Flail chest
Flail chest is defined as two or more contiguous rib fractures with two or more breaks per rib with paradoxical chest wall movement 1. A flail chest arises when these injuries cause a segment of the chest wall to move independently of the rest of the chest wall. A flail chest can create a significant disturbance to respiratory physiology 2. Flail chest is considered a clinical diagnosis as everybody with this fracture pattern does not develop a flail chest. Flail chest is one of the most serious of chest injuries and is often associated with considerable morbidity and mortality (18.7%) in both young and old trauma victims due to the associated complications of acute respiratory distress syndrome, pneumonia and hemorrhage 3. Flail chest in particular has a high mortality rate as chest wall disruption causes an increase in the work of breathing for patients who are often in significant pain 4. Flail chest occurs when a portion of the chest wall is destabilized, usually from severe blunt force trauma. This alters the mechanics of breathing so that the floating segment of chest wall and soft tissue moves paradoxically in the opposite direction from the rest of the rib cage. Until recently, ribs fractures were allowed to heal on their own or treated with continuous positive pressure ventilation 5. Now, surgical stabilization of fractured ribs is becoming more widely accepted, especially for flail chest. Surgical fixation is thought to be beneficial to patients with respiratory failure 6, intractable pain 7 or if failing to wean from invasive ventilation secondary to chest trauma 8. Fixation has potential to restore chest wall biomechanics and reduce the complications associated with poor ventilation and secretion clearance 9.
The American Association for the Surgery of Trauma gives trauma statistics for the US. 1% of the US population/year will experience a significant traumatic event. Chest trauma occurs in 20% of major trauma and is responsible for 25% of traumatic deaths. Flail chest occurs in about 7% of chest trauma 10. Flail chest patients usually require hospitalization. Flail chest occurs in isolation in less than 40% of cases. More often it is accompanied by pulmonary contusions, hemo/pneumotharax, head injury and occasionally major vascular injury. The mortality of flail chest ranges from 10% to 20% but is often due to accompanying injury rather than the flail chest alone 11. Morbidity is high due to long and complicated hospital stays and recovery.
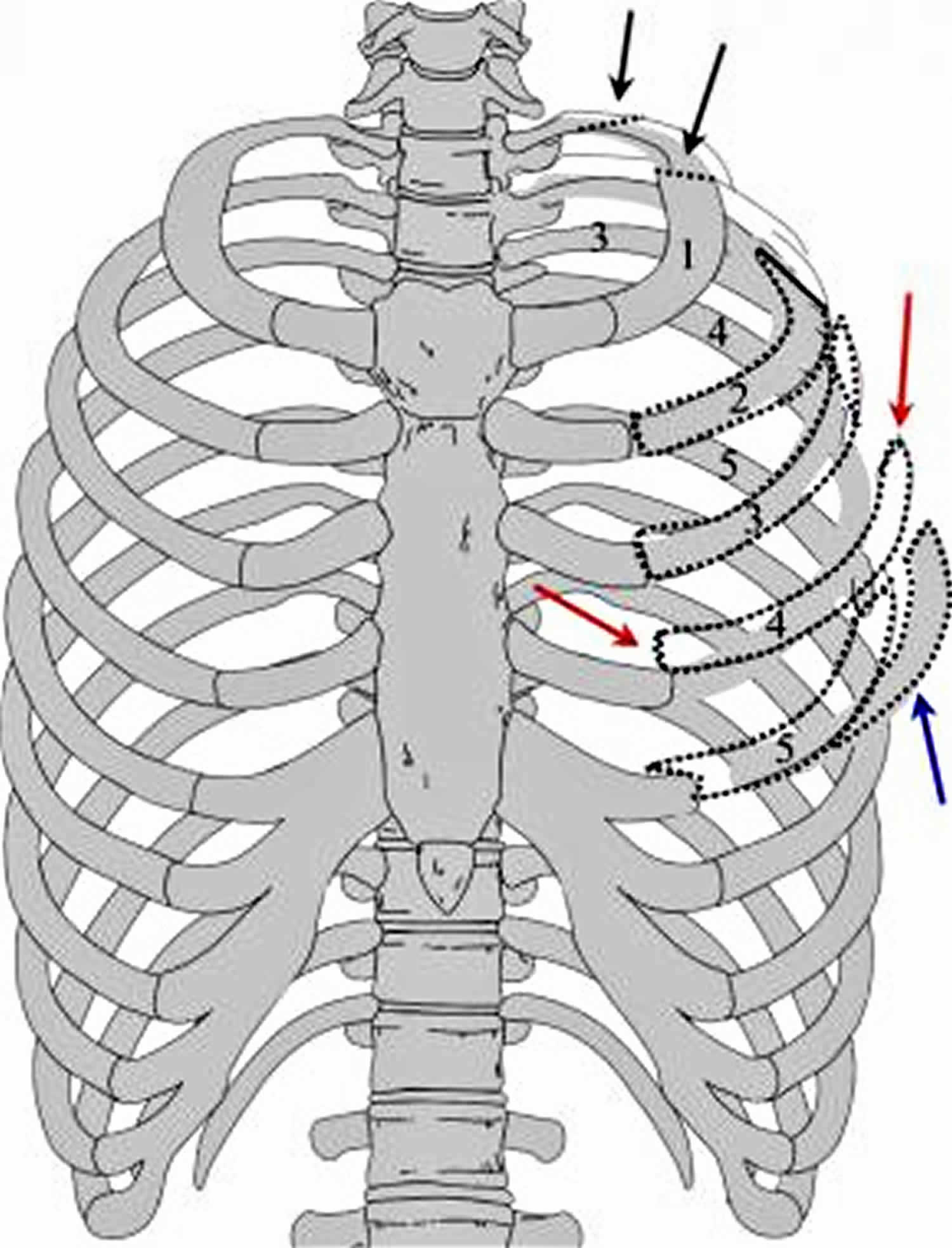
Figure 1. Flail chest anatomy
Footnote: Image depicting multiple fractures of the left upper chest wall. The first rib is often fractured posteriorly (black arrows). If multiple rib fractures occur along the midlateral (red arrows) or anterior chest wall (blue arrows), a flail chest (dotted black lines) may result.
Flail chest causes
Flail chest requires significant blunt force trauma to the trunk to fracture the ribs in multiple areas. Such trauma may be caused by motor vehicle accidents, falls, and assaults in younger, healthy patients. Flail chest is an indicator of significant kinetic force to the chest wall and rib cage, but it may also may occur with lesser trauma in persons with underlying pathology, including osteoporosis, total sternectomy, and multiple myeloma, as well as individuals with congenital absence of the sternum.
Because flail chest is a traumatic disorder, risk factors for flail chest include the risk factors for major trauma. Male sex and intoxication being independent risk factors. Motor vehicle collisions are the cause of 75% of the major trauma which result in flail chest. Falls particularly in the elderly cause another 15% 12. Certain traumatic events like direct blows to the chest are more likely to cause 2 fractures on a given rib. Rollover and crush injuries more commonly break ribs at only one point and thus do not, as often, cause flail chest. In childhood metabolic bone disease and osteogenesis imperfecta predispose to this condition. The elderly are predisposed to flail chest both because they have an age-related physiologic stiffening of the chest wall and because they may have osteoporosis. Because they are also more likely to have pre-existing lung disease they are also at highest risk for the complications of flail chest.
Flail chest pathophysiology
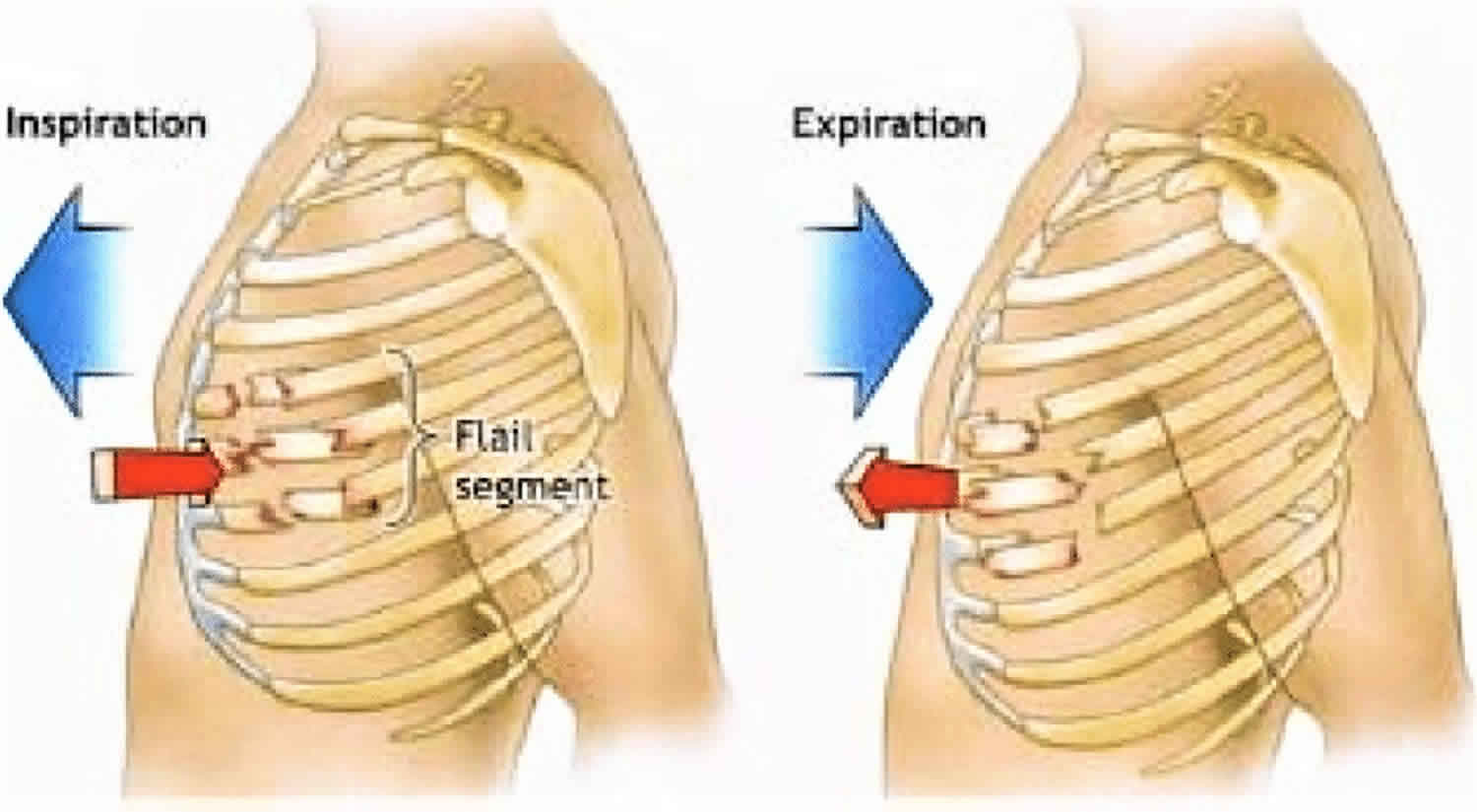
The movement of air in and out of the lungs is dependent on changes in intrathoracic pressure. Inspiration relies on the coordinated function of respiratory muscle groups including the diaphragm, external intercostal, parasternal internal intercostal and accessory muscles. The descent of the diaphragmatic dome increases in the vertical dimension of the chest cavity and creates negative pressure. The diaphragm alone can maintain adequate ventilation at rest. The intercostals play an increasingly important role to inspiration during exercise and in pathologic states. Exhalation is usually passive due to the elastic recoil of the lung, but the abdominal muscles and the intercostals may participate. With a flail chest, the continuity of the chest wall is disrupted, and the physiologic action of the ribs is altered. The motion of the flail segment is paradoxical to the rest of the chest. It is paradoxical because the flail segment moves inward while the rest of the chest wall moves outward. The severity of this paradoxical motion and the physiological effect is determined by a three factors; pleural pressure, the extent of the flail, and the activation of intercostals muscles during inspiration 13.
A flail segment of the chest wall will negatively affect respiration in three ways: ineffective ventilation, pulmonary contusion and hypoventilation with atelectasis. There is ineffective ventilation because of increased dead space, decreased intrathoracic pressure and increased oxygen demand from injured tissue. Pulmonary contusion in adjacent lung tissue is almost universal with flail chest. Pulmonary contusion lead to edema, hemorrhage and may eventually have some element of necrosis. Pulmonary contusions impairs gas exchange and decreases compliance. Hypoventilation and atelectasis result from the pain of the injury. The pain causes splinting which decreases the tidal volume and predisposes to the formation of atelectasis.
Flail chest signs and symptoms
Flail chest is a clinical anatomic diagnosis noted in blunt trauma patients with paradoxical or reverse motion of a chest wall segment while spontaneously breathing. This clinical finding disappears after intubation with positive pressure ventilation, which occasionally results in a delayed diagnosis of the condition.
The strict definition of 3 ribs broken in 2 or more places can be confirmed only by x-ray, but the inherent structural stability of the chest wall due to the ribs and intercostal muscles usually does not show abnormal or paradoxical motion without 3 or more ribs involved. Patients may demonstrate only the paradoxical chest wall motion, and they may have minimal to incapacitating respiratory insufficiency, although these individuals usually show some tachypnea with a notable decrease in resting tidal volume due to fracture pain. The degree of respiratory insufficiency is typically related to the underlying lung injury, rather than the chest wall abnormality.
Flail chest complications
Reports in the medical literature note a high level of long-term disability in patients sustaining flail chest. Beal and Oreskovich reported a 22% disability rate with over 63% having long-term problems, including persistent chest wall pain, deformity, and dyspnea on exertion 14. Kishikawa et al 15, however, noted resolution of altered pulmonary function within 6 months, even with chest wall deformity still present.
Flail chest diagnosis
Evaluation of the trauma patient should include all of the usual exams and studies used in a major multi-trauma patient.
The physical exam should be the exam performed in all patients with potential thoracic trauma. Fully expose the patient. Obtain a full set of vitals including an accurate measure of respiratory rate and oxygen saturation. Start with the ABC’s and continue through the secondary survey. Always listen for bilateral breath sounds then palpate for pain, deformity or crepitus. Examine the chest for bruising or bleeding, seatbelt signs. The patient usually complains of severe chest wall pain and may have tachypnea and splinting or manifest respiratory insufficiency.
Specifically, observe the chest for paradoxical wall motion. In inspiration the flail segment will go in while the rest of the chest expands and in expiration the flail segment will be pushed out while the rest of the chest contracts. Of note the absence of observable paradoxical motion does not exclude this disease and it may become more apparent as the intercostals become fatigued.
Because of the pressure changes with positive pressure ventilation, patients on bipap or those who are mechanically intubated do not exhibit paradoxical chest wall motion. Thus, in mechanically ventilated trauma patient, the diagnosis of flail chest may be delayed and become apparent only after extubation 12.
The chest x-ray may be the first study that helps specifically with flail chest. Chest x-ray is not very sensitive and may miss rib fractures identified by CT; hence the diagnosis of flail chest may be missed if one just relies on the chest x-ray. A rib series is better but may still miss ¼ of the rib fractures 16. The test of choice for evaluating not only the flail chest but also for associated injury is the CT scan, specifically with 3D reconstruction. Finding 3 ribs broken in 2 places on x-ray or CT is suggestive of flail chest but need to be clinically correlated. Findings on chest CT may also help decide on treatment.
Complete trauma labs should be ordered including a blood gas. Labs have limited direct role in the diagnosis of flail chest but may aid in monitoring the patient for signs of impending respiratory failure.
Flail chest treatment
Management of a flail chest should include these areas of concern; maintaining adequate ventilation, fluid management, pain management and management of the unstable chest wall. Ventilation should be maintained with oxygen and non-invasive ventilation when possible. Invasive mechanical ventilation used only when other methods fail and extubation should be attempted as early as possible.
The judicious use of fluid is recommended in most trauma settings and is important in flail chest because of the almost ubiquitous lung contusion.
Pain management should be addressed early and aggressively. This may include nerve blocks or epidural anesthesia. There should also be a focus on excellent pulmonary toilet and steroids should be avoided 17.
Internal pneumatic stabilization has been used successfully to treat complicated cases 18. Two recent clinical reports, one from Turkey (prospective) 19 and one from Japan (retrospective) 20, showed that continuous positive airway pressure (CPAP) by mask may decrease mortality and nosocomial pneumonia in the ICU, but CPAP by mask does not appear to change the length of ICU stay.
Surgical stabilization may be considered in patients who are getting a thoracotomy for other reasons, in those who fail to wean off a ventilator and in those whose respiratory status continues to decline despite other treatments.
Surgical stabilization of the chest was rarely considered necessary in the past, but increasing numbers of reports of positive outcomes in more severe cases are now available in the world literature. Both external (lower efficacy) and internal stabilization have been advocated, usually in reports from outside the United States. As previously noted in traumatic causes, however, severity of respiratory failure is less a result of either the paradoxical motion of the chest wall (tidal volume abnormalities) or chest wall instability. Accordingly, surgical stabilization is still not routinely performed, although many reports show a benefit in decreasing mechanical ventilator days, long-term outcome, and overall lower cost of hospitalization in select patients with severe flail chest 21.
In general, operative fixation is most commonly performed in patients requiring a thoracotomy for other reasons or in cases of gross chest wall deformity. Flail chest from multiple myeloma, sternal absence, or total sternectomy more frequently responds well to surgical fixation. Underlying pulmonary injury with respiratory insufficiency resulting from changes in tidal volume and minute ventilation in these patients is rare.
A 2015 Cochrane Review 22 evaluated the effectiveness and safety of surgical stabilization compared with clinical management for people with flail chest. The study found some evidence from three small studies that showed surgical treatment was preferable to nonsurgical management in reducing pneumonia, chest deformity, tracheostomy, duration of mechanical ventilation, and length of ICU stay. Further studies are needed to confirm these results 22.
In a retrospective study involving 21 patients with flail chest who were admitted to a level I trauma center between September 2009 and June 2010, Doben et al 23 examined the effectiveness of surgical rib fixation for patients in whom standard therapy had failed. Standard therapy consisted of pain control, aggressive pulmonary hygiene, positive pressure therapy with an acapella device, and frequent chest therapy (chest wall percussion, deep breathing, and coughing exercises). The surgical rib fixation surgeries were performed via a standard anterolateral or posterolateral muscle-sparing thoracotomy incision; ribs were reduced and internally fixated through use of osteosyntheses plates and intramedullary nails. Surgical rib fixation resulted in a significant decrease in ventilator days (4.5 vs 16.0), and the authors concluded that the technique may represent a means to decrease morbidity in patients with flail chest whose pulmonary status is declining 23.
In a retrospective meta-analysis that included 11 studies with a total of 753 patients with flail chest, Slobogean et al 24 compared the results of surgical fixation with those of nonoperative treatment. Surgical fixation resulted in better outcomes for all pooled analyses, including substantial decreases in ventilator days (mean, 8 days) and the odds of developing pneumonia (odds ratio 0.2). Additional benefits included decreased ICU days (mean, 5 days), mortality (odds ratio 0.31), septicemia (odds ratio 0.36), tracheostomy (odds ratio 0.06), and chest deformity (odds ratio 0.11). The authors concluded that surgical fixation offers substantial clinical benefits over nonopoerative treatment 24.
Flail chest prognosis
Overall, patients with flail chest have a 5-10% reported mortality if they reach the hospital alive. Patients who do not need mechanical ventilation do better statistically, and overall mortality seems to increase with increasing injury severity scores, age, and number of total rib fractures.
Few long-term follow-up studies regarding flail chest are available. In the absence of concomitant lethal injuries, Freedland et al 25 reported adverse outcomes to be more likely with more severe associated injuries noted by injury severity scores scoring, excessive blood loss and transfusion requirements, bilateral flail chest, and patient age older than 50 years. A report by Albaugh and associates in New Jersey 26 noted flail chest mortality increased 132% with each decade of life, but another report by Athanassiadi and associates 27 found no correlation with age. Both studies noted increasing mortality with increasing injury severity scores. As previously noted, some reports suggest a high rate of disability after flail chest; however, most patients do well and return to normal function after 6-12 months.
Dehghan et al 28 conducted a retrospective analysis of data from the National Trauma Data Bank of injury patterns, management, and clinical outcomes for 3,467 patients in whom flail chest was identified from 2007 to 2009. The mean age of the patients was 52 years; 77.5% were male. Treatment practices included use of epidural catheters (8%); surgical fixation of the chest wall (0.7%); and mechanical ventilation (59%). Complications included pneumonia (21%); adult respiratory distress syndrome (14%); sepsis (7%); and death (16%). More than 99% of patients were treated nonoperatively, and a small proportion (8%) received aggressive pain management with epidural catheters. The authors concluded that alternative methods of treatment, including more consistent use of epidural catheters for pain and surgical fixation, should be investigated 28.
References- Ingoe HM, Coleman E, Eardley W, Rangan A, Hewitt C, McDaid C. Systematic review of systematic reviews for effectiveness of internal fixation for flail chest and rib fractures in adults. BMJ Open. 2019;9(4):e023444. Published 2019 Apr 1. doi:10.1136/bmjopen-2018-023444 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6500198
- Perera TB, Daley BJ. Flail Chest. [Updated 2018 Dec 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534090
- Kilic D, Findikcioglu A, Akin S, Akay TH, Kupeli E, Aribogan A, et al. Factors affecting morbidity and mortality in flail chest: comparison of anterior and lateral location. Thorac Cardiovasc Surg. 2011 Feb. 59(1):45-8.
- Veysi VT, Nikolaou VS, Paliobeis C, et al. Prevalence of chest trauma, associated injuries and mortality: a level I trauma centre experience. Int Orthop 2009;33:1425–33. 10.1007/s00264-009-0746-9
- Brasel KJ, Moore EE, Albrecht RA, et al. Western Trauma Association Critical Decisions in Trauma: Management of rib fractures. J Trauma Acute Care Surg 2017;82:200–3. 10.1097/TA.0000000000001301
- Vyhnánek F, Jirava D, Očadlík M, et al. [Surgical Stabilisation of Flail Chest Injury: Indications, Technique and Results]. Acta Chir Orthop Traumatol Cech 2015;82:303–7.
- de Moya M, Bramos T, Agarwal S, et al. Pain as an indication for rib fixation: a bi-institutional pilot study. J Trauma 2011;71:1750–4. 10.1097/TA.0b013e31823c85e9
- Velasquez M, Ordoñez CA, Parra MW, et al. Operative versus Nonoperative Management of Multiple Rib Fractures. Am Surg 2016;82:E103–5.
- Bhatnagar A, Mayberry J, Nirula R. Rib fracture fixation for flail chest: what is the benefit? J Am Coll Surg 2012;215:201–5. 10.1016/j.jamcollsurg.2012.02.023
- Dehghan N, de Mestral C, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014 Feb;76(2):462-8.
- Benjamin E, Recinos G, Aiolfi A, Inaba K, Demetriades D. Flail Chest: Less Deadly than Originally Thought. World J Surg. 2018 Jun 19
- Bastos R, Calhoon JH, Baisden CE. Flail chest and pulmonary contusion. Semin. Thorac. Cardiovasc. Surg. 2008 Spring;20(1):39-45.
- Poirier WJ, Vacca VM. Flail chest. Nursing. 2013 Dec;43(12):10-1.
- Beal SL, Oreskovich MR. Long-term disability associated with flail chest injury. Am J Surg. 1985 Sep. 150(3):324-6.
- Kishikawa M, Minami T, Shimazu T, et al. Laterality of air volume in the lungs long after blunt chest trauma. J Trauma. 1993 Jun. 34(6):908-12; discussion 912-3.
- Chardoli M, Hasan-Ghaliaee T, Akbari H, Rahimi-Movaghar V. Accuracy of chest radiography versus chest computed tomography in hemodynamically stable patients with blunt chest trauma. Chin. J. Traumatol. 2013;16(6):351-4.
- Balci AE, Ozalp K, Duran M, Ayan E, Vuraloğlu S. [Flail chest due to blunt trauma: clinical features and factors affecting prognosis]. Ulus Travma Acil Cerrahi Derg. 2004 Apr;10(2):102-9.
- Nishiumi N, Fujimori S, Katoh N, Iwasaki M, Inokuchi S, Inoue H. Treatment with internal pneumatic stabilization for anterior flail chest. Tokai J. Exp. Clin. Med. 2007 Dec 20;32(4):126-30.
- Gunduz M, Unlugenc H, Ozalevli M, Inanoglu K, Akman H. A comparative study of continuous positive airway pressure (CPAP) and intermittent positive pressure ventilation (IPPV) in patients with flail chest. Emerg Med J. 2005 May. 22(5):325-9.
- Tanaka H, Tajimi K, Endoh Y, Kobayashi K. Pneumatic stabilization for flail chest injury: an 11-year study. Surg Today. 2001. 31(1):12-7.
- Althausen PL, Shannon S, Watts C, Thomas K, Bain MA, Coll D, et al. Early surgical stabilization of flail chest with locked plate fixation. J Orthop Trauma. 2011 Nov. 25(11):641-7.
- Cataneo AJ, Cataneo DC, de Oliveira FH, Arruda KA, El Dib R, de Oliveira Carvalho PE. Surgical versus nonsurgical interventions for flail chest. Cochrane Database Syst Rev. 2015 Jul 29. CD009919
- Doben AR, Eriksson EA, Denlinger CE, Leon SM, Couillard DJ, Fakhry SM, et al. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J Crit Care. 2014 Feb. 29(1):139-43.
- Slobogean GP, MacPherson CA, Sun T, Pelletier ME, Hameed SM. Surgical fixation vs nonoperative management of flail chest: a meta-analysis. J Am Coll Surg. 2013 Feb. 216(2):302-11.e1.
- Freedland M, Wilson RF, Bender JS, Levison MA. The management of flail chest injury: factors affecting outcome. J Trauma. 1990 Dec. 30(12):1460-8.
- Albaugh G, Kann B, Puc MM, et al. Age-adjusted outcomes in traumatic flail chest injuries in the elderly. Am Surg. 2000 Oct. 66(10):978-81.
- Athanassiadi K, Gerazounis M, Theakos N. Management of 150 flail chest injuries: analysis of risk factors affecting outcome. Eur J Cardiothorac Surg. 2004 Aug. 26(2):373-6.
- Dehghan N, de Mestral C, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014 Feb. 76(2):462-8.