What is gout?
Gout is a type of arthritis that leads to painful inflammation in a joint. Gout causes sudden and severe joint pain that usually starts in your big toe, but gout can also affect your hands, wrists, knees, ankles, feet, elbows or any other joints. Urate crystals may also be deposited throughout the body (e.g., vertebrae, skin, soft tissues), mimicking other disease states 1. Gout is the most common type of inflammatory arthritis. Men are three times more likely than women to develop gout. It tends to affect men after age 40 and women after menopause. Gout symptoms can be confused with another type of arthritis called calcium pyrophosphate deposition (pseudogout or CPPD). However, the crystals that irritate the joint in pseudogout are calcium phosphate crystals, not uric acid. However, it is caused by calcium phosphate, not uric acid. Pseudogout has similar symptoms and is sometimes confused with gout. In other words, both gout and pseudogout have such similar symptoms that it usually takes a microscope to know for sure what you’ve got. The big difference is that gout is a treatable disease. If it can be diagnosed and treated properly, gout can go away completely.
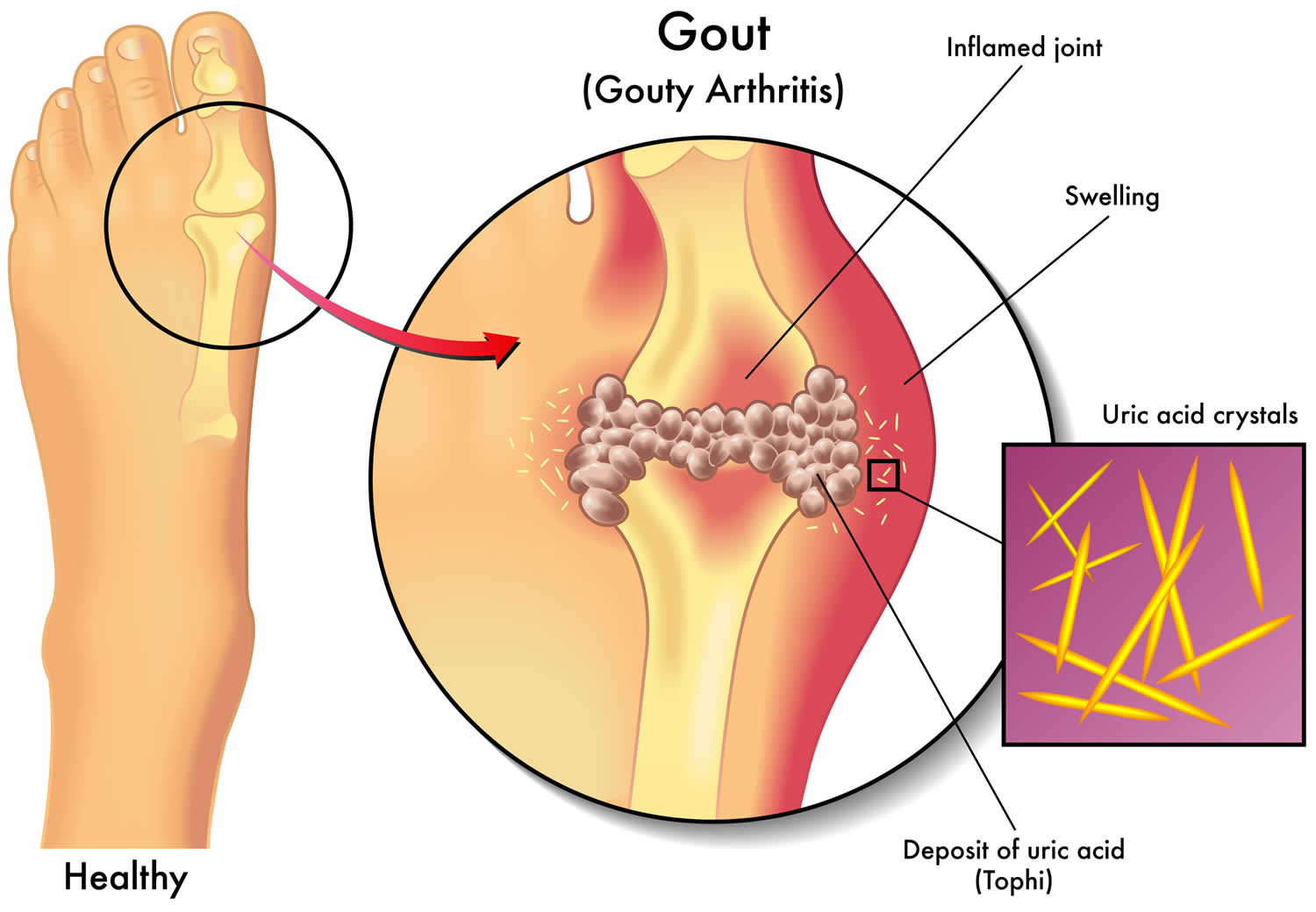
Gout is caused by high uric acid levels (currently defined as a value of at least 6.8 mg per dL or 405 μmol per L), which builds up in your body causing monosodium urate crystals to form in and around your joint, resulting in inflammation and joint damage 2. Uric acid comes from the breakdown of substances called purines. Purines are in your body’s tissues and in foods, such as liver, dried beans and peas, and anchovies. In any day, about three-quarters of the urate in your body comes from the breakdown of purines produced within your body, while only about a quarter comes from the breakdown of purines in food and drink you consume. Normally, uric acid dissolves in your blood. It passes through the kidneys and out of your body in your urine. But sometimes uric acid can build up and form needle-like crystals. They mainly occur in and around firm joint tissues, such as the cartilage. But urate crystals can also appear under your skin and may even occur in your internal organs, such as the kidneys. When they form in your joints, it is very painful. The crystals can also cause kidney stones.
Gout usually presents with an abrupt onset of a red, hot, swollen, painful joint, most often in your big toe, but less frequently in your foot, ankle, knee, wrist, elbow or finger; usually confined to just one joint in early disease. Gout symptoms may come and go, at first, gout attacks usually get better in days. Eventually, attacks last longer and happen more often, but there are ways to manage your symptoms and prevent flares.
If you experience sudden, intense pain in a joint, see your doctor. Gout that goes untreated can lead to worsening pain and joint damage. Seek medical care immediately if you have a fever and a joint is hot and inflamed, which can be a sign of joint infection (septic arthritis).
You are more likely to get gout if you:
- Are a man
- Have family member with gout
- Are overweight
- Drink alcohol
- Eat too many foods rich in purines
Gout can be hard to diagnose. Your doctor may take a sample of fluid from an inflamed joint to look for crystals. You can treat gout with medicines.
For gout flare up or acute attack treatment your doctor may prescribe nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids and colchicine. Gout disease management may include dietary changes and uric-acid lowering drugs to prevent future attacks. You should avoid eating high-purine foods. Try to limit the amount of moderate-purine foods you eat.
With the proper treatment, your gout attack should go away in a few days. If left untreated, it can last for several days or weeks.
Talk to your doctor if you continue to have gout attacks. The more frequent they are, the longer they can last and the more joints it can affect. Your doctor can prescribe medicines to help prevent future gout attacks. These medicines wash the uric acid from your joints, lower the level in your body, and reduce swelling. Aspirin can interfere with the way these medicines work. Work with your doctor on a treatment plan to manage gout. You may need routine visits to check your uric acid level.
Over time, gout attacks can lead to tophi. These are uric acid crystals that form lumps under your skin. Tophi can form on your toes, fingers, hands, and elbows. They cause chronic pain and can destroy the bones around your joints. You also may develop kidney stones or kidney disease from uric acid crystals that collect in your urinary tract.
Gout key points:
- Intensely painful, swelling joints (most often in your big toe or other part of your foot) and/or bouts of arthritis that come and go may indicate gout.
- The symptoms of gout may be sudden and often start at night. The affected joint swells and becomes red, hot, and painful. The joint may become stiff and hurt more when you touch it.
- Finding the characteristic uric acid crystals in the fluid of joints allows health care providers to correctly diagnose gout.
- Gout can be acute (short-lasting) or chronic (long-lasting). An acute attack of gout lasts 3 to 10 days on average. Chronic gout occurs more often, but may be less severe.
- Men develop gout more often than women. Women are more likely to develop gout after menopause.
- Too much uric acid in your body causes gout. Uric acid forms naturally when your body breaks down purines. Purines also are found in some foods you eat. Purines aren’t all bad, but you want to avoid high amounts. When your body digests purine, it produces a waste product called uric acid. Normally, uric acid dissolves in your blood and passes through your kidneys into your urine. In people who have gout, uric acid builds up and forms sharp crystals in their joint space. Gout is also genetic and can run in families. Stress, poor diet, alcohol use, and other health problems can trigger gout attack.
- Gout is a red flag for associated cardiovascular risk factors. A patient with gout has been shown in a broad range of studies to be at higher risk of coronary artery disease and should have an evaluation appropriate to coronary risk (for example, lab testing for cholesterol and triglyceride level) 3.
- Gout treatments exist, but therapy should be tailored for each person. Treatment choices depend on kidney function, other health problems, personal preferences and other factors.
- Treatment for gout attack should be instituted quickly, since quick treatment can often be rewarded with a quick improvement. If an attack of gout is allowed to last more than a day or so before treatment is started, the response to treatment may be much slower.
- Local ice has been shown to help (for not more than 10 minutes at a time, to avoid skin damage). Leg elevation is helpful for some.
- Patients may need medications to lower their elevated blood uric acid levels that predispose to gout.
- Gout treatment aims for a uric acid level of 6 mg/dL or lower to dissolve or prevent crystals.
- There are two types of medicine for gout. For control of acute attacks of joint pain, there are NSAIDs, colchicine and corticosteroids. After gout flares have resolved, there are medications that can lower the level of uric acid over time in order to prevent or lessen attacks.
- Lifestyle changes such as controlling weight, limiting alcohol intake and limiting meals with meats and fish rich in purines also can help control gout.
Figure 1. Gout in foot (big toe with acute gout attack)
Footnote: When gout occurs, the joint tends to be extremely painful and is warm, red and swollen. Since gout attacks are usually quite painful and often make walking difficult, most gout sufferers will request specific treatment for their painful condition.
Figure 2. Gout in knee
Figure 3. Gouty tophi finger
Footnote: Gout attacks can occur in joints that look normal, or in joints that have easily visible deposits of uric acid. These deposits are called tophi and can be in numerous locations, but especially on the feet and elbows. Tophi are subcutaneous nodules comprised of monosodium urate crystals in a matrix of lipids, protein, and mucopolysaccharides and may also form at the joint space.
[Source 4 ]Figure 4. Gouty tophi toe
Who gets gout?
Gout can develop in a person either because they are producing too much uric acid or because they are unable to put enough of it into the urine (or both). The most common cause of gout (about 90% of cases) is the inability to excrete enough uric acid in the urine. This inability may occur for a number of reasons. The most common is a genetic defect in substances referred to as organic anion transporters in the kidney, which leads to an excessive reabsorption of uric acid from the kidney – and thus too much uric acid in the blood. However, a defect in excretion of uric acid can also occur due to medications, such as diuretics, low dose aspirin, or alcohol. Defective uric acid excretion also occurs when the kidneys are functioning poorly.
About 10% of cases of gout are due to overproduction of uric acid. When uric acid is overproduced, it is high not only in the blood but in the urine, raising the risk of both gout and kidney stone. Some people overproduce uric acid due to a genetic defect in an enzyme in the purine breakdown pathway (See Figure 4) which leads to overactivity of this pathway. Since cells contain DNA, and DNA contains purines, anything that increases the breakdown of cells in the body can lead to more uric acid and gout. For example, if a patient is receiving chemotherapy for a tumor, as the treatment kills the tumor cells a gout attack or kidney stone can develop as a result of the breakdown of the purines from those cells.
Foods can also lead to overproduction of uric acid, such as meats and meat gravies and beer, which contain high levels of purines.
Men get gout more than women, and at younger ages; the male to female ratio is 9:1. The most common age of onset is from age 40 to 60 years. Gout is fairly rare in women until they reach menopause. One theory is that estrogen blocks the anion exchange transporter (see above) in the kidney, causing more uric acid to be excreted in the urine, and thus lowering the level of uric acid in the blood. Gout most commonly starts in a person’s 40’s to 60’s, although it can start earlier than the 40’s for those with a genetic predisposition, and it can also occur for the first time when someone is in their 80’s.
In some cases, injuries can set off an attack of gout. A “stub of the toe” can lead to a gout attack if there were already enough uric acid crystals saturating the cartilage.
Whatever the mechanism of the elevated uric acid, the key event in gout is the movement of uric acid crystals into the joint fluid. The body’s defense mechanisms, including the white blood cells (neutrophils) engulf the uric acid crystals, which leads to a release of inflammatory chemicals (called cytokines) which cause all the signs of inflammation, including heat, redness, and swelling and pain. This cycle also recruits more white blood cells to the joint, which accelerates the inflammatory process.
When thinking of gout, a useful model has been proposed by Wortmann 5. Uric acid crystals can be thought of like matches, which can sit quietly or can be ignited. Crystals can be present for years in the cartilage, or even in the joint fluid, without causing inflammation. Then, at some point, due to increasing number of crystals or other inciting factor, the matches are “struck” and the inflammation begins. This analogy is important both for conceptualizing the uric acid crystals in the joint and for understanding the various types of gout treatment (see below), some of which attack the inflammation (pour water on the flaming matches) and some of which remove the uric acid crystals (take away the matches).
Will gout go away by itself?
A gout flare up will go away by itself, but it will take around 2 weeks and be very painful. The other problem is that recurrent untreated gout flare ups can lead to permanent joint damage, so it is best to take medication for gout attacks. This not only greatly reduces how many days you’ll will be in pain, but also reduces the chances of joint damage.
Some people with gout experience recurrent attacks, which may be prevented by using prescription medications. These medicines work by lowering uric acid levels in the blood. The most commonly used is allopurinol. This helps to lower uric acid levels by reducing the body’s production of uric acid. It is likely they’ll need to take gout-preventing medication for life. Some people do however come off medication successfully, in particular if they’ve addressed the things that were putting them at risk of gout (i.e. they’ve lost weight, changed their diet) and they’ve had a normal blood uric acid level for years.
You can also reduce your chance of having further attacks of gout by adopting some sensible lifestyle changes, such as:
- reducing alcohol intake — avoid binge drinking, in particular (see alcohol.gov.au for Australian Government guidelines on recommended alcohol intake)
- gradually losing weight if you are overweight, while avoiding fad diets
- eating a healthy, balanced diet
- drinking plenty of water, especially when at risk of dehydration (e.g. when you are sick or travelling in a plane)
What is normal uric acid level
- Normal values range between 3.5 to 7.2 milligrams per deciliter (mg/dL).
- Normal urine uric acid levels range from 250 to 750 milligrams per 24 hours (1.48 to 4.43 millimoles per 24 hours).
Normal value ranges may vary slightly among different laboratories. Some labs use different measurements or test different samples. Normal serum urate levels do not exclude the diagnosis of gout. Talk to your doctor about the meaning of your specific test results.
Which joints are involved in gouty arthritis, and why is it most common in the foot?
As with all other known types of arthritis, gout has particular joints it tends to attack and the foot is its most common location. Gout especially favors the bunion joint, known as the first metatarsophalangeal joint (at the base of the big toe), but the ankle, midfoot and knee are also common locations, as is the bursa that overlies the elbow.
The bunion joint is the first joint involved in 75% of patients and is ultimately involved in over 90% of those with this condition. It is thought that this joint is especially involved in gout because it is the joint that receives the highest pounds per square inch of pressure when walking or running.
Late in gout, if untreated, multiple joints can be involved, including the fingers and wrists. The shoulder joint is very rarely involved by gout and the same is true of the hip.
What is gouty tophi?
Gouty tophi are deposits of uric acid or monosodium urate monohydrate crystals that form lumps below the skin around joints or other places such as the elbows, fingers, hands, feet, Achilles tendons along the backs of your ankles and ears. You can sometimes see the white color of the urate crystals under the skin. Tophi usually aren’t painful, but they can become swollen and tender during gout attacks. They can sometimes become inflamed, break down and leak pus-like fluid with gritty white material – these are the urate crystals.
The most common areas for gouty tophi are:
- over the top of the toes
- back of the heel
- front of the knee
- backs of the fingers and wrists
- around the elbow
- the ears.
Tophi can also grow within your joints and cause damage to your cartilage and bone. This can lead to more regular, daily pain when you use the affected joints.
Gout signs and symptoms
The signs and symptoms of gout almost always occur suddenly, and often at night. Gout is characterized by sudden, severe attacks of pain, swelling, redness and tenderness in one or more joints, most often in your big toe.
The symptoms of gout include:
- Intense pain in a joint, which can be quite severe. Gout usually affects your big toe, but it can occur in any joint. Other commonly affected joints include the ankles, knees, elbows, wrists and fingers. The pain is likely to be most severe within the first four to 12 hours after it begins.
- Lingering discomfort. After the most severe pain subsides, some joint discomfort may last from a few days to a few weeks. Later attacks are likely to last longer and affect more joints.
- Inflammation and redness. The affected joint or joints become swollen, tender, warm and red.
- Restricted movement of the joint. As gout progresses, you may not be able to move your joints normally.
Signs of gout include
In over three quarters of people with gout, their first ever episode tends to be in the big toe. The typical signs include:
- Severe pain in the joint
- Swollen joint
- Red or hot joint
An attack of gout can occur suddenly, often waking you up in the middle of the night with the sensation that your big toe is on fire. The affected joint is hot, swollen and so tender that even the weight of the bedsheet on it may seem intolerable. These symptoms usually develop rapidly and can last for 1 to 2 weeks.
A red, warm, painful and swollen big toe joint in a man aged over 40 usually points to gout. However, that could also indicate an infection in the joint or bone, or an unusual condition known as ‘pseudogout’.
Furthermore, sometimes it can be hard to differentiate gout from an infected joint. Infected joints often require urgent medical treatment, so anyone with a painful joint as well as a high fever or that’s generally feeling unwell, should see a doctor as soon as possible.
Gout stages
Gout is best understood by seeing it as having four phases or stages.
- Stage 1: High uric acid. Elevated uric acid without gout or kidney stone, this stage has no symptoms and is generally not treated.
- Stage 2: Acute flares. This stage is marked by acute gout attacks causing pain and inflammation in one or more joints.
- Stage 3: Intercritical periods. These are periods of time between acute attacks, during which a person feels normal but is at risk for recurrence of acute attacks.
- Stage 4: Advanced gout. This is a stage of chronic gouty arthritis, in which there are “lumps” of uric acid, or tophi, frequent attacks of acute gout, and often a degree of pain even between attacks.
Gout complications
People with gout can develop more-severe conditions, such as:
- Recurrent gout. Some people may never experience gout signs and symptoms again. Others may experience gout several times each year. Medications may help prevent gout attacks in people with recurrent gout. If left untreated, gout can cause erosion and destruction of a joint leading to a condition known as osteoarthritis.
- Advanced gout. Untreated gout may cause deposits of urate crystals to form under the skin in nodules called tophi. Tophi can develop in several areas, such as your fingers, hands, feet, elbows or Achilles tendons along the backs of your ankles. Tophi usually aren’t painful, but they can become swollen and tender during gout attacks.
- Kidney stones. Urate crystals may collect in the urinary tracts of people with gout, causing kidney stones. Medications can help reduce the risk of kidney stones.
- An increased risk of developing kidney disease or worsening of the kidney condition if you already have it
- A patient with gout has been shown in a broad range of studies to be at higher risk of coronary artery disease, and should have an evaluation appropriate to coronary risk (for example, lab testing for cholesterol and triglyceride level) 3. Having high urate levels and gout for a long time can lead to narrowing of your arteries, which can lead to an increased risk of stroke or heart attacks or other heart problems.
- An increased risk of some cancers, especially prostate cancer
- Mental health problems, including depression
- Underactive thyroid (hypothyroidism)
- Erectile dysfunction in men.
- Gout might also cause ocular complications, such as conjunctivitis, uveitis, or scleritis from the urate crystal precipitation 6.
It is important that damage to bone from gout be diagnosed, since documented damage is a clear indication for long-term therapy. Once damage has begun, it’s important to reduce the total body uric acid level, which, by equilibration, causes uric acid to move out of the joints. This is because the blood and joint levels of uric acid reach a certain level, called a “steady state,” at a given level of blood uric acid. If the blood level is reduced, then the joint level of uric acid will gradually decrease as well. This leads to gout attacks diminishing or completely ceasing over time, and to tophi getting reabsorbed and shrinking or fully disappearing.
Gout causes
Gout is caused by a build-up of uric acid, a normal waste product typically found in the blood. Your body produces uric acid when it breaks down purines — substances that are found naturally in your body. Purines are also found in certain foods, including red meat and organ meats, such as liver. Purine-rich seafood includes anchovies, sardines, mussels, scallops, trout and tuna. Alcoholic beverages, especially beer, and drinks sweetened with fruit sugar (fructose) promote higher levels of uric acid.
Uric acid can build up either because your kidneys do not excrete it quickly enough, or because too much is being produced. The excess can form crystals in the joints (known as ‘urate’ crystals). Gout occurs when these crystals cause sudden and severe inflammation of the join and the intense pain a gout attack.
Normally, uric acid dissolves in your blood and passes through your kidneys into your urine. But sometimes either your body produces too much uric acid or your kidneys excrete too little uric acid. When this happens, uric acid can build up, forming sharp, needlelike urate crystals in a joint or surrounding tissue that cause pain, inflammation and swelling.
Genetic mutations may be associated with overproduction or more often underexcretion of uric acid because of defects in the renal urate transporter system 7. Genome-wide association studies (GWAS) have found several genes that are associated with gout. These include SLC2A9, ABCG2, SLC22A12, GCKR, and PDZK1 8.
Gout triggers
Every condition that causes alterations in extracellular urate concentration has the potential to trigger a gout flare-up. These conditions include stress (surgical procedure, recent trauma or starvation), dietary factors (e.g., fatty food, beer, wine, and spirits), and drugs (e.g., aspirin, diuretics, or even allopurinol) 9.
Several things can cause the urate crystals to shake loose into your joint cavity, triggering an attack. These include:
- a knock or injury to the joint
- an illness that may make you feverish
- having an operation
- having an unusually large meal, especially a fatty meal
- drinking too much alcohol
- dehydration
- starting urate lowering therapy, especially at a high dose, or not taking your treatment regularly each day.
Risk factors for developing gout
You’re more likely to develop gout if you have high levels of uric acid in your body. Factors that increase the uric acid level in your body include:
- Being male and being older. Gout occurs more often in men, primarily because women tend to have lower uric acid levels. Female sex hormones increase urinary excretion of uric acid, pre-menopausal women have a substantially lower prevalence of gout compared with men (2.0% vs. 5.9%) 7. After menopause, however, women’s uric acid levels approach those of men. Men are also more likely to develop gout earlier — usually between the ages of 30 and 50 — whereas women generally develop signs and symptoms after menopause. The prevalence of gout increases with age and peaks at more than 12% in persons older than 80 years 10.
- Having close family members who have had gout. If other members of your family have had gout, you’re more likely to develop the disease.
- Having high levels of uric acid in the blood
- Being dehydrated
- Taking medications that increase water excretion by the kidneys (diuretics). Diuretics can increase your risk of developing gout because diuretics increase urination, which reduces the amount of fluid in your body causing dehydration. But the remaining fluid is more concentrated, which can increase the risk that you’ll develop the crystals that cause gout. Some types of diuretics also reduce the kidneys’ excretion of urate, a component of uric acid.
- Certain medications. Low-dose aspirin and some medications used to control hypertension — including thiazide diuretics, angiotensin-converting enzyme (ACE) inhibitors and beta blockers — also can increase uric acid levels. So can the use of anti-rejection drugs prescribed for people who have undergone an organ transplant.
- Being overweight. If you’re overweight, your body produces more uric acid and your kidneys have a more difficult time eliminating uric acid.
- Eating a diet with a lot of meat, offal and shellfish. Eating a diet rich in red meat and shellfish (shrimp and lobster) and drinking beverages sweetened with fruit sugar (fructose) increase levels of uric acid, which increase your risk of gout.
- Having kidney disease, high blood pressure, diabetes or abnormal levels of fat and cholesterol in the blood.
- Drinking a lot of alcohol, especially beer, port or spirits. Alcohol consumption, especially of beer, also increases the risk of gout.
- Going on a crash diet or fasting.
- Recent surgery or trauma. Experiencing recent surgery or trauma can sometimes trigger a gout attack. In some people, receiving a vaccination can trigger a gout flare.
- Being of Black, Taiwanese, Pacific Islander, and New Zealand Maori origin, which can predispose a person to high uric acid levels 11
Gout is more common in men than in women, and among women it’s more common after menopause. It’s more likely to occur in older people, but can affect anyone.
It can also affect people with certain types of blood disorder (such as the blood cancers leukemia and lymphoma) and people in treatment for cancer.
Foods that cause gout
Purines are a natural substance found in some foods. Purines aren’t all bad, but you want to avoid high amounts. When your body digests purine, it produces a waste product called uric acid. A buildup of uric acid crystals in the joints can cause certain health issues. The main ones are kidney stones and a type of arthritis known as gout.
Foods which you should try to avoid having large quantities of include:
- red meat and offal such as liver, kidneys and heart
- seafood, especially shellfish, scallops, mussels, herring, mackerel, sardines and anchovies
- foods containing yeast such as Vegemite, Marmite, Bovril, and beer
Drinking too much alcohol, especially beers and spirits, may increase urate levels.
People react to food in different ways. Over time, you will learn what foods affect you. You might find that certain foods make your gout or other health issues affected by high purine levels flare up. This practice allows you to avoid those foods and enjoy others.
A low-purine diet can reduce your symptoms. However, dietary changes alone do not get rid of gout and similar medical conditions. It’s best to seek the advice of your doctor or an accredited practising dietitian before making any changes to your diet. Most people with gout find that a healthy, balanced diet — along with medication — is enough to reduce their uric acid levels.
It’s also important not to lose weight too quickly. Rapid weight loss and fasting actually can increase the amount of uric acid in your body. Discuss the diet plan with your doctor before starting. Check in with them to manage progress and health issues.
Gout prevention
There are several ways you can help lower your risk of gout and prevent future gout attacks and diet plays a key role diet in gout prevention. Your doctor may recommend that you follow a low-purine diet. This applies if you have gout or kidney stones. It also can help people who have high blood uric acid levels (hyperuricemia). This is a condition caused by high levels of uric acid. You also can choose to keep a low-purine diet as part of living healthy.
- Dietary control may be sufficient in a patient with mildly elevated uric acid, for example, 7.0 mg/dL (noting that any uric acid level above 6.0 mg/dL is considered elevated for a patient with gout, even if within what the lab calls the “normal range.”)
- For those with a higher uric acid level, for example, 10.0 mg/dL, diet alone will not usually prevent gout. For the latter, even a very strict diet only reduces the blood uric acid by about 1 mg/dL- not enough, in general, to keep uric acid from precipitating in the joints. The cutoff where patients with gout seem to dramatically reduce their number of attacks is when their uric acid level is taken below 6.0 mg/dL 12.
Serum urate–lowering therapy should be initiated to prevent recurrences in persons with a history of gout and any one of the following: at least two flares per year (one per year in persons with chronic kidney disease stage 2 or greater), tophi, or a history of kidney stone (nephrolithiasis) 13.
Serum urate should be lowered to a target of less than 5 to 6 mg per dL (297 to 357 μmol per L), depending on the crystal and tophaceous burden 13. Normal serum urate levels do not exclude the diagnosis of gout. They should be monitored periodically to assess preventive therapy in patients with recurrent gout and a history of elevated urate levels 14. Urate-lowering therapy should be continued for three to six months after a flare if there are no ongoing symptoms. Therapy should continue indefinitely if there are ongoing signs or symptoms (e.g., one or more tophi on examination) 13.
With the above qualifications, attention to diet in gout patients is helpful, and especially so when first starting medication to lower the uric acid (which may, paradoxically, initially set off gout attacks). There are a few basic principles of diet in gout which have stood up to a variety of studies: drink lots of water, limit sugary drinks, limit red meat and meat gravies, limit shellfish, and avoid alcohol, especially beer to help reduce uric acid buildup 15, 16. All types of alcohol cause more uric acid to be reabsorbed by the kidneys, raising blood uric acid levels, but beer has its own high purine level and so contributes to blood uric acid elevation in two different ways. Red meat and shellfish (for example, scallops, shrimp, and mussels) should, ideally, be eaten less frequently, in smaller portions (for example, 3 oz). Vegetable protein is broken down to purine, but does not seem to be a significant contributing factor in gout. Low fat dairy products, despite mild protein being broken down to purine, likewise seems not to contribute to gout risk (and may even be protective) 15. Certain carbohydrates, such as oatmeal, wheat germ, and bran have moderate purine content but have not been shown to be significant gout risk factors.
An exercise program combined with diet in gout can reduce risk for attacks 17. If an attack seems to be coming on in the lower extremity, patients are well-advised to try to get off their feet, since impact seems to worsen gout attacks. Clues to an attack of gout coming on include local swelling, heat, redness, and tenderness in a joint, especially in the foot, ankle, or knee. Some patients have fever and chills as the first warning that an attack of gout is coming on.
Measures that you can take to lower uric acid include:
- Eating a healthy and balanced diet with an emphasis on vegetables, fruits, plant proteins, low-fat dairy products and whole grains, and reduced servings of meat and seafood. Purine-rich vegetables do not increase the risk of gout 18. Consumption of vegetables and low-fat or nonfat dairy products should be encouraged 18. Try to eat foods that are low in salt and fat.
- Limit or avoid foods that are rich in purines. Common purine-rich foods include red meats and organ meats (liver, kidney, tongue, and sweetbreads), salmon, sardines, mackerel, herring and game meats.
- Limit the amount of alcohol you drink.
- Drink lots of water to help flush uric acid from your body.
- Limiting beverages that are sugar sweetened and limiting foods and beverages that contain high fructose corn syrup. Intake of high-fructose corn syrup should be restricted 20, because the fructose contributes to increased uric acid production as a byproduct of adenosine triphosphate catabolism 21.
- Losing weight and maintaining a healthy weight based on your body mass index
To help manage gout, it’s also important to stay hydrated by drinking plenty of water. Each day, drink 8 to 16 eight-ounce cups of liquid. At least half of the liquid you drink should be water. Water and other liquids help your body get rid of uric acid. You can also limit your intake of foods rich in the compound purine, which form uric acid when they are broken down. Common purine-rich foods include liver, mackerel, herring, game meats and sardines.
Certain health conditions can increase your chance of gout. Get treatment if you have high cholesterol, high blood pressure, or diabetes. Medicines that may cause gout include:
- Diuretics (“water pills”) used to treat high blood pressure
- Niacin (a B-complex vitamin)
- Aspirin (taken in low doses)
- Cyclosporine (used to prevent the body from rejecting a new organ after transplant surgery)
- Some drugs used to treat cancer
- Pyrazinamide and ethambutol (used to treat tuberculosis)
Gout diet
Eat a healthy and balanced diet that includes plenty of vegetables, fruits, fiber and whole grains, as well as low-fat or fat-free dairy products, poultry, and oils. Limiting foods high in saturated fats, as well as sugar-sweetened foods and drinks.
Extreme weight loss or starvation diets increase cell breakdown in your body, which can raise urate levels. However, you should be OK to do some daytime fasting.
Research has shown that vitamin C may slightly reduce uric acid levels in people with gout. This is another reason to make sure your diet includes plenty of fruit and vegetables. But if you’re considering taking vitamin C supplements, talk to your doctor first, as there’s a very slight risk that vitamin C supplements could interact with other medications.
Cherry products such as whole cherries or unsweetened cherry juice may reduce gout flares.
Research also suggests drinking skimmed milk and eating low-fat yoghurt may help to prevent attacks of gout.
A low-purine diet is an eating plan that limits foods with high purine. Purines are a natural substance found in some foods. Purines aren’t all bad, but you want to avoid high amounts. When your body digests purine, it produces a waste product called uric acid. A buildup of uric acid crystals in the joints can cause certain health issues. The main ones are kidney stones and a type of arthritis known as gout.
The purpose of a low-purine diet is not to fully avoid purines. Instead, the goal is to manage how much purine you consume. Below, you will find what types of food and drink to avoid and limit. It helps to learn how your body responds to foods that contain purine.
The general principles of a gout diet are essentially the same as recommendations for a balanced, healthy diet:
Avoid
- eating a lot of red meat, kidneys, liver or seafood
- drink more than 14 units of alcohol a week
- eating sugary drinks and snacks
- eating full-fat dairy products
- eating more than 2 servings of low-fat dairy foods a day
Proteins. Limit daily proteins from lean meat, fish and poultry to 4 to 6 ounces (113 to 170 grams). Add protein to your diet with low-fat or fat-free dairy products, such as low-fat yogurt or skim milk, which are associated with reduced uric acid levels.
Complex carbs. Eat more fruits, vegetables and whole grains, which provide complex carbohydrates. Avoid foods such as white bread, cakes, candy, sugar-sweetened beverages and products with high-fructose corn syrup.
Water. Keep yourself hydrated by drinking water. An increase in water consumption has been linked to fewer gout attacks. Aim for eight to 16 glasses of fluids a day with at least half of that as water. A glass is 8 ounces (237 milliliters). Talk to your doctor about appropriate fluid intake goals for you.
Fats. Cut back on saturated fats from red meats, fatty poultry and high-fat dairy products.
Recommendations for specific foods or supplements include the following:
- High-purine vegetables. Studies have shown that vegetables high in purines do not increase the risk of gout or recurring gout attacks. A healthy diet based on lots of fruits and vegetables can include high-purine vegetables, such as asparagus, spinach, peas, cauliflower or mushrooms. You can also eat beans or lentils, which are moderately high in purines but are also a good source of protein.
- Organ and glandular meats. Avoid meats such as liver, kidney and sweetbreads, which have high purine levels and contribute to high blood levels of uric acid.
- Selected seafood. Avoid the following types of seafood, which are higher in purines than others: anchovies, herring, sardines, mussels, scallops, trout, haddock, mackerel and tuna.
- Alcohol. The metabolism of alcohol in your body is thought to increase uric acid production, and alcohol contributes to dehydration. Beer is associated with an increased risk of gout and recurring attacks, as are distilled liquors to some extent. The effect of wine is not as well-understood. If you drink alcohol, talk to your doctor about what is appropriate for you.
- Vitamin C. Vitamin C may help lower uric acid levels. Talk to your doctor about whether a 500-milligram vitamin C supplement fits into your diet and medication plan. Talk to your doctor about what a reasonable dose of vitamin C may be. And don’t forget that you can increase your vitamin C intake by eating more vegetables and fruits, especially oranges.
- Coffee. Some research suggests that moderate coffee consumption may be associated with a reduced risk of gout, particularly with regular caffeinated coffee. The available evidence isn’t enough to encourage noncoffee drinkers to start, but it may give researchers clues to new ways of treating gout in the future. Plus drinking coffee may not be appropriate for other medical conditions. Talk to your doctor about how much coffee is right for you.
- Cherries. There is some evidence that eating cherries is associated with a reduced risk of gout attacks. However, more research needs to be done to confirm this. Eating more cherries and drinking cherry extract may be a safe way to supplement your gout treatment, but discuss it with your doctor first.
Table 1. Gout diet
| Avoid high-purine foods | Limit moderate-purine foods | Enjoy low-purine foods |
|---|---|---|
| Wild game, like veal, venison, and duck | Meat and poultry | Peanut butter and nuts |
| Anchovies, sardines, herring, mussels, codfish, scallops, trout, tuna, and haddock | Crab, lobster, oysters, and shrimp | Low-fat and fat-free dairy products, such as milk, cheese, and yogurt |
| Organ meats, such as liver, kidneys, and sweetbreads | Lunch meats, especially high-fat versions | Eggs (in moderation) |
| Foods high in fat (red meats, fatty poultry—dark meats and skin, high-fat dairy products) | Beans, peas, and lentils | Fat and oil |
| Gravy | Vegetables, such as spinach, cauliflower, asparagus, and mushrooms | Other vegetables |
| Yeast | Oatmeal and oats | Potatoes, bread, rice, and pasta |
| Beer | Liquor | Wine (in moderation) |
| Fruits and fruit juices | ||
| Coffee (in moderation) |
Gout diagnosis
Doctors usually diagnose gout based on your symptoms and the appearance of the affected joint. Tests to help diagnose gout may include:
- Joint fluid test. Your doctor may use a needle to draw fluid from your affected joint. Urate crystals may be visible when the fluid is examined under a microscope.
- Blood test. Your doctor may recommend a blood test to measure the levels of uric acid in your blood. Blood test results can be misleading, though. Some people have high uric acid levels, but never experience gout. And some people have signs and symptoms of gout, but don’t have unusual levels of uric acid in their blood.
- X-ray imaging. Joint X-rays can be helpful to rule out other causes of joint inflammation.
- Ultrasound. This test uses sound waves to detect urate crystals in joints or in tophi.
- Dual-energy computerized tomography (DECT). This test combines X-ray images taken from many different angles to visualize urate crystals in joints.
Since the treatment for gout is lifelong, it’s very important to make a definitive diagnosis. Ideally, gout diagnosis is made by identifying uric acid crystals in joint fluid or in a mass of uric acid (tophus). These can be seen by putting a drop of fluid on a slide and examining it using a polarizing microscope, which takes advantage of the way uric acid crystals bend light. A non-rheumatologist, when possible, can remove fluid from the joint by aspirating it with a small needle and send it to a lab for analysis. A rheumatologist is likely to have a polarizing attachment on their microscope at their office. Gout crystals have a needle-like shape, and are either yellow or blue, depending on how they are arranged on the slide (see Figure 5: Uric Acid Crystals Under Polarizing Light Microscopy).
The American College of Rheumatology criteria are the most widely used for diagnosis of gout (Table 2) 22.
Table 2. American College of Rheumatology Diagnostic Criteria for Gout
| Presence of characteristic urate crystals in the joint fluid | |
| or | |
| Presence of a tophus proven to contain urate crystals by chemical means or polarized light microscopy | |
| or | |
| Presence of six or more of the following clinical, laboratory, or radiologic findings: | |
| Asymmetric swelling within a joint on radiography | |
| Attack of monoarticular arthritis | |
| Culture of joint fluid negative for microorganisms during attack of joint inflammation | |
| Development of maximal inflammation within one day | |
| Hyperuricemia | |
| Joint redness | |
| More than one attack of acute arthritis | |
| Pain or redness in the first metatarsophalangeal joint | |
| Subcortical cyst without erosions on radiography | |
| Suspected tophus | |
| Unilateral attack involving first metatarsophalangeal joint | |
| Unilateral attack involving tarsal joint | |
There are many circumstances where, however ideal it would be, no fluid or other specimen is available to examine, but a diagnosis of gout needs to be made. A set of criteria has been established to help make the diagnosis of gout in this setting (see list below – Diagnosis of Gout When No Crystal Identification Possible). The diagnosis of gout is made in the presence of 6 of the 10 criteria listed below.
Diagnosing gout when no crystal identification is possible
Ideally, 6 of 10 features will be present of the following 23:
- Inflammation reaches a maximum within one day (rapid acceleration of inflammation).
- Having a history of similar episode of inflammation
- Attack of arthritis in a single joint.
- Redness over an involved joint (gout is highly inflammatory)
- Involvement of the base of the big toe on one side (the most common site for gout)
- Involvement of the joints at the middle of the foot
- Uric acid elevation on blood testing
- X-ray findings of swelling of joints which is not symmetrical
- Joint fluid is tested for infection and is negative.
- X-ray shows characteristic changes of gout, including cysts in bone and erosions.
The red and hot joints, coupled with rapid acceleration of joint pain, strongly suggest gout, and identifying tophi, if present (see Figures 3 and 4) help further.
Special effort should be made to distinguish gout from the other crystal-induced types of arthritis. For example, pseudogout, caused by a different type of crystal (calcium pyrophosphate), causes the same type of hot, red joint, and the same rapid acceleration of pain as does gout. Pseudogout can be distinguished by seeing calcium deposits within the joints on X-ray, which deposits in a different way than it does in gout. When fluid is examined from an inflamed joint in pseudogout, the specific causative crystal can be seen. Findings of calcium pyrophosphate crystals and normal serum uric acid levels on joint fluid analysis can differentiate pseudogout from gout.
A third type of crystal-induced arthritis, hydroxyapatite deposition disease, has a type of crystal that needs special studies (one such study is electron microscopy) for identification. The presence of these other types of crystal-related inflammation further emphasizes the value of identifying uric acid crystals as the cause of a particular patient’s arthritis whenever possible, to insure that the correct condition is being treated.
Septic arthritis may present without a fever or elevated white blood cell count; arthrocentesis is required to distinguish this condition from acute gout. Gout and septic arthritis can occur concomitantly, but this is rare 24.
Trauma-associated joint swelling is typically identified by the history; however, trauma may result in an acute gout flare caused by increased concentrations of synovial urate 25. Imaging may be necessary to rule out fracture in a patient with gout-like symptoms after a joint injury.
When the diagnosis of gout is made, the individual must be evaluated for the complications of gout:
- Collections of uric acid (tophi) need to be searched for, and they can be in numerous locations (see Figures 3 and 4).
- Inquiry should be made regarding a history of kidney stone, since a patient with gout and kidney stones (see Figure 6) will likely require faster and more aggressive lowering of uric acid (see below) than one without stones, to try and prevent recurrent stone formation.
- A patient with gout has been shown in a broad range of studies to be at higher risk of coronary artery disease, and should have an evaluation appropriate to coronary risk (for example, lab testing for cholesterol and triglyceride level) 3.
It is important that damage to bone from gout be diagnosed, since documented damage is a clear indication for long-term therapy (see below). Once damage has begun, it’s important to reduce the total body uric acid level, which, by equilibration, causes uric acid to move out of the joints. This is because the blood and joint levels of uric acid reach a certain level, called a “steady state,” at a given level of blood uric acid. If the blood level is reduced, then the joint level of uric acid will gradually decrease as well. This leads to gout attacks diminishing or completely ceasing over time, and to tophi getting reabsorbed and shrinking or fully disappearing.
Different approaches can be taken to lowering total body uric acid. The production of uric acid can be decreased in the body (for example, by allopurinol, see below) or the excretion of uric acid can be increased (for example, by probenecid, see below). The crystals can also be broken down in the body (see rasburicase, and pegylated uricase).
X-rays are the standard imaging technique for gout but in special cases, such as when gout needs to be separated from infection or tumor, magnetic resonance imaging (MRI) will be helpful.
Figure 5. Uric acid crystals
Figure 6. Uric acid stones (kidney stones)
Gout treatment
Gout is best treated with a combination of self-care and medications. The sooner you start treatment, the sooner your pain will go away. Trying to ignore the attack can lead to a more prolonged duration. To achieve rapid and complete resolution of symptoms, treatment of acute gout should commence within 24 hours of symptom onset 13. Putting ice on the affected area to help reduce swelling and pain (for not more than 10 minutes at a time, to avoid skin damage). Gout medications are available in two types and focus on two different problems. The first type helps reduce the inflammation and pain associated with gout attacks. The second type works to prevent gout complications by lowering the amount of uric acid in your blood. Which type of medication is right for you depends on the frequency and severity of your symptoms, along with any other health problems you may have.
Medications are often the most effective way to treat gout attacks and prevent recurrent symptom flares. However, making changes to your diet and lifestyle also are important, and you may want to:
- Choose healthier beverages. Avoid alcoholic beverages completely and limit drinks sweetened with fruit sugar (fructose). Instead, drink plenty of nonalcoholic beverages, especially water.
- Drink extra water to flush your body of uric acid.
- Avoid foods high in purines. Red meat and organ meats, such as liver, are especially high in purines. Purine-rich seafood includes anchovies, sardines, mussels, scallops, trout and tuna. Low-fat dairy products may be a better source of protein for people prone to gout.
- Keep clothes and bedding off the joint to avoid irritation.
- Elevate your joint to help reduce swelling.
- Rest the affected joint. Although exercise is great for helping you lose weight and is generally fine for gout patients, when you have a gout flare in your toe, foot, ankle or knee it is advised to stay off the foot as much as possible until the flare resolves. Pounding on an inflamed gouty joint can prolong the flare. It’s fine to do other kinds of exercise, for example any exercise involving the upper body, but give the gouty joint a rest. This is another reason to treat gout flares quickly, since starting early often means the flare will be short – and you can limit your time off your feet.
- Take medicine to reduce swelling and relieve pain. Over-the-counter medicines include ibuprofen (one brand name: Advil) and naproxen (one brand name: Aleve). Your doctor also can prescribe medicine for you. Examples include corticosteroids, like prednisone, or colchicine.
- Exercise regularly and lose weight. Keeping your body at a healthy weight helps reduce urate levels and can help stop or lower the number of flares you have if you are overweight or obese. Choose low-impact activities such as walking, bicycling and swimming — which are easier on your joints.
Exercise is extremely important, not only to reduce the chances of an attack, but also for your general health and wellbeing. It doesn’t matter how much exercise you do, a little is better than none at all. Start off slowly and gradually build up how much you do until you’re doing regular sessions. As your confidence increases, you can increase the length and intensity of what you’re doing.
Exercises that get you out of breath are particularly good for burning calories. You could try dancing, walking in hilly countryside or doubles tennis.
It helps to find a sport or exercise which you enjoy and will keep doing. Some people find joining a leisure centre or sports club to be really fun and motivational. Have a look around and see what’s available in your area.
You should avoid exercising during a flare up of gout, as it could make your pain worse. It’s important to rest and recover and begin exercising after the pain and swelling has gone down.
Medications for immediate gout pain relief
The management of an acute attack of gout is very different from the prevention of subsequent attacks. Medications used to treat gout flares and prevent future attacks include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs include over-the-counter options such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve), as well as more-powerful prescription NSAIDs such as indomethacin (Indocin, Tivorbex) or celecoxib (Celebrex). Examples include naproxen 500mg twice daily, indomethacin 25mg three times daily or celecoxib 200mg twice a day. NSAIDs carry risks of stomach pain, bleeding and ulcers. Patients with gastric ulcers, hypertension, coronary heart disease, and fluid retention must be careful with these agents, even for the short courses (usually 3-7 days) needed to resolve a gout attack.
- Colchicine. Your doctor may recommend colchicine (Colcrys, Gloperba, Mitigare), an anti-inflammatory drug that effectively reduces gout pain. Using colchicine can be seen as “dampening” the uric acid “matches.” Colchicine does not lower the body’s store of uric acid, but it decreases the intensity of the body’s inflammatory reaction to these crystals. Recent studies have shown that at least one mechanism of colchicine’s action is by acting to prevent a cascade of reactions that lead to the production of interleukin 1-beta, which is an inflammatory protein (cytokine), which is important in gouty inflammation 26. The drug’s effectiveness may be offset, however, by side effects such as nausea, vomiting and diarrhea. In the past, high doses of colchicine were used for gout attacks, but this tended to cause nausea, vomiting, and diarrhea in a large number of patients 27. It has been shown that lower doses of colchicine are as effective as high doses for an attack of gout, and much better tolerated. Assuming no other medical problems that require an adjusted dose, for an attack of gout a patient would receive two tablets of colchicine, 0.6mg each (1.2 mg initially), as soon as possible after a gout attack starts. They would then receive one additional tablet an hour later, then 0.6 to 1.2 mg per day. Colchicine dose needs to be adjusted in patients with significantly decreased kidney function and hepatic insufficiency 14. The long-term adverse effects of colchicine include reversible axonal neuromyopathy (less than 1%). Patients should be advised to stop taking colchicine and tell their physician if they experience leg weakness or pain. Treatment should be discontinued if any signs or symptoms of nerve or muscle damage are present. Colchicine has interactions with certain other medications, most notably clarithromycin (Biaxin®). The rare risk of rhabdomyolysis is increased when colchicine is used concomitantly with statins or clarithromycin (Biaxin), especially in older adults or those with chronic kidney disease; therefore, close monitoring is recommended 28.
- Corticosteroids. Corticosteroid medications, such as prednisone, may control gout inflammation and pain. Corticosteroids may be in pill form, or they can be injected into your joint. Corticosteroids are an appropriate alternative for patients who cannot tolerate NSAIDs or colchicine 14. Side effects of corticosteroids may include mood changes, increased blood sugar levels and elevated blood pressure. Short-term use, as in gout, generally much better tolerated than long-term use. Rebound flares are common after discontinuation of corticosteroid therapy for acute gout. To reduce the risk of a rebound flare, preventive treatment and initiation of a tapered course of corticosteroids over 10 to 14 days is recommended after resolution of symptoms.
- Examples of oral anti-inflammatory corticosteroids include prednisone 40mg first day, 30mg 2nd day, 20mg third day, 10mg fourth day OR 40 mg for four days, then 20 mg for four days, then 10 mg for four days.
- Example of steroid injections: different doses used depending on the size of joint involved, and multiple preparations available. Possible side-effects: 1-2% of the time, a local reaction to the injection can occur, and the joint can temporary worsening the next day, requiring ice application. In diabetics, a single local injection can temporarily raise blood sugar.
During acute flare-ups, low-dose colchicine, NSAIDs, and glucocorticoids delivered orally, intramuscularly, or intra-articularly are similarly effective 29. Nonsteroidal anti-inflammatory drugs (NSAIDs) are the first-line treatment. Indomethacin (Indocin) has historically been the preferred choice; however, there is no evidence it is more effective than any other NSAID. Intramuscular ketorolac appears to have similar effectiveness 27. Any oral NSAID may be given at the maximal dosage and continued for one to two days after relief of symptoms.
Historically, urate-lowering medication was thought to worsen acute gout flares, but recent evidence suggests that allopurinol (Zyloprim) can be started during an acute flare if it is used in conjunction with an NSAID and colchicine 30. Patients receiving a urate-lowering medication should be treated concurrently with an NSAID, colchicine, or low-dose corticosteroid to prevent a flare. Treatment should continue for at least three months after uric acid levels fall below the target goal in those without tophi, or for six months in those with a history of tophi 13. NSAIDs and corticosteroids should not be used for long periods without a urate-lowering medication because uric acid crystals continue to accumulate and damage the joint, despite a lack of pain or clinical signs of inflammation 14. If a patient has a gout flare while receiving a urate-lowering agent, the medication should be continued while the flare is treated acutely 13.
Medications to prevent gout attacks and complications
If you experience several gout attacks each year or if your gout attacks are less frequent but particularly painful, your doctor may recommend medication to reduce your risk of gout-related complications. If you already have evidence of damage from gout on joint X-rays, or you have tophi, chronic kidney disease or kidney stones, medications to lower your body’s level of uric acid may be recommended.
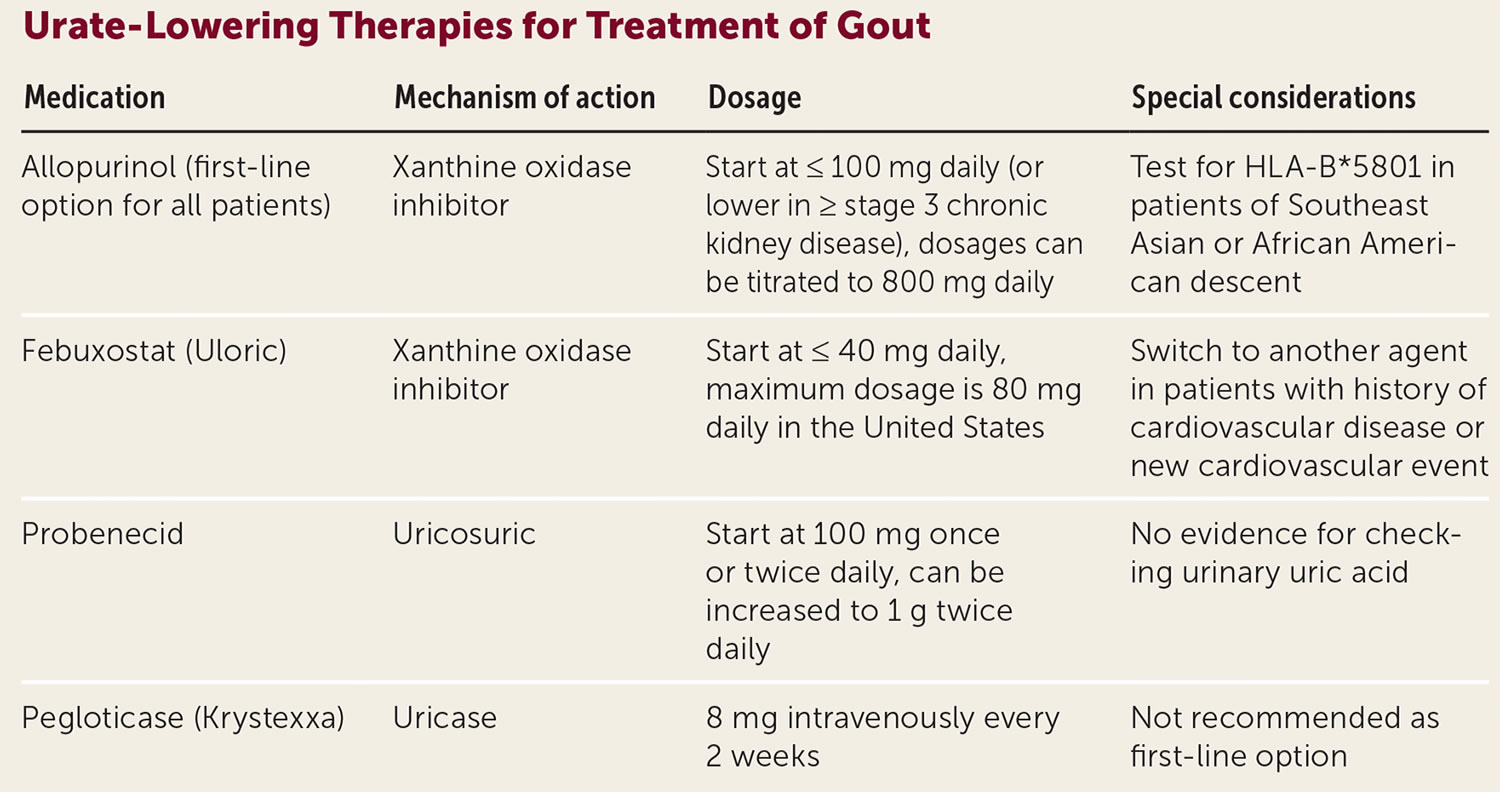
- Medications that block uric acid production. Drugs such as allopurinol (Aloprim, Lopurin, Zyloprim) and febuxostat (Uloric) help limit the amount of uric acid your body makes. In patients with gout and chronic kidney disease or congestive heart failure, allopurinol has the added benefit of preventing chronic disease progression 30. Side effects of allopurinol include fever, rash, hepatitis and kidney problems. Certain ethnic groups have a higher risk of a severe hypersensitivity skin reaction when starting allopurinol therapy. Hypersensitivity reactions to allopurinol occur in patients with the HLA-B*5801 allele. Because this allele affects 7% of people of Southeast Asian descent (Han Chinese, Koreans or Thai descent) and 4% of people of African American descent, HLA-B*5801 genotype testing is recommended for these patients before starting allopurinol 31. Febuxostat (Uloric) is a xanthine oxidase inhibitor that was approved by the FDA in 2009. Although febuxostat is superior to 300 mg allopurinol at lowering serum uric acid levels, it is not more effective at reducing the frequency of gout flares 32. Febuxostat side effects include rash, nausea and reduced liver function. Febuxostat also may increase the risk of heart-related death.
- Medications that improve uric acid removal. Drugs such as probenecid (Probalan) help improve your kidneys’ ability to remove uric acid from your body and is typically used as a second-line treatment because of numerous drug interactions. Of particular concern, probenecid increases blood levels of methotrexate and ketorolac, which may result in severe toxicity. Probenecid may be used in combination with allopurinol or febuxostat when one drug does not independently lower serum uric acid to target levels. Side effects include a rash, stomach pain and kidney stones. Nephrolithiasis (kidney stones) is a common adverse effect that may be avoided by high fluid intake and urine alkalization with potassium citrate 18.
- Lesinurad (Zurampic®): (Although we provide information on this medication, it is no longer available in the United States.) This once-a-day oral medication increases the amount of uric acid that comes out in the urine, a mechanism it shares with probenecid. Lesinurad (Zurampic®) was approved for gout by the FDA in 2016, to be used together with either allopurinol or febuxostat to help get patients to their goal uric acid of less than 6 mg per dL. It is not approved to be used alone for gout. This medication was generally well-tolerated in studies 33. It is not approved for use in people with significant decrease in kidney function, and some patients have had worsened kidney function (which was generally reversible) while taking lesinurad. Kidney function is thus checked before and during treatment. Lesinurad is taken once a day, so more convenient than probenecid. In theory this medication, like probenecid, can increase the risk of uric acid-induced kidney stones, but this was minimal risk in published studies and the combination with either allopurinol or probenecid likely dramatically reduces this risk. Lesinurad is now available in combination with allopurinol, allowing a person taking both medications to take a single pill a day. The combination pill is marketed as Duzallo®, which comes as either a combination of allopurinol 300mg with 200mg of lesinurad or a combination of 200mg allopurinol and 200mg lesinurad.
- Pegloticase (Krystexxa®). Pegloticase (Krystexxa) is an intravenous uricase approved by the FDA in 2010. The mechanism of action involves metabolism of uric acid to allantoin. It is a third-line agent and is indicated for treatment of refractory gout. It is usually administered by a rheumatologist and is given every two weeks at a cost of more than $5,000 per dose 34. Cardiac events have occurred during the studies of Krystexxa®, and the FDA reviewed them closely and concluded that they did not appear due to the medication. There were also allergic-type events and events where patients dropped their blood pressure while this intravenous agent was running into them. None of these episodes of drop in blood pressure led to death or long-term problems for the patients, however, and the blood pressure returned to baseline in these cases. The drop in blood pressure is still a concern, and this medication must be used in a setting where treatment of the drop in blood pressure can be managed. Pegloticase may be especially useful in patients with very large collections of uric acid (tophi), especially if these are draining to the skin. Like febuxostat (Uloric), pegloticase does not appear dependent on the kidney to be removed from the body, allowing it to be considered in patients with decreased kidney function. Because pegloticase is given intravenously, it would be expected that the great majority of its use would be by rheumatologists rather than by internists or primary care physicians. More recent data has looked at ways to reduce the body forming antibodies to pegloticase. Early data has looked at medications such as methotrexate, mycophenolate mofetil (Cellcept®) and azathioprine (Imura®) given during the course of pegloticase treatement, and the results to date have been very encouraging. A larger trial with methotrexate and pegloticase is in progress.
During a second gout flare-up in one year, low-dose allopurinol (Aloprim, Lopurin, Zyloprim) can be started with anti-inflammatory therapy without worsening the flare-up 29.
Allopurinol is a xanthine oxidase inhibitor and is the preferred urate-lowering agent 18, but HLA testing should be offered to patients of Southeast Asian or African American descent before starting to identify patients at risk for an allergic reaction. Hypersensitivity reactions to allopurinol occur in patients with the HLA-B*5801 allele. Because this allele affects 7% of people of Southeast Asian descent (Han Chinese, Koreans or Thai descent) and 4% of people of African American descent, HLA-B*5801 genotype testing is recommended for these patients before starting allopurinol 31. Allopurinol desensitization can be performed after an allergic response 29. If the rash was relatively mild, one option is an oral desensitization regimen that involves having a pharmacist put together a solution of allopurinol of very low dose and then gradually increasing concentrations over the course of a month. Although at times the rash will reoccur during this process, often a patient can be desensitized in this way and subsequently tolerate allopurinol. Although some patients develop a mild rash to allopurinol that remains mild over time, or respond to antihistamines, continuing the allopurinol despite a rash is not advised, since the rash can worsen unpredictably.
If a patient can’t tolerate allopurinol, and meets the criteria for probenecid, that can be tried. There are some medications which are used for other indications but that have modest effect in lowering uric acid levels, such as losartan (Cozaar®), used for hypertension, and fenofibrate (Tricor®), used for elevated triglycerides, but these only infrequently can sufficiently lower uric acid level.
If none of the above options is possible or successful, physicians often seek a clinical trial of a new agent for gout, if available, for their patient to enter.
The starting allopurinol dosage is 100 mg per day and 300 mg per day is a common maintenance dosage. Dosing is guided by the target serum uric acid level 18. Titrating urate-lowering therapy to reach a serum urate level of 6 mg/dL decreases flare-ups and increases treatment adherence 29.
In patients with chronic kidney disease, low initial allopurinol doses are recommended with slow titration to achieve target uric acid levels 35. Dosages higher than 300 mg may be used—even in those with renal impairment—as long as patients are closely monitored for adverse effects 18.
Urate-lowering therapies
Allopurinol is the first-line urate-lowering therapy 29. Febuxostat (Uloric), the other xanthine oxidase inhibitor, is limited by increased cardiovascular and all-cause mortality seen in studies 29. Urate-lowering therapies are summarized in Table 3.
Urate-lowering therapy is started at a low dose to monitor the side effects and response to treatment. Titration of the dose is every 2 to 6 weeks to achieve serum urate levels of less than 6 mg/dl or 5 mg/dl in those patients with tophi 18.
During the initiation of urate-lowering therapy, there is an increased risk of gout flare-ups, so colchicine prophylaxis is recommended for 3 for months after achieving serum urate goal in the patients without tophi or 6 months with tophi to reduce the flare-up risk 27.
Table 3. Urate-lowering therapy for gout treatment
[Source 29 ]When to consider Urate-Lowering Therapy
Urate-lowering therapy is recommended for patients with two or more gout flare-ups per year, tophaceous gout, or damage attributable to gout visible on radiography. Consider starting therapy for patients with a second flare-up even if not within one year. With a first gout flare-up, shared decision-making is appropriate in patients at high risk because of a serum urate level of 9 mg per dL (0.54 mmol per L) or higher, urolithiasis, or stage 3 or greater chronic kidney disease 29. Urate-lowering therapy has not been shown to be beneficial for patients with asymptomatic hyperuricemia.
The American College of Rheumatology recommends starting urate-lowering therapy during an acute flare-up instead of waiting until it resolves. Urate-lowering therapy started during a flare-up does not increase or prolong symptoms as long as anti-inflammatory treatments are provided. The American College of Rheumatology notes that patients are most motivated for treatment during a gout attack. Anti-inflammatory medications such as colchicine or nonsteroidal anti-inflammatory drugs (NSAIDs) should be continued for three to six months after starting urate-lowering therapy.
Foods to avoid with gout
Avoid foods high in purines. Red meat and organ meats, such as liver, are especially high in purines. Purine-rich seafood includes anchovies, sardines, mussels, scallops, trout and tuna. Low-fat dairy products may be a better source of protein for people prone to gout.
Alternative medicine
Cherry juice, which has long been an alternative remedy and which had anecdotal support, now has been studied. Cherry products such as whole cherries or unsweetened cherry juice may reduce gout flares. At the American College of Rheumatology meeting in November 2010 there were two studies looking at cherry juice. It appears that cherry juice may have a small effect in decreasing production of uric acid. It also, possibly through its vitamin C content, can increase the excretion of uric acid by the kidney.
In separate earlier study, vitamin C itself did appear to increase uric acid excretion. However, the effect (using 500mg a day dosing) was small–only a drop in blood uric acid level of about 0.5 mg/dL, and almost all gout patients need to come down more than this to get to the goal of less than 6.0 mg/dL. These early studies of cherry juice are interesting, and might be relevant for a patient who was “almost there” in their uric acid goal, but a gout sufferer should be very careful about trusting to cherry juice to manage their uric acid. Based on the data, the result is likely not going to be sufficient.
A glass of skim milk and eating low-fat yogurt daily may also help to lower uric acid over time and prevent attacks of gout.
Glucosamine is made from the outer shells of shellfish and it doesn’t contain purines. However, there’s no evidence that glucosamine can prevent or treat gout.
Devil’s claw (Harpagophytum procumbens), curcumin (a component of turmeric) and many other herbal treatments have been proposed as gout therapy, and further study of these is indicated.
Possible future treatments of gout
Fortunately, present medications are successful in the vast majority of gout patients. But some patients cannot tolerate our present arsenal of gout medications. For others, these agents are not sufficiently effective. Therefore, new treatments are continually being sought. Some of the more promising include anakinra, rilonacept, canakinumab, BCX4208 and arhalofenate.
- Anakinra (Kineret®): This interleukin-1 (IL-1) inhibitor is presently approved by the FDA for the treatment of rheumatoid arthritis, and doctors do use it “off label” in many cases of difficult-to-manage gouts. It works to block the receptor for interleukin 1-beta, an important inflammatory chemical (cytokine). Since interleukin 1-beta has been shown to be a key player in gouty inflammation, this agent has been studied in the treatment of gout attacks and appears to have been successful in preliminary study 36.
- Rilonacept (Arcalyst®) is a fusion protein which acts as a blocker of interleukin 1- beta, and it has a longer duration of action than Anakinra. This agent has been studied in a 14-week trial and showed improvement in gouty symptoms 37. This agent may have a future role in preventing gout attacks when patients are started on a uric acid lowering agent but can take the usual prophylactic agents against the attacks that often are an early result of this therapy (for example, they can’t use colchicine). There may also be selected patients where rilonacept treatment might be a longer-term alternative.
- Canakinumab (Ilaris®) is a human monoclonal antibody which targets interleukin 1- beta, and a recent abstract looked at its ability to treat and prevent gout attacks, which showed some success 37. As with Rilonacept above, this agent may have a future role in the acute treatment and relatively short-term prevention of gout, and may have a longer-term role in selected patients with problems with multiple other options.
- BCX4208: This is a compound being studied as an alternative way to decrease the production of uric acid. It might be used alone, or together with a drug such as allopurinol or febuxostat in patients who otherwise could not have their uric acid level brought below 6. This agent works as a purine nucleoside phosphorylase inhibitor, a different mechanism than any of the medications to chronically lower uric acid described above. Early studies suggest that this new mechanism is effective in lowering uric acid levels 38.
- Arhalofenate: This medication both lowers uric acid and decreases inflammation in gout, and is being studied as a medication that might allow urate to be lowered without adding a medication to decrease inflammation (such as colchicine).
When is surgery considered for gout?
The question of surgery for gout most commonly comes up when a patient has a large clump of urate crystals (a tophus), which is causing problems. This may be if the tophus is on the bottom of the foot, and the person has difficulty walking on it, or on the side of the foot making it hard to wear shoes. An especially difficult problem is when the urate crystals inside the tophus break out to the skin surface. This then can allow bacteria a point of entry, which can lead to infection, which could even track back to the bone. Whenever possible, however, doctors try to avoid surgery to remove tophi. The problem is that the crystals are often extensive, and track back to the bone, so there is not a good healing surface once the tophus is removed. In some rare cases, such as when a tophus is infected or when its location is causing major disability, surgical removal may be considered.
Since it is hard to heal the skin after a tophus is removed, a skin graft may be needed. For this reason, doctors often try hard to manage the tophus medically. Giving high doses of medication to lower the urate level, such as allopurinol, over time the tophus will gradually reabsorb. In severe cases, rheumatologists may consider using the intravenous medication pegloticase (Krystexxa®), since it lowers the urate level the most dramatically, and can lead to the fastest shrinkage of the tophus.
Gout prognosis
The prognosis of gout depends on the comorbidity of each individual. Mortality is higher in individuals with cardiovascular comorbidity. When gout receives proper treatment, most patients will live a normal life with mild complications. For patients whose symptoms appear at an earlier age, they usually will have a more severe disease at presentation. For those who do not modify their lifestyle, recurrent flare-ups are common.
Living with gout
Gout affects quality of life by both the intermittent attacks and the potential for chronic (lasting) arthritis. Compliance with your treatment plan is critical. Lifestyle changes may make it easier to manage this lifelong disease. Suggestions include gradual weight loss, avoidance of alcohol and reduced consumption of fructose‐containing drinks and foods high in purines.
References- Ning TC, Keenan RT. Unusual clinical presentations of gout. Curr Opin Rheumatol. 2010;22(2):181–187.
- Neogi T. Clinical practice. Gout. N Engl J Med. 2011;364(5):443–452.
- Baker et al: Serum uric acid and cardiovascular disease: Recent developments, and where do they leave us? Am J Med, 118:816-26, 2005. A review article concluding that uric acid is an independent risk factor for coronary disease.
- Sapkota SK, Kolade VO, Brit ML. Gouty tophi. J Community Hosp Intern Med Perspect. 2014;4(1):10.3402/jchimp.v4.22920. Published 2014 Feb 17. doi:10.3402/jchimp.v4.22920 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3937563
- Wortmann RL. Effective management of gout: an analogy. Am J Med. 1998 Dec; 105(6):513-4. A review article that includes the “match” analogy to help patients understand the management of the various stages of gout, seeing uric acid as matches which can be “lit” (i.e. cause inflammation), “dampened” to decrease inflammation or removed from the joint.
- Berman EL. Clues in the eye: ocular signs of metabolic and nutritional disorders. Geriatrics. 1995 Jul;50(7):34-6, 43-4.
- Reginato AM, Mount DB, Yang I, Choi HK. The genetics of hyperuricaemia and gout. Nat Rev Rheumatol. 2012;8(10):610–621.
- Neogi T. Gout. Ann Intern Med. 2016 Jul 5;165(1):ITC1-ITC16. doi: 10.7326/AITC201607050
- Fenando A, Rednam M, Widrich J. Gout. [Updated 2021 Sep 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546606
- Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum. 2011;63(10):3136–3141.
- Singh JA. Racial and gender disparities among patients with gout. Curr Rheumatol Rep. 2013;15(2):307.
- Shoji et al: A retrospective study of the relationship between serum urate level and recurrent attacks of gouty arthritis: evidence for reduction of recurrent gouty arthritis with antihyperuricemic therapy. Arthritis Rheum, 51(3):321-5, 2004. This is one among a group of studies demonstrating the benefit of keeping uric acid below 6.0 in gout patients.
- Janssens HJ, Janssen M, van de Lisdonk EH, van Riel PL, van Weel C. Use of oral prednisolone or naproxen for the treatment of gout arthritis: a double-blind, randomised equivalence trial. Lancet. 2008;371(9627):1854–1860.
- Burns CM, Wortmann RL. Latest evidence on gout management: what the clinician needs to know. Ther Adv Chronic Dis. 2012;3(6):271–286.
- Choi HK et al: Purine-rich foods, dairy and protein intake, and the risk of gout in men. New Engl J Med, (11):1093-103, 2004. This article emphasizes the finding that red meat and shellfish increase gout risk while low-fat dairy intake seems to decrease it.
- Choi HK et al: Alcohol intake and risk of incident gout in men: a prospective study. Lancet, 363(9417):1277-81, 2004. This article pinpoints beer as being a particular risk factor for gout.
- Saag KG and Choi H: Epidemiology, risk factors, and lifestyle modifications for gout. Arthritis Res Ther 8 Suppl 1:S2, 2006. This article reviews lifestyle modifications that can influence gout risk, including weight loss, alcohol and diet.
- Khanna, D., Fitzgerald, J. D., Khanna, P. P., Bae, S., Singh, M. K., Neogi, T., Pillinger, M. H., Merill, J., Lee, S., Prakash, S., Kaldas, M., Gogia, M., Perez-Ruiz, F., Taylor, W., Lioté, F., Choi, H., Singh, J. A., Dalbeth, N., Kaplan, S., Niyyar, V., … American College of Rheumatology (2012). 2012 American College of Rheumatology guidelines for management of gout. Part 1: systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis care & research, 64(10), 1431–1446. https://doi.org/10.1002/acr.21772
- Choi HK. Diet, alcohol, and gout: how do we advise patients given recent developments? Curr Rheumatol Rep. 2005;7(3):220–226.
- Choi HK, Willett W, Curhan G. Fructose-rich beverages and risk of gout in women. JAMA. 2010;304(20):2270–2278.
- Kedar E, Simkin PA. A perspective on diet and gout. Adv Chronic Kidney Dis. 2012;19(6):392–397.
- Wallace SL, Robinson H, Masi AT, Decker JL, McCarty DJ, Yü TF. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977;20(3):895–900.
- Modified from Wallace, SL, et al: Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum., 20:895, 1977.
- Yu KH, Luo SF, Liou LB, et al. Concomitant septic and gouty arthritis—an analysis of 30 cases. Rheumatology (Oxford). 2003;42(9):1062–1066.
- Pittman JR, Bross MH. Diagnosis and management of gout. Am Fam Physician. 1999;59(7):1799–1806, 1810.
- Drenth J and van der Meer J: The Inflammasome — A Linebacker of Innate Defense. N Engl J Med 355:730-732, 2006. A review of a recently recognized pathway by which colchicine inhibits the inflammatory process of gout.
- Khanna, D., Khanna, P. P., Fitzgerald, J. D., Singh, M. K., Bae, S., Neogi, T., Pillinger, M. H., Merill, J., Lee, S., Prakash, S., Kaldas, M., Gogia, M., Perez-Ruiz, F., Taylor, W., Lioté, F., Choi, H., Singh, J. A., Dalbeth, N., Kaplan, S., Niyyar, V., … American College of Rheumatology (2012). 2012 American College of Rheumatology guidelines for management of gout. Part 2: therapy and antiinflammatory prophylaxis of acute gouty arthritis. Arthritis care & research, 64(10), 1447–1461. https://doi.org/10.1002/acr.21773
- Chattopadhyay I, Shetty HG, Routledge PA, Jeffery J. Colchicine induced rhabdomyolysis. Postgrad Med J. 2001;77(905):191–192.
- Management of Gout: Update from the American College of Rheumatology. Am Fam Physician. 2021 Aug ;104(2):209-210. https://www.aafp.org/afp/2021/0800/p209.html
- Goicoechea M, de Vinuesa SG, Verdalles U, et al. Effect of allopurinol in chronic kidney disease progression and cardiovascular risk. Clin J Am Soc Nephrol. 2010;5(8):1388–1393.
- Hershfield MS, Callaghan JT, Tassaneeyakul W, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for human leukocyte antigen-B genotype and allopurinol dosing. Clin Pharmacol Ther. 2013;93(2):153–158.
- Love BL. Febuxostat (Uloric) for hyperuricemia and gout. Am Fam Physician. 2010;81(10):1287–1289.
- Saag KG, Fitz-Patrick D, Kopicko J, Fung M, Bhakta N, Adler S, Storgard C, Baumgartner S, Becker MA: Lesinurad Combined With Allopurinol: Randomized, Double-Blind, Placebo-Controlled Study in Gout Subjects With Inadequate Response to Standard of Care Allopurinol (A US-based Study).Arthritis Rheumatol. 2016 Aug 26. doi: 10.1002/art.39840. [Epub ahead of print]. Demonstration of effectiveness of lesinurad, in combination with allopurinol, in getting patients to their uric acid goal.
- Drugs for gout. Med Lett Drugs Ther. 2014;56(1438):22–24.
- Stamp LK, Taylor WJ, Jones PB, et al. Starting dose is a risk factor for allopurinol hypersensitivity syndrome: a proposed safe starting dose of allopurinol. Arthritis Rheum. 2012;64(8):2529–2536.
- Terkeltaub R et al: The interleukin 1 inhibitor rilonacept in treatment of chronic gouty arthritis: results of a placebo-controlled, monosequence crossover, non-randomised, single-blind pilot study. Annals of Rheumatic Disease 68:1613-1617, 2009
- So A at al: Canakinumab (ACZ885) Vs. Triamcinolone Acetonide for Treatment of Acute Flares and Prevention of Recurrent Flares in Gouty Arthritis Patients Refractory to or Contraindicated to NSAIDs and/or Colchicine. American College of Rheumatology Abstract LB4, October 2009. https://acr.confex.com/acr/2009/webprogram/Paper17258.html
- Fitz-patrick D et al: Abstract 150: Effects of a Purine Nucleoside Phosphorylase Inhibitor, BCX4208, on the Serum Uric Acid Concentrations in Patients with Gout. Abstract from the American College of Rheumatology Meeting November 2010.