Head and neck cancer
Head and neck cancer is cancer that arises in the head or neck region such as in the nasal cavity, sinuses, lips, mouth, salivary glands, throat, or larynx (voice box). Tobacco use, heavy alcohol use, and infection with human papillomavirus (HPV) increase the risk of head and neck cancers.
Head and neck cancers account for approximately 4% of all cancers in the United States 1. These cancers are more than twice as common among men as they are among women 2. Head and neck cancers are also diagnosed more often among people over age 50 than they are among younger people.
Researchers estimated that more than 65,000 men and women in this country would be diagnosed with head and neck cancers in 2017 2.
Types of head and neck cancer
Cancers that are known collectively as head and neck cancers usually begin in the squamous cells that line the moist, mucosal surfaces inside the head and neck (for example, inside the mouth, the nose, and the throat). These squamous cell cancers (SCCs) are often referred to as squamous cell carcinomas of the head and neck. Head and neck cancers can also begin in the salivary glands, but salivary gland cancers are relatively uncommon. Salivary glands contain many different types of cells that can become cancerous, so there are many different types of salivary gland cancer.
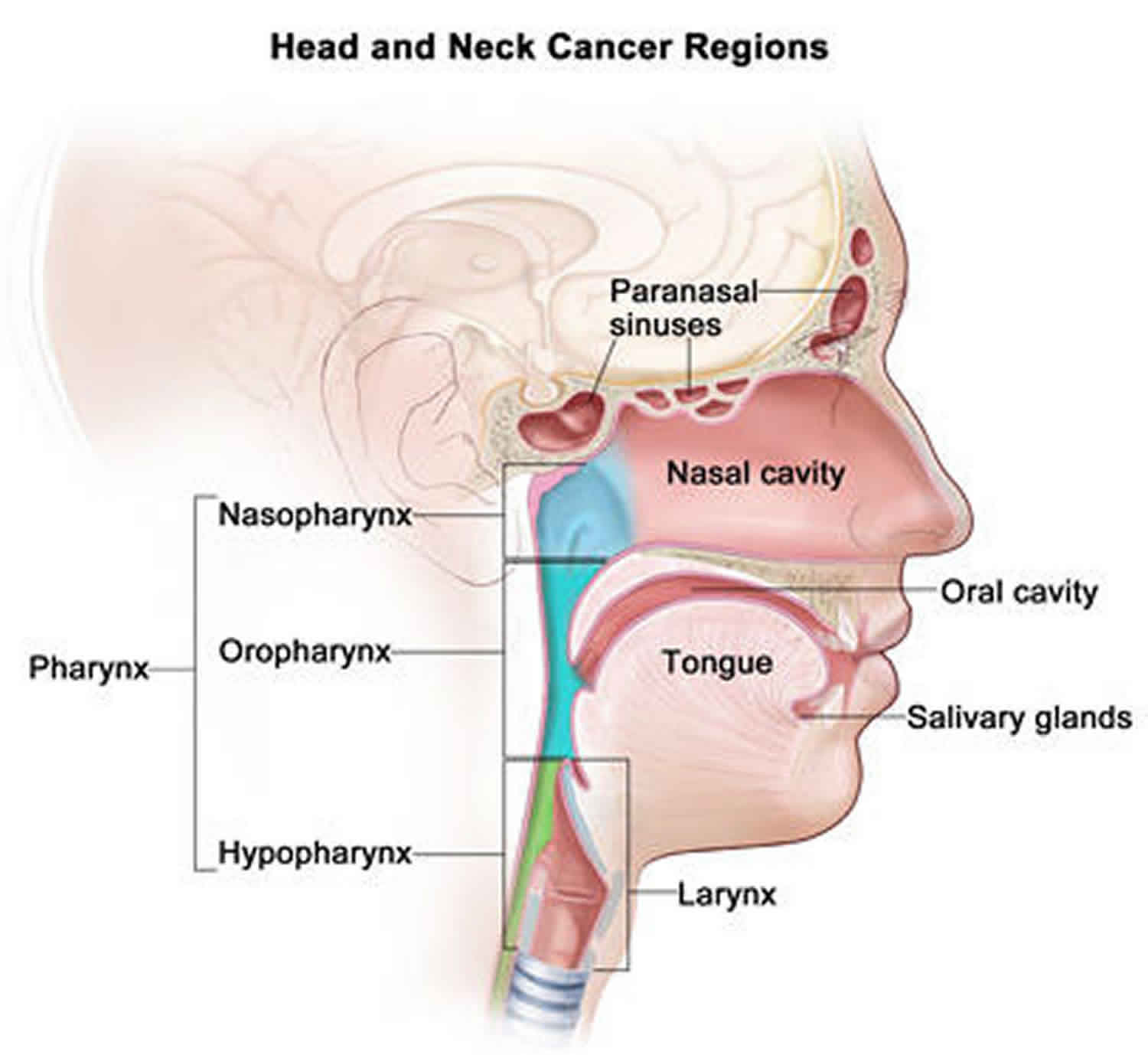
Cancers of the head and neck are further categorized by the area of the head or neck in which they begin. These areas are described below and labeled in the image of head and neck cancer regions.
- Oral cavity: Includes the lips, the front two-thirds of the tongue, the gums, the lining inside the cheeks and lips, the floor (bottom) of the mouth under the tongue, the hard palate (bony top of the mouth), and the small area of the gum behind the wisdom teeth.
- Pharynx: The pharynx (throat) is a hollow tube about 5 inches long that starts behind the nose and leads to the esophagus. It has three parts: the nasopharynx (the upper part of the pharynx, behind the nose); the oropharynx (the middle part of the pharynx, including the soft palate [the back of the mouth], the base of the tongue, and the tonsils); the hypopharynx (the lower part of the pharynx).
- Larynx: The larynx, also called the voicebox, is a short passageway formed by cartilage just below the pharynx in the neck. The larynx contains the vocal cords. It also has a small piece of tissue, called the epiglottis, which moves to cover the larynx to prevent food from entering the air passages.
- Paranasal sinuses and nasal cavity: The paranasal sinuses are small hollow spaces in the bones of the head surrounding the nose. The nasal cavity is the hollow space inside the nose.
- Salivary glands: The major salivary glands are in the floor of the mouth and near the jawbone. The salivary glands produce saliva.
Nasal and paranasal sinus cancer
Nasal and paranasal sinus cancer can start in the lining of the space behind the nose (nasal cavity) or the nearby air filled spaces within the bones close to the nasal cavity (paranasal sinuses) and sometimes spread to lymph nodes.
Cancer of the nasal cavity and sinuses is rare. Only around 400 cases are diagnosed in the UK each year. Compared with around 41,300 cases of bowel cancer diagnosed each year, you can see how rare it is.
There are different types of cancer of the lining of the space behind the nose (nasal cavity) or the nearby air cavities (paranasal sinuses). Several layers of tissue make up each part of the nasal cavity and paranasal sinuses. Each layer contains many different types of cells. Different cancers can develop from each type of cell. Recognizing these differences helps doctors decide on how best to treat the cancer.
Squamous cell cancer
Squamous cell carcinoma (SCC) is the most common type of head and neck cancer. More than 6 out of 10 (60%) of nasal cavity and paranasal sinus cancers are SCCs.
Squamous cells are the flat, skin like cells that cover the lining of the mouth, nose, larynx, thyroid and throat. Carcinoma means cancer. So squamous cell carcinoma is cancer that starts in these cells.
Squamous cell cancer is by far the most common, but not the only type of cancer that can develop in the nose and nasal sinuses.
Other types of nasal cavity and paranasal sinus cancers
- Adenocarcinomas: Adenocarcinomas are the next most common type of cancer in the nose and paranasal sinuses. It affects around 10 out of every 100 people (10%) diagnosed. The nasal and ethmoid sinuses are the most common site for adenocarcinoma of the head and neck. Adenocarcinoma starts in the gland cells (adenomatous cells). They are in the surface tissues inside the nose. These cells produce phlegm (mucus). The number of adenocarcinomas has increased in the last 20 years, but we don’t know why.
- Adenoid cystic cancers: Adenoid cystic cancers are rare cancers of gland tissue. They most often grow in the salivary glands but, much more rarely, can grow in the nose or nasal sinuses.
- Lymphomas: Lymphomas are cancers that start in the lymph nodes. There are many lymph nodes in the neck. Painless swelling of a lymph node is the most common symptom of lymphoma.
- Plasmacytomas: Plasmacytomas are tumors made up of plasma cells, and are closely related to myeloma.
- Melanomas: Melanomas develop from the pigment producing cells that give the skin its color. Melanomas of the head and neck can occur anywhere on the skin or inside the nose or mouth (oral cavity).
- Olfactory neuroblastomas: Olfactory neuroblastomas and neuroendocrine carcinomas are very rare tumors found in the nose (nasal cavity). Neuroblastomas develop in the top part of the inside of the nose from cells left behind from a baby’s development in the womb. Neuroendocrine tumours develop from specialist cells that respond to signals from other cells by producing hormones.
- Sarcomas: Sarcomas develop from the cells that make up soft tissue.
Nasal and paranasal sinus cancer causes and risk factors
Scientists do know that a few things can increase your risk, including the following:
- Smoking: Smoking increases your risk of nasal cavity cancer. If you smoke you are at a higher than average risk of developing nasal and paranasal sinus cancer. Cigarettes contain nitrosamines and other chemicals that cause cancer. When you smoke, the smoke may pass through your nasal cavity on its way to your lungs. Your risk increases the longer you smoke. If you smoke a lot, you increase your risk even more. Stopping smoking is the best thing you can do for your health and will reduce the risk of developing cancer.
- Exposure to some substances at work: Research suggests that working in some jobs increases your risk of developing cancers in the nasal cavity and paranasal sinuses. This is because they can expose you to certain chemicals. The Health and Safety Executive produced a report in 2012 that looked at whether there were particular occupations that increase the risk of nasal and paranasal cancers. They state that around a third of nasal and paranasal sinus cancers are linked to occupation.
- The following may increase your risk:
- Wood dust – people who work in carpentry, including furniture and cabinet makers, wooden floors and any other wood related industry
Leather dust – shoe makers may be exposed to leather dust - Chromium – is a chemical used in stainless steel, textiles, plastics, leather. The use of chromium is now restricted in Europe.
- Nickel – is a metal used to make stainless steel
- Formaldehyde – an industrial chemical used to make other chemicals, building materials, and household products
- Cloth fibers – people who work in the textile manufacturing may be exposed to these fibers
- Wood dust – people who work in carpentry, including furniture and cabinet makers, wooden floors and any other wood related industry
- Human papilloma virus (HPV): HPV is a common virus that can cause small growths or warts. There are lots of different strains of HPV and some are high risk for other types of cancer, such as cervical cancer. More than 1 in 5 cases of nasal and paranasal sinus cancers are linked to HPV. Of the different types of HPV, type 16 is the most common with nasal and sinus cancers.
- Radiotherapy for hereditary retinoblastoma: A long term follow up study has shown an increased risk of nasal cancer in people treated with radiotherapy for hereditary retinoblastoma compared to the general population.
- Previous non Hodgkin lymphoma: A study has shown that people who have had non Hodgkin lymphoma may have a higher risk of nasal cavity cancer compared to the general population.
There are also possible risk factors. This means some researchers suspect they may be risk factors, but there isn’t enough evidence to be sure.
Nasal and paranasal sinus cancer symptoms
There are many conditions much less serious than cancer that can cause these symptoms. But it is important that you report any of the following symptoms to your doctor.
Nose problems
Nasal and paranasal cancers may cause:
- blockages causing stuffiness in one side of your nose that does not go away
- nosebleeds
- decreased sense of smell
- mucus coming from the nose
- mucus draining into the back of your nose and throat
Most people diagnosed with cancer of the nose will have a blockage. Nosebleeds are also a common symptom.
Eye problems
People with nose and paranasal sinus cancer may notice:
- bulging of one eye
- complete or partial loss of sight
- double vision
- pain above or below the eye
- a watery eye with tears running down the cheek
Other symptoms
There are other symptoms you may have including:
- a lump or growth anywhere on the face, nose or roof of the mouth that does not go away
- pain or numbness in parts of your face, particularly the upper cheek, that doesn’t go away
- loose teeth
- difficulty opening your mouth
- swollen (enlarged) lymph nodes in your neck
- pain or pressure in one of your ears
Mouth and oropharyngeal cancer
Mouth cancer can start in different parts of the mouth, including the lips, gums or soft sides of the mouth. Oropharyngeal cancer starts in the oropharynx. The oropharynx is the part of the throat (pharynx) just behind the mouth. It includes tonsil cancer and cancer in the back part of the tongue.
Mouth and oropharyngeal cancers often start in the same type of cell. Doctors use similar tests and treatments for these cancers although there are some differences.
If your cancer started on your tongue, you might also find it useful to look at the information about tongue cancer.
Mouth and oropharyngeal cancer causes and risk factors
Scientists don’t know what causes all mouth or oropharyngeal cancers. But there are some factors that can increase your risk of developing it.
Having any of these risk factors does not mean that you will definitely develop cancer.
- Smoking: Smoking tobacco (cigarettes, pipes, cigars) increases your risk of developing mouth and oropharyngeal cancer. Research suggests that more than 60 out of 100 (more than 60%) of mouth and oropharyngeal cancers in the US are caused by smoking. There is some evidence that people exposed to second hand smoke (passive smoking) at home or in the workplace may have a small increase in their risk of mouth and oropharyngeal cancer.
- Alcohol: Drinking alcohol increases your risk of mouth and oropharyngeal cancer. Research shows around 30 out of 100 (30%) of mouth and oropharyngeal cancers are caused by drinking alcohol. Smoking and drinking together further increases the risk of cancer more than either by itself.
- Chewing tobacco or betel quid: Smokeless tobacco, including chewing tobacco, such as betel quid (gutkha) or paan is known to cause mouth and oropharyngeal cancer. It is not a safe alternative to cigarettes. In the US, it is often popular with South Asian communities.
- Diet: A diet low in fruit and vegetables may increase your risk of mouth and oropharyngeal cancer. This might be due to a lack of vitamins and minerals. A balanced diet usually means you are getting enough vitamins and minerals.
- Human papilloma virus (HPV): The human papilloma virus (HPV) is a type of virus that infects the skin and the cells lining body cavities. For most people, HPV causes no harm and gets better on its own. You don’t catch cancers like an infection. But the virus can cause changes in the mouth and throat making them more likely to become cancerous in the future. Around 70 out of 100 oropharyngeal cancers (around 70%) are linked to the human papilloma virus (HPV). This is a common virus which causes no harm in most people. But in some people, the virus can cause changes in the throat making them more likely to become cancerous in the future. HPV spreads through close skin to skin contact, usually during sexual activity. The virus is very common. But only a very small percentage of people with HPV develop mouth or oropharyngeal cancer. The risk of HPV in the mouth and throat is linked to certain sexual behaviors, such as oral sex, and having a higher number of sexual partners.
- Weak immune system: Your body’s immune system fights infection. Some illnesses and medication can weaken your immune system. Research shows an increased risk of mouth cancer if you are:
- having treatment for HIV or AIDS
- taking medicines to suppress your immune system after an organ transplant
- Sunlight and sunbeds: Too much ultraviolet (UV) radiation from the sun or sunbeds is the main cause of skin cancer. Skin cancers are relatively common on the head and neck as these areas are often exposed to UV radiation. Skin cancer can develop on the lip.
- Previous cancer: People who have had a mouth or oropharyngeal cancer have an increased risk of getting a second one. People who have the following cancers are also at increased risk of mouth and oropharyngeal cancer:
- cancer of the food pipe (oesophagus)
- squamous cell skin cancer
- cervical cancer
- penile cancer
- anal cancer
- Family history: Research shows a slight increase in risk of mouth and oropharyngeal cancer if you have a close relative (parent, sibling, or child) who has had mouth cancer. Further research is needed to understand why this is.
- Mouth conditions: Changes can happen in the cells in the lining of the mouth. They can appear as red or white patches. The red patches are called erythroplakia. White patches are called leukoplakia. In some people, these conditions may develop into cancer over some years. Doctors call these conditions pre cancerous. Dentists can spot these patches during your dental appointments, so it is important to go for regular check ups.
- Genetic conditions: People with certain conditions caused by inherited cell changes (mutations) have an increased risk of mouth and oropharyngeal cancer. These conditions include:
- Fanconi anaemia (a genetic condition affecting the bone marrow)
- dyskeratosis congenita (a condition causing changes to bone marrow, skin or fingernails)
- Blood pressure drug (hydrochlorothiazide): Hydrochlorothiazide is a drug to treat high blood pressure (hypertension). A side effect is increased sensitivity to sunlight (photo sensitivity). A small study showed this medicine might lead to an increased risk of developing lip cancer.
Cancer controversies
Stories about potential causes of cancer are often in the media and it isn’t always clear which ideas are supported by evidence. There might be things you have heard of that we haven’t included here. This is because either there is no evidence about them or it is less clear.
An example of this is teeth whiteners. Teeth whiteners have become widely used in recent years. Dentists can apply them, but some types are available for people to use at home.
There is no proof that teeth whiteners cause mouth cancer. But there has been very little research into a possible connection between the two. So you should always check first with your dentist before using these products.
Mouth and oropharyngeal cancer symptoms
Symptoms of mouth and oropharyngeal cancer and when to see your doctor.
- Ulcers that do not heal: A broken area in the lining of the mouth (ulcer) that will not heal is a common symptom of mouth cancer.
- Pain in your mouth: Pain or discomfort in your mouth that doesn’t go away is the other most common symptom of mouth cancer.
- Red or white patches in the mouth or throat: An abnormal looking patch could be a sign of cancer or precancerous changes:
- White patches are called leukoplakia.
- Red patches are called erythroplakia.
- These patches are not cancer, but if left untreated they may lead to cancer. Red and white patches in the mouth can also be caused by a fungal infection called thrush. The white patches usually rub off, leaving a sore red patch underneath. If you have anti fungal treatment, and the patches go away, they are not related to cancer.
- Difficulty swallowing: Mouth cancer can cause pain or a burning sensation when chewing and swallowing food. Or you might feel like your food is sticking in your throat. Difficulty swallowing can also be caused by a narrowing of the foodpipe (esophagus).
- Speech problems: Cancer in your mouth or throat can affect your voice. Your voice might sound different. It may be quieter, husky, or sound as if you have a cold all the time. Or you might slur some of your words, or have trouble with pronouncing some sounds.
- A lump in your neck: You may have a lump in your neck caused by an enlarged lymph node. Swelling in one or more lymph nodes in the neck is a common symptom of mouth and orpharyngeal cancer. A hot red painful lump usually means an infection, rather than a cancer. Lumps that come and go are not usually due to cancer. Cancer usually forms a lump that slowly gets bigger.
- Weight loss: Weight loss is a common symptom of many different types of cancer. Mouth and oropharyngeal cancer can make it painful to eat and difficult to swallow. This might cause weight loss. Extreme weight loss (when you are not dieting) can be a sign of advanced cancer.
- Bad breath: Most people have bad breath at some point in their life and it is not cancer. But if you have cancer, bad breath might be worse and happen more often.
- Other symptoms. These can include one or more of the following:
- a lump or thickening of your lip
- a lump in your mouth or throat
- unusual bleeding or numbness in your mouth
- loose teeth for no clear reason
- difficulty moving your jaw.
You should see your doctor if you have:
- an ulcer in your mouth that will not heal
- pain or discomfort in the mouth that will not go away
- symptoms that are unusual for you
- symptoms that don’t go away
Your symptoms are unlikely to be cancer but it is important to get them checked by a doctor.
Nasopharyngeal cancer
Nasopharyngeal cancer is a cancer that begins in the part of your throat called the nasopharynx. The nasopharynx connects the back of your nose to the back of your mouth. Nasopharyngeal cancer most commonly starts in the squamous cells that line the nasopharynx.
Nasopharyngeal cancer is more common in some ethnic groups (having Chinese or Asian ancestry) living in the US. For example in people of Chinese origin. It is also more common in men than women.
Nasopharyngeal cancer causes and risk factors
The risk factors for nasopharyngeal cancer are:
Infection
You can’t catch cancer, but some viruses can increase the risk of developing cancer. Epstein Barr virus (EBV) is a very common virus that can increase the risk of nasopharyngeal cancer. Most people carry EBV and it does them no harm. This virus is linked to other cancers including Hodgkin lymphoma and Burkitt’s lymphoma, which is a type of non Hodgkin lymphoma.
Epstein Barr virus (EBV) can cause genetic changes in cells that make them more likely to become cancerous in the future. 8 in 10 cases of nasopharyngeal cancer are caused by EBV. But many people will be infected with EBV and not develop cancer.
Smoking
People who have ever smoked are at an increased risk of nasopharyngeal cancer. The risk is higher in long term smokers.
Diet
Certain foods might increase your risk of nasopharyngeal cancer. Nasopharyngeal cancer is more common in parts of Asia and Northern Africa than it is in Europe. Diets very high in salt cured meats and fish or pickled foods are more common in some of these places. These foods can be very high in nitrates and nitrites, which react with protein to form nitrosamines. These chemicals can damage DNA.
Studies in Asia have shown that people who eat Chinese cured and salted fish are at an increased risk of nasopharyngeal cancer. People from China, or with Chinese ancestry living in the US, have higher rates of nasopharyngeal cancer than other ethnic groups. This might be due to their diet.
There is also some evidence that eating lots of fruit and vegetables could decrease the risk of nasophayngeal cancer.
Inherited risk
The risk of nasopharyngeal cancer is higher in people who have a close relative who has had it. This increased risk might be due to inherited genes as well as shared environmental and lifestyle factors.
Occupational risk
People exposed to wood dust through their work have an increased risk of nasopharyngeal cancer. We don’t know exactly how it increases cancer risk, but it could be from breathing in chemicals from treated wood.
People exposed to formaldehyde also have an increased risk of nasopharyngeal cancer. Formaldehyde is an industrial chemical used to make other chemicals and building materials.
Ear, nose and throat conditions
People who have had long term (chronic) ear, nose and throat conditions in the past might have an increased risk of nasopharyngeal cancer. These conditions include a chronic blocked and runny nose (rhinitis), middle ear infections (otitis media) and polyps. This is very rare.
Alcohol
There is some research that suggests drinking alcohol can increase the risk of nasopharyngeal cancer, but the evidence isn’t clear. However drinking alcohol can lead to other head and neck cancers.
Other possible causes
Stories about potential causes of cancer are often in the media. It isn’t always clear which ideas are supported by good evidence.
You might hear about possible causes we haven’t included here. This is because there is no evidence about them or because it is not clear what the available evidence shows.
Nasopharyngeal cancer symptoms
Some people with nasopharyngeal cancer have no symptoms at all. But it is important that you tell your doctor if you have any of the following symptoms:
- a lump or growth anywhere in the neck area that does not go away after 3 weeks (this might be the only sign you have)
- hearing loss – usually on one side only
- ringing in your ears (tinnitus)
- fluid collecting in your ear (glue ear)
- blocked or stuffy nose – particularly if it’s only blocked on one side
- blood stained discharge from your nose and nosebleeds
- headaches
- double vision
- numbness of the lower part of your face
- difficulty with swallowing
- changes in your voice, such as hoarseness
- weight loss
Tell your doctor if you have any of these symptoms, particularly if they have lasted for more than 3 weeks.
Your symptoms are unlikely to be cancer. But it’s important to get them checked by a doctor.
The earlier a cancer is picked up, the easier it is to treat. And the more likely it is that the treatment will be successful.
If your doctor suspects your symptoms could be because of nasopharyngeal cancer they will refer you to a specialist.
Laryngeal cancer
Laryngeal cancer is a rare cancer that starts in the larynx (voice box). Laryngeal cancer is a rare type of head and neck cancer. Laryngeal cancer is more common in men than in women. It is diagnosed in more than 5 times as many men as women. As with most cancers, laryngeal cancer is more common in older people than in younger people. There are very few cases in people under 40 years of age.
Laryngeal cancer causes and risk factors
There are some factors that are known to increase your risk. Having any of the below risk factors doesn’t mean that you’ll definitely develop laryngeal cancer.
Risk factors for laryngeal cancer include:
- Age: As with most cancers, laryngeal cancer is more common in older people than younger people. There are very few cases in people under 40 years of age.
- Smoking: When you smoke, it passes through the larynx on its way to your lungs. This smoke contains harmful chemicals. Smoking tobacco (cigarettes, pipes, cigars) increases your risk of developing laryngeal cancer. It is one of the main risk factors for laryngeal cancer in the western world. Your cancer risk increases the longer you smoke and the more cigarettes smoked per day.
- Drinking alcohol: Drinking alcohol increases your risk of laryngeal cancer. Smoking and drinking together further increases your risk of cancer.
- Diet: There is some evidence to suggest a diet low in fruit and vegetables may increase your risk of laryngeal cancer.
- HPV infection: HPV stands for human papilloma virus. Some research has suggested that HPV is linked to laryngeal cancer but more research is needed. HPV is a common infection and for most people it doesn’t cause any problems and goes away on its own.
- Family history: People who have a first degree relative diagnosed with a head and neck cancer have an increased risk of laryngeal cancer of someone without a family history. A first degree relative is a parent, brother, sister or child.
- Low immunity: Your body’s immune system fights infection. Some illnesses and medications can weaken your immune system. Research shows there may be an increased risk of laryngeal cancer if you:
- have HIV or AIDS
- are taking medication to suppress your immune system after an organ transplant
- Exposure to substances: Some chemicals may increase your risk of laryngeal cancer. You may have an increased risk if you have been regularly exposed over some years to high levels of:
- wood dust
- soot or coal dust
- paint fumes
- coal as a fuel source
- The chemicals in these substances can irritate the lining of your larynx. If these irritants are around you, you’re likely to breathe in and swallow small amounts.
- You also have a higher risk or laryngeal cancer if you are exposed to these chemicals:
- formaldehyde
- nickel
- isopropyl alcohol
- sulphuric acid mist
- diesel fumes
- asbestos
- But only a small number of cases of laryngeal cancer are caused by factors such as these.
Other possible causes
Stories about potential causes are often in the media. It isn’t always clear which of the ideas reported are supported by good evidence. You might have heard about a possible cause which we haven’t included here. This is because there is either no evidence to support it, or that what the evidence shows is not fully clear.
Laryngeal cancer symptoms
Having a hoarse voice for more than 3 weeks is one of the most common symptoms of laryngeal cancer. Other symptoms include difficulty swallowing, weight loss, a cough that doesn’t go away and shortness of breath.
You should see your doctor if you have a hoarse voice for more than 3 weeks. Remember that it’s more likely to be due to a cough or irritation than cancer.
The earlier a cancer is picked up, the easier it is to treat it and the more likely the treatment is to be successful. So it is important that you go to your doctor as soon as possible if you notice worrying symptoms.
Hoarseness or a change in your voice
If you have a hoarse voice for more than 3 weeks, it could be a sign of laryngeal cancer.
This is one of the most common symptoms. But many other things can cause a hoarse voice. One of the most common causes is acute laryngitis (inflammation of the larynx). This usually happens due to a cold, a chest infection or over use of the voice, such as shouting or screaming.
Smoking can also cause hoarseness because it irritates the throat lining (mucous membranes). Other causes of hoarseness include:
- acid reflux
- post nasal drip
- allergies
- thyroid problems
- injury
Many people develop hoarseness as they get older.
Acid reflux is acid leaking from your stomach up into your esophagus (food pipe). It can cause hoarseness, as stomach acid comes back up the esophagus and irritates the larynx.
Post nasal drip means mucus dripping from the back of your nose down into your throat. This can happen if you have a cold, an allergy or because you smoke. It makes you cough and can give you a hoarse voice.
Difficulty in swallowing
There are many different ways this can affect you. You might get the feeling:
- that there is something small stuck in your throat
- you are completely unable to swallow food
- of some pain or a burning sensation when swallowing food
- that your food is sticking in your throat
If you experience any of these symptoms for more than a few weeks, then you need to see your doctor for advice and further tests.
Weight loss
Weight loss is a common symptom of many cancers, including advanced laryngeal and hypopharyngeal cancer. It is very unlikely to be the only symptom.
It may happen because you’re eating less due to pain or difficulty in swallowing.
You should see your doctor if you have lost 4 to 5 kg (10lbs) or more in a short time and you are not dieting.
Cough and shortness of breath
Some people find they have a cough that doesn’t go away or they find it difficult to breath. Their breathing may become noisy (stridor).
Shortness of breath and stridor is a serious symptom that should not be ignored. You need to see your doctor urgently.
Other symptoms
Other symptoms include:
- a feeling that there’s a lump in your throat
- bad smelling breath (halitosis)
- an ear ache that doesn’t go away (this is rare)
You should see your doctor if you:
- have a hoarse voice for more than 3 weeks
- have lost 4 to 5 kg (10lbs) or more in a short time and you are not dieting
- are short of breath or have a cough that doesn’t go away, or your breathing becomes noisy (stridor)
- have difficulty swallowing
- have any other symptoms that are unusual for you or that don’t go away
Your symptoms are unlikely to be cancer but it’s important to get them checked by a doctor.
Esophageal cancer
Esophageal cancer is when abnormal cells in the food pipe (esophagus) grow in an uncontrolled way. The esophagus is also known as the gullet. It is the tube that carries food from your mouth to your stomach. Most people are over the age of 60 when they are diagnosed.
The wall of the esophagus is made of several layers of tissue. These include the inner layer (mucosa), muscle, and connective tissue. Esophageal cancer starts in the inner lining of the esophagus and spreads outward through the other layers.
Esophageal cancer cell type
There are 2 main types of cell lining the esophagus:
- squamous cells
- glandular (adenomatous) cells
Esophageal cancer can start in either type of cell. So there are 2 main types of esophageal cancer
- squamous cell carcinoma and
- adenocarcinoma.
Esophageal cancer is more common in men than women. It’s more common in older people. On average each year around 40 out of 100 (around 40%) of new cases are in people aged 75 and over. It’s very rare in people younger than 40.
Esophageal cancer causes and risk factors
Your risk of developing esophageal cancer depends on many things including your age, lifestyle and other medical conditions.
Anything that can increase your risk of cancer is called a risk factor. Those that lower the risk are called protective factors.
Having one or more risk factors doesn’t mean that you will definitely get esophageal cancer.
Age
Cancer of the esophagus is more common in older people. Around 40 out of 100 esophageal cancers (around 40%) develop in people aged 75 and over.
Being overweight or obese
Obesity means being very overweight with a body mass index (BMI) of 30 or higher.
Try to maintain a healthy weight by being active and eating a healthy diet.
Being overweight or obese increases your risk of getting esophageal cancer. More than 25 out of 100 esophageal cancers (more than 25%) are caused by being overweight or obese. The more overweight you are the higher your risk.
Smoking or using tobacco
Your risk increases the longer you smoke. It’s never too late to give up but the sooner you stop, the better.
Smoking increases your risk of the 2 main types of esophageal cancer – squamous cell cancer and adenocarcinoma. Around 35 out of 100 esophageal cancer cases (around 35%) are caused by smoking.
Smoking and drinking together further increases the risk of some esophageal cancers more than either by itself.
You also have an increased risk of esophageal cancer if you:
- chew tobacco
- chew areca nut
- use snuff
- use betel quid (paan or pan)
Alcohol
Your risk increases if you drink more than 14 units of alcohol a week. The less you drink, the lower your risk of developing cancer.
Drinking alcohol increases your risk of squamous cell esophageal cancer. Your risk is higher if you drink and smoke but your risk reduces after you stop smoking or drinking.
Diet
You should eat at least 5 portions of fresh fruit and vegetables every day.
Not eating enough fruit and vegetables may increase your risk of getting esophageal cancer.
Barrett’s esophagus
Barrett’s esophagus increases your risk of oesophageal cancer, although the risk is still small.
Barrett’s esophagus is a condition where the cells lining your esophagus have become abnormal. This can happen due to long term acid indigestion (acid reflux). Not everyone with Barrett’s esophagus has reflux.
Between 3 and 13 people out of 100 (between 3 and 13%) with Barrett’s esophagus will develop esophageal adenocarcinoma.
Your risk is affected by how long the area of Barrett’s is and how abnormal the cells look. People with longer areas of Barrett’s or very abnormal cells have a higher risk than people with shorter areas or less abnormal cells.
Medical conditions
Gastroesophageal reflux disease (GERD) increases your risk of developing esophageal adenocarcinoma. The longer you’ve had symptoms, the higher your risk.
GERD is a common condition where stomach acid flows back into the esophagus from the stomach. This is called acid reflux. Symptoms include chronic heartburn and indigestion.
Radiotherapy
Radiotherapy for other cancers slightly increases your risk of oesophageal cancer, including:
- breast cancer
- lung cancer
- oropharyngeal cancer
- laryngeal cancer
Your risk of getting esophageal cancer is still small. You would be at a higher risk from your existing cancer if you didn’t have the radiotherapy your doctor recommends.
Very hot drinks
Your risk of developing esophageal cancer is increased if you drink tea, coffee or other drinks at hot temperatures.
Esophageal cancer symptoms
The most common symptoms of esophageal cancer include:
- difficulty swallowing (dysphagia)
- indigestion or heartburn that don’t go away
- weight loss
- pain in your throat or behind your breastbone
- a cough that won’t go away
There are many other conditions that cause these symptoms. Most of them are much more common than esophageal cancer.
You should see your doctor if you have difficulty swallowing, or you have symptoms that are unusual for you or that won’t go away. Your symptoms are unlikely to be cancer but it is important to get them checked by a doctor.
Difficulty swallowing (dysphagia)
You may feel pain or a burning sensation when you swallow, or your food may stick in your throat or chest. This is the most common symptom of esophageal cancer.
A harmless narrowing of the esophagus called a stricture can also make it difficult for you to swallow. It is important to get this symptom checked by your doctor.
Indigestion or heartburn that don’t go away
You can get indigestion when acid from your stomach goes back up (refluxes) into the esophagus. Or when the stomach is inflamed or irritated.
The valve between the stomach and esophagus normally stops this from happening. The valve is called the cardiac sphincter. A tumour that develops here can stop the valve working, causing indigestion.
Remember that indigestion is common and it’s not usually caused by cancer. It can be very painful, even when there’s nothing seriously wrong.
See your doctor if you’ve had heartburn most days for 3 weeks or more, even if you’re taking medicine and it seems to help. Heartburn is burning chest pain or discomfort that happens after eating.
Weight loss
You may be put off eating if you find it hard to swallow or have pain when you swallow your food. This can make you lose weight. Rarely, extreme weight loss can be a sign of an advanced cancer.
Pain in your throat or behind your breastbone
You may feel pain in the centre of your chest, or more rarely in your back or shoulder. This can get worse when you swallow or have indigestion.
A cough that won’t go away
A cough that won’t go away or that happens when you try to eat can be caused by esophageal cancer.
Other symptoms
Other symptoms can include:
- Food coming back up: You may regurgitate food – this is when food comes back up soon after you swallow it. It usually starts with food like meat and bread. You may start to bring up soft foods such as mashed potato, drinks and saliva if you don’t have treatment.
- Hoarseness: Your voice can become raspy or croaky. It’s not a common symptom and can be caused by other harmless conditions.
- Coughing up blood: You may cough up blood or have blood in your vomit (or food that you bring back up) if your esophagus is bleeding. This isn’t common.
- Dark poop: Your poo may be darker – almost black – if cancer is making your esophagus bleed. This is uncommon. You can get darker poo if you’re taking iron tablets.
Salivary gland cancer
Salivary gland cancer can start in any of the glands that make spit (saliva). As well as 3 major pairs of salivary glands we have over 600 smaller, minor salivary glands throughout the lining of the mouth and throat.
Most salivary gland cancers start in the parotid glands. Around 8 in 10 (around 80%) salivary gland cancers start here. Just over 1 in 10 (just over 10%) start in the submandibular glands. The rest start in either the sublingual glands or the minor glands.
It is much more common to have a non cancerous (benign) lump in these glands, than cancer. Around 3 out of 4 tumours in the parotid gland (around 75%) are benign. Around half (around 50%) of the tumours found in the submandibular glands are benign.
Sublingual gland tumors are very rare, but are often cancer.
Salivary gland cancer is a very rare cancer. It is slightly more common in men than women. The number of people getting salivary cancer has remained stable in recent years.
Scientists don’t know what causes salivary gland cancer but several factors can increase your risk.
Salivary gland cancer causes and risk factors
Scientists don’t know what causes salivary gland cancer but several factors can increase your risk.
Age
Your risk of getting salivary gland cancer increases as you get older. Most people who develop it are in their 50s or 60s. Remember, the risk is still small because this is a rare cancer. For most cancers, the biggest risk factor is getting older.
Being exposed to radiation
You are at higher risk of developing salivary gland cancer if you have been exposed to radiation. This may be because you had radiotherapy to your head or neck for another type of cancer. Or you may have previously come into contact with radioactive substances through your work.
There is some evidence of risk from radioiodine therapy, which is an effective type of internal radiotherapy treatment for thyroid cancer.
Having radiotherapy for a childhood cancer may increase the risk of salivary gland cancer for at least 20 years after treatment.
Previous cancer
If you have had Hodgkin lymphoma in the past, you have an increased risk of cancer of the salivary glands.
Family history
Your risk of developing salivary cancer may be increased if someone else in your family has had it.
This may be due to lifestyle factors that are common within families and not necessarily anything to do with a genetic link. More research is needed to work out how strong the link might be.
Other possible causes
Stories about potential causes are often in the media and it isn’t always clear which ideas are supported by evidence. There might be things you have heard of that we haven’t included here. This is because either there is no evidence about them or it is less clear.
Salivary gland cancer symptoms
The most common symptom is a lump or swelling on or near your jaw, or in your mouth or neck. This is often slow growing and not painful. Remember this is a rare cancer and a lump in this area doesn’t necessarily mean you have cancer.
Overall, around 3 out of 4 tumours of the salivary gland (75%) are benign (non cancerous). But this might be different for some rarer types of salivary gland cancers.
Other symptoms
Apart from lump or swelling in the jaw area or in the mouth or neck other symptoms include:
- numbness in a part of your face
- drooping on one side of your face (facial palsy)
- pain in the area of the lump or swelling
- problems swallowing
- difficulty opening your mouth fully
- swelling on one side of your face
You should have a check up with your doctor if you have any of these symptoms. Remember all these symptoms can be caused by conditions other than cancer.
If it is cancer, the sooner it is diagnosed the better. And if it isn’t a cancer, there might well be treatment that will relieve or cure your symptoms.
Tonsil cancer
Cancer of the tonsil develops in the part of the throat just behind your mouth, called the oropharynx. It is a type of head and neck cancer. The main risk factors for tonsil cancer are smoking, drinking alcohol and infection with the HPV virus.
Most tonsil cancers are a type called squamous cell carcinoma. A small number of tonsil cancers are lymphomas.
Tonsil cancer causes and risk factors
The main risk factors for developing tonsil cancer are:
- smoking
- regularly drinking a lot of alcohol
- infection with a virus called human papilloma virus (HPV)
If you smoke and drink a lot together, you increase your risk even further.
There are many types of HPV. Tonsil cancer is especially linked to type 16. HPV is a sexually transmitted infection. It is very common. For many people, HPV causes no harm and goes away without treatment. Only a very small number of people with HPV develop tonsil cancer.
Tonsil cancer symptoms
Symptoms often include a painless neck lump and a sore throat.
Tonsil cancer symptoms can include:
- a sore throat
- ear pain
- a painless lump in your neck
- difficulty swallowing
Tongue cancer
Tongue cancer is classed as a mouth or oropharyngeal cancer, depending on where the cancer develops on the tongue. Tongue cancer symptoms can include a patch, spot or lump on your tongue that doesn’t go away. The main risk factors are smoking, drinking a lot of alcohol and infection with the HPV virus.
The most common type of tongue cancer is squamous cell carcinoma (SCC). Squamous cells are the flat, skin like cells that cover the lining of the mouth, nose, larynx, thyroid and throat. Squamous cell carcinoma is the name for a cancer that starts in these cells.
Treatments include surgery, radiotherapy and chemotherapy.
Tongue cancer causes and risk factors
Scientists don’t know the exact causes of most head and neck cancers, but several risk factors have been identified.
Smoking tobacco (cigarettes, cigars and pipes) and drinking a lot of alcohol are the main risk factors for cancers of the head and neck in the western world. The HPV virus transmitted through sexual contact is another risk factor.
Having a risk factors means that your risk is increased. But it does not mean that you will definitely develop cancer.
Tongue cancer symptoms
The symptoms of tongue cancer might include:
- a red or white patch on the tongue that won’t go away
- a sore throat that doesn’t go away
- a sore spot (ulcer) or lump on the tongue that doesn’t go away
- pain when swallowing
- numbness in the mouth that won’t go away
- unexplained bleeding from the tongue (that’s not caused by biting your tongue or other injury)
- pain in the ear (rare)
It’s important to remember that these symptoms might be due to a less serious medical condition. But it’s best to check symptoms with your doctor just to make sure.
Head and neck cancer causes
Alcohol and tobacco use (including smokeless tobacco, sometimes called “chewing tobacco” or “snuff”) are the two most important risk factors for head and neck cancers, especially cancers of the oral cavity, oropharynx, hypopharynx, and larynx 3. At least 75% of head and neck cancers are caused by tobacco and alcohol use 4. People who use both tobacco and alcohol are at greater risk of developing these cancers than people who use either tobacco or alcohol alone 5. Tobacco and alcohol use are not risk factors for salivary gland cancers.
Infection with cancer-causing types of human papillomavirus (HPV), especially HPV type 16, is a risk factor for some types of head and neck cancers, particularly oropharyngeal cancers that involve the tonsils or the base of the tongue 6. In the United States, the incidence of oropharyngeal cancers caused by HPV infection is increasing, while the incidence of oropharyngeal cancers related to other causes is falling 6.
Other risk factors for cancers of the head and neck include the following:
- Paan (betel quid). Immigrants from Southeast Asia who use paan (betel quid) in the mouth should be aware that this habit has been strongly associated with an increased risk of oral cancer 7.
- Preserved or salted foods. Consumption of certain preserved or salted foods during childhood is a risk factor for nasopharyngeal cancer 8.
- Oral health. Poor oral hygiene and missing teeth may be weak risk factors for cancers of the oral cavity (16, 17). Use of mouthwash that has a high alcohol content is a possible, but not proven, risk factor for cancers of the oral cavity 9.
- Occupational exposure. Occupational exposure to wood dust is a risk factor for nasopharyngeal cancer 10. Certain industrial exposures, including exposures to asbestos and synthetic fibers, have been associated with cancer of the larynx, but the increase in risk remains controversial 11. People working in certain jobs in the construction, metal, textile, ceramic, logging, and food industries may have an increased risk of cancer of the larynx 12. Industrial exposure to wood or nickel dust or formaldehyde is a risk factor for cancers of the paranasal sinuses and nasal cavity 13.
- Radiation exposure. Radiation to the head and neck, for noncancerous conditions or cancer, is a risk factor for cancer of the salivary glands 14.
- Epstein-Barr virus infection. Infection with the Epstein-Barr virus is a risk factor for nasopharyngeal cancer 15 and cancer of the salivary glands 16.
- Ancestry. Asian ancestry, particularly Chinese ancestry, is a risk factor for nasopharyngeal cancer 8.
Head and neck cancer prevention
People who are at risk of head and neck cancers, particularly those who use tobacco, should talk with their doctor about ways that they may be able to reduce their risk. They should also discuss with their doctor how often to have checkups. In addition, ongoing clinical trials are testing the effectiveness of various medications in preventing head and neck cancers in people who have a high risk of developing these diseases.
Avoiding oral HPV infection may reduce the risk of HPV-associated head and neck cancers. However, it is not yet known whether the Food and Drug Administration-approved HPV vaccines Gardasil®, Gardasil 9®, and Cervarix® prevent HPV infection of the oral cavity, and none of these vaccines has yet been approved for the prevention of oropharyngeal cancer.
Head and neck cancer symptoms
The symptoms of head and neck cancers may include a lump or a sore that does not heal, a sore throat that does not go away, difficulty in swallowing, and a change or hoarseness in the voice. These symptoms may also be caused by other, less serious conditions. It is important to check with a doctor or dentist about any of these symptoms. The earlier a cancer is picked up, the easier it is to treat it and the more likely the treatment is to be successful. So it is important that you go to your doctor as soon as possible if you notice worrying symptoms. Symptoms that may affect specific areas of the head and neck include the following:
- Oral cavity. A white or red patch on the gums, the tongue, or the lining of the mouth; a swelling of the jaw that causes dentures to fit poorly or become uncomfortable; and unusual bleeding or pain in the mouth.
- Pharynx. Trouble breathing or speaking; pain when swallowing; pain in the neck or the throat that does not go away; frequent headaches, pain, or ringing in the ears; or trouble hearing.
- Larynx. Pain when swallowing or ear pain.
- Paranasal sinuses and nasal cavity. Sinuses that are blocked and do not clear; chronic sinus infections that do not respond to treatment with antibiotics; bleeding through the nose; frequent headaches, swelling or other trouble with the eyes; pain in the upper teeth; or problems with dentures.
- Salivary glands. Swelling under the chin or around the jawbone, numbness or paralysis of the muscles in the face, or pain in the face, the chin, or the neck that does not go away.
Head and neck cancer diagnosis
To find the cause of the signs or symptoms of a problem in the head and neck area, a doctor evaluates a person’s medical history, performs a physical examination, and orders diagnostic tests. The exams and tests may vary depending on the symptoms. Examination of a sample of tissue under a microscope is always necessary to confirm a diagnosis of cancer.
If the diagnosis is cancer, the doctor will want to learn the stage (or extent) of disease. Staging is a careful attempt to find out whether the cancer has spread and, if so, to which parts of the body. Staging may involve an examination under anesthesia (in an operating room), x-rays and other imaging procedures, and laboratory tests. Knowing the stage of the disease helps the doctor plan treatment.
Head and neck cancer treatments
The treatment plan for an individual patient depends on a number of factors, depends on where your cancer is, how big it is, the stage of the cancer, whether it has spread anywhere else in your body and your age and general health. A team of doctors and other professionals decide on the best treatment and care for you. Treatment for head and neck cancer can include surgery, radiation therapy, chemotherapy, targeted therapy, or a combination of treatments.
People who are diagnosed with HPV-positive oropharyngeal cancer may be treated differently than people with oropharyngeal cancers that are HPV-negative. Recent research has shown that patients with HPV-positive oropharyngeal tumors have a better prognosis and may do just as well on less intense treatment. An ongoing clinical trial is investigating this question.
Nasal and paranasal sinus cancer treatment
Early diagnosis of nasal and paranasal sinus cancer means that it will be easier to control. It is also possible to cure it at this stage. Surgery alone will cure some types, but others will respond better to radiotherapy.
Planning your treatment
Your doctor will plan your treatment according to:
- the type of cancer you have
- whether the cancer has spread (the stage)
- what the cells look like under a microscope (the grade)
- your general health
Your specialist may advise surgery as the best treatment for you. This can be because of the stage or position of your cancer. Or they might suggest that radiotherapy is better. This can be with or without chemotherapy. You may have fewer problems after treatment.
In some situations you may have a choice between types of treatment. Your doctor and specialist head and neck cancer nurse will be able to help you decide what is best for you.
You might want to get a second opinion before you have your treatment. This can give you more information. You might also feel more confident about your treatment plan. Most doctors are happy to refer you to another specialist for a second opinion.
Getting a second opinion doesn’t mean that the second doctor will take over your care. Your original specialist will usually still manage your treatment.
Surgery
Surgery is a common treatment for nasal cavity and paranasal sinus tumors. The type of operation you have will depend on the position of the cancer and its size.
For some very early stage cancers, it may be possible to remove the tumor. This can be under local or general anaesthetic using laser surgery. The surgeon uses a narrow, intense beam of light to cut out the cancer. The laser beam works like a surgical knife (scalpel).
For larger tumors you will need a bigger operation and a general anesthetic.
Your surgeon will examine the area around the tumor. They might remove some of the lymph nodes from around the tumor. This is to try and get rid of any remaining cancer cells. It also lowers the risk of the cancer coming back.
Sometimes the cancer spreads to lymph nodes in your neck. You might have all the nodes on one or both sides of your neck removed when this happens. Your doctor may call this operation a modified radical or radical neck dissection.
Radiotherapy
Radiotherapy on its own can treat some types of nasal cavity and paranasal sinus cancers. This is usually when the cancer hasn’t spread. It will cure most people with small tumors of the nose (nasal cavity).
An advantage is that you don’t have any tissue removed, so it causes less of a change to your appearance.
Your doctor may recommend that you have radiotherapy if you have an operation first. This will get rid of any remaining cancer cells and lowers the risk of the cancer coming back.
Chemotherapy
You might have chemotherapy for any of the following reasons:
- before or after surgery or radiotherapy
- to treat some cancers that have spread to other parts of the body
- if your cancer has come back after surgery and radiotherapy
- during a course of radiotherapy (chemoradiotherapy) for locally advanced cancer
Research shows that giving chemotherapy with radiotherapy (chemoradiotherapy) can work better for many people than radiotherapy on its own.
If your cancer has spread
Surgery won’t cure your cancer if it has already spread to another part of your body. It might help to control the cancer for a time and reduce symptoms.
A large cancer can start to block your airway. In these situations your doctor might recommend surgery to remove all or part of the cancer. This will make your breathing easier.
Your doctor may also suggest:
- surgery and radiotherapy together
- radiotherapy alone
- chemotherapy alone or with radiotherapy (chemoradiotherapy)
Treatments that are still in development might be another option for you. This will mean taking part in a clinical trial.
Palliative care
Your doctor is also likely to refer you to a palliative care team. They are health care professionals who specialize in people whose cancer isn’t curable.
Some people assume that they are going to die very soon when their doctor suggests cancer is not curable. This is often not the case. It also doesn’t mean that the doctors who have been caring for you up until now won’t be involved in your care.
Palliative care means:
- controlling any symptoms you have, such as pain, sickness or breathing problems
- giving treatment that can shrink the cancer and control symptoms
- supporting you with both physical care and psychological care
- ensuring that you have the best possible care in place before going home from hospital.
Mouth and oropharyngeal cancer treatment
Your treatment depends on where in your mouth or oropharynx your cancer is, how big it is, whether it has spread anywhere else in your body and your general health.
A team of doctors and other professionals discuss the best treatment and care for you. They are called a multidisciplinary team.
The treatment you have depends on:
- where your cancer is
- how far it has grown or spread (the stage)
- the type of cancer
- how abnormal the cells look under a microscope (the grade)
- your general health and level of fitness
Your doctor will talk to you about your treatment, its benefits and the possible side effects.
You might have one type of treatment or a combination of treatments. The main treatments are:
- surgery
- radiotherapy
- chemotherapy
- chemotherapy with radiotherapy (chemoradiotherapy)
- targeted cancer drugs
Surgery
Surgery is a common treatment for early stage mouth and oropharyngeal cancer. How much surgery you have depends on the size and location of your cancer. You are most likely to have an operation under general anesthetic.
Radiotherapy
You can have radiotherapy alone or together with chemotherapy. Radiotherapy alone is a treatment for some types of mouth and oropharyngeal cancer that have not spread.
You may also have radiotherapy after surgery. This is to kill any cancer cells that might have been left behind. It lowers the risk of the cancer coming back.
Chemotherapy
You may have chemotherapy if your cancer has come back. Or if your cancer has spread into surrounding tissues or to other parts of the body. Sometimes you can have it before other treatments (such as radiotherapy) to make the cancer smaller.
Chemoradiotherapy
This is chemotherapy and radiotherapy together. You may have chemoradiotherapy instead of surgery if your cancer has spread into surrounding tissues or into nearby lymph nodes. For some people, this may get rid of the cancer completely.
Targeted cancer drugs
You might have a targeted or immunotherapy cancer drugs. For example, cetuximab (also known as Erbitux) or nivolumab (Opdivo).
Treatment by stage
Your treatment depends on the stage of your cancer.
Stage 0 (carcinoma in situ)
The cancer cells are all contained within the lining of the mouth or oropharynx. If left untreated, there is a high chance of the cells developing into a cancer.
Your doctor may completely remove the cancer cells during a biopsy, if the affected area is very small. Or you may need to have minor surgery. Your doctor removes the cancer cells by taking a thin layer of tissue from the affected area.
Your doctor will monitor you closely after treatment. If the cancer cells come back, you may have radiotherapy.
If you smoke and continue to do so, it is much more likely that you will develop cancerous cells again in the future.
Stage 1 and 2
Your treatment depends on where in the mouth or oropharynx your cancer is. You might have:
- surgery
- radiotherapy
- surgery followed by radiotherapy
- chemoradiotherapy
When deciding on your treatment plan, your doctor considers the possible side effects of treatment, and your general health.
Stage 3 and 4
You might have surgery to remove the cancer. This usually includes removing some of the lymph nodes in the neck during an operation called a neck dissection. This is because there is a high risk that the cancer has spread to the lymph nodes.
You may also have radiotherapy to your neck after surgery. This is to kill off any remaining cancer cells.
When the cancer is too big or cannot be removed by surgery, you might have radiotherapy. You may have radiotherapy alongside chemotherapy or targeted cancer drugs. You might have a targeted drug on its own if chemotherapy drugs are not working.
Clinical trials
Your doctor might ask if you’d like to take part in a clinical trial. Doctors and researchers do trials to make existing treatments better and develop new treatments.
Laryngeal cancer treatment
Your treatment depends on where your cancer is, how big it is, whether it has spread anywhere else in your body and your general health.
The treatment you’ll have depends on:
- your type of laryngeal cancer
- where the cancer is in your larynx
- how far it has grown or spread (the stage)
- how abnormal the cells look under a microscope (the grade)
- your general health and level of fitness
Your doctor will discuss your treatment, its benefits and the possible side effects with you.
In some situations, you might not have a choice of treatment because it is clear which treatment will work best.
But you may be given a choice, especially if you have a small, early tumor. For example, you might be able to choose between trans-oral laser surgery (endoscopic resection) or radiotherapy. The outcomes of this type of surgery and radiotherapy are very similar.
Your doctor will discuss the risks and benefits of the different options with you.
You might have a combination of treatments. And you might need to see various people from the multidisciplinary team who specialize in different aspects of your treatment.
You can ask your doctor or nurse to introduce you to a patient who has had treatment if you think this would be helpful to you.
You might have one or more of the following treatments:
- surgery
- radiotherapy
- chemotherapy
- targeted cancer drug
Laryngeal cancer treatment by stage
Tis (Tumor in situ)
The surgeon might completely remove the abnormal area when you have the biopsy. Or you might have laser treatment.
If the cancer cells come back again you might have further laser surgery or radiotherapy.
T stage 1 and 2
Treatment might include:
- surgery using a laser to remove the cancer through your mouth (trans-oral laser surgery)
- surgery to remove part of your voice box (a partial laryngectomy)
- radiotherapy
If your cancer is above your vocal cords (supraglottis) the surgeon will do everything possible to leave the vocal cords unharmed.
If your doctor thinks there is any risk of the cancer coming back, they might offer you radiotherapy after surgery.
T stage 3
You might have chemotherapy with radiotherapy (chemoradiotherapy). There may be reasons why you can’t have chemotherapy (for example, due to other medical conditions). If this is the case, you may have a targeted cancer drug instead, or radiotherapy alone.
Instead of chemoradiotherapy, you might have surgery. The surgeon may use a laser to remove the cancer through your mouth (trans-oral laser surgery.) Or you might have surgery to remove part of your voice box (partial laryngectomy). The surgeon is also likely to remove your lymph nodes. Or you have radiotherapy to these lymph nodes.
If your cancer is in the area below your vocal cords (subglottis), you might have surgery to remove all of your voice box (total laryngectomy). You have radiotherapy afterwards to lower the risk of the cancer coming back. Or you may have radiotherapy alone.
T stage 4
You might be able to have radiotherapy with chemotherapy or a targeted cancer drug. This means you avoid surgery to remove your larynx.
But you might need surgery to remove your whole larynx (laryngectomy) and surrounding lymph nodes, followed by radiotherapy.
You might have radiotherapy and chemotherapy to shrink your cancer before surgery. Some people may not need surgery after this, so it can be kept in reserve in case the cancer comes back.
Laryngeal cancer that comes back
Your treatment depends on what treatment you had first time round.
Before treatment, your doctor might take another sample of tissue (biopsy). This is because it can sometimes be difficult to tell if a new lump in the treatment area is scar tissue or a cancer that has come back.
If your cancer comes back after radiotherapy your doctor will probably suggest surgery to remove your voicebox (total laryngectomy).
If your cancer comes back after surgery, you are most likely to have radiotherapy. You might have this alongside chemotherapy or a targeted cancer drug.
Esophageal cancer treatment
Your treatment depends on several factors. These include what type of esophageal cancer you have, how big it is and whether it has spread (the stage), and what the cancer cells look like under the microscope (grade). It also depends on your general health.
Your treatment depends on:
- where your cancer is in your food pipe
- how far it has grown or spread (the stage)
- the type of cancer
- how abnormal the cells look under a microscope (the grade)
- your general health and level of fitness
A team of health professionals will discuss your treatment, its benefits and the possible side effects with you.
The main treatments are:
- surgery
- radiotherapy
- chemotherapy
- chemoradiotherapy
You have one or more of these treatments depending on the stage of your cancer.
You might also have treatment for symptoms when you’re first diagnosed. This includes treatment to help you swallow because some cancers of the food pipe can block it. Doctors can put a small tube into your esophagus (stent) to clear the blockage so you can swallow. Treatment for eating problems helps to make you fit enough for your cancer treatment.
If you’re not having surgery
Health problems might mean you can’t have surgery, or you could decide you don’t want it. You have tests to check how fit you are before you have any treatment including heart and lung tests.
When surgery isn’t possible, you might have one or more of these treatments
- chemotherapy
- radiotherapy
- chemoradiotherapy – chemotherapy with radiotherapy
- symptom control
Esophageal cancer treatment by stage
Stage 0 cancer
Removing the lining of your esophagus is the main treatment.
You have this surgery through a tube called an endoscope. This surgery is endoscopic mucosal resection or removing the lining of the esophagus.
You might also need treatment to destroy any abnormal areas that the doctor couldn’t remove. This includes photodynamic therapy (PDT), which is also called light treatment.
Stage 1 cancer
Surgery is the main treatment.
You might also need these treatments before and after surgery:
- chemotherapy
- chemoradiotherapy
Stage 2 and 3 cancers
For cancers in the lower part of the esophagus you have either:
- chemotherapy
- chemoradiotherapy
You then have surgery to remove all or part of your esophagus.
Depending on the results of your surgery, you might need more chemotherapy or chemoradiotherapy. This lowers the chances of the cancer coming back.
For cancers in the upper part of the esophagus you usually have chemoradiotherapy, without surgery.
Stage 4 cancer
Treatment aims to control the cancer and maintain a good quality of life. You might have
- chemotherapy
- radiotherapy
- symptom control eg. treatment to help you swallow food
- trastuzumab (Herceptin) biological therapy for cancers in the gastro esophageal junction area and the cells have HER2 protein
Clinical trials
Doctors are always looking to improve treatments for esophageal cancer, and reduce side effects. As part of your treatment, your doctor may ask you to take part in a clinical trial. This might be to test a new treatment or to look at different combinations of existing treatments.
Salivary gland cancer treatment
Treatment for salivary gland cancer depends on where the cancer is, its size, whether it has spread anywhere else and your health. Surgery and radiotherapy are the main treatments for salivary gland cancer. Chemotherapy is usually only used as a treatment for advanced salivary gland cancers.
Surgery alone will cure some salivary gland cancers. For other cancers, a combination of surgery and radiotherapy will work better. Doctors might use chemotherapy to control more advanced cancers or as part of a clinical trial.
Your doctor will plan your treatment according to:
- the type of salivary gland cancer you have
- whether the cancer has spread (the stage)
- what the cells look like under a microscope (the grade)
- how the treatment will affect your speech, chewing and swallowing
- your general health and fitness
Surgery
Surgery is the most common treatment for salivary gland cancer. It works very well for early stage cancers.
The type of operation you have depends on:
- the size of the cancer
- where it is – it can be harder to remove a cancer in the deeper parts of the salivary gland
- whether there is a risk that the cancer has spread to the lymph nodes around your salivary gland or in your neck
Surgery to remove the lymph nodes in your neck
During surgery, the doctor will examine the area around your cancer. They may remove some of the lymph nodes near the tumour. This is called a selective neck dissection.
Your surgeon does this to help to find out where the cancer is (the stage) and to get rid of any remaining cancer cells. This reduces the risk of the cancer coming back in the lymph nodes.
Your surgeon is likely to remove all the nodes on one, or both sides of your neck if your cancer has already spread to lymph nodes in the neck. You may hear your doctor call this operation a modified radical neck dissection.
Radiotherapy
Radiotherapy uses high energy rays to kill cancer cells. Your doctor may recommend that you have radiotherapy after surgery. This helps to kill any cancer cells that might have been left behind and reduces the risk of the cancer coming back.
You might also have radiotherapy as the main treatment if it isn’t possible to remove your cancer in an operation. You may not be able to have surgery because:
- the position of your tumor makes it difficult to reach
- you have other illnesses or conditions and you can’t have a long anaesthetic
- the cancer is advanced and can’t be completely removed
Chemotherapy
Chemotherapy uses anti cancer (cytotoxic) drugs to disrupt and kill cancer cells. Chemotherapy doesn’t work as well as surgery and radiotherapy for salivary gland cancer. So this isn’t a common treatment.
You may have chemotherapy:
- to treat advanced cancers, or those that have spread to other parts of your body
- if your cancer has come back after surgery and radiotherapy
- as part of a clinical trial
Advanced salivary gland cancer
Salivary gland cancer can spread to other parts of the body. This is advanced cancer. When this happens, using surgery to remove the tumour in your salivary gland will not cure the cancer. But surgery may still help to control your symptoms and the disease for some time.
Your doctor might recommend surgery to remove all or part of the cancer and help relieve symptoms if your tumour is large. They may also suggest radiotherapy and chemotherapy.
Tongue cancer treatment
The main treatments for tongue cancer are surgery, radiotherapy and chemotherapy, either combined or on their own. Your treatment depends on how far your cancer has grown and whether it has spread (the stage). It also depends on which part of the tongue is affected.
Treating the oral tongue cancer
The front two thirds of the tongue (oral tongue) are treated like a mouth cancer.
Early stage
Early cancer means your cancer is smaller than 4cm and is contained within the tongue.
The most common treatment is surgery to remove the affected area. You might also have surgery to remove lymph nodes in your neck.
Advanced stage
Advanced cancer means your cancer is larger than 4cm. Or it has grown outside the tongue, invading other tissues or lymph nodes. You are most likely to have a combination of all of these treatments:
- surgery to remove the cancer from your tongue and the lymph nodes in your neck
- reconstructive surgery
- radiotherapy after surgery – this might be combined with chemotherapy (chemoradiotherapy)
You might have chemotherapy if your cancer has come back. Or if your cancer has spread into surrounding tissues or to other parts of the body.
Treating the back of the tongue cancer
The back third of the tongue (base of the tongue) is treated like oropharyngeal cancer. Oropharyngeal cancer starts in the part of the throat just behind the mouth.
Early cancer
Early cancer means your cancer is smaller than 4cm and is contained within the tongue.
You might have either:
- surgery to remove the cancer and some of the lymph nodes in your neck
- radiotherapy to the throat and neck
You might need radiotherapy or chemoradiotherapy after surgery if your doctor thinks there is a high risk that your cancer will come back. Chemoradiotherapy means you have chemotherapy and radiotherapy together.
Advanced cancer
Advanced cancer means your cancer is larger than 4cm. Or it has grown outside the tongue, invading other tissues or lymph nodes.
You might have one of the following:
- chemotherapy and radiotherapy together (chemoradiotherapy) to your throat and neck
- surgery to remove part of the throat (including all or part of the tongue) and some of the lymph nodes in your neck, followed by radiotherapy or chemoradiotherapy
- radiotherapy on its own
You might have radiotherapy, chemotherapy or surgery to control symptoms of advanced cancer.
Surgery
Your surgeon removes the cancer and an area (margin) of normal tissue around it. This helps to make sure that they have removed all the cancer. The operation is called a primary tumour resection. There are different types of primary tumour resection. It depends on the location of your cancer.
You might only need a simple operation if the cancer is very small. This can be done using local anaesthetic or with laser surgery, and you don’t need to stay overnight in hospital.
For larger cancers, you might need a more complicated operation and stay in hospital for a while. You might have an operation to remove part or all of your tongue (a glossectomy). This is quite a big operation. Your surgeon rebuilds (reconstructs) your tongue.
The surgeon usually removes the lymph nodes from one or both sides of your neck. This operation is called a neck dissection. It lowers the risk of your cancer coming back in the future.
Radiotherapy
Radiotherapy uses high energy waves similar to x-rays to kill cancer cells. You might have radiotherapy:
- on its own as your main treatment or after surgery
- combined with chemotherapy (chemoradiotherapy) as your main treatment or after surgery
- to help relieve the symptoms of advanced tongue cancer
You have radiotherapy to the part of the tongue affected by cancer. And the doctor might also treat the lymph nodes in your neck.
You usually have radiotherapy treatment once a day for a few weeks.
Chemotherapy
Chemotherapy uses anti cancer (cytotoxic) drugs to destroy cancer. You might have chemotherapy combined with radiotherapy (chemoradiotherapy). The chemotherapy helps the radiotherapy work better. You might have this:
- after surgery if there is a high risk of your cancer coming back
- as your main treatment
You usually have a PET-CT scan a few months after chemoradiotherapy. This is to check if your lymph nodes contain cancer. If there are signs of cancer, you usually have surgery to remove the lymph nodes.
Some people have chemotherapy to shrink the cancer before the main treatment, although this isn’t very common. This is called neo adjuvant treatment.
The most commonly used drug is cisplatin. You might have this with fluoracil (5FU). Some people have carboplatin instead of cispatin.
Targeted cancer drugs
Cetuximab ( Erbitux) is a type of targeted cancer drug called a monoclonal antibody. You might have cetuximab together with radiotherapy if you can’t have chemotherapy for any reason.
Nivolumab is a type of immunotherapy. This type of treatment stimulates the body’s immune system to fight cancer cells. You might be able to have nivolumab if your cancer has started to grow again within 6 months of stopping chemotherapy. To be able to have this, your doctor needs to make an individual application to a special fund called Cancer Drugs Fund.
Tonsil cancer treatment
The main treatments for tonsil cancer are surgery, radiotherapy and chemotherapy, either combined or on their own. Your treatment depends on how far your cancer has grown and whether it has spread – this is called the stage of your cancer.
The stage of your cancer also depends on whether your cancer cells contain the HPV virus.
Tonsil cancer treatment by stage
Early tonsil cancer
Early tonsil cancer means a tumour that is smaller than 4cm and is contained within the tonsil.
You might have either:
- surgery to remove the cancer and some of the lymph nodes in your neck
- radiotherapy to the throat and neck
You might need radiotherapy or chemoradiotherapy after surgery if your doctor thinks there is a high risk that your cancer will come back. Chemoradiotherapy means you have chemotherapy and radiotherapy together.
Advanced tonsil cancer
Advanced tonsil cancer means your cancer is larger than 4cm. Or it has grown outside the tonsil, invading other tissues or lymph nodes.
You might have:
- chemotherapy and radiotherapy together (chemoradiotherapy) to your throat and neck
- surgery to remove the part of the throat affected by cancer and some of the lymph nodes in your neck, followed by radiotherapy or chemoradiotherapy
- radiotherapy on its own
You might have chemotherapy before surgery if your cancer is very large, although this isn’t very common.
You usually have a PET CT scan a few months after chemoradiotherapy. This is to check if your lymph nodes contain cancer. If there are signs of cancer, you usually have surgery to remove the lymph nodes.
You might have radiotherapy, chemotherapy or surgery to control symptoms of advanced cancer.
Surgery
You might have an operation to remove the part of the throat that contains the cancer. There are different types of operation. The type of surgery depends on the site and size of your cancer.
Early cancers
You might only need a simple operation, if your cancer is very small. This can be done using local anaesthetic or with laser surgery, and you don’t need to stay overnight in hospital.
Usually surgery for early stage cancer is through your mouth (endoscopic surgery). This is also called:
- transoral laser microsurgery (TLM)
- transoral robotic surgery (TORS)
The surgeon might also remove lymph nodes in some areas of your neck. They send the nodes to the laboratory to check them for cancer cells. This is called a selective neck dissection.
If there is cancer in the lymph nodes you might need to have more surgery to remove more nodes.
Larger cancers
For larger cancers you may need a more complicated operation and need to stay in hospital for a while.
For the most complicated surgery, you might have to have part of your soft palate or the back of your tongue removed. Your surgeon rebuilds this with tissue taken from another part of the body.
Radiotherapy
Radiotherapy uses high energy waves similar to x-rays to kill cancer cells. You might have radiotherapy:
- on its own as your main treatment or after surgery
- combined with chemotherapy (chemoradiotherapy) as your main treatment or after surgery
- to help relieve the symptoms of advanced tonsil cancer
You have radiotherapy to the part of the throat affected by cancer. And the doctor might also treat the lymph nodes in your neck.
You usually have radiotherapy treatment once a day for a few weeks.
Chemotherapy
Chemotherapy uses anti cancer (cytotoxic) drugs to destroy cancer.
You might have chemotherapy combined with radiotherapy (chemoradiotherapy). The chemotherapy helps the radiotherapy work better. You might have this
- after surgery if there is a high risk of your cancer coming back
- as your main treatment
- Some people have chemotherapy to shrink the cancer before the main treatment, although this isn’t very common. This is called neo adjuvant treatment.
The most commonly used drug is cisplatin. You might have this with fluoracil (5FU). Some people have carboplatin instead of cisplatin.
Targeted cancer drugs
Cetuximab ( Erbitux) is a type of targeted cancer drug called a monoclonal antibody. You might have cetuximab together with radiotherapy if you can’t have chemotherapy for any reason.
Nivolumab is a type of immunotherapy. This type of treatment stimulates the body’s immune system to fight cancer cells. You might be able to have nivolumab if your cancer has started to grow again within 6 months of stopping chemotherapy. To be able to have this, your doctor needs to make an individual application to a special fund called Cancer Drugs Fund.
Nasopharyngeal cancer treatment
The treatment you have depends on the stage and type of your nasopharyngeal cancer. Your doctor might suggest one type of treatment or a combination of treatments.
Radiotherapy is the main treatment for nasopharyngeal cancer. You might have radiotherapy alone, or with chemotherapy (this is called chemoradiotherapy).
Surgery is not often used to treat nasopharyngeal cancer. Its mainly used when the cancer comes back after the original treatment.
Radiotherapy
Radiotherapy on its own cures most early stage nasopharyngeal cancers. This includes stage 1 nasopharyngeal cancers and some people with stage 2 cancers.
For locally advanced nasopharyngeal cancer, you usually have chemoradiotherapy.
Chemotherapy
You might have chemotherapy if nasopharyngeal cancer has spread to:
- the lymph nodes in your neck
- other parts of your body, such as the lungs or bones
You might have:
- chemotherapy together with radiotherapy (chemoradiotherapy)
- chemotherapy on its own
You might have chemotherapy before radiotherapy. This aims to shrink the tumour and make it easier to treat with radiotherapy.
You might have 2 or more chemotherapy drugs together. Using 2 or more drugs together sometimes works better than using one drug.
Chemoradiotherapy
Having chemotherapy and radiotherapy at the same time is called chemoradiotherapy. The chemotherapy makes the cancer cells more sensitive to the radiotherapy.
You might have this treatment if your cancer has grown into the tissue around the nasopharynx, or into the nearby lymph nodes.
Chemoradiotherapy can be quite a tough treatment to have. The side effects can be more severe than the side effects of radiotherapy or chemotherapy on their own. So you have tests to see if you’re fit enough to have it.
Surgery
Surgery is not a common treatment for nasopharyngeal cancer. This is because the area is very difficult to get to and is surrounded by important nerves and blood vessels. And also because the cancer responds to radiotherapy and chemotherapy.
The surgery you are most likely to have is to remove lymph nodes. You might have this if your doctor thinks they could contain cancer cells.
Your specialist might suggest surgery to remove your tumour if:
- your cancer comes back quite soon after treatment with radiotherapy
- you have a rare type of nasopharyngeal cancer such as adenocarcinoma
Clinical trials
Your doctor might ask if you’d like to take part in a clinical trial. Doctors and researchers do trials to make existing treatments better and develop new treatments.
Nasopharyngeal cancer treatment by stage
The stage of a cancer means how far it has grown and whether it has spread. It helps your doctor decide what kind of treatment would be best for you.
Stage 1
Radiotherapy is the main choice of treatment for stage 1 nasopharyngeal cancers.
With stage 1 cancers there is no sign that the cancer has spread to the lymph nodes. But you may have radiotherapy to the nodes in your neck, just in case any cancer cells have strayed there.
Stage 2
For stage 2 nasopharyngeal cancers you might have:
- radiotherapy to the tumour and the lymph nodes in your neck
- chemotherapy and radiotherapy together (chemoradiotherapy)
Stage 3 or 4
For stage 3 and stage 4A and 4B nasopharyngeal cancers, you might have:
- chemotherapy before or after chemoradiotherapy
- chemotherapy and radiotherapy together (chemoradiotherapy)
- radiotherapy to the tumour and the lymph nodes in your neck
Nasopharyngeal cancer that has come back
The treatment you might have for nasopharyngeal cancer that has come back depends on where in your body the cancer is. For cancer that has come back in the same place (called the primary site) there are several treatment options. You may have radiotherapy again. Or you might have chemotherapy on its own. In some circumstances, you might have surgery to remove the tumour.
For cancer that has come back in the lymph nodes in your neck, you are most likely to have surgery to remove them. This is called a neck dissection. You might have more radiotherapy, but this is less likely. The treatment depends on how far the cancer has spread.
For cancer that comes back in another part of your body, you are likely to have chemotherapy. You might have radiotherapy if cancer has spread to your bones.
Advanced nasopharyngeal cancer that is unlikely to get better
Your doctor might suggest further treatment with radiotherapy, chemotherapy or both. The aim in this situation is to shrink the cancer and help to control your symptoms. This is called palliative treatment. Although it is not likely to cure your cancer, it could control it for some time.
If your cancer is very advanced your doctor will refer you to a palliative care team for expert control of your symptoms. Palliative care specialists care for people in the final stages of their illness, but they also work with people with any stage of cancer. They can give expert help including:
- controlling symptoms such as pain, sickness and breathing problems
- supporting you with diet and physical care
- helping you have the best possible quality of life, whether you are at home or in a hospital or hospice
Head and neck cancer survival
Survival depends on many different factors. So no one can tell you exactly how long you will live. It depends on your:
- type and stage of cancer
- level of fitness
- previous treatment
These are general statistics based on large groups of patients. Remember, they can’t tell you what will happen in your individual case.
Nasal and paranasal sinus cancer survival rate
Survival depends on many factors, so no one can tell you exactly how long you’ll live. It depends on your individual condition, type of cancer, treatment and level of fitness.
Statistics for this cancer are harder to estimate than for other, more common cancers.
Some of the statistics have to be based on a small number of people. Remember, they can’t tell you what will happen in your individual case.
Your doctor can give you more information about your own outlook (prognosis).
What affects survival
Your outcome depends on the stage of the cancer when it was diagnosed. This means how big it is and whether it has spread.
The type of cancer can also affect your likely survival. And your outlook also depends on which parts of the nasal cavity or paranasal sinuses are involved.
Your general health and fitness also affect survival. The fitter you are, the better you may be able to cope with your cancer and treatment.
About these statistics
The terms 1 year survival and 5 year survival don’t mean that you will only live for 1 or 5 years. They relate to the number of people who are still alive 1 year or 5 years after their diagnosis of cancer.
Some people live much longer than 5 years.
Nasal and paranasal sinus cancer survival by stage
The following statistics are based on people diagnosed with nasal cavity and paranasal sinus cancer between 1998 and 1999.
Please be aware that due to differences in health care systems, data collection and the population, these figures are not a true picture of survival in the UK.
- Stage 1: Almost 65 out of 100 people (almost 65%) will survive their cancer for 5 years or more after diagnosis.
- Stage 2: Around 60 out of 100 people (around 60%) will survive their cancer for 5 years or more after diagnosis.
- Stage 3: 50 out of 100 people (50%) will survive their cancer for 5 years or more after they are diagnosed.
- Stage 4: 35 out of 100 people (35%) will survive their cancer for 5 years or more after diagnosis.
Survival for all stages of nasal cavity and paranasal sinus cancer
The following statistics are from a large European study that looked at survival in rare cancers.
For people diagnosed with nasal cavity or paranasal sinus cancer in the UK and Ireland:
- more than 70 out of 100 people (more than 70%) will survive their cancer for 1 year or more after diagnosis
- around 50 out of 100 people (50%) will survive their cancer for 5 years or more after they are diagnosed.
Mouth and oropharyngeal cancer survival rate
Survival depends on many factors, so no one can tell you exactly how long you’ll live. It depends on your individual condition, type of cancer, treatment and level of fitness.
Some of the statistics have to be based on a small number of people. Remember, they can’t tell you what will happen in your individual case.
Your doctor can give you more information about your own outlook (prognosis).
What affects survival
Your outcome depends on the stage of the cancer when it was diagnosed. This means how big it is and whether it has spread.
The outlook for mouth cancers also depends on which part of the mouth or oropharynx is involved.
Some oropharyngeal cancers are caused by the human papilloma virus (HPV). Oropharyngeal cancers that contain HPV tend to do better than oropharyngeal cancers that don’t contain HPV.
About these statistics
The terms 1 year survival and 5 year survival don’t mean that you will only live for 1 or 5 years. They relate to the number of people who are still alive 1 year or 5 years after their diagnosis of cancer.
Some people live much longer than 5 years.
Mouth and oropharyngeal cancer survival by stage
The following statistics are from the National Cancer Intelligence Network. They are for people diagnosed with mouth (oral cavity) cancer in England and Wales, between 2004 and 2011. The figures are for 1 and 3 year survival. At the moment there are no statistics available for 5 year survival.
For men diagnosed with stage 1 and 2 mouth (oral cavity) cancer:
- more than 90 out of 100 (more than 90%) survive their cancer for 1 year or more
- around 80 out of 100 (around 80%) survive their cancer for 3 years or more
For women diagnosed with stage 1 and 2 mouth cancer:
- around 95 out of 100 (around 95%) survive their cancer for 1 year or more
- more than 80 out of 100 (more than 80%) survive their cancer for 3 years or more
For men diagnosed with stage 3 and 4 mouth cancer:
- almost 70 out of 100 (almost 70%) survive their cancer for a year or more
- almost 50 out of 100 (almost 50%) survive their cancer for 3 years or more
For women diagnosed with stage 3 or 4 cancer:
- around 65 out of 100 (around 65%) survive their cancer for a year or more
- almost 50 out of 100 (almost 50%) survive their cancer for 3 years or more
Mouth and oropharyngeal cancer survival by site of tumor
Survival for mouth and oropharyngeal cancer depends on where the cancer is.
For mouth (oral cavity) cancer:
- almost 80 out of 100 people (almost 80%) survive their cancer for 1 year or more after they are diagnosed
- almost 60 out of 100 people (almost 60%) survive their cancer for 5 years or more after diagnosis.
For oropharyngeal cancer:
- almost 85 out of 100 (almost 85%) survive their cancer for a year or more
- around 65 out of 100 (around 65%) survive their cancer for 5 years or more
The oropharynx is the part of the throat just behind your mouth.
For tongue cancer:
- around 80 out of 100 (around 80%) survive their cancer for a year or more
- around 60 out of 100 (around 60%) survive their cancer for 5 years or more.
Laryngeal cancer survival rate
Survival depends on many different factors. So no one can tell you exactly how long you will live. It depends on your:
- type and stage of cancer
- level of fitness
- previous treatment
These are general statistics based on large groups of patients. Remember, they can’t tell you what will happen in your individual case.
What affects survival
Your outlook depends on the stage of the cancer when it was diagnosed. This means how big it is and whether it has spread.
The grade of the cancer cells can also affect your likely survival. Grade means how abnormal the cells look under the microscope. The location of the cancer in the larynx also affects survival.
Your general health and fitness affects survival. Also, if you carry on smoking after your cancer, this affects your likely survival. And there is a higher risk that you will get a second cancer.
About these statistics
The terms 1 year survival and 5 year survival don’t mean that you will only live for 1 or 5 years. They relate to the number of people who are still alive 1 year or 5 years after their diagnosis of cancer.
Some people live much longer than 5 years.
Laryngeal cancer survival by stage
The figures presented use the number staging system. This staging system is slightly different to the T stages used by doctors. But if you are uncertain, do ask your doctor or nurse to help you understand this information.
Stage 1
Around 90 out of 100 adults (around 90%) will survive their cancer for 5 years or more after diagnosis.
Stage 1 laryngeal cancer is only in one part of the larynx and the vocal cords are still able to move. The cancer has not spread to nearby tissues, lymph nodes or other organs.
Stage 2
Around 60 out of 100 adults (around 60%) will survive their cancer for 5 years or more after they are diagnosed.
Stage 2 laryngeal cancer has spread to another part of the larynx from where it started. In some types of laryngeal cancer, it has grown into the vocal cords and these may not be able to move. The cancer has not spread to lymph nodes or other organs.
Stage 3
Almost 60 out of 100 adults (almost 60%) will survive their cancer for 5 years or more after they are diagnosed.
Stage 3 laryngeal cancer has grown throughout the larynx but has not spread to other parts of the body. OR at least one vocal cord is fixed and can’t move. OR the cancer may also have spread to a nearby lymph node, which is no larger than 3cm across.
Stage 4
More than 40 out of 100 adults (more than 40%) will survive their cancer for 5 years or more after they are diagnosed.
Stage 4 cancer may have spread into tissue outside the larynx such as the thyroid or food pipe. It may have spread to lymph nodes which are further away and larger in size. And it may have spread to other parts of the body.
Laryngeal cancer survival for all stages
There are only statistics available for men. This is because so few women are diagnosed with cancer of the larynx.
Generally for men with cancer of the larynx:
- around 85 out of every 100 (around 85%) will survive their cancer for 1 year or more after they are diagnosed
- around 65 out of every 100 (around 65%) will survive their cancer for 5 years or more after diagnosis
- around 55 out of every 100 (around 55%) will survive their cancer for 10 years or more after they are diagnosed
Esophageal cancer survival rate
Survival depends on many different factors. So no one can tell you exactly how long you will live. It depends on your:
- type and stage of cancer
- level of fitness
- previous treatment
These are general statistics based on large groups of patients. Remember, they can’t tell you what will happen in your individual case.
What affects survival
Your outlook depends on the stage of the cancer when it was diagnosed. This means how big it is and whether it has spread.
The type of cancer and grade of the cancer cells can also affect your survival. Grade means how abnormal the cells look under the microscope.
Your general health and fitness also affect survival, the fitter you are, the better you may be able to cope with your cancer and treatment.
About these statistics
The term 1 year survival does not mean that you will only live for 1 year. They relate to the number of people who are still alive 1 year after their diagnosis of cancer.
Some people live much longer than 1 year.
Esophageal cancer survival by stage
These figures are for people diagnosed between 2013 and 2017.
- Stage 1: Almost 55 out of 100 people (almost 55%) with stage 1 esophageal cancer will survive their cancer for 5 years or more after they’re diagnosed.
- Stage 2: 30 out of 100 people (30%) with stage 2 esophageal cancer will survive their cancer for 5 years or more after they’re diagnosed.
- Stage 3: Around 15 out of 100 people (around 15%) with stage 3 esophageal cancer will survive their cancer for 5 years or more after they’re diagnosed.
- Stage 4: There are no statistics for stage 4 cancer because sadly many people don’t live for that long after diagnosis.
Survival for all stages of esophageal cancer
For people with esophageal cancer:
- more than 40 out of every 100 (more than 40%) will survive their cancer for 1 year or more after they are diagnosed
- 15 out of every 100 (15%) will survive their cancer for 5 years or more
- more than 10 out of 100 (more than 10%) will survive their cancer for 10 years or more
Salivary gland cancer survival rate
Survival depends on many different factors. It depends on your individual condition, type of cancer, treatment and level of fitness. So no one can tell you exactly how long you will live.
Statistics for salivary gland cancer are harder to estimate than for other, less rare cancers. Some of the statistics have to be based on a small number of people. They can’t tell you what will happen in your individual case.
Your doctor can give you more information about your own outlook (prognosis).
What affects survival
Your outcome depends on the stage of the cancer when it was diagnosed. This means how big it is and whether it has spread.
Survival is also affected by the site of the cancer.
About these statistics
The term 5 year survival doesn’t mean you will only live for 5 years. It relates to the number of people who live 5 years or more after their diagnosis of cancer. Many people live much longer than 5 years.
Some of the statistics on this page are for relative survival. Relative survival takes into account that some people will die of causes other than cancer.
This gives a more accurate picture of cancer survival. Relative survival statistics are used for survival by stage for major salivary gland cancer, and for survival of all types and stages of salivary cancer.
Clinical trials
Research evidence shows that taking part in clinical trials may improve outlook. No one is completely sure why this is. It is probably partly to do with your doctors and nurses monitoring you more closely if you are in a trial. For example, you may have more scans and blood tests.
Survival by stage for major salivary cancers
The statistics below are based on people diagnosed with cancer of the major salivary glands between 1998 and 1999.
- Stage 1: Around 90 out of 100 people (around 90%) survive their cancer for 5 years or more after their cancer was diagnosed.
- Stage 2: Around 75 out of 100 people (around 75%) survive their cancer for 5 years or more after diagnosis.
- Stage 3: 65 out of 100 people (65%) survive their cancer for 5 years or more after they are diagnosed.
- Stage 4: Around 40 out of 100 people (around 40%) survive their cancer for 5 years or more after diagnosis.
Survival by stage for minor salivary cancers
Minor salivary gland cancers are very rare. So survival figures are harder to find. The figures below come from 2 small studies, one American and the other European.
- Generally for people with minor salivary gland cancer: between 50 and 60 out of 100 (50 to 60%) survive for 10 years or more after their diagnosis
The stage of the cancer affects the outlook.
- Stage 1: Around 80 out of 100 people (around 80%) survive for 5 years or more after diagnosis
- Stage 2: Around 70 out of 100 people (around 70%) survive for 5 years or more after diagnosis
- Stage 3: Around 60 out of 100 people (around 60%) survive for 5 years or more after they are diagnosed
- Stage 4: Around 30 out of 100 people (around 30%) survive for 5 years or more after diagnosis
Survival for all types and stages of salivary cancer
Overall, for all people with salivary gland cancer:
- around 85 out of 100 people (around 85%) survive their cancer for 1 year or more
- more than 65 out of 100 people (more than 65%) survive their cancer for 5 years or more
- around 60 out of 100 people (around 60%) survive their cancer for 10 years or more.
Nasopharyngeal cancer survival rate
Survival depends on many different factors. So no one can tell you exactly how long you will live. It depends on your:
- type and stage of cancer
- level of fitness
- previous treatment
These are general statistics based on large groups of patients. Remember, they can’t tell you what will happen in your individual case. Your doctor can give you more information about your own outlook (prognosis).
What affects survival
Your outcome depends on the stage of the cancer when it was diagnosed. This means how big it is and whether it has spread.
The type of cancer can also affect your likely survival. Your outlook also depends on which part of the nasopharynx is involved.
Your general health and fitness also affect survival because overall, the fitter you are, the better you may be able to cope with your cancer and treatment. Also, if you smoke, your outlook is worse.
About these statistics
The terms 1 year survival and 5 year survival don’t mean that you will only live for 1 or 5 years. They relate to the number of people who are still alive 1 year or 5 years after their diagnosis of cancer.
Some people live much longer than 5 years.
Nasopharyngeal cancer survival by stage
The figures below are based on people diagnosed between 1998 and 1999.
- Stage 1: More than 70 out of every 100 people (70%) will survive their cancer for 5 years or more after they are diagnosed.
- Stage 2: Around 65 out of 100 (65%) will survive their cancer for 5 years or more after they are diagnosed.
- Stage 3: More than 60 out of 100 (60%) will survive their cancer for 5 years or more after they are diagnosed.
- Stage 4: Almost 40 out of 100 (40%) will survive their cancer for 5 years or after they are diagnosed.
Survival for all stages of nasopharyngeal cancer
For all people diagnosed with nasopharyngeal cancer:
- almost 80 out of 100 people (80%) will survive their cancer for 1 year after diagnosis
- around 50 out of 100 people (50%) will survive their cancer for 5 years or more after they are diagnosed
- Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA: A Cancer Journal for Clinicians 2017; 67(1):7-30.
- Cancer Facts & Figures 2017. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2017.html
- Gandini S, Botteri E, Iodice S, et al. Tobacco smoking and cancer: a meta-analysis. International Journal of Cancer 2008; 122(1):155–164.
- Blot WJ, McLaughlin JK, Winn DM, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Research 1988; 48(11):3282–3287.
- Hashibe M, Brennan P, Chuang SC, et al. Interaction between tobacco and alcohol use and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiology, Biomarkers and Prevention 2009; 18(2):541–550.
- Chaturvedi AK, Engels EA, Pfeiffer RM, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. Journal of Clinical Oncology 2011; 29(32):4294–4301.
- Goldenberg D, Lee J, Koch WM, et al. Habitual risk factors for head and neck cancer. Otolaryngology and Head and Neck Surgery 2004; 131(6):986–993.
- Yu MC, Yuan JM. Nasopharyngeal Cancer. In: Schottenfeld D, Fraumeni JF Jr., editors. Cancer Epidemiology and Prevention. 3rd ed. New York: Oxford University Press, 2006.
- Guha N, Boffetta P, Wünsch Filho V, et al. Oral health and risk of squamous cell carcinoma of the head and neck and esophagus: results of two multicentric case-control studies. American Journal of Epidemiology 2007; 166(10):1159–1173.
- Yu MC, Yuan JM. Epidemiology of nasopharyngeal carcinoma. Seminars in Cancer Biology 2002; 12(6):421–429.
- Olshan AF. Cancer of the Larynx. In: Schottenfeld D, Fraumeni JF Jr., editors. Cancer Epidemiology and Prevention. 3rd ed. New York: Oxford University Press, 2006.
- Boffetta P, Richiardi L, Berrino F, et al. Occupation and larynx and hypopharynx cancer: an international case-control study in France, Italy, Spain, and Switzerland. Cancer Causes and Control 2003; 14(3):203–212.
- Littman AJ, Vaughan TL. Cancers of the Nasal Cavity and Paranasal Sinuses. In: Schottenfeld D, Fraumeni JF Jr., editors. Cancer Epidemiology and Prevention. 3rd ed. New York: Oxford University Press, 2006.
- Mayne ST, Morse DE, Winn DM. Cancers of the Oral Cavity and Pharynx. In: Schottenfeld D, Fraumeni JF Jr., editors. Cancer Epidemiology and Prevention. 3rd ed. New York: Oxford University Press, 2006.
- Chien YC, Chen JY, Liu MY, et al. Serologic markers of Epstein-Barr virus infection and nasopharyngeal carcinoma in Taiwanese men. New England Journal of Medicine 2001; 345(26):1877–1882.
- Chan JK, Yip TT, Tsang WY, et al. Specific association of Epstein-Barr virus with lymphoepithelial carcinoma among tumors and tumorlike lesions of the salivary gland. Archives of Pathology and Laboratory Medicine 1994; 118(10):994–997.