What is a gastrectomy
Gastrectomy is surgery to remove part or all of the stomach.
There are 4 main types of gastrectomy, depending on which part of your stomach needs to be removed:
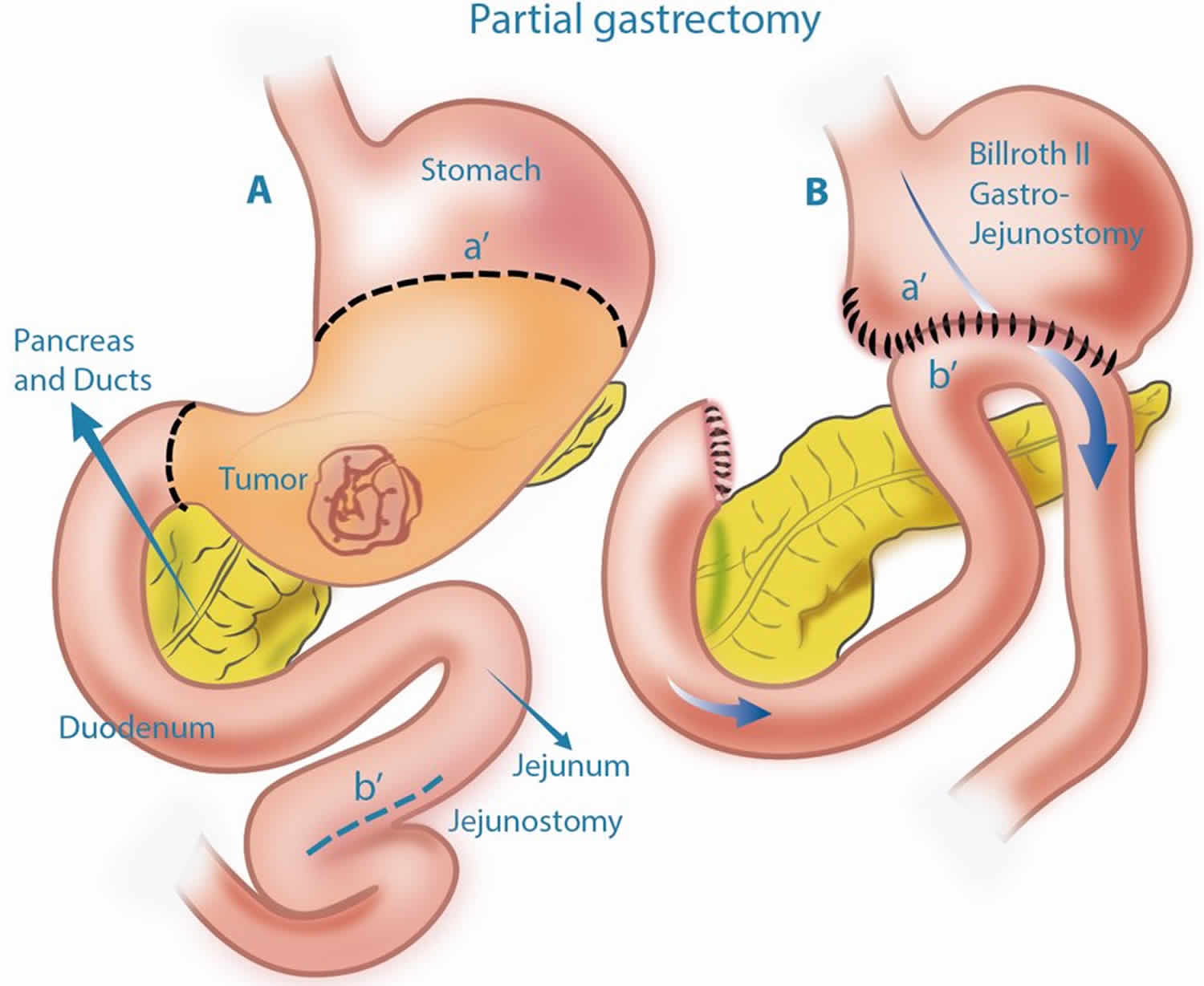
- Partial gastrectomy – the lower part of the stomach is removed
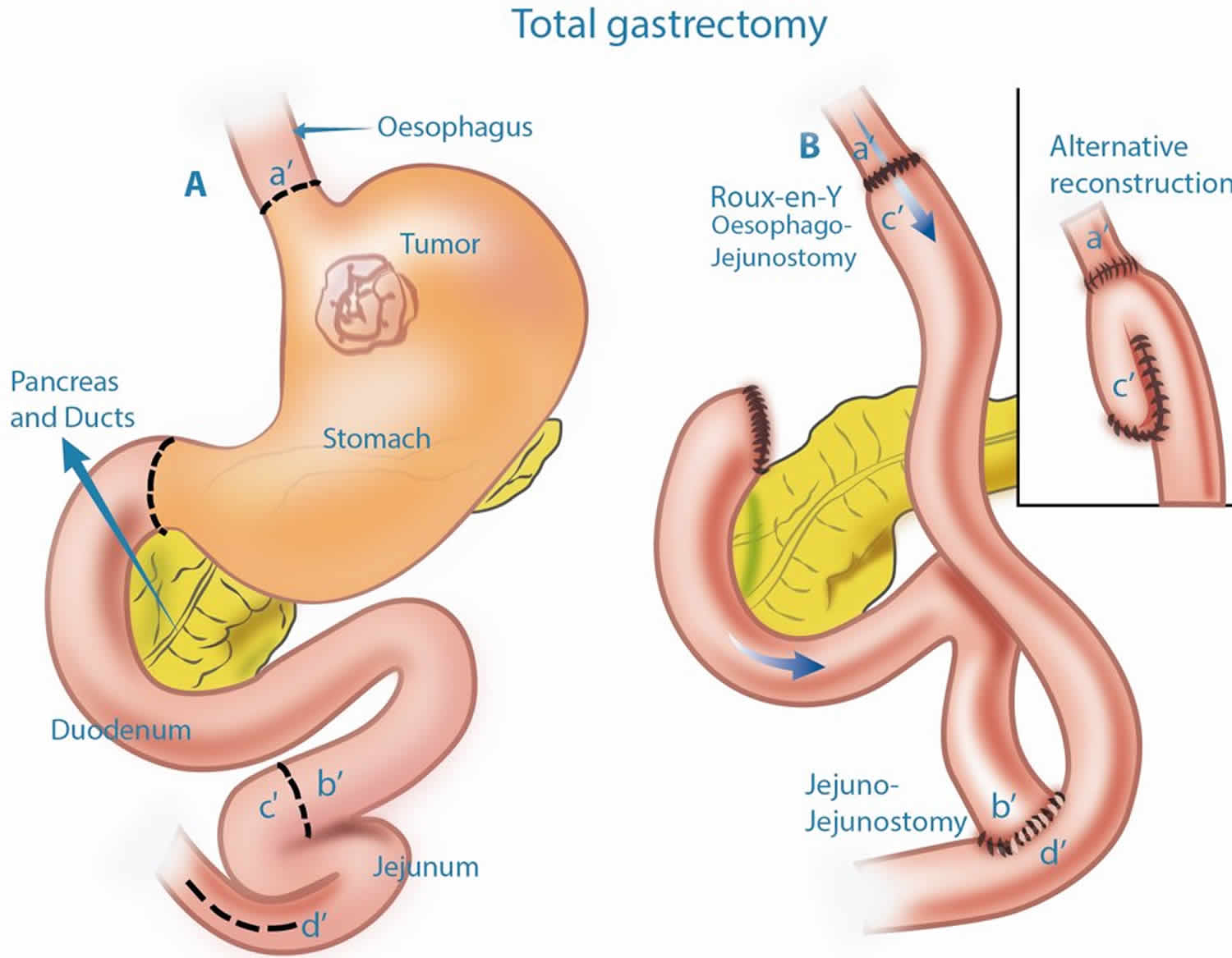
- Total gastrectomy – the whole stomach is removed
- Sleeve gastrectomy – the left side of the stomach is removed
- Esophagogastrectomy – the top part of the stomach and part of the esophagus (gullet), the tube connecting your throat to your stomach, is removed.
A gastrectomy is often used to treat stomach cancer.
Less commonly, gastrectomy surgery is used to treat:
- Life-threatening obesity
- Esophageal cancer
- Stomach ulcers (peptic ulcers)
- Non-cancerous tumors
- Stomach bleeding
- Stomach inflammation
- Stomach polyps
Gastrectomy is usually an effective treatment for cancer and obesity.
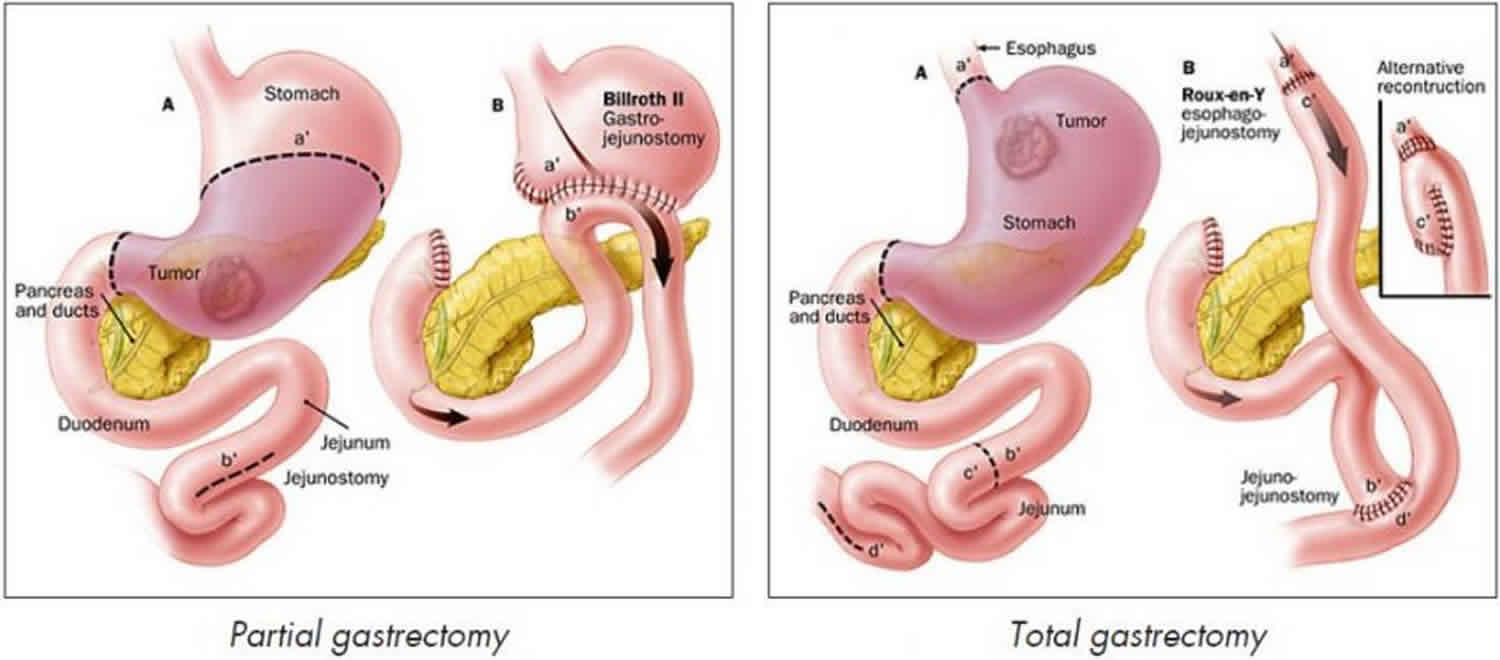
The top of the stomach is connected to the gullet (esophagus), the bottom of the stomach to the first part of the small intestine (duodenum), and the esophagus to either the small intestine or the remaining section of stomach. This means you will still have a working digestive system, although it won’t function as well as it did before.
All types of gastrectomy are carried out under general anesthetic, so you’ll be asleep and pain-free during the operation. The surgeon makes a cut in the abdomen and removes all or part of the stomach, depending on the reason for the procedure.
Depending on what part of the stomach was removed, the intestine may need to be re-connected to the remaining stomach (partial gastrectomy) or to the esophagus (total gastrectomy).
Today, some surgeons perform gastrectomy using a camera. The surgery, which is called laparoscopy is done with a few small surgical cuts. The advantages of this surgery are a faster recovery, less pain, and only a few small cuts.
Figure 1. Partial gastrectomy
Figure 2. Total gastrectomy
Techniques for gastrectomy
Two different techniques can be used to carry out a gastrectomy:
- Open gastrectomy – where a large cut is made in your stomach or chest
- Keyhole surgery (laparoscopic gastrectomy) – where several smaller cuts are made and special surgical instruments are used
People who have keyhole surgery usually recover faster and have less pain after the procedure than those who have an open gastrectomy. You may also be able to leave hospital a little sooner.
Complication rates after keyhole surgery are similar to those for open gastrectomies.
Open gastrectomies are usually more effective in treating advanced stomach cancer than keyhole surgery is. This is because it’s usually easier to remove affected lymph nodes (small glands that are part of the immune system) during an open gastrectomy.
Before you decide which procedure to have, discuss the advantages and disadvantages of both with your surgeon.
Gastrectomy risks
Risks for anesthesia and surgery in general include:
- Reactions to medicines or breathing problems
- Bleeding, blood clots, or infection
Risks for gastrectomy surgery include:
- Leak from connection to the intestine which can cause infection or abscess
- The connection to the intestine narrows, causing blockage
Gastrectomy preparation
Before the gastrectomy procedure
If you are a smoker, you should stop smoking several weeks before surgery and not start smoking again after surgery. Smoking slows recovery and increases the risk of problems. Tell your health care provider if you need help quitting.
Tell your surgeon or nurse:
- If you are or might be pregnant
- What medicines, vitamins, herbs, and other supplements you are taking, even ones you bought without a prescription
During the week before your surgery:
- You may be asked to stop taking aspirin, ibuprofen (Advil, Motrin), vitamin E, warfarin (Coumadin), and any other drugs that make it hard for your blood to clot.
- Ask your surgeon which drugs you should still take on the day of your surgery.
On the day of your surgery:
- Follow instructions about not eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
Recovering after a gastrectomy
How well you do after gastrectomy surgery depends on the reason for the surgery and your condition. A gastrectomy is a major operation, so recovery can take a long time. After surgery, there may be a tube in your nose (nasogastric tube) which will help keep your stomach empty for about 48 hours. The nasogastric tube allows fluids produced by your stomach to be regularly removed, which will stop you feeling sick. It is removed as soon as your bowels are working well.
Most people have pain from the surgery. You can control this with pain medicines.
You’ll also have a catheter placed in your bladder. This is to monitor your fluids, and to drain and collect urine while you recover.
You’ll usually stay in hospital for 1 or 2 weeks after the gastrectomy procedure, where you may receive nutrition directly into a vein until you can eat and drink again. Most people can begin eating a light diet about a week after a gastrectomy.
You’ll eventually be able to digest most foods and liquids. However, you may need to make changes to your diet, such as eating frequent small meals instead of 3 large meals a day. You may also need vitamin supplements to ensure you’re getting the correct nutrition.
Ask your surgeon if there are any activities you shouldn’t do after you go home. It may take several weeks for you to recover fully. While you are taking narcotic pain medicines, you should not drive.
Post gastrectomy diet
Whatever type of gastrectomy you have, you’ll need to make changes to your diet. It may be months before you can return to a more normal diet. A dietitian should be able to help you with this adjustment.
Food or drink you enjoyed before the operation may give you indigestion. You may find it helpful to keep a food diary to record the effects that certain types of food have on your digestion.
You’ll probably have to eat frequent small meals, rather than 3 large meals a day, for a fairly long time after having a gastrectomy. However, over time, your remaining stomach and small intestine will stretch and you’ll gradually be able to eat larger, less frequent meals.
High-fiber foods
Avoid eating high-fiber foods immediately after having a gastrectomy, as they’ll make you feel uncomfortably full. High-fiber foods include:
- wholegrain bread, rice and pasta
- pulses – which are edible seeds that grow in a pod, such as peas, beans and lentils
- oats – found in some breakfast cereals
You’ll gradually be able to increase the amount of fiber in your diet.
Vitamins and minerals
If you’ve had a partial gastrectomy, you may be able to get enough vitamins and minerals from your diet by eating foods that are high in nutrients – in particular, foods high in iron, calcium, and vitamins C and D. If you’ve had a total gastrectomy, you may be unable to get enough of these from your diet so may require supplements.
Eating after your gastrectomy surgery
Depending on exactly what surgery you have had, you may now have no stomach at all, or you may have a much smaller stomach. This means that you no longer have the capacity to eat large amounts of food in one sitting, but this may gradually increase. You may feel “full up” more quickly, but the sensation will probably be different.
It will take you a while to judge how much you are able to eat. If you have had a bad experience with a food, do not exclude it permanently – try reintroducing it again at a later date. Try to eat a wide variety of foods.
After your surgery, you will need to adopt a little and often meal pattern, as discussed previously. If you are having problems with weight loss, you may find the suggestions and recipes below helpful. If you previously followed a specific diet for medical reasons, check with your dietician/specialist nurse/hospital team if this is still necessary.
Snacks and Small Meals
- Keep snacks to hand so you can nibble throughout the day. Examples include:
- Peanut butter/pate/cheese/dahl on crackers
- Dips (e.g. hummus, guacamole, tzatziki, taramasalata, salsa) with breadsticks, tortilla chips, crisps, nachos or crackers
- Cocktail sausages, scotch eggs, samosas, olives, sausage rolls, nuts, Bombay mix, pasties
- Fresh/tinned/dried fruit, popcorn,
- Yogurt, rice puddings, ice creams, ice lollies
- Breakfast cereal, cereal bars
- Chocolate, sweets, cake, biscuits
- Teacakes, muffins, crumpets, croissants, pastries
Examples of nourishing small meals include:
- Sandwiches: These can be made from sliced bread, toast, bagels, baguettes, rolls, wraps, chapatti or pitta bread. Fill with cold meats, tinned fish, pate, dhal, hummus, egg, bacon, cheese or peanut butter. Add butter, mayonnaise, pickles, chutneys, salad or avocado to make them more interesting.
- On toast: Baked beans, cheese, sardines, eggs – poached, scrambled or fried. Add plenty of butter or margarine and top with grated cheese.
- French toast (eggy bread) or omelette. Add cheese / mushrooms/ ham
- Jacket potatoes with butter and fillings such as cheese, baked beans, tuna mayonnaise, chilli con-carne, coleslaw, bolognaise sauce, hummus or sour cream.
- Ready made meals: Can be frozen, chilled, tinned or boil in bag
- Nourishing Soups: If having soup as a meal, choose one that contains meat, fish, cheese, lentils peas or beans. Make soup with full cream milk or add cream and serve with a buttered roll.
- Pasta: Instant or microwaved pasta with added cheese, cream, buttered &/ or ham
- Puddings:
- Milk puddings such as rice or semolina. Add jam, fresh or tinned fruit or cinnamon, sultanas or brown sugar.
- Thick and creamy or custard style yoghurt, fromage frais, fruit mousse or fool, trifle.
- Sponge pudding, jelly with tinned fruit and ice cream or cream. Add raspberry or chocolate sauce.
- Hot or cold pie or crumble with cream, ice cream or custard.
- Waffles or pancake with maple syrup and cream or ice cream.
- Cheesecake or sweet pastries with cream.
- Baked apple or banana with brown sugar and sultanas. Serve with custard, cream or ice cream.
- Whisk a small tin of evaporated milk into a cooled jelly made with ½ pint water to make a milk jelly.
- Use custard and stewed or pureed fruit to make a fruit fool.
- Banana and chocolate or other confectionery can be chopped into Angel Delight.
- Full fat Greek yogurt with honey and soft fruit. This can be topped with brown sugar and grilled to make crème brulee.
- Adding cream to any pudding will boost the energy content. For convenience try aerosol creams, these keep well in the fridge. Long life cream is also useful.
- Adding Calories and Protein
- Melt butter on vegetables, meat and fish
- Add grated cheese or cream to mashed potato, vegetables and soup.
- Use sauces or gravy with meat and fish
- Add dried skimmed milk powder to full cream milk (4 tablespoons milk powder mixed into a pint of milk) and use this for your drinks and in cooking (e.g. porridge, sauces, soup and milk puddings.)
- Add chopped ham or shredded chicken to soups
- Add sugar/honey/syrup to drinks, cereals, desserts and fruit.
- Add cream to desserts, milk puddings, fruit and sauces.
Nourishing Drinks
Milk based drinks
- Fortified milk: Add 2 oz (4 tablespoons) of milk powder such as Marvel or 5 pints to 1 pint of full cream milk. Use fortified milk to make up:
- Hot milk drinks:
- Ovaltine, Horlicks, Bournvita, hot chocolate (Avoid low calorie types)
- Milky coffee
- Double cream or evaporated milk can be added to a hot milky drink
- Cold milk drinks:
- Milk shakes made with cordials, fruit juice, milk shake syrup or powder. Add a scoop of ice cream for extra nourishment
- Fruit smoothie: blend fruit e.g. banana with milk plus ice cream/yogurt and honey or malt
- Savory milk drinks:
- Instant soups
- Bovril or Marmite
- Yogurt Drinks:
- Can be purchased, or yogurts can be diluted with milk to make yogurt shakes
- Hot milk drinks:
Fruity Drinks
- Fruit juice – fresh or long life
- Fruit juice mixed with fizzy drinks e.g. lemonade are refreshing
- Fizzy drinks e.g. Lucozade, Appletize, Schloer, lemonade, Coca Cola, tonic water
- Try to avoid “low calorie” and “diet” options
Ice cream soda
- Can be made by adding ice cream to a fizzy drink
Supplement Drinks
- Complan and Build Up shakes and soups are available from most pharmacies and supermarkets. They come in a variety of sweet and savoury flavours.
- There is also a wide range of nutritional supplement drinks available on prescription. They can be used to supplement your intake and help to maintain your weight. If you feel that you would benefit from using these products, ask your dietician who will be able to advise you.
Swallowing
Your ability to swallow should not be impaired but some anxiety about food entering the adapted digestive system can make it feel a little difficult and lumpy at first. Start with soft foods and gradually move onto a normal diet as you feel able. There are no foods that you should avoid. Chew foods well, and take time to eat. Bread may be difficult for some people to swallow. If this is the case, try toast and crispbreads as they may be easier to manage.
Do not be alarmed in the early weeks if you have problems with swallowing. This often occurs due to narrowing of the join.
Appetite
You may find that you have a reduced appetite or none at all during the early stages of recovery. This should improve with time and establishing a little and often meal pattern should help with this.
Tips to Stimulate your Appetite:
- Relax and avoid rushing meals
- Try using a smaller plate and serve meals which are attractive and colorful.
- If you are too tired to prepare a meal, have a ready meal instead or tinned foods.
- If food has no taste, try stronger flavors such as seasoned/marinated foods.
- Try getting some fresh air before a meal.
- Establishing a little and often meal pattern will help to stimulate appetite in time, so try not to miss meals or snacks.
- Make the most of the foods that you enjoy. No food is forbidden.
- Make the most of when you do feel hungry, even if this is outside conventional meal/snack times.
- If you are having problems with nausea, you may prefer having your food at room temperature or cold.
- If you find cooking smells a problem, avoid the kitchen or use cold or microwaved foods. Perhaps someone else can prepare your food for you. However, for some, the smell of food will tempt the appetite.
- A small drink of sherry or other aperitif, or even a small beer, before a meal may help to stimulate your appetite and improve taste.
Little and often mean pattern
The key to eating well after surgery is not to eat large meals, but to eat smaller amounts regularly. You may find this difficult at first, but try to eat six times a day; three small meals and nourishing snacks in-between. Eat slowly and chew your food well. This will help you digest your food and prevent you feeling full too quickly. You will feel uncomfortable if you eat too much at one time. You will gradually get to know what the right amount is for you. Eating more frequently can be a pleasure – biscuits with coffee in the morning; a scone or cake with tea in the afternoon; a gap between courses. Try to make it an enjoyable activity.
Taste changes
After any operation you may find that your sense of taste can be affected. This should improve with time. You may prefer foods that you previously did not enjoy and vice versa. Some of the tips suggested above may be helpful.
Drinking
Drinking is important and you should make sure that you drink plenty of fluids. However, you must be careful not to fill yourself up with fluids before or during a meal or you will not want to eat your food. Try not to drink for 20 minutes before or after a meal and when eating, just take sips instead. There is no reason why alcohol should not be taken but the effect may be felt a little earlier than prior to your operation – so beware. Remember certain medicines can react with alcohol – check with your doctor or pharmacist. It is not just water that contributes to your fluid intake – think of more nourishing drinks.
Dealing with weight loss
It is quite common to lose weight after gastrectomy and this may continue for some time. You may not return to the weight you were prior to your illness; however you should establish a new stable weight. Eating little and often and choosing high calorie and high protein foods can help to minimize weight loss. If you have any concerns about weight loss, you should speak with your dietitcian/doctor/specialist nurse/hospital team.
Life after total gastrectomy
Every individual recovers at a different rate – some recover more slowly than others. Your energy levels will return over time, however be prepared for episodes of reduced stamina in the months after your operation. If you were working before your operation you may require a prolonged time off work.
The first few weeks
You start moving about soon after the operation, sometimes with the help of a physiotherapist. This is a very important part in your recovery. Initially, moving around will be challenging, however day by day this will improve. It is recommended that you increase your activity levels over a number of weeks. Building up your activity during this early period should be taken by increasing speed or distance – not both. Bear in mind that outdoor walking is more difficult – there may be slopes/wind and heavier clothing to wear – and do not forget the return journey.
It is not recommended that you do any heavy lifting or driving until you are reviewed by your surgical team. If you feel able, light duties can be undertaken. Continue the breathing exercises given to you in hospital.
During the early stages you may be concerned about causing damage to yourself. Coughing, vomiting, and physical activity may be uncomfortable, but be assured it will not cause you harm.
During the operation, muscles have been stitched together but these heal well in the first few weeks. Nerves, which are necessarily cut in any operation, repair very slowly and some areas around the wound may remain numb.
You may find that your ability to concentrate has been affected. This can be very frustrating, but it will gradually return. It may help to take up a new hobby while you have got time on your hands.
Driving
It may be helpful to inform your motor insurance company that you have undergone major surgery before you start to drive again. You must be capable of performing an emergency stop with ease. Discuss this at your first outpatient appointment with the surgical team.
Eating out
Eating with others is a very social activity, which you should still be able to enjoy. Friends and family should be aware that you may need smaller portions. Do not worry about leaving food on your plate.
Sleep
It may take several weeks to establish your normal sleeping pattern. If required, you can take a pain killer before going to bed to help with comfort during the night. You may benefit from an afternoon nap in the early stages of recovery.
Psychological effects and support
The treatment that you have had may be stressful for both you and your family, you may benefit from talking to family, friends or a professional such as a psychologist or counselor. Your doctor or specialist nurse can refer you. Patients may also find it helpful to talk to somebody who has also had the surgery. There are local groups around the country and you can be told about the one nearest to you.
Relationships and sex
The trauma of being diagnosed with cancer and undergoing surgery often affects your relationships with others. Both partners may be worried about having sex after surgery. It is normal to feel anxious, but sex should be possible and as enjoyable as it was before. It may be best to wait 4-6 weeks, but allow yourself plenty of time if you feel uneasy about resuming sex. Treat it like any other activity; if you are tired and tense wait until you are ready.
Exercise
Be sensible – when you feel able to start exercising, start slowly and build on this. Swimming or walking are good exercises to start with. Be careful of strenuous or weight lifting exercises. These and sports like running can be added later (up to marathon standard if you are really determined – one of our former patients has run several). If you were previously overweight, now is your chance to keep that new slim figure by taking up a sport that you used to find too energetic. There are no limitations to the type of exercise you can do, when you feel confident and strong enough. The most important things about exercise are that it should be taken regularly and be enjoyable.
Back to work
The timing of a return to work depends on many factors; age, type of work, effort put into regaining fitness. In any event it may be some months before you do, but we are all individuals. Heavy work makes more demands and might in fact not be suitable if much bending and lifting is involved. Hopefully your employer may be able to help by using your skills and knowledge for lighter work. A gradual or staged return to work may be helpful in building stamina. Also you may tire more quickly so if driving or working with machinery is involved in your job, extra care and planning may be necessary. It is important to think about what you can eat in work. If you are being more active now that you are back at work, remember you will need to eat more. You will need to consider what foods are available in your workplace and whether you need to plan ahead, and bring convenient snacks.
Follow up after gastrectomy surgery
You should be seen by your surgical team soon after discharge following your operation. Further appointments may then be made but some hospitals leave it to the patient to make contact if they feel the need. If you have had surgery for cancer, it is natural for you to worry about the cancer coming back. You can discuss this at your appointment. Some hospitals provide specialist nutrition advice by a dietician for patients after this surgery and you should seek their support regarding problems with your weight or eating and drinking. If you do not have direct access to a dietician, your doctor or specialist nurse can facilitate a referral.
Gastrectomy possible complications
As with any type of surgery, a gastrectomy carries a risk of complications. Problems can also occur because of changes in the way you digest food.
Gastrectomy to treat cancer
Gastrectomies to treat stomach cancer carry a higher risk of complications because most people who have this type of surgery are elderly and often in poor health.
Complications can also occur after a gastrectomy to treat oesophageal cancer. The oesophagus, also called the gullet, is the tube connecting your throat to your stomach.
Possible complications of a gastrectomy include:
- wound infection
- leaking from a join made during surgery
- stricture – where stomach acid leaks up into your esophagus and causes scarring, leading to the esophagus becoming narrow and constricted over time
- chest infection
- internal bleeding
- blockage of the small intestine
An infection can usually be treated with antibiotics, but some other complications require further surgery. Before your operation, ask your surgeon to explain the possible risks and how likely they are.
Gastrectomy to treat obesity
Possible complications of a gastrectomy for obesity include:
- nausea and vomiting – this usually gets better over time
- internal bleeding
- blood clots
- leaking from where the stomach has been closed
- acid reflux – where stomach acid leaks back up into the esophagus
- infection
It may be possible to treat some complications with medication, but others may need further surgery. Before your operation, ask your surgeon to explain the possible risks and how likely they are to affect you.
Vitamin deficiency
One the stomach’s functions is to absorb vitamins – particularly vitamins B12, C and D – from the food you eat.
If your entire stomach has been removed, you may not get all the vitamins your body needs from your diet. This could lead to health conditions such as:
- anemia
- increased vulnerability to infection
- brittle bones (osteoporosis) and weakened muscles
Changing your diet may help to compensate for your stomach’s inability to absorb vitamins. However, you may need vitamin supplements even after changing your diet. The healthcare professionals treating you can advise on this.
Dumping syndrome
Dumping syndrome is a set of symptoms that can affect people after a gastrectomy. It’s caused when particularly sugary or starchy food moves suddenly into your small intestine.
Before a gastrectomy, your stomach digested most of the sugar and starch. However, after surgery, your small intestine has to draw in water from the rest of your body to help break down the food.
Early Dumping Syndrome
The amount of water that enters your small intestine can be as much as 1.5 liters (3 pints). Much of the extra water is taken from your blood, which means you experience a sudden fall in blood pressure.
The drop in blood pressure can cause symptoms such as:
- faintness
- sweating
- palpitations
- a need to lie down
The extra water in your small intestine will cause symptoms such as:
- bloating
- rumbling noises
- nausea
- indigestion
- diarrhea
If you have dumping syndrome, resting for 20 to 45 minutes after eating a meal may help. To ease the symptoms of dumping syndrome:
- eat slowly
- avoid sugary foods – such as cakes, chocolate and sweets
- slowly add more fiber to your diet
- avoid soup and other liquid foods
- eat smaller, more frequent meals
Seek advice from your hospital team or dietitian if you have symptoms of dumping syndrome. For most people, the symptoms improve over time.
It can be unpleasant and distressing, but is not serious and generally the frequency of attacks becomes less. Relaxing or taking a rest may be helpful after eating.
Late Dumping Syndrome
Late Dumping Syndrome results from your blood sugar levels dropping. This is in response to too much insulin being produced. It can happen up to two hours after eating, with or without an earlier episode or early dumping syndrome.
Late Dumping Syndrome symptoms include:
- tiredness
- tremor
- palpitations
- sweating
- giddiness.
If this happens, you should have something containing sugar e.g. fruit juice, a sugary drink or biscuits. Some people find it helpful to carry glucose/dextrose tablets.
Dumping Syndrome is a complex subject. It can be improved by appropriate dietary changes and the frequency of episode will improve with time. However, it is important not to put any unnecessary restrictions on your eating. Seek advice from your dietician/hospital team if you are experiencing any of these symptoms.
Delayed gastric emptying and sickness
Food can sometimes remain in the stomach too long, causing you to feel sick and bloated; this may be as a result of nerves that are necessarily cut during the operation. It is very common and your doctor/surgical team will be able to give you a medicine (for example, Metoclopramide or Domperidone) which you should take half an hour before each main meal to improve stomach emptying. It usually improves with time. If the problem persists, speak to your doctor/surgeon/specialist nurse.
Morning vomiting
After a partial gastrectomy, a small number of people may experience morning vomiting. Vomiting occurs when bile – a fluid used by the digestive system to break down fats – and digestive juices build up in the first part of your small intestine (duodenum) overnight, before moving into what remains of your stomach.
Because of its reduced size, your stomach is likely to feel uncomfortably full, triggering a vomiting reflex to get rid of the excess fluids and bile.
Taking indigestion medication, such as aluminium hydroxide, may help to reduce the symptoms of morning vomiting. See your GP if your symptoms are particularly troublesome.
Food sticking
After surgery scar tissue at the join in the esophagus may restrict the flow of food. This can be worrying and a reminder of your original symptoms. It is treated by dilating/stretching the join with a balloon during an endoscopy. It is a routine procedure and may only have to be carried out once but a few patients may need to have it done several times in the early months. Do not persist with the problem too long; it is better to treat it early. Consult your doctor/surgeon/specialist nurse if you feel this aspect could be improved.
Acid reflux
Acid reflux is a common problem after surgery. It occurs most commonly at night or in the early morning. The symptoms can be a burning feeling in the stomach or throat or an unpleasant taste in the mouth or coughing on waking. Reflux can be treated by taking an acid suppressant (e.g. Omeprazole, Lansoprazole). You should liaise with your doctor/surgeon/specialist nurse regarding the dosage and timing of your medication. Certain medications (e.g. Metoclopramide, Domperidone) may also be helpful and are available on prescription.
Keeping some food in the digestive system may help prevent a build up of acid. Extra pillows or raising the bed head by about 4 – 6 inches with blocks of wood or a house brick can be very beneficial, and a pillow under the knee area may prevent slipping down during the night. Electric beds are now available much more cheaply than in the past.
Burping or belching
You will probably experience a tendency to burp more than before. Sometimes it can almost be involuntary but with practice some control is gained and embarrassment can be avoided. You may also feel as if you have trapped wind. This can be painful and worrying, but it does improve fairly quickly. You may find drinking peppermint tea helpful.
Diarrhea
During a gastrectomy, it’s sometimes necessary to cut a nerve called the vagus nerve, causing many people to experience bouts of diarrhea. The vagus nerve helps to control the movement of food through your digestive system.
Speak to your doctor or nurse if you have diarrhea, as treatments are available.
Change in bowel habit
Due to the surgery you may experience changes in bowel habit which also should settle with time. Most people will find that their stools are looser/softer. However some may have watery stools and this may be accompanied by colicky pain. These problems are easily managed by medication and are rarely associated with any particular food. If this is affecting your quality of life speak to your doctor/surgeon/specialist nurse. If you notice that your stools are pale/oily/difficult to flush, it may be a sign that you are not absorbing the fat from the food that you eat and may cause further weight loss. This can be improved by taking a medication at the same time as your food. Speak to your doctor/surgeon/specialist nurse/dietician for advice.
Weight loss
Immediately after surgery, you may find that even eating a small meal makes you feel uncomfortably full. This could lead to weight loss.
Losing weight may be desirable if you’ve had a gastrectomy because you’re obese, but it can be a health risk if you’ve been treated for cancer.
Some people who have a gastrectomy regain weight once they have adjusted to the effects of surgery and have changed their diet. But if you continue to lose weight, see a dietitian. They can give you advice on how to gain weight without upsetting your digestive system.
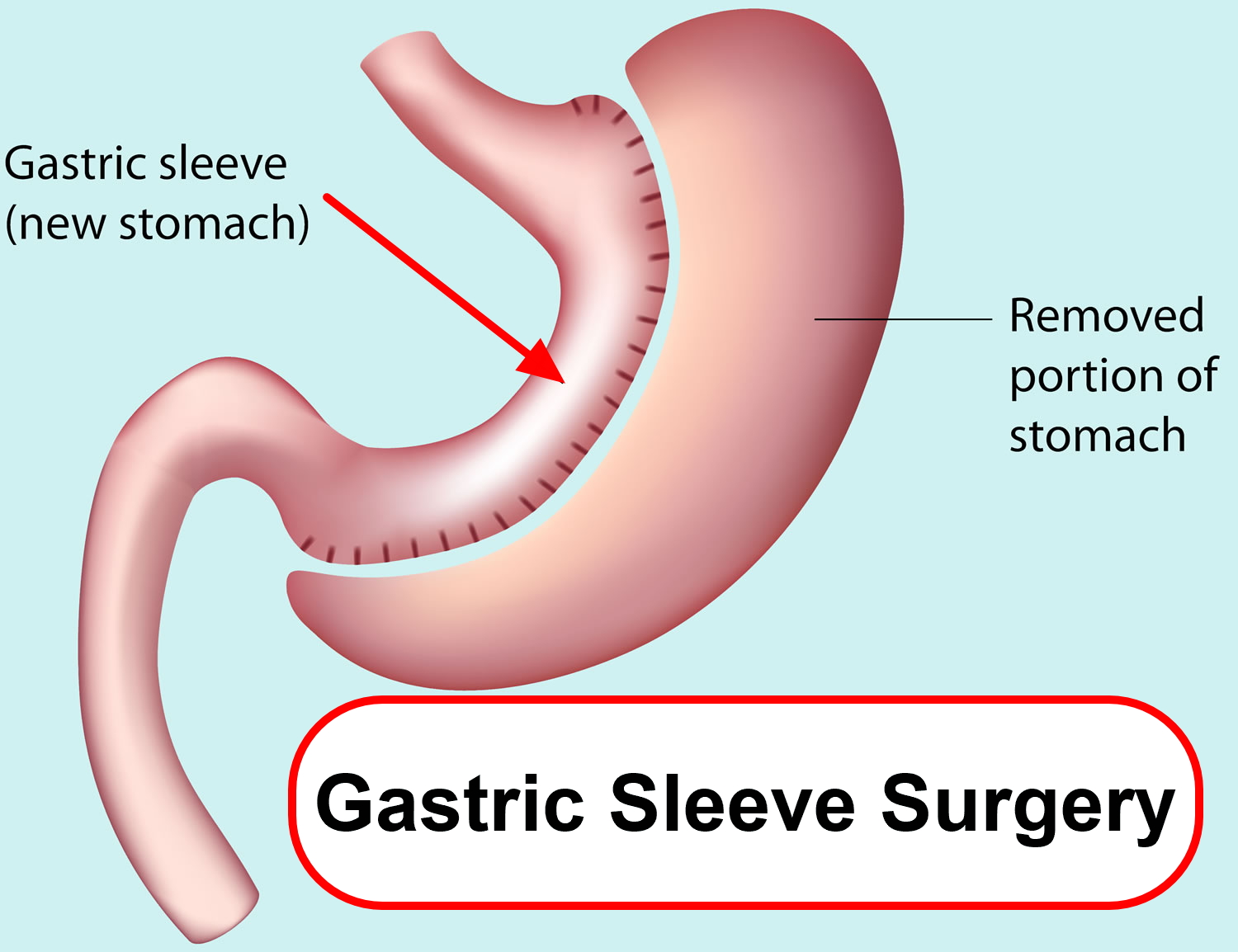
What is a sleeve gastrectomy
Sleeve gastrectomy, also called a vertical sleeve gastrectomy, is a surgical weight-loss procedure. This procedure is typically performed laparoscopically (laparoscopic sleeve gastrectomy), which involves inserting small instruments through multiple small incisions in the upper abdomen. During sleeve gastrectomy, about 80 percent of the stomach is removed, leaving a tube-shaped stomach about the size and shape of a banana.
Limiting the size of your stomach restricts the amount of food you are able to consume. In addition, the procedure prompts hormonal changes that assist with weight loss. The same hormonal changes also help relieve conditions associated with being overweight, such as high blood pressure or heart disease.
Figure 3. Gastric sleeve surgery
Why is sleeve gastrectomy done?
Sleeve gastrectomy is done to help you lose excess weight and reduce your risk of potentially life-threatening weight-related health problems, including:
- Gastroesophageal reflux disease (GERD)
- Heart disease
- High blood pressure
- High cholesterol
- Obstructive sleep apnea
- Type 2 diabetes
- Stroke
- Infertility
Sleeve gastrectomy is typically done only after you’ve tried to lose weight by improving your diet and exercise habits.
In general, sleeve gastrectomy surgery could be an option for you if:
- Your body mass index (BMI) is 40 or higher (extreme obesity).
- Your BMI is 35 to 39.9 (obesity), and you have a serious weight-related health problem, such as type 2 diabetes, high blood pressure or severe sleep apnea.
- In some cases, you may qualify for certain types of weight-loss surgery if your BMI is 30 to 34 and you have serious weight-related health problems.
You must also be willing to make permanent changes to lead a healthier lifestyle. You may be required to participate in long-term follow-up plans that include monitoring your nutrition, your lifestyle and behavior, and your medical conditions.
Check with your health insurance plan or your regional Medicare or Medicaid office to find out if your policy covers weight-loss surgery.
Sleeve gastrectomy surgery risks
As with any major surgery, sleeve gastrectomy poses potential health risks, both in the short term and long term.
Risks associated with the sleeve gastrectomy can include:
- Excessive bleeding
- Infection
- Adverse reactions to anesthesia
- Blood clots
- Lung or breathing problems
- Leaks from the cut edge of the stomach
Longer term risks and complications of sleeve gastrectomy surgery can include:
- Gastrointestinal obstruction
- Hernias
- Gastroesophageal reflux
- Low blood sugar (hypoglycemia)
- Malnutrition
- Vomiting
Very rarely, complications of sleeve gastrectomy can be fatal.
Preparing for gastric sleeve surgery
If you qualify for endoscopic gastric sleeve surgery, your health care team will give you specific instructions on how to prepare for your surgery. You may need to have various lab tests and exams before surgery. You may have restrictions on eating, drinking and which medications you can take. You also may be required to start a physical activity program.
Preparing for this major operation takes months of work. You need to show that you are willing and able to make big changes in your eating and exercise habits before the surgery.
Before having surgery, you’ll need to enroll in a bariatric surgery education program. This will help you get ready for surgery, and life after surgery. You’ll have nutritional counseling. And you may have a psychological evaluation. You’ll also need physical exams and tests. You will need blood tests. You may have imaging studies of your stomach, or have an upper endoscopy.
If you smoke, you will need to stop several months before surgery. Your surgeon may ask you to lose some weight before surgery. This will help make your liver smaller, and make surgery safer. You’ll need to stop taking aspirin, ibuprofen, and other blood-thinning medicines in the days before your surgery. You shouldn’t eat or drink anything after midnight before surgery.
If you’re a candidate for gastric sleeve surgery, the best place to get it is at a hospital with a bariatric surgery program that involves a team of specialists. Members of the team will explain what’s involved, help you prepare for your surgery, and care for you after surgery. For several months before surgery, you will work with the medical team to build the skills needed for success.
Here are some of the people who work as a team to help teens prepare for gastric sleeve surgery:
- Doctors and surgeons
Several months before your surgery, you’ll meet with a medical doctor and surgeon. They will explain what happens during surgery, examine you, and talk about what to expect before and after surgery. Your doctors will also let you know about some of the things that can go wrong (you’ll probably hear doctors call these “complications”).
- Psychologists
People go through lots of emotions before and after surgery. A psychologist can help you understand your feelings and help you prepare emotionally for surgery and the changes that will follow. For example, when you’re out with friends after your surgery, you won’t be able to eat the way you used to.
The psychologist will help you develop coping strategies as you learn to change your relationship with food. He or she also will help you with things like worry, stress, or emotional eating. It’s always a good idea to take advantage of a psychologist’s expertise as you prepare for gastric sleeve surgery.
- Dietitians
Because patients often depend on other family members for meals, a dietitian will teach you and your family healthy eating basics like good nutrition, how to get regular meals, and the right portion sizes.
Gastric sleeve surgery permanently decreases the size of your stomach. You will have to eat less than you did before. Your dietitian will explain what and how much you can eat after surgery, both immediately after the operation and for the rest of your life.
- Exercise specialists
These experts help patients get more active. They’ll work with you to develop an exercise program you’ll like and workouts you can stick with. It’s like having a personal trainer. Exercising during the months before surgery helps patients get in better shape for the operation. This will make recovery easier.
There’s another reason why it’s good to exercise regularly before surgery: After the operation, it will be easier to get back into working out if you’ve already made a habit of it. Lots of patients find that having a workout routine helps them feel better after surgery, but you will have to go slow. Talk to your doctor and exercise specialist to get their advice on how to gradually get back into your exercise routine.
What happens during gastric sleeve surgery?
Endoscopic gastric sleeve surgery is done in the endoscopy unit as an outpatient procedure. General anesthesia is used for the procedure, so you’ll be unconscious throughout the surgery.
The gastric sleeve surgery is done using an endoscope, a flexible tube with a camera and an endoscopic suturing device attached. The endoscope is inserted down your throat into the stomach. The tiny camera allows the doctor operating the endoscope (endoscopist) to see and operate inside your stomach without making incisions in your abdomen.
Using the endoscope, the doctor places approximately 12 sutures in the stomach. The sutures change the structure of your stomach, leaving it shaped like a tube. This restricts the amount of calories your body absorbs.
The procedure takes about 90 minutes. After the endoscopic sleeve gastroplasty, you’ll awaken in a recovery room, where medical staff monitors you for any complications.
The majority of people leave go home the same day after recovering from sedation. Some people might require a short admission to the hospital for one day or less for observation after the procedure.
Laparoscopic gastric sleeve surgery
In other surgical centers, your surgeon will use laparoscopy instead of the endoscope. In the laparoscopic gastric sleeve surgery (keyhole surgery), your surgeon will make several small cuts (incisions) in your upper abdomen. The surgeon will then insert a laparoscope and put small surgery tools into these incisions.
The surgeon will then use a laparoscopic stapler to divide the stomach, leaving a narrowed vertical sleeve. The part of the stomach that was removed is then taken out of the abdomen through an incision. Your surgeon may then test for any leaks in the sleeve using a dye study or an upper endoscopy.
Gastric sleeve surgery recovery time
After the gastric sleeve surgery, you generally won’t be allowed to eat for about eight hours. People usually recover from gastric sleeve surgery in a week. But it will take several weeks before you can eat regular food again. Gastric sleeve surgery makes your stomach smaller — permanently. To ease into having a much smaller stomach, you’ll need to follow a special diet that starts with liquids only, wich you need to continue for at least two weeks. Over four weeks, you’ll move on to semi-solid foods, and then to a regular healthy diet. You’ll also have medical checkups and meet with a nutritionist and psychologist frequently after your gastric sleeve surgery.
Sleeve gastrectomy diet
Your surgery team will give you a schedule of types of meals over the next weeks. After the surgery, you’ll start with liquid foods. Over the next few weeks you will change to pureed food, then to solid food. Your meals will be much smaller and you may have to stop drinking with meals due to your small stomach. Each meal needs to be very small.
You should make sure to eat slowly and chew each bite well. Don’t move too quickly to regular food. This can cause pain and vomiting. Work with your healthcare team to figure out what’s best for you to eat. After your stomach heals, you will need to change your eating habits. You’ll need to eat small meals for your small stomach.
Your dietitian will give you an eating plan that gradually works up to solid foods; for example:
- For the first 2 to 3 weeks after surgery, you’ll get all your nutrition from high-protein drinks.
- For the next 2 weeks or so, you’ll eat puréed foods.
- Finally, you’ll move on to soft foods for another couple of weeks before you can eat regular food.
How quickly someone moves from one stage to the next depends on the person. Your medical team will advise you based on what’s best for you.
If you rush a stage or eat something before your body’s ready for it — or if you eat too much — you’ll feel very uncomfortable. You may throw up. Eventually you’ll be able to eat more of the foods you’re used to. But for the rest of your life, you’ll always have to eat much smaller portions. You’ll also feel full faster.
Because you can’t eat as much, the foods you choose to eat really matter. Your dietitian will help you put together a lifelong healthy diet that includes fruits and vegetables and emphasizes protein. Your dietitian also will recommend vitamin and mineral supplements so you don’t miss out on key nutrients.
Your new diet will limit the amount of processed foods and snacks like chips and candy that you can eat. This is because these foods don’t have a lot of nutritional value (dietitians sometimes call them “empty calories”).
In addition to eating a sensible diet, exercising is a key part of staying healthy and maintaining weight loss after surgery.
People who follow the recommended diet and exercise plan often lose a large amount of weight in the months after gastric sleeve surgery. After that, weight begins to stabilize. Your team of specialists will keep seeing you for several months after surgery to monitor your diet and health, and to help you stay on track.
You will need to make significant lifestyle changes after bariatric surgery to lose weight and keep it off. For example, you’ll get nutritional advice from a dietitian on how to change your eating habits to keep healthy while losing weight.
People who have weight-loss surgery may have trouble getting enough vitamins and minerals. This is because they take in less food, and may absorb fewer nutrients. You may need to take a daily multivitamin, plus a calcium-vitamin D supplement. You may need additional nutrients, such as vitamin B-12 or iron. Your medical team will give you instructions.
You’ll need to have regular blood tests every few months in the year after surgery. This is to make sure you don’t have low blood iron (anemia), high blood glucose, or low calcium or vitamin D levels. If you have heartburn, you may need to medicine to reduce stomach acid.
After losing weight, it’s possible to regain some of the weight that you lose. To avoid this, make sure to follow a healthy diet and get regular exercise. The sleeve may widen (dilate) over time. This will let you eat more. But keep in mind that if you eat all you can, you can regain weight. You may want to join a weight-loss surgery support group to help you stick with your new eating habits.
You will also have to, and be able to, increase the amount of physical activity you do.
Vertical sleeve gastrectomy results
Sleeve gastrectomy can provide long-term weight loss. The amount of weight you lose depends on your change in lifestyle habits. It is possible to lose approximately 60 percent, or even more, of your excess weight within two years.
In addition to weight loss, sleeve gastrectomy may improve or resolve conditions related to being overweight, including:
- Heart disease
- High blood pressure
- High cholesterol
- Obstructive sleep apnea
- Type 2 diabetes
- Stroke
- Infertility
Sleeve gastrectomy surgery can also improve your ability to perform routine daily activities, and can help improve your quality of life.
When sleeve gastrectomy doesn’t work
It’s possible to not lose enough weight or to regain weight after sleeve gastrectomy surgery. This weight gain can happen if you don’t follow the recommended lifestyle changes. If you frequently snack on high-calorie foods, for instance, you may have inadequate weight loss. To help avoid regaining weight, you must make permanent healthy changes in your diet and get regular physical activity and exercise.
It’s important to keep all of your scheduled follow-up appointments after weight-loss surgery so your doctor can monitor your progress. If you notice that you aren’t losing weight or you develop complications after your surgery, see your doctor immediately.