Fremitus
Fremitus is a palpable vibration transmitted through your body. In common medical usage, fremitus usually refers to tactile vocal fremitus, although there are several other types. Vocal fremitus also called pectoral fremitus or tactile vocal fremitus, is palpation of the chest wall to detect changes in the intensity of vibrations created with certain spoken words in a constant tone and voice indicating underlying lung pathology 1.
Vocal fremitus refers to the assessment of the lungs by either the vibration intensity felt on the chest wall (tactile fremitus) and/or heard by a stethoscope on the chest wall with certain spoken words (vocal resonance). The vocal cords produce vibrations in the tracheobronchial tree that are felt throughout the lungs and chest wall. This is usually assessed by asking a patient to repeat a word such as “ninety-nine,” while the healthcare provider feels the chest wall.
Evaluating for vocal fremitus, in the hands of an experienced examiner, can quickly rule in or out clinical issues of concern.
- Causes of increased vocal fremitus: pneumonia, lung abscess.
- Causes of decreased vocal fremitus: pleural effusion, pneumothorax, emphysema.
Other types of fremitus 2:
- Ronchial fremitus – palpable ronchi
- Pleural fremitus – palpable pleural rub
Sound vibrations produced in the larynx during phonation are transmitted to the bronchi and lungs and then communicated to the chest wall. Transmission of spoken tones depends on the state of the underlying lung parenchyma in the pleural space. Normal lung parenchyma is a mixture of air-filled spaces and solid lung parenchyma. Air is a poor conductor of low sound frequencies whereas a solid or dense medium increases the transmission of low sound frequencies. Vocal fremitus may be decreased in conditions affecting the lung parenchyma, pleura, or chest wall 3.
Vocal fremitus is decreased in bronchial asthma, emphysema, or bronchial obstruction due to air trapping and decreased density of lung parenchyma. In case of pleural effusion and pneumothorax, air/fluid accumulates in the potential space between the chest wall and lung parenchyma, decreasing the transmission of lower frequency sound vibrations. Vocal fremitus also may be decreased in individuals with obesity.
On the other hand, inflammation and consolidation create a dense medium which increases the transmission of lower frequency sounds and vocal fremitus.
Vocal resonance is the auscultatory counterpart of vocal fremitus. The following changes in vocal resonance are seen 4.
- Bronchophony: A louder sound heard over an area of consolidation.
- Whispering pectoriloquy: While the examiner auscultates over the lung fields, the patient is asked to whisper “one, two, three.” Whispered words are heard clearly in the presence of consolidation. Whispered pectoriloquy has the same significance as increased fremitus and adds no new information to those approaches.
- Egophony or an “E to A” change: A qualitative change in the voice that resembles the bleating of a goat. Select sound frequencies are able to pass through consolidation and tend to distort the sound of the vowel “E” so that it is perceived by the examiner as “A” or “AAAH.”
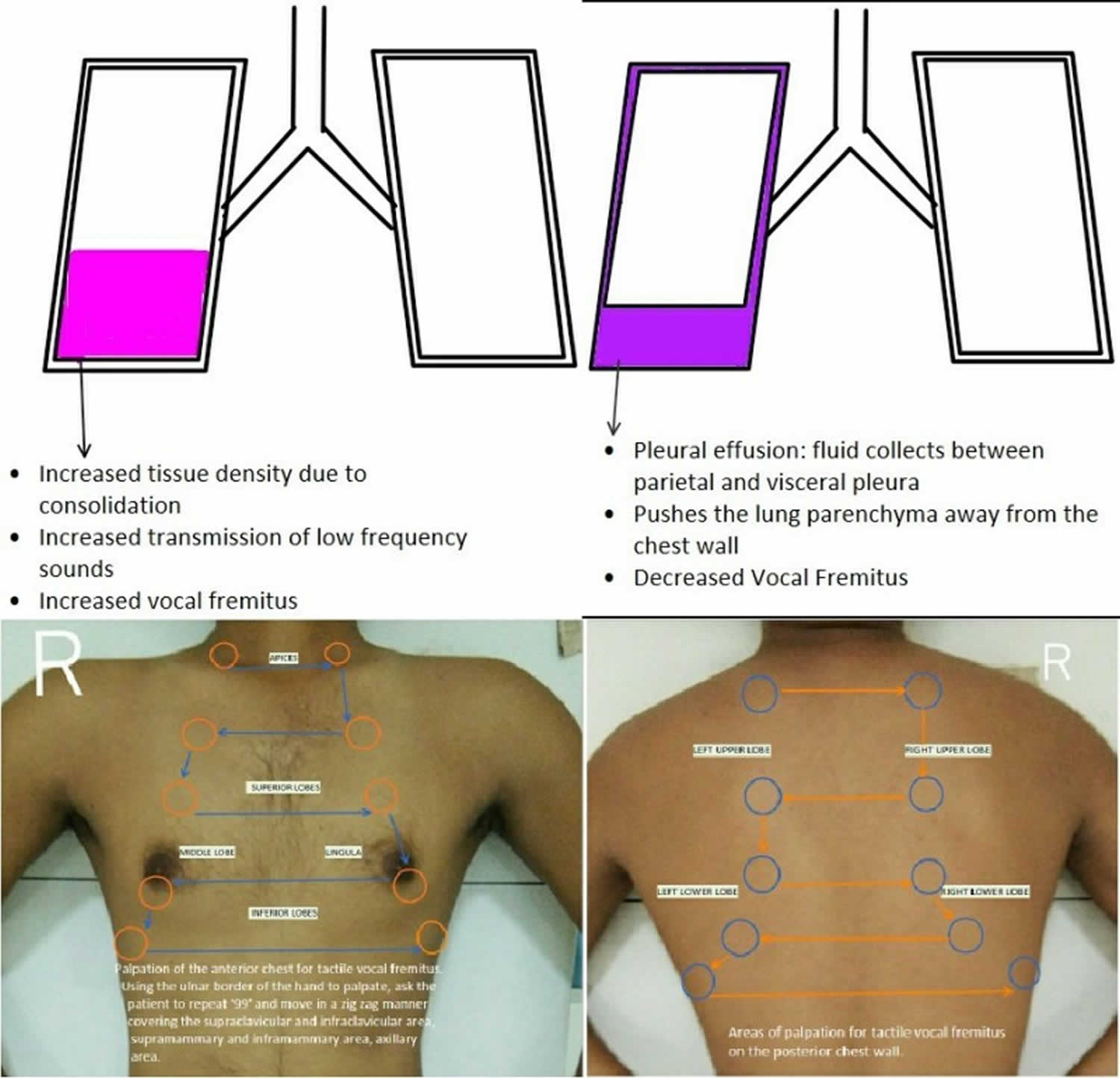
Figure 1. Tactile fremitus
Tactile fremitus test
The reliability of findings obtained using these maneuvers are controversial, and they are not frequently used by physicians in daily practice 2. However, undergraduate and postgraduate students are frequently required to perform these maneuvers during clinical assessments. A study among 100 general practitioners in Queensland, Australia was conducted to assess how frequently they performed vocal fremitus and vocal resonance and their opinions of the value of this procedure. Majority (65.7%) rarely performed vocal fremitus or vocal resonance as a routine during chest examination and more than half (53.7%) did not hold that routine vocal fremitus or vocal resonance examination is desirable 5.
Studies have shown variable inter-rater agreement for vocal fremitus assessments with some studies showing good and others showing poor inter-rater agreement.
On the other hand, it has been suggested that artifacts produced by vibrations of the thorax on color doppler sonographic examinations of breast tissue can be useful in differentiating benign and malignant mammary tumors. These artifacts are in the form of small color pixels which can be brought about by vocal fremitus. In benign tumors, color pixels are found only in surrounding tissue, whereas in malignant tumors, artifacts can be found within the tumor and the surrounding tissue. Power Doppler Vocal Fremitus can be used as an adjunct tool to B mode ultrasonogram for identification of breast lesions.
Examination method
Before palpating the posterior chest for tactile fremitus, the patient is asked to fold his or her arms across the chest wall to displace both scapulae. The patient is asked to repeat “ninety-nine” or “one, two, three” in a constant tone while the practitioner simultaneously palpates the chest wall on both sides, using the ulnar border of the hand or the palmar base. Palpation begins with the lung apex and moves to the same location on the opposite side of the chest wall. The perceived vibrations on both sides are compared while moving hands from the apex to the base of the lung, covering the entire posterior chest wall. The same maneuver is repeated on the anterior and lateral chest walls.
Interpretation of examination findings
Integration of history and physical findings of the respiratory system are important for formulating a differential diagnosis and planning further management. As discussed earlier, an increase in vocal fremitus indicates denser lung tissue, which can be caused by consolidation in diseases such as pneumonia. A decrease in vocal fremitus suggests air or fluid in the pleural spaces or a decrease in lung tissue density, which can be caused by diseases such as chronic obstructive pulmonary disease or asthma.
Pneumothorax tactile fremitus
- Inspection: Diminished chest movements on the affected side.
- Palpation: Diminished chest movements on palpation. Decreased vocal fremitus on the affected side.
- Percussion: Tympanic note on percussion of the affected side.
- Auscultation: Diminished breath sounds and vocal resonance on the affected side.
Pleural effusion tactile fremitus
- Inspection: Fullness of intercostal spaces and diminished chest movements on the affected side. The apical impulse may not be visualized.
- Palpation: Diminished chest movements on palpation of the affected side. Decreased vocal fremitus on the affected side. Trachea may be shifted to the opposite. The apical impulse may not be palpable.
- Percussion: Stony dullness on percussion of the affected side.
- Auscultation: Diminished breath sounds and vocal resonance on the affected side. Egophony may be present on the upper border of the effusion.
Tactile fremitus pneumonia
- Inspection: Diminished chest movements on the affected side.
- Palpation: Diminished chest movements on palpation of the affected side. Increased vocal fremitus on the affected side.
- Percussion: Dullness on percussion of the affected side.
- Auscultation: Bronchial breathing sounds may be present. Increased vocal resonance on the affected side may be associated with bronchophony and whispering pectoriloquy.
- Thomas DC, K P, Harigovind G, Sen D. Lung Consolidation Detection through Analysis of Vocal Resonance Signals. Conf Proc IEEE Eng Med Biol Soc. 2018 Jul;2018:957-960.
- Modi P, Tolat S. Vocal Fremitus. [Updated 2019 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499838
- Fiser W, Pai B, Vallurupalli S. Doppler vocal fremitus. Echocardiography. 2017 Mar;34(3):472-473.
- Kim MJ, Kim JY, Yoon JH, Youk JH, Moon HJ, Son EJ, Kwak JY, Kim EK. How to find an isoechoic lesion with breast US. Radiographics. 2011 May-Jun;31(3):663-76.
- Hla KS. Clinical usefulness of ‘vocal fremitus’ and ‘vocal resonance’–GP perceptions and practice. Aust Fam Physician. 2007 Jul;36(7):573, 576.