Hair tourniquet syndrome
Hair tourniquet syndrome is a rare clinical phenomenon that involves is a strangulation of body appendages by hair, thread, or similar material becoming so tightly wrapped around an appendage that it results in pain, injury, and, sometimes, loss of the appendage 1. Hair thread tourniquet syndrome is a rare and often misdiagnosed condition which may result in accidental organ amputation 2. Essentially, any appendage may be involved, including a toe, wrist, penis, scrotum, tongue, uvula, vaginal labium, ear lobe, umbilicus, or nipple 3. In a meta-analysis review of 210 cases of hair tourniquet syndrome, 44.2% involved the penis, 40.4% the toes, 8.6% fingers, and another 6.8% represented other sites 4. One should always bear in mind that hair tourniquet syndrome could be due to more than one strand of hair 5. Hair tourniquet syndrome confers an inherent risk of loss of function and autoamputation. However, it is easily treatable and long-term effects are largely preventable with prompt diagnosis. Clinicians should maintain a high index of suspicion when confronted with such presentations.
Circumferential digital strangulation impairs lymphatic and venous drainage causing distal edema. Further obstruction may cause arterial occlusion and ischemic injury 6. Prolonged ischemic injury leads to tissue necrosis and ultimately autoamputation. Treatment is prompt removal of the constricting hair or fiber. It can usually be removed by direct inspection. Surgical exploration is mandatory if doubt persists as to the completeness of removal, especially as the hair cuts through the skin and becomes invisable 7.
Complications such as constrictive scarring, flexion deformity, and even urocutaneous fistulae may affect healing post release 8.
Hair tourniquet syndrome can be observed across all ages. The majority of cases of hair tourniquet syndrome have been reported in infants of less than 2 months of age 9. The younger age group, especially infants younger than 4 months, is thought to be more at risk because 90% of mothers experience excessive postpartum hair loss, called telogen effluvium 10. Hair tourniquet syndrome involving the toes or toe tourniquet syndrome occurs during the time period when postpartum mothers are experiencing increased hair loss 11.
Most cases of hair tourniquet syndrome are felt to be accidental, but intentional cases consistent with child abuse have been cited in the literature 12, 13. Most cases of hair wrapping occur in young children. The most often observed age range of reported cases of finger wrapping is in the first days of life up to 19 months, and penile involvement is 4 months to 6 years 14. Labial and clitoral wrapping have been described in an older age group (age 7-13 years) 15. Case reports have documented 80- and 84-year-old men with involved extremities 16.
Although most cases are felt to be accidental, child abuse must be considered in selected cases 13.
Hair tends to lacerate the skin or the mucosa, and embeds in deeper tissues 17. Swelling of the strangulated appendage and the physical characteristics of hair contribute to progressive cutting of the soft tissues resulting in excruciate pain 18. Human hair is extremely thin and, hence, easily overlooked, especially when a patient presents with a foreign body reaction and local swelling 19. Hair may wrap and create a tourniquet resulting in lymphatic obliteration, venous congestion, and arterial obstruction which occasionally lead to necrosis and amputation of the part involved 20. Once constricted over an appendage, reepithelialization may occur if the offending fiber is not removed in a timely fashion. This may further obscure the hair or thread below an overlying skin bridge, making recognition more difficult 21. Hair has high tensile strength and the ability to stretch when wet and contract or tighten as it dries 19. The wrapping of the offending fiber or hair around a digit is thought to be caused by repetitive movement of the appendage in a confined area, such as hands in mittens or feet in pajamas 22. The tissue injury from constricting bands may be caused by ischemic compression of blood vessels and the direct cutting action of the tourniquet 21. In addition to soft-tissue damage, this mechanism is even capable of disrupting bone 4.
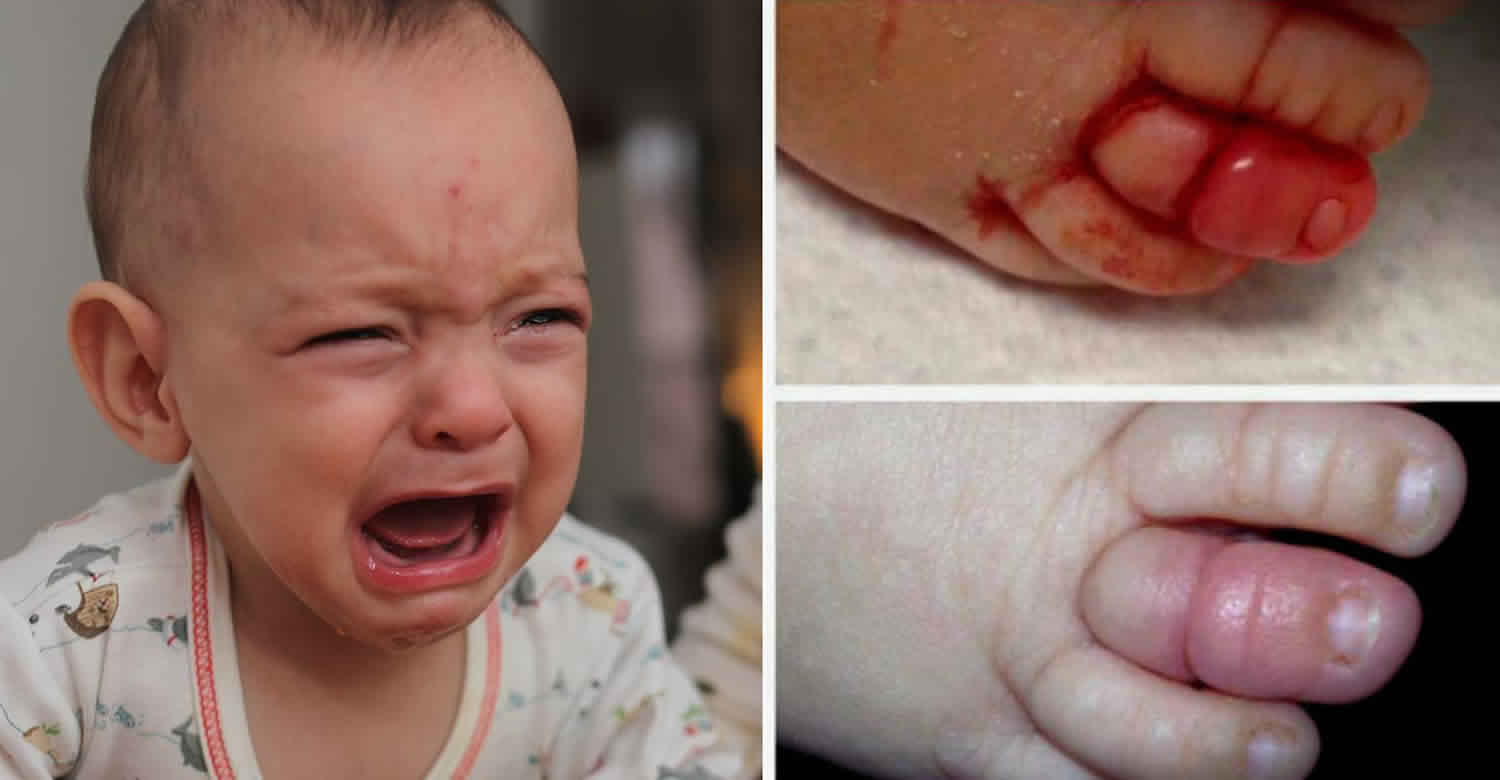
Although the affected patient can present in several ways, the classic presentation is that of the irritable and inconsolable infant. The diagnosis can be made after identification of a swollen and painful appendage with sharp circumferential demarcation from normal tissue proximally. Examination in the emergency department may carry a risk of incomplete removal of the strangulation, as patient may not be cooperative 23. Most of the time, the affected child will be straining and makes examination difficult. The ideal examination should be performed under general anesthesia 23. In cases of incomplete removal, one should always think of buried constricting hair. A longitudinal incision can be made over the constriction band to make sure that the strangulation is completely release. Incision can be made at the dorsal anteromedial or anterolateral of the finger 24. After removal, the children should be monitored. There will be tremendous improvement of symptoms once it is completely removed.
Figure 1. Toe tourniquet syndrome
Figure 2. Penile hair tourniquet
Footnote: 10-year-old boy was admitted for surgery to treat hypospadias failure after multiple previous surgeries. (a and b) Pre-operative presentation, before removal the entangled hair coil. Please notice the epithelialization of the cut surface in the glans and proximal penile surface and the absence of edema and open wounds. (c) The hair coil, after removal.
[Source 25 ]Hair tourniquet symptoms
Hair tourniquets become very painful, so a baby who has one will likely cry a lot. Looking for a hair tourniquet is a unique but important addition to any parent or caregiver’s checklist when helping a crying baby.
If your baby is crying or seems in pain, and you’ve tried the standard feed-change-sleep routine, it’s a good idea to look over the whole body for a hair tourniquet.
Signs and symptoms include:
- excessive crying
- red or discolored finger, toe, genitalia, umbilical stump, or tongue
- mild to severe swelling in the appendage
- an indentation or groove on the appendage, even if no hair is visible
Hair tourniquets are dangerous if they go unnoticed for too long. Babies risk injuring or losing the affected body part. Hair tourniquets can also cause a complication called ischemia, which is a lack of blood flow to the affected area.
Hair tourniquet treatment
Removal of the offending fiber is indicated in all cases of hair or thread tourniquet syndrome and should be implemented as early as possible.
Adequately visualized constricting bands with little or no tissue edema are good candidates for the unwrapping technique.
Cases associated with mild-to-moderate edema are candidates for the blunt probe cutting technique.
In cases in which other techniques have failed, when the swelling is so severe that the constricting band is not visible, or when epithelialization has occurred, the incisional approach should be implemented.
The use of depilatory creams is a safe alternative to instrumentation and can be done with minimal discomfort, while taking care and using caution on the application to the skin of the penis; it should be avoided when it involves the vagina and mucosal surfaces, as this could lead to burns or irritation 26.
Cases requiring surgical debridement have been described 27. When formation of excessive granulation tissue or involution under edematous skin is present, consider urgent surgical referral.
Hair tourniquet treatment key points:
- Always document neurovascular status, tendon function, or both after the procedure.
- If the skin or distal structures have been lacerated or compromised by the hair tourniquet or its removal, appropriate tetanus wound prophylaxis should be provided.
- A urology consultation should be obtained immediately in all cases of hair tourniquet that involve the penis.
- Surgical consultation may be necessary in cases involving significant tissue edema, distorted anatomy, necrosis, or uncertainty about the completeness of the removal.
- Antibiotic therapy should be considered for patients who are immunocompromised, have diabetes, or have contaminated wounds 28.
- Very young, preverbal children with constricting bands should be evaluated for child neglect or abuse 12.
- Urgent follow-up is required, and patients should be discharged with wound care instructions and return precautions.
Hair tourniquet removal
The choice of hair tourniquet removal technique may vary depending on the clinician’s skill, the appendage involved, the patient’s age, and the patient’s ability to cooperate.
Unwrapping method
This technique is likely to be successful in cases with minimal edema and clear access to the constricting fibers.
Look closely to identify a free end of the hair or thread.
Grasp the free end, then slowly pull and unwind the hair from the appendage using gloved fingers or a pincer instrument (eg, fine-tipped forceps, hemostat).
If no free end is visible, but a hair knot is visible, break the knot off the strand at one end using fine-tipped forceps, and then unwrap the hair as described 21.
The unwrapping method may require multiple attempts, as the hair strand may break apart during removal or multiple hair strands may be involved.
Cutting method
Blunt probe method
This method is likely to be successful in cases in which the constricting band is not too deeply embedded in the soft tissue.
Gently wedge a blunt probe or metal earwax curette between the skin and the hair. Insertion is facilitated when performed in a proximal-to-distal direction while applying traction to the skin, allowing the hair to penetrate less deeply 21.
Cut the hair with fine-tipped scissors or a No. 11 scalpel blade directed against the surface of the probe or curette so as to protect the underlying skin. Alternatively, lift a strand of hair gently away from the skin with the upturned scalpel blade until the hair is divided 28.
Once divided, the hair can be removed using the simple unwrapping method described above.
Incisional approach for digital involvement
This approach is the most invasive and should be reserved for severe cases of digital involvement.
A digital nerve block is recommended.
The involved area must be adequately sterilized with povidone-iodine solution and then draped, with close adherence to sterile protocol throughout the procedure.
Once the area is anesthetized and prepared, make an incision using a No. 11 scalpel blade at either the 3- or 9-o’clock position of the digit.
The incision should be made longitudinally, with the blade perpendicular to the strand and skin surface, going from proximal to distal, and deep to bone to ensure incision of the fiber 21.
Using the 3- and 9-o’clock positions tends to avoid the dorsal and ventral neurovascular bundles of the digits.
An alternative incision site is along the dorsal aspect or 12-o’clock position 14. A dorsal longitudinal incision parallel to the extensor tendon fibers is typically found to heal well with splinting and general wound care 21.
Incisional approach for penile involvement
This approach is the most invasive and should be reserved for severe cases of penile involvement.
A dorsal nerve block with or without topical anesthetic is recommended.
The area involved must be adequately sterilized with povidone-iodine solution and draped, with close adherence to sterile protocol throughout the procedure.
The recommended site for the incision is the inferolateral surface at the 4- or 8-o’clock position, as these sites are ideal for minimizing risk of injury to the dorsal neurovascular structures of the penis.
The incision should be made longitudinally, staying in the deep penile fascia between the corpus cavernosum and spongiosum 29.
The deep fascia of the penis is relatively tough. In light of this, the clinician may elect to make light incisions along the initial incision, slightly deeper with each stroke, with the goal of cutting the constricting band without penetrating the fascial layer into the lumen of the corpora 21.
Depilatory method
Although such use is off-label, chemical depilatories are easy and painless to use, relinquishing the need for anesthetic agents 30.
A 2015 single center retrospective study showed that 64% of the 81 patients enrolled had successful treatment of the hair tourniquet with one or two treatments. None had success past two applications 31.
Chemical depilatories should not be used on broken skin or with any sign of tissue necrosis. Exercise caution using these creams on the skin of the penis so as to avoid the meatus; limit application to the shortest time necessary. Depilatory creams should be avoided all together on the vaginal area or any area near a mucosal surface, and the clinician then should proceed with mechanical removal 26.
Standard chemical depilatory agents (eg, NairTM) are thioglycolate-based and work to disrupt the chemical bonds of hair keratin, causing the hair to break in half. Consequently, their use is limited to hair tourniquets and will not be of utility in removal of thread tourniquets.
The manufacturer’s instructions recommend that a small site be tested before use 24 hours prior to the main application to assess for irritation or allergic reactions. This should not preclude the use of depilatory creams in emergent situations.
Apply the depilatory cream to the region of the hair tourniquet, with specific attention to the knotted area, and wait the time indicated on the product (typically, 3-10 min) for complete hair breakage 28. A second application can be applied 10-15 minutes after the initial application 31.
After the specified time has passed, wash off the depilatory cream with soap and water.
Hair tourniquet complications
Prolonged ischemia, the cutting action of the tourniquet, or the removal incision may all cause damage to the neurovascular structures of the involved appendage. The incisional approach is most fraught with risk for the complication of injury and poses the additional risk of damage to underlying structures. Incisional removal of hair tourniquets from the penis could damage the corpus callosum, corpus spongiosum, or urethra. The incisional approach on the digits may involve injury to the dorsal or palmar neurovascular bundles or flexor tendons when using the 3- or 9-o’clock incisions. Although the dorsal incision alternative should spare these digital structures, the extensor tendon or the tendon sheath may be damaged, with the latter potentially resulting in tenosynovitis 21.
As with all procedures, if the skin is penetrated, either by the constricting band or an incision, bleeding and infection are known risks.
The use of commercial depilatory cream to remove a hair tourniquet may provoke local skin irritation or contact dermatitis.
Among the methods described, the simple unwrapping approach carries the least risk for iatrogenic complication.
Depending on the degree and duration of the constricted appendage, necrosis of distal structures may ensue.
References- Sivathasan N, Vijayarajan L. Hair-thread tourniquet syndrome: a case report and literature review. Case Rep Med. 2012. 2012:171368.
- Barton DJ, Sloan GM, Nichter LS, Reinish JF. Hair-thread tourniquet syndrome. Pediatrics. 1988; 82:925-8.
- Flores JR. Hair tourniquet syndrome in the dental patient. Anesth Prog. 2014 Fall. 61 (3):111-2.
- Mat Saad AZ, Purcell EM, McCann JJ. Hair-thread tourniquet syndrome in an infant with bony erosion: a case report, literature review, and meta-analysis. Ann Plast Surg. 2006 Oct. 57(4):447-52.
- Karalezli K, Karakoc Y, Iltar S, Karalezli N, Irgit K. Hair-thread tourniquet syndrome. Acta Orthop Belg. 2004;70:180–1.
- Mackey S, Hettiaratchy S, Dickinson J. Hair-tourniquet syndrome_multiple toes and bilaterality. Eur J Emerg Med. 2005;12:191–2.
- Alverson B. A genital hair tourniquet in a 9-year-old girl. Pediatr Emerg Care. 2007;23:169–170.
- Liow RY, Budny P, Regan PJ. Hair thread tourniquet syndrome. J Accid Emerg Med. 1996 Mar. 13(2):138-9.
- Sudhan ST, Gupta S, Plutarco C. Toe-tourniquet syndrome_accidental or intentional? Eur J Pediatr. 2000;159:866.
- Strahlman RS. Toe tourniquet syndrome in association with maternal hair loss. Pediatrics. 2003 Mar. 111(3):685-7.
- Strahlman RS. Toe tourniquet syndrome in association with maternal hair loss. Pediatr. 2003;111:685–7.
- Johnson CF. Constricting bands. Manifestations of possible child abuse. Case reports and a review. Clin Pediatr (Phila). 1988 Sep. 27(9):439-44.
- Cevik Y, Kavalci C. Hair tourniquet syndrome. Ann Saudi Med. 2010;30(5):416–417. doi:10.4103/0256-4947.67088 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941260
- Barton DJ, Sloan GM, Nichter LS, et al. Hair-thread tourniquet syndrome . Pediatrics. 1988 Dec. 82(6):925-8.
- Bacon JL, Burgis JT. Hair thread tourniquet syndrome in adolescents: a presentation and review of the literature. J Pediatr Adolesc Gynecol. 2005 Jun. 18(3):155-6.
- Srinivasaiah N, Yalamuri R, Vetrivel S, Irwin L. Limb tourniquet syndrome – A cautionary tale. Injury Extra. Apr 2008. 39:140-42.
- Dua A, Jamshidi R, Lal DR. Labial hair tourniquet. Pediatr Emerg Care. 2013; 29:829-30.
- Rich MA, Keating MA. Hair tourniquet syndrome of the clitoris. J Urol. 1999; 162:190-1.
- Bangroo AK, Chauhan S. Hair tourniquet syndrome (Case Report). Indian Assoc Pediatr Surg. 2005. 10(1):55-56.
- Panagidis A, Sinopidis X, Alexopoulos V, Georgiou G. Hair Tourniquet Syndrome of Labia Minora. APSP J Case Rep. 2015;6(2):22. Published 2015 May 1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4448105
- Loiselle J, Cook RT. Henretig FM, King C. Textbook of Pediatric Emergency Procedures. Baltimore, Md: Williams and Wilkins; 1997.
- Bothner J. Hair entrapment removal techniques. UpToDate. August 20, 2003.
- Hussin P, Mawardi M, Masran MS, Ganaisan P. Hair tourniquet syndrome: revisited. G Chir. 2015;36(5):219–221. doi:10.11138/gchir/2015.36.5.219 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4711978
- Hussain HM. A hair tourniquet resulting in strangulation and amputation of penis: case report and literature review. J Paediatr Child Health. 2008;44:606–7.
- Jesus LE, Bragança JJ, Rocha JM, Dekermacher S, Anderson KM. Penile hair tourniquet resulting in hypospadias failure. Indian J Urol. 2014;30(3):345–347. doi:10.4103/0970-1591.128508 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4120226
- King I, Lipede C, Varma S. Always read the label: a case report of a penile burn. Int Wound J. 2013 Aug. 10 (4):482-3.
- Okeke LI. Thread embedded into penile tissue over time as an unusual hair thread tourniquet injury to the penis: a case report. J Med Case Rep. 2008 Jul 16. 2:230.
- Peckler B, Hsu CK. Tourniquet syndrome: a review of constricting band removal. J Emerg Med. 2001 Apr. 20(3):253-62.
- Kerry RL, Chapman DD. Strangulation of appendages by hair and thread. J Pediatr Surg. 1973 Feb. 8(1):23-7.
- O’Gorman A, Ratnapalan S. Hair tourniquet management. Pediatr Emerg Care. 2011 Mar. 27(3):203-4.
- Bean JF, Hebal F, Hunter CJ. A single center retrospective review of hair tourniquet syndrome and a proposed treatment algorithm. J Pediatr Surg. 2015 Sep. 50 (9):1583-5.