extra bone
Swellings that look like tumors:
- Sometimes red, painful and hot to the touch
- Typically in the shoulder and back areas and sometimes on the scalp or head
- Swellings eventually clear up, but leave behind a new piece of mature bone
Bone formation in muscle, ligaments and connective tissue:
- Stiffness, locking and permanent immobility
- Usually begins during the first two decades of life
- Instead of crawling, toddlers scoot on their buttocks due to facet joints on the back of the neck not forming properly or fusing together
Minor trauma (e.g., intramuscular immunizations; mandibular blocks for dental work; muscle fatigue; blunt muscle trauma from bumps, bruises, falls) or influenza-like viral illnesses may trigger episodes of muscle swelling and inflammation followed by more rapid heterotopic ossification in the injured area
Episodic, painful soft tissue swellings or exacerbations usually develop in the preteen years 5.
Although some exacerbations spontaneously regress, most transform soft connective tissues (including aponeuroses, fascia, ligaments, tendons, and skeletal muscles) into mature bone.
Most patients with fibrodysplasia ossificans progressiva are confined to a wheelchair by the third decade of life and require lifelong assistance in performing activities of daily living.
The severe disability of fibrodysplasia ossificans progressiva results in low reproductive fitness.
Two clinical features define classic fibrodysplasia ossificans progressiva
Malformations of the great toes and progressive heterotopic endochondral ossification in characteristic anatomic patterns. Individuals with fibrodysplasia ossificans progressiva appear normal at birth except for malformations of the great toes that are present in all classically affected individuals. During the first decade of life, most children with fibrodysplasia ossificans progressiva develop episodic, painful inflammatory soft tissue swellings (or flare-ups). While some flare-ups regress spontaneously, most transform soft connective tissues including aponeuroses, fascia, ligaments, tendons, and skeletal muscles into mature heterotopic bone. Ribbons, sheets, and plates of heterotopic bone replace skeletal muscles and connective tissues through a process of endochondral ossification that leads to an armament-like encasement of bone and permanent immobility. Minor trauma such as intramuscular immunizations, mandibular blocks for dental work, muscle fatigue, blunt muscle trauma from bumps, bruises, falls, or influenza-like viral illnesses can trigger painful new flare-ups of fibrodysplasia ossificans progressiva leading to progressive heterotopic ossification 6. Surgical removal of heterotopic bone provokes explosive and painful new bone growth.
Heterotopic endochondral ossification in fibrodysplasia ossificans progressiva progresses in characteristic anatomic and temporal patterns that mimic the patterns of normal embryonic skeletal formation. Heterotopic ossification typically occurs first in the dorsal, axial, cranial, and proximal regions of the body and later seen in the ventral, appendicular, caudal, and distal regions 7. Several skeletal muscles including the diaphragm, tongue, and extra-ocular muscles are spared from fibrodysplasia ossificans progressiva. Cardiac muscle and smooth muscle are not involved.
Heterotopic endochondral ossification in fibrodysplasia ossificans progressiva is episodic, but disability is cumulative 8. Most patients with fibrodysplasia ossificans progressiva are confined to a wheelchair by the third decade of life, and require lifelong assistance in performing activities of daily living. Severe weight loss may result following ankylosis of the jaw. Pneumonia or right-sided heart failure may complicate rigid fixation of the chest wall. The median age of survival is approximately 40 years, and death often results from complications of thoracic insufficiency syndrome 9.
Anomalies of the normotopic skeleton in fibrodysplasia ossificans progressiva
While malformation of the great toes is characteristic of fibrodysplasia ossificans progressiva, other developmental anomalies are frequently observed, particularly in the thumbs and cervical spine. Stiffness of the neck is an early finding in most patients and can precede the appearance of heterotopic endochondral ossification at that site. Crawling is often limited due to lack of neck extension. Characteristic anomalies of the cervical spine include large posterior elements, tall narrow vertebral bodies, and fusion of the facet joints between C2 and C7. Although the cervical spine often becomes ankylosed early in life, any minimal residual movement may eventually result in painful arthritic symptoms 10.
Other skeletal anomalies associated with fibrodysplasia ossificans progressiva include short malformed thumbs, clinodactyly, short broad femoral necks, and proximal medial tibial osteochondromas 11.
Fibrodysplasia ossificans progressiva diagnosis
Due to a lack of knowledge of fibrodysplasia ossificans progressiva among doctors, the rate of misdiagnosis of the disease is estimated at 80 percent or higher. These errors in diagnosing fibrodysplasia ossificans progressiva have caused pain and suffering for fibrodysplasia ossificans progressiva patients and their families worldwide. For instance, misdiagnosis has led to unnecessary invasive procedures, such as biopsies, as well as permanent complications from medical interventions, including loss of mobility.
Three of the most common misdiagnoses for fibrodysplasia ossificans progressiva are cancer, aggressive juvenile fibromatosis, also called desmoid tumors, and progressive osseous heteroplasia, another rare disease characterized by the abnormal growth of bone.
Definitive genetic testing of fibrodysplasia ossificans progressiva is now available 12. Clinical suspicion of fibrodysplasia ossificans progressiva early in life on the basis of malformed great toes can lead to early clinical diagnosis, confirmatory diagnostic genetic testing (if appropriate), and the avoidance of harmful diagnostic and treatment procedures 13. At the present time, genetic testing is available on a clinical and research basis at several laboratories.
In most cases, an accurate diagnosis of fibrodysplasia ossificans progressiva can be made based on a patient’s characteristic malformation of the big toe, in addition to rapidly changing swellings on the head, neck or back.
Fibrodysplasia ossificans progressiva prognosis
Unfortunately, fibrodysplasia ossificans progressiva does not improve over time. The “P” in fibrodysplasia ossificans progressiva stands for “progressiva.” That means that fibrodysplasia ossificans progressiva will progress, or get worse, as a person ages. As fibrodysplasia ossificans progressiva is part of a person’s genetic make-up, people with fibrodysplasia ossificans progressiva are born with the condition, even though the extra bone may not have appeared at birth. So people with fibrodysplasia ossificans progressiva will not outgrow the condition. Nor can the extra bone that has been produced by fibrodysplasia ossificans progressiva disappear. The body of a person with fibrodysplasia ossificans progressiva does not make extra bone all of the time; a person with fibrodysplasia ossificans progressiva may go months or years without a flare-up. Yet there is always a chance that extra bone can form, either without any warning (“spontaneous flare-up”) or following trauma, such as a bump, fall, muscle overexertion, an injury, intramuscular injections, surgery, or even some viruses. It is unclear why the disease is active some times and quiet or dormant at other times.
As heterotopic bone accumulates in fibrodysplasia ossificans progressiva, range of motion is progressively lost, leading to near complete immobility. Most patients with fibrodysplasia ossificans progressiva are confined to a wheelchair by the third decade of life, and require lifelong assistance in performing activities of daily living. Severe weight loss may result following ankylosis of the jaw.
Patients with fibrodysplasia ossificans progressiva develop thoracic insufficiency syndrome that can lead to life-threatening complications. Pneumonia and right-sided heart failure are the major life-threatening hazards that result from thoracic insufficiency syndrome in patients with fibrodysplasia ossificans progressiva.
Fibrodysplasia ossificans progressiva life expectancy
The median age of survival is approximately 40 years, and death often results from complications of thoracic insufficiency syndrome 9.
Fibrodysplasia ossificans progressiva treatment
There is currently no definitive treatment. However, a brief course of high-dose corticosteroids, such as Prednisone, started within the first 24 hours of a flare-up, may help reduce the intense inflammation and tissue swelling seen in the early stages of fibrodysplasia ossificans progressiva. Other medications, such as muscle relaxants, mast cell inhibitors, and aminobisphosphonates, if appropriate, should be closely monitored by a physician. Surgery to remove heterotopic and extra-skeletal bone is risky and can potentially cause painful new bone growth 14.
Flare-ups
Widespread favorable anecdotal reports from the fibrodysplasia ossificans progressiva community suggest that a brief 4-day course of high-dose corticosteroids, started within the first 24 hours of a flare-up, may help reduce the intense inflammation and tissue edema seen in the early stages of the disease. The use of corticosteroids should be restricted to the extremely early symptomatic treatment of flare-ups that affect major joints, the jaw, or the submandibular area. Corticosteroids should not generally be used for the symptomatic treatment of flare-ups that involve the back, neck, or trunk due to the long duration and recurring nature of these flare-ups and the difficulty in assessing the true onset of such flare-ups.
The dose of corticosteroids depends on body weight. A typical dose of prednisone is 2 mg/kg/d, administered as a single daily dose for no more than 4 days. The potentially dangerous nature of flare-ups in the submandibular region may dictate a slightly longer use of corticosteroids with an appropriate taper for the duration of the flare-up or until the acute swelling subsides.
When prednisone is discontinued, a nonsteroidal anti-inflammatory drug (NSAID) or cox-2 inhibitor (in conjunction with a leukotriene inhibitor) may be used symptomatically for the duration of the flare-up.
The use of mast cell inhibitors and aminobisphosphonates are less well-defined and should be used at the physician’s discretion.
Pain management
Many fibrodysplasia ossificans progressiva flare-ups, especially those around the hips and knees, are extremely painful and may require a brief course of well-monitored narcotic analgesia in addition to the use of NSAIDs, cox-2 inhibitors, and oral or intravenous glucocorticoids. Other types of transient pain syndromes may be caused by neuropathies resulting from acute flare-ups, transient bursitis, inflammation of osteochondromas, arthritis, and muscle fatigue.
Muscle relaxants
Areas of relatively healthy skeletal muscle bordering the acute fibrodysplasia ossificans progressiva lesion are subject to metabolic changes that lead to muscle spasm and fiber shortening. The judicious short-term use of muscle relaxants such as cyclobenzaprine (Flexeril), metaxalone (Skelaxin), or Lioresal (Baclofen) may help to decrease muscle spasm and maintain more functional activity.
Surgical care
Attempts to surgically remove heterotopic bone risks provoking explosive and painful new bone growth. Biopsies of fibrodysplasia ossificans progressiva lesions are never indicated and may cause additional heterotopic ossification.
Activity
Falls suffered by patients with fibrodysplasia ossificans progressiva can lead to severe injuries and flare-ups. Patients with fibrodysplasia ossificans progressiva have a self-perpetuating fall cycle. Minor soft tissue trauma often leads to severe exacerbations of fibrodysplasia ossificans progressiva, which result in heterotopic ossification and joint ankylosis. Mobility restriction from joint ankylosis severely impairs balancing mechanisms and causes instability, resulting in more falls. Compared with people who do not have fibrodysplasia ossificans progressiva, falls in those with fibrodysplasia ossificans progressiva are more likely to result in severe head injuries, loss of consciousness, concussions, and neck and back injuries due to the inability to use the upper limbs to absorb the impact of a fall and to anatomic abnormalities of the cervical spine in individuals with fibrodysplasia ossificans progressiva.
For children, redirection of activity to less physically interactive play may be helpful. Complete avoidance of high-risk circumstances may reduce falls but may also compromise a patient’s functional level and independence and may be unacceptable to many.
Can the extra bone be removed?
No, new bone will grow back and further impair mobility. Surgical intervention often results in a worsening of the condition.
References- Cappato S, Giacopelli F, Ravazzolo R, Bocciardi R. The Horizon of a Therapy for Rare Genetic Diseases: A “Druggable” Future for Fibrodysplasia Ossificans Progressiva. Int J Mol Sci. 2018;19(4):989. Published 2018 Mar 26. doi:10.3390/ijms19040989 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5979309
- Sun, Y., Xia, W., Jiang, Y., Xing, X., Li, M., Wang, O., Zhang, H., Hu, Y., Liu, H., Meng, X., & Zhou, X. (2009). A Recurrent Mutation c.617G>A in the ACVR1 Gene Causes Fibrodysplasia Ossificans Progressiva in Two Chinese Patients. Calcified Tissue International, 84, 361-365.
- Fibrodysplasia ossificans progressiva. https://ghr.nlm.nih.gov/condition/fibrodysplasia-ossificans-progressiva
- Sferopoulos NK, Kotakidou R, Petropoulos AS. Myositis ossificans in children: a review. Eur J Orthop Surg Traumatol. 2017 May. 27 (4):491-502.
- Rocke DM, Zasloff M, Peeper J, Cohen RB, Kaplan FS. Age- and joint-specific risk of initial heterotopic ossification in patients who have fibrodysplasia ossificans progressiva. Clin Orthop Relat Res. 1994 Apr. 243-8
- Kaplan FS, Le Merrer M, Glaser DL, Pignolo RJ, Goldsby RE, Kitterman JA, Groppe J, Shore EM. Fibrodysplasia ossificans progressiva. Best Pract Res Clin Rheumatol. 2008;22:191–205.
- Cohen RB, Hahn GV, Tabas JA, Peeper J, Levitz CL, Sando A, Sando N, Zasloff M, Kaplan FS. The natural history of heterotopic ossification in patients who have fibrodysplasia ossificans progressiva. A study of forty-four patients. J Bone Joint Surg Am. 1993;75:215–219
- Rocke DM, Zasloff M, Peeper J, Cohen RB, Kaplan FS. Age- and joint-specific risk of initial heterotopic ossification in patients who have fibrodysplasia ossificans progressiva. Clin Orthop Relat Res. 1994:243–248.
- Kaplan FS, Glaser DL. Thoracic insufficiency syndrome in patients with fibrodysplasia ossificans progressiva. Clin Rev Bone Miner Metab. 2005;3:213–216.
- Schaffer AA, Kaplan FS, Tracy MR, O’Brien ML, Dormans JP, Shore EM, Harland RM, Kusumi K. Developmental anomalies of the cervical spine in patients with fibrodysplasia ossificans progressiva are distinctly different from those in patients with Klippel-Feil syndrome: clues from the BMP signaling pathway. Spine. 2005;30:1379–1385
- Kaplan FS, Xu M, Seemann P, Connor JM, Glaser DL, Carroll L, Delai P, Fastnacht-Urban E, Forman SJ, Gillessen-Kaesbach G, Hoover-Fong J, Koster B, Pauli RM, Reardon W, Zaidi SA, Zasloff M, Morhart R, Mundlos S, Groppe J, Shore EM. Classic and atypical fibrodysplasia ossificans progressiva (FOP) phenotypes are caused by mutations in the bone morphogenetic protein (BMP) type I receptor ACVR1. Hum Mutat. 2009;30:379–390.
- Kaplan FS, Xu M, Glaser DL, et al. Early diagnosis of fibrodysplasia ossificans progressiva. Pediatrics. 2008 May. 121(5):e1295-300.
- Kitterman JA, Kantanie S, Rocke DM, Kaplan FS. Iatrogenic harm caused by diagnostic errors in fibrodysplasia ossificans progressiva. Pediatrics. 2005 Nov. 116(5):e654-61.
- Pediatric Fibrodysplasia Ossificans Progressiva (Myositis Ossificans). https://emedicine.medscape.com/article/1007104-overview