Hemoglobinuria
Hemoglobinuria means “hemoglobin in urine”. Hemoglobin is the red part of red blood cells, makes urine look dark. Hemoglobinuria is a condition in which the oxygen transport protein hemoglobin is found in abnormally high concentrations in the urine. Hemoglobinuria is often associated with hemolytic anemia, in which red blood cells are destroyed, thereby increasing levels of free plasma hemoglobin. The excess hemoglobin is filtered by the kidneys, which release it into the urine, giving urine a red color.
Hemoglobinuria causes
Red blood cells develop in your bone marrow, which is the sponge-like tissue inside your bones. Red blood cells normally live for 110 to 120 days. After that, they naturally break down and are most often removed from the circulation by your spleen. Your body normally destroys old or faulty red blood cells in the spleen or other parts of your body through a process called hemolysis. Anemia is a condition in which your body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues. Hemolytic anemia occurs when you have a low number of red blood cells due to too much hemolysis in the body and your bone marrow isn’t making enough red cells to replace the ones that are being destroyed.
Some diseases and processes cause red blood cells to break down too soon. This requires the bone marrow to make more red blood cells than normal. The balance between red blood cell breakdown and production determines how low the red blood cell count becomes.
Conditions that can cause hemolysis or hemolytic anemia include:
- Immune reactions
- Infections
- Exposure to certain chemicals, medicines, and toxins
- Blood clots in small blood vessels
- Transfusion of blood from a donor with a blood type that does not match yours
- Toxins and poisons
- Treatments such as hemodialysis or the use of the heart-lung bypass machine
- Hereditary disorders may cause hemolysis as a result of erythrocyte membrane abnormalities, enzymatic defects, and hemoglobin abnormalities. Hereditary disorders include the following 1:
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency
- Hereditary spherocytosis
- Sickle cell anemia
- Acquired causes of hemolysis include the following:
Recent articles have noted that intravenous immunoglobulin G (IVIG) therapy given during pregnancy 5, the contrast medium iomeprol 6 and mitral valve replacement 7 can cause hemolysis.
There are many types of hemolytic anemia, which doctors diagnose based on the underlying cause of your anemia. Certain conditions can cause hemolysis to happen too fast or too often. Conditions that may lead to hemolytic anemia include inherited blood disorders such as sickle cell disease or thalassemia, autoimmune disorders, bone marrow failure, or infections. Some medicines or side effects to blood transfusions may cause hemolytic anemia.
Hemolytic anemia can develop suddenly or slowly, and it can be mild or severe. Signs and symptoms may include fatigue, dizziness, heart palpitations, pale skin, headache, confusion, jaundice, and a spleen or liver that is larger than normal. Severe hemolytic anemia can cause chills, fever, pain in the back and abdomen, or shock. Severe hemolytic anemia that is not treated or controlled can lead to serious complications, such as irregular heart rhythms called arrhythmias; cardiomyopathy, in which the heart grows larger than normal; or heart failure.
Autoimmune hemolytic anemia (AIHA) can be due to warm or cold autoantibody types and, rarely, mixed types 8 . Most warm autoantibodies belong to the immunoglobulin IgG class. These antibodies can be detected by a direct Coombs test, which also is known as a direct antiglobulin test. Autoimmune hemolytic anemia may occur after allogeneic hematopoietic stem cell transplantation. The 3-year cumulative incidence in this population has been reported at 4.44% 9.
Autoimmune hemolytic anemia is rare in children and has a range of causes. Autoimmune hemolysis can be primary or secondary to conditions such as infections (viral, bacterial, and atypical), systemic lupus erythematosus (SLE), autoimmune hepatitis, and H1N1 influenza. H1N1 influenza–associated autoimmune hemolytic anemia in children may respond to treatment with oseltamivir and intravenous immunoglobulin 10.
Fetal splenomegaly and associated hepatomegaly could be due to hemolysis, but infections are the most likely cause. Congestive heart failure and metabolic disorders should be considered. Rarely, leukemia, lymphoma, and histiocytosis are associated with splenomegaly 11.
Microangiopathic hemolytic anemia, which results in the production of fragmented erythrocytes (schistocytes), may be caused by any of the following 12:
- Defective prosthetic cardiac valves
- Disseminated intravascular coagulation (DIC)
- Hemolytic uremic syndrome (HUS)
- Thrombotic thrombocytopenic purpura (TTP)
In paroxysmal nocturnal hemoglobinuria (PNH), hemolysis is due to intravascular complement-mediated destruction of erythrocytes.
Paroxysmal cold hemoglobinuria (PCH) is an autoimmune disorder, a disorder in which the body’s natural defenses against invading organisms destroy healthy tissue for unknown reasons. In paroxysmal cold hemoglobinuria, antibodies mistakenly attack red blood cells causing the cells to breakdown prematurely, a condition called (hemolysis). When antibodies attack healthy tissue, they are referred to as autoantibodies.
To diagnose hemolytic anemia, your doctor will do a physical exam and order blood tests. Additional tests may include a urine test, a bone marrow test, or genetic tests. People who are diagnosed with mild hemolytic anemia may not need treatment at all. For others, hemolytic anemia can often be treated or controlled. Treatments may include lifestyle changes, medicines, blood transfusions, blood and bone marrow transplants, or surgery to remove the spleen. If your hemolytic anemia is caused by medicines or another health condition, your doctor may change your treatment to control or stop the hemolytic anemia.
Hemoglobinuria symptoms
For specific symptoms of hemoglobinuria see paroxysmal nocturnal hemoglobinuria (PNH) and paroxysmal cold hemoglobinuria (PCH) symptoms below.
Hemolytic anemia symptoms
You may not have symptoms if the anemia is mild. If the problem develops slowly, the first symptoms may be:
- Feeling weak or tired more often than usual, or with exercise
- Feelings that your heart is pounding or racing
- Headaches
- Problems concentrating or thinking
If the anemia gets worse, symptoms may include:
- Lightheadedness when you stand up
- Pale skin
- Shortness of breath
- Sore tongue
- Enlarged spleen
Hemoglobinuria diagnosis
A test called a complete blood count (CBC) can help diagnose anemia and offer some hints to the type and cause of the problem. Important parts of the CBC include red blood cell count (RBC), hemoglobin, and hematocrit (HCT).
These tests can identify the type of hemolytic anemia:
- Absolute reticulocyte count
- Coombs test, direct and indirect
- Donath-Landsteiner test
- Cold agglutinins
- Free hemoglobin in the serum or urine
- Hemosiderin in the urine
- Platelet count
- Protein electrophoresis – serum
- Pyruvate kinase
- Serum haptoglobin levels
- Serum LDH
- Carboxyhemoglobin level
Hemoglobinuria treatment
Treatment depends on the type and cause of the hemolytic anemia:
- In emergencies, a blood transfusion may be needed.
- For immune causes, medicines that suppress the immune system may be used.
- When blood cells are being destroyed at a fast pace, the body may need extra folic acid and iron supplements to replace what is being lost.
In rare cases, surgery is needed to take out the spleen. This is because the spleen acts as a filter that removes abnormal cells from the blood.
Hemoglobinuria prognosis
Outcome depends on the type and cause of hemolytic anemia. Severe anemia can make heart disease, lung disease, or cerebrovascular disease worse.
Paroxysmal nocturnal hemoglobinuria
Paroxysmal nocturnal hemoglobinuria (PNH) also called Marchiafava-Micheli Syndrome or paroxysmal hemoglobinuria, is a rare acquired blood disorder that causes red blood cells to break apart prematurely and impaired production of blood cells 13. Doctors call this breaking apart of red blood cells “hemolysis.” It happens because the surface of a person’s blood cells are missing a protein that protects them from the body’s immune system. Hemolysis happens when the complement system, a part of your body’s immune system, becomes more active and attacks your PNH red blood cells. The complement is made of small proteins that attack foreign objects, such as viruses and bacteria. Because PNH cells are abnormal, they are seen as foreign and attacked, causing them to burst.
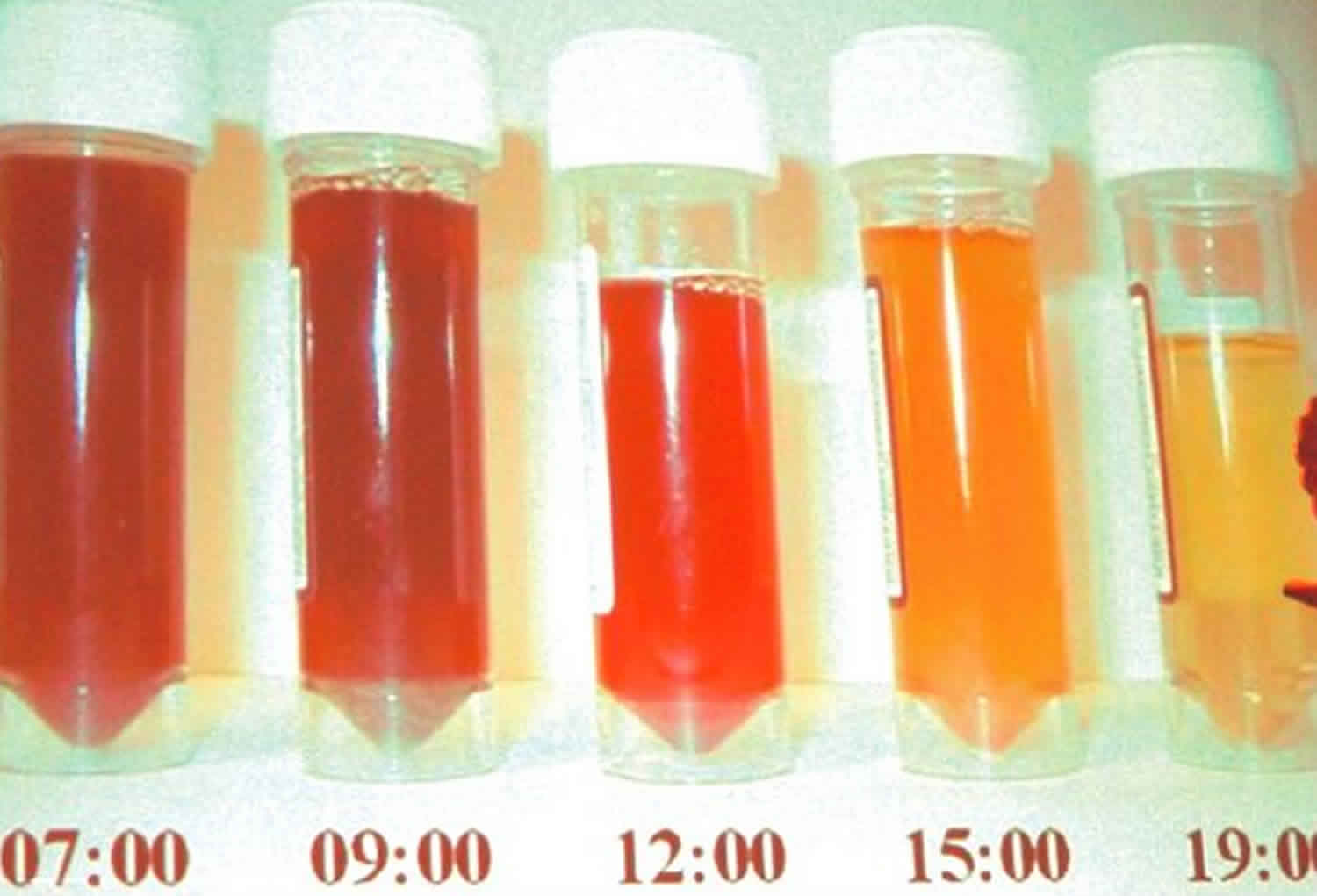
When red blood cells break apart, the hemoglobin inside is released. Hemoglobin is the red part of red blood cells that carries oxygen around the body. The release of hemoglobin causes many of the PNH symptoms. Paroxysmal means “sudden and irregular”. The term “nocturnal” refers to the belief that hemolysis is triggered by acidosis during sleep. However, this observation was later disproved. In individuals with paroxysmal nocturnal hemoglobinuria, hemolysis has been shown to occur throughout the day, but the urine concentrated overnight produces the dramatic change in color 14. Paroxysmal nocturnal hemoglobinuria (PNH) is most noticeable in the morning, upon passing urine that has accumulated in the bladder during the night 13. So, “paroxysmal nocturnal hemoglobinuria” means sudden, irregular episodes of passing dark colored urine, especially at night or in the early morning. It is important to note this can be a bit misleading, because many people with PNH do not have dark urine.
Paroxysmal nocturnal hemoglobinuria affects red blood cells (erythrocytes), which carry oxygen; white blood cells (leukocytes), which protect the body from infection; and platelets (thrombocytes), which are involved in blood clotting. This results in a deficiency of various types of blood cells and can cause signs and symptoms such as fatigue, weakness, abnormally pale skin (pallor), shortness of breath, and an increased heart rate. People with PNH may also be prone to infections and abnormal blood clotting (thrombosis) or hemorrhage, and are at increased risk of developing leukemia.
Paroxysmal nocturnal hemoglobinuria is a rare disorder, estimated to affect between 1 and 5 per million people. Experts estimate between 400 and 500 PNH cases are diagnosed in the U.S. each year 15. Paroxysmal nocturnal hemoglobinuria affects both sexes equally, and can occur at any age, although it is most often diagnosed in young adulthood. Paroxysmal nocturnal hemoglobinuria can occur at any age, but is usually diagnosed in young adulthood in people in their 30s and 40s. People with PNH have recurring episodes of symptoms due to hemolysis, which may be triggered by stresses on the body such as infections or physical exertion.
Paroxysmal nocturnal hemoglobinuria is caused by acquired, rather than inherited, mutations in the PIGA gene (located on Xp22.1); the condition is not passed down to children of affected individuals 16. Sometimes, people who have been treated for aplastic anemia may develop PNH 13. The treatment of paroxysmal nocturnal hemoglobinuria is largely based on symptoms; stem cell transplantation is typically reserved for severe cases of PNH with aplastic anemia or those whose develop leukemia 14.
What is bone marrow failure?
Bone marrow failure happens when the marrow does not produce enough red cells, white cells or platelets, or the blood cells that are produced are damaged or defective. This means the body can not supply itself with the blood it needs. PNH, along with aplastic anemia and myleodysplastic syndromes (MDS), are bone marrow failure diseases.
What happens to my blood with PNH?
Blood consists of blood cells floating in plasma. Plasma is mostly made of water. It also includes salts, proteins, hormones, minerals, vitamins and other nutrients and chemicals your body needs.
The 3 basic types of blood cells:
- Red blood cells (RBCs) are also called erythrocytes. They make up almost half of blood. Red blood cells are filled with the protein hemoglobin that picks up oxygen in the lungs and brings it to cells all around the body.
- White blood cells (WBCs) are also called leukocytes. They fight disease and infection by attacking and killing germs that get into the body. There are several kinds of white blood cells, each of which fights a different kind of germ.
- Platelets are also called thrombocytes. They are small pieces of cells that help blood clot and stop bleeding.
Blood cells formation
The process of making blood cells is called hematopoiesis. Blood cells are made in the bone marrow, a spongy tissue located inside certain bones. Marrow contains blood-forming stem cells that make copies of themselves to create all 3 types of blood cells. When blood cells are fully mature and functional, they leave the bone marrow and enter the bloodstream. Healthy people have enough stem cells to make all the blood cells they need.
What is the complement system in PNH?
The complement system is a group of proteins in the blood. They help support (complement) the work of white blood cells by fighting infections.
These proteins are always active at a very low level. But when bacteria, viruses and other foreign or abnormal cells get into your body, these proteins become more active. They work together to attack and destroy these abnormal cells.
Normal red blood cells have a shield of proteins. This shield protects the cells from being attacked by the complement system. The gene in charge of making this protective shield is called PIGA (phosphatidylinositol glycan class A).
Why are blood clots so common for people with PNH?
Scientists are not sure exactly why people with PNH are more likely to get blood clots. But some believe that PNH patients have abnormal platelets that are too “sticky.” This means the platelets make clots too easily.
Many people with PNH have a shortage of nitric oxide. Nitric oxide helps prevent blood clots by making it harder for platelets to stick together. Hemolysis – another symptom of PNH – can cause a shortage of nitric oxide.
How do I find out if I have a blood clot?
To diagnose a blood clot, your doctor may take pictures of your insides using:
- CT scan (Cat Scan)
- MRI (Magnetic Resonance Imaging)
- Doppler scan
- V-Q Scan (Ventilation-Perfusion Scan)
Your doctor may also order a lab test called D-dimer. It is also called Fragment D-Dimer, or Fibrin degradation fragment.
What immunizations should a PNH patient get?
Patients with PNH should receive vaccinations against certain types of bacteria to prevent infection. Ask your doctor which ones are right for you.
Seasonal flu vaccines protect against the three influenza viruses (trivalent) that research indicates will be most common during the upcoming season. Talk with your hematologist about whether you should get a flu shot. He will help you weigh the risks and benefits of getting a flu shot. Don’t forget to ask whether your family members and others in close contact with you should get a flu vaccine. This may reduce your chance of getting the flu. To read more about flu shots, read our article.
There have been a few case reports of PNH patients getting flares of hemolysis (when red blood cells are destroyed) after receiving a flu shot. Although case reports are not the same as randomized clinical trials, one case of hemolysis was severe enough to put the patient in the hospital. That is why some PNH experts recommend against having a flu shot, but each case is different. PNH patients who are receiving eculizumab may be less likely to have hemolysis after receiving a flu shot.
Can PNH patients get pregnant and have a healthy delivery?
Pregnancy is possible with PNH, but it is not a good idea. It carries serious risks for both mother and child.
A woman with PNH faces a number of risks during pregnancy:
- Her blood may have fewer healthy cells.
- Her bone marrow may make fewer healthy cells.
- She is more likely to get blood clots. Most doctors place pregnant women with PNH on blood thinners to prevent clots. But warfarin (Coumadin®) cannot be used during the first trimester, since it may affect fetus development.
- She is more likely to get preeclampsia, a dangerous condition that causes very high blood pressure and can put both mother and baby at risk.
- She may need red blood cell transfusions more often.
A baby whose mother has PNH has a greater risk of:
- Premature birth
- Dying in the womb
- Having a low birth weight
- Having delayed growth and development
Still, about 1 out of 3 babies whose mothers have PNH do not have any of these problems.
If you do get pregnant, look for a PNH specialist and an obstetrician who specializes in high-risk births.
Is surgery safe for PNH patients?
Surgery can also be risky for people with PNH because it:
- Makes the complement system more active, which can cause hemolysis
- Increases the risk of getting blood clots
- Can cause serious bleeding in people with a low platelet count
- May require platelet transfusions before surgery.
If you do have surgery, it is a good idea to:
- Make sure your PNH specialist talks with your surgeon
- Take the blood thinner Heparin (Calciparine or Liquaemin) as soon as possible after surgery, as long as your platelet count is good and your doctor advises it.
Special precautions for PNH patients
Airplane travel and high altitudes
The farther you move away from sea level, the less oxygen there is. If you have anemia, flying in an airplane or visiting places at higher elevations than you’re used to may cause a shortage of oxygen. It may also cause chest pain. Before you do either of these things, it’s a good idea to:
- Check with your doctor
- Get a red blood cell count
- Get treatment for your anemia (blood transfusions or growth factors)
- If you do fly, remember to:
- Drink plenty of water
- Get up and walk around every hour or two if it is safe to do so
Paroxysmal nocturnal hemoglobinuria causes
Paroxysmal nocturnal hemoglobinuria or PNH is caused by a genetic change (mutation) in the PIGA gene of a single stem cell in your bone marrow. The PIGA gene provides instructions for making a protein called phosphatidylinositol glycan class A. This protein takes part in a series of steps that produce a molecule called GPI anchor. GPI anchor attaches many different proteins to the cell membrane, thereby ensuring that these proteins are available when needed at the surface of the cell.
Here are the steps that lead to PNH:
- The abnormal stem cell makes copies of or “clones” itself. This leads to a whole population of bone marrow stem cells that have mutant PIGA.
- The abnormal cells mature into red blood cells that have mutant PIGA. These are called PNH red blood cells. Doctors also call them your PNH clone.
- The PNH red blood cells lack the shield of proteins that protect normal red blood cells from the complement system, leaving them open to attack and destruction by the complement system proteins.
Many healthy people have a small number of PNH stem cells. In people with PNH, however, these stem cells grow fast and make lots of mature PNH red blood cells.
Some doctors believe this growth happens because people with PNH have bone marrow that is weaker than normal. This weakening may be caused by aplastic anemia or another mild and/or undiagnosed bone marrow failure disease.
If you have had aplastic anemia, you are more likely to get PNH. There are no other known factors that increase your chances of getting PNH.
Some gene mutations are acquired during a person’s lifetime and are present only in certain cells. These changes, which are called somatic mutations, are not inherited. In people with paroxysmal nocturnal hemoglobinuria, somatic mutations of the PIGA gene occur in blood-forming cells called hematopoietic stem cells, which are found mainly in the bone marrow. These mutations result in the production of abnormal blood cells. As the abnormal hematopoietic stem cells multiply, increasing numbers of abnormal blood cells are formed, alongside normal blood cells produced by normal hematopoietic stem cells.
The premature destruction of red blood cells seen in paroxysmal nocturnal hemoglobinuria is caused by a component of the immune system called complement. Complement consists of a group of proteins that work together to destroy foreign invaders such as bacteria and viruses. To protect the individual’s own cells from being destroyed, this process is tightly controlled by complement-regulating proteins. Complement-regulating proteins normally protect red blood cells from destruction by complement. In people with paroxysmal nocturnal hemoglobinuria, however, abnormal red blood cells are missing two important complement-regulating proteins that need the GPI anchor protein to attach them to the cell membrane. These red blood cells are prematurely destroyed, leading to hemolytic anemia.
Research suggests that certain abnormal white blood cells that are also part of the immune system may mistakenly attack normal blood-forming cells, in a malfunction called an autoimmune process. In addition, abnormal hematopoietic stem cells in people with paroxysmal nocturnal hemoglobinuria may be less susceptible than normal cells to a process called apoptosis, which causes cells to self-destruct when they are damaged or unneeded. These features of the disorder may increase the proportion of abnormal blood cells in the body. The proportion of abnormal blood cells affects the severity of the signs and symptoms of paroxysmal nocturnal hemoglobinuria, including the risk of hemoglobinuria and thrombosis.
Paroxysmal nocturnal hemoglobinuria inheritance pattern
Paroxysmal nocturnal hemoglobinuria is acquired, rather than inherited. Paroxysmal nocturnal hemoglobinuria results from new mutations in the PIGA gene, and generally occurs in people with no previous history of the disorder in their family. Paroxysmal nocturnal hemoglobinuria is not passed down to children of affected individuals.
Risk factors of having PNH
Having aplastic anemia is the only known risk factor for developing PNH. More than 10 out of every 100 people with aplastic anemia will develop PNH. In addition, some people with PNH will develop aplastic anemia. People with PNH can share symptoms with aplastic anemia patients, such as low blood cell counts.
On average, 2 out of 100 people with PNH go on to develop myelodysplastic syndrome (MDS).
Paroxysmal nocturnal hemoglobinuria symptoms
When your PNH red blood cells break apart, their hemoglobin is released into your plasma. Hemoglobin is the red part of red blood cells. Its carries oxygen around your body. The release of hemoglobin can cause a number of symptoms, including:
- Dark or tea colored urine, but it does not darken in all cases
- Low red blood cell count (anemia) which can cause you to:
- Feel tired
- Have headaches
- Have trouble breathing when you exercise
- Have an irregular heartbeat
- Muscle spasms in certain parts of your body. This happens when the released hemoglobin binds with nitric oxide and removes it from your blood. Nitric oxide helps your muscles stay smooth and relaxed. When you have a shortage of nitric oxide, you may experience the following:
- Mild to severe pain in your abdomen or belly area.
- Spasms in your esophagus which is a “tube” in your throat that goes from your mouth to your stomach; the spasms can make it hard to swallow.
- Men may have trouble getting or keeping an erection (become impotent).
- Thrombosis is a blood clot in a vein. It is often simply called a blood clot. At least 1 out of 3 people with PNH get blood clots. The symptoms of blood clots depend on where the blood clots occur. People who are otherwise healthy and do not have PNH sometimes get blood clots in the veins of the leg. People with PNH tend to get blood clots in other parts of the body, such as in the brain or abdomen (belly area).
- Blood clot in abdomen (belly area): You may get a blood clot in your abdomen, or belly area. That’s the area below your chest and above your hips. Some places in the abdomen where you may get a blood clot include:
- Your spleen
- The major vein that leaves your liver; this is called Budd-Chiari syndrome
- Your intestine (bowel) may not get enough blood; this is called ischemia
- Symptoms of getting a blood clot in your abdomen may include:
- Having fluid and swelling in the belly area; this is called ascites.
- The area where the clot is may feel warm to the touch.
- The area where the clot is may be painful.
- If the blood clot in your abdomen is not treated:
- Part of your intestine may die (dead bowel)
- Your liver may be damaged and stop working
- Blood clot in brain: You may get a blood clot in the veins covering your brain. If this happens, symptoms may include:
- A very bad headache.
- Trouble speaking, seeing, or moving parts of your body.
- Blood clot in skin: You may get a blood clot in the veins of your skin. If this happens, your skin in that area may get red, puffy, warm or painful
- Blood clot in arm or leg: You may get a blood clot in the veins of your arm or leg. If this happens that limb may get warm, puffy or painful
- Blood clot in lung: Sometimes, a blood clot breaks off and travels to your lung. This is called a pulmonary embolism. If you have a pulmonary embolism, symptoms may include:
- A sharp pain in your chest; it may get worse when you breathe deeply
- Trouble breathing (shortness of breath), or you may start breathing fast
- Suddenly feeling anxious
- Coughing up some blood
- Feeling dizzy; you may even faint
- Sweating a lot
- Blood clot in abdomen (belly area): You may get a blood clot in your abdomen, or belly area. That’s the area below your chest and above your hips. Some places in the abdomen where you may get a blood clot include:
People with paroxysmal nocturnal hemoglobinuria have sudden, recurring episodes of symptoms (paroxysmal symptoms), which may be triggered by stresses on the body, such as infections or physical exertion. During these episodes, red blood cells are prematurely destroyed (hemolysis). Affected individuals may pass dark-colored urine due to the presence of hemoglobin, the oxygen-carrying protein in blood. The abnormal presence of hemoglobin in the urine is called hemoglobinuria. In many, but not all cases, hemoglobinuria is most noticeable in the morning, upon passing urine that has accumulated in the bladder during the night (nocturnal).
The premature destruction of red blood cells results in a deficiency of these cells in the blood (hemolytic anemia), which can cause signs and symptoms such as fatigue, weakness, abnormally pale skin (pallor), shortness of breath, and an increased heart rate. People with paroxysmal nocturnal hemoglobinuria may also be prone to infections due to a deficiency of white blood cells.
Abnormal platelets associated with paroxysmal nocturnal hemoglobinuria can cause problems in the blood clotting process. As a result, people with this disorder may experience abnormal blood clotting (thrombosis), especially in large abdominal veins; or, less often, episodes of severe bleeding (hemorrhage).
Individuals with paroxysmal nocturnal hemoglobinuria are at increased risk of developing cancer in blood-forming cells (leukemia).
In some cases, people who have been treated for another blood disease called aplastic anemia may develop paroxysmal nocturnal hemoglobinuria.
Low red blood cell count
PNH will mostly cause low red blood cell counts and anemia. A low red blood cell count is called anemia. If you have a low red blood cell count, you may:
- Feel a little tired or very tired
- Feel less alert or have trouble concentrating
- Have a loss of appetite or lose weight
- Have paler-than-normal skin
- Have trouble breathing – shortness of breath
- Have rapid heartbeat
- Have difficulty exercising or climbing stairs
Low white blood cell counts
A low white blood cell count is called neutropenia. In general, a low white cell count lowers an aplastic anemia patient’s ability to fight bacterial infections. If you have a low white blood cell count, you may:
- Have repeated fevers and infections
- Get bladder infections that make it painful to urinate or make you urinate more often
- Get lung infections that cause coughing and difficulty breathing
- Get mouth sores
- Get sinus infections and a stuffy nose
- Get skin infections
A fever in an aplastic anemia patient is potentially serious. A doctor should be notified if a fever occurs.
Low platelet counts
A low platelet count is called thrombocytopenia. If you have a low platelet count, you may:
- Bruise or bleed more easily, even from minor scrapes and bumps
- Get heavier than normal menstrual periods
- Get nose bleeds
- Get tiny, flat red spots under your skin (petechiae) caused by bleeding
- Have bleeding gums, especially after dental work or from brushing your teeth.
If platelet counts are not too low, there may be no obvious symptoms. In rare cases, the number of platelets can get so low that dangerous internal bleeding occurs.
Bleeding that will not stop is a medical emergency. A PNH patient needs to seek immediate medical help if they have bleeding that can’t be stopped by usual methods, such as applying pressure to the area.
Paroxysmal nocturnal hemoglobinuria diagnosis
When you have anemia caused by the destruction of red blood cells, doctors call this hemolytic anemia. In addition to a complete blood cell count (CBC), the principal studies used to establish the diagnosis of paroxysmal nocturnal hemoglobinuria (PNH) are flow cytometry of peripheral blood and bone marrow analysis. Flow cytometry measures the percentage of cells that are deficient in the glycosyl phosphatidylinositol–anchored proteins (GPI-APs) and identifies discrete populations with different degrees of deficiency. Because of the missing GPI-APs, red blood cells (RBCs) and other cells in patients with PNH lack DAF (CD55) and MIRL (CD59), which regulate complement.
Hemosiderin is nearly always present in the urine sediment and can accumulate in the kidneys; this is visible on magnetic resonance images (MRI) or computed tomography (CT) scans. An elevated reticulocyte count and serum lactate dehydrogenase (LDH) level with a low serum haptoglobin level in the absence of hepatosplenomegaly are the hallmarks of intravascular hemolysis.
Bone marrow examination will differentiate classic PNH from PNH that develops in the setting of other bone marrow disorders 17. In addition, bone marrow examination will identify an erythroid and hyperplastic bone marrow during the hemolytic phase or a hypoplastic bone marrow in the aplastic phase.
Imaging studies are indicated in patients with venous thrombosis.
PNH test
There are several blood tests used to help confirm a diagnosis of PNH by looking for signs of hemolytic anemia. Specific tests include:
- A complete blood count (CBC) to look for signs of low hemoglobin. This test uses a number of methods to measure how many of each blood cell type are in your blood sample.
- An LDH test looks at the level of an enzyme called lactate dehydrogenase. High levels of LDH in the blood can mean that red blood cells are breaking apart (hemolysis) or that there is tissue damage in the body. It is important for patients with PNH to have LDH monitored regularly.
- A bilirubin test measures the total amount of this substance in your blood. High levels may indicate destruction of red blood cells.
- A reticulocyte count measures the number of young red blood cells in your blood. People who have PNH may have elevated reticulocyte counts because their bone marrow is making lots of new red blood cells.
Flow Cytometry
The gold standard for confirming the presence of PNH is a flow cytometry test. This test tells your doctor if any proteins are missing from the surface of blood cells. PNH cells are missing some or all of two proteins on their surface. These proteins are called CD55 and CD59. FLAER is a new type of flow cytometry test that is also used.
Using flow cytometry, your doctor can usually divide your blood cells into 3 types:
- PNH I cells, or Type I cells: These cells are normal. They respond in a healthy way to the complement system.
- PNH II cells, or Type II cells: These cells are partially sensitive to the complement system. They are missing some of the CD55 and CD59 proteins that protect them from attack.
- PNH III cells, or Type III cells: These cells are extremely sensitive to the complement system. Of the 3 groups of cells, these break apart most easily. They are missing all the proteins that protect normal cells from attack. Most people with PNH have Type I and Type III cells, but the amount of each type of cell can vary greatly.
Other blood tests
Doctors may ask you do to several types of blood tests to help them understand your case of PNH and create a treatment plan. These include:
- EPO level, also called erythropoietin, measures how much of this protein is being made by your kidneys. EPO is created in response to low oxygen levels in the body, typically caused by low red cell counts and anemia. EPO causes your bone marrow to make more red blood cells. A low EPO level may indicate a problem other than PNH, or it may make anemia worse in people who have PNH.
- Iron level test, also called a ferritin test, checks the level of iron in your blood. If a shortage of iron is causing anemia, it can be easily treated with iron supplements. If you have too much iron in your body this is called iron overload. It can be caused from getting lots of red blood cell transfusions or by genetic conditions. A number of treatments exist to remove iron from your body.
- Vitamin B12 and a folate level may be done to rule out other causes of low red cell counts. If your red blood cells have an abnormal shape, size or look, this can be caused by low levels of vitamin B12 and folate (folic acid). These abnormal looking cells don’t work right, and this can lead to anemia.
Bone marrow tests
An examination of your bone marrow is important for the diagnosis of PNH. It is usually a simple 30-minute procedure. First, the doctor uses a hollow needle to remove some bone marrow aspirate (liquid bone marrow), typically from the pelvic or breast bone. A solid piece of bone marrow is also removed for a bone marrow biopsy.
The doctor will look at your liquid bone marrow under a microscope and send a sample of your bone marrow to a lab.
A bone marrow test is done for two main reasons:
- To help confirm a diagnosis of PNH
- To understand how well or poorly your bone marrow is making blood cell
The bone marrow test shows:
- The quantity (cellularity) of your bone marrow occupied by different cells
- Exactly what types and amounts of cells your bone marrow is making
- Increased, decreased, or normal levels of iron in your bone marrow
- Chromosomal (DNA) abnormalities
Paroxysmal nocturnal hemoglobinuria treatment
According to current understanding of paroxysmal nocturnal hemoglobinuria (PNH), the ideal treatment is to replace the defective hematopoietic stem cell with a normal equivalent by stem cell transplantation; however, this is not realistic for many patients, because stem cell transplantation requires a histocompatible donor and is associated with significant morbidity and mortality 18. This form of treatment is reserved for severe cases of PNH with aplastic anemia or transformation to leukemia, both of which are life-threatening complications.
Androgens
Androgens are natural male hormones that can cause your bone marrow to make more red blood cells. This can improve anemia. Androgens are sometimes used to treat aplastic anemia and PNH.
Blood transfusions
A blood transfusion is a safe and common procedure. Most people who have a bone marrow failure disease like aplastic anemia, MDS or PNH will receive at least one blood transfusion. When you receive a blood transfusion, parts of blood from a donor are put into your bloodstream. This can help some patients with low blood counts.
Eculizumab
In 2007, eculizumab (Soliris), an anti-complement antibody targeting the CD5 complement component, was approved by the US Food and Drug Administration (FDA) and the European Medicines Evaluation Agency (EMEA) to treat PNH. It works by making your complement system less active and reduces hemolysis Soliris® is approved for the treatment of patients with PNH in nearly 50 countries worldwide.
Eculizumab alleviates the hemolysis associated with PNH and its complications, dramatically improving symptoms, improving quality of life, and eliminating complications of PNH 19. However, eculizumab does not alter the underlying defect of the disease, thus, treatment needs to continue life-long or until spontaneous remission, which occurred only in a minority of patients (12 of 80 patients in one study) before the advent of eculizumab 20.
Folic acid
Folic acid, also called folate or vitamin B-12, is found in fresh or lightly cooked green vegetables. It helps your bone marrow make normal blood cells. When your bone marrow has to make more cells, it needs a larger supply of folic acid.
Most people get enough folate in their diet. But if you have PNH, it’s a good idea to take 1 mg each day of a man-made form of folate called folic acid.
Growth factors
Growth factors are naturally occurring hormones in your body that signal your bone marrow to make more of certain types of blood cells. Man-made growth factors may be given to some people with bone marrow failure diseases to help increase red blood cell, white blood cell or platelet counts.
Iron chelation
Iron chelation therapy is the main treatment used when you have a condition called iron overload. Iron overload means you have too much iron in your body. This can be a problem for people who get lots of red blood cell transfusions.
Ravulizumab-cwvz (Ultomiris)
Ravulizumab-cwvz (Ultomiris) is a drug approved by the U.S. Food and Drug Administration (FDA) in 2018 to treat PNH. Ravulizumab-cwvz (Ultomiris) is a long-acting C5 inhibitor that works by inhibiting the C5 protein in the terminal complement cascade.
Treatment of bone marrow hypoplasia
Bone marrow hypoplasia is a serious cause of morbidity and mortality. Bone marrow hypoplasia is treated most effectively with bone marrow transplantation also called a stem cell transplant (SCT) or hematopoietic stem cell transplant (HSCT). The procedure replaces unhealthy blood-forming stem cells with healthy ones and offers some patients the possibility of a cure. But for many patients, a bone marrow transplantation is not an option due to the risks and potential long-term side effects as an “imperfect cure”.
Moroover, if there is no suitable donor available, antithymocyte globulin has been used in the treatment of aplastic anemia with considerable success.
Thromboembolism
Patients with PNH who develop acute thrombosis should immediately be started on eculizumab, if they are not already taking it, as this reduces the risk of thrombosis extension or recurrence 21. Otherwise, management of thrombotic complications follows standard principles, including using heparin emergently, then maintenance therapy with the use of an oral anticoagulant, such as warfarin. Sometimes, heparin can exacerbate the thrombotic problem, possibly by activating complement. This can be prevented using inhibitors of the cyclooxygenase system, such as aspirin, ibuprofen, and sulfinpyrazone.
Primary prophylaxis of thromboembolism for patients with PNH has been advocated. Whether this approach is safe and effective in all patients with PNH remains controversial, however.
Corticosteroids
Modulation of complement is controlled poorly by high doses of glucocorticoids. The usual adult dose of prednisone is 20-40 mg/d (0.3-0.6 mg/kg/day) given daily during hemolysis and changed to alternate days during remission. On this regimen, about 70% of adult patients experience improvement in hemoglobin levels, but long-term therapy is fraught with complications.
Investigational agents
A variety of agents that inhibit complement are under development for treatment of PNH. Novel anti-C5 agents include monoclonal antibodies and an anti-C5 small interfering RNA 22. Because clinically relevant C3-mediated extravascular hemolysis can occur in PNH 23, the anti-C3 small peptide compstatin and its derivatives are being investigated, along with inhibitors of complement Factor D or B 22.
Yuan et al 24 reported that two novel small-molecule inhibitors of Factor D, which is a component of the alternative complement pathway, show potential as oral agents for treating PNH. In the Ham test, using cells from PNH patients, the Factor D inhibitors significantly reduced complement-mediated hemolysis at concentrations as low as 0.01 μM. In an animal model, the compound ACH-4471 blocked alternative pathway activity.
PNH prognosis
The prognosis in patients with paroxysmal nocturnal hemoglobinuria (PNH) may vary from person to person, depending on the severity of symptoms and the presence of complications. You may have only mild symptoms, or you may have severe symptoms and need medicines or blood transfusions. An aplastic phase is a serious prognostic factor, because the resulting pancytopenia and thrombosis of hepatic, abdominal, and cerebral veins can have life-threatening consequences. Prophylactic anticoagulation has not been shown to be of benefit because of a lack of data from a clinical trial setting.
In many patients with paroxysmal nocturnal hemoglobinuria (PNH), the abnormal clone may eventually disappear. This usually takes at least 5 years, and often as long as 15-20 years. Reactivation of PNH in these patients has been observed with acute infections. Patients with chronic anemia alone, without thrombotic complications, can live relatively normal lives for many years.
Many people with PNH live for decades. People who develop blood clots in key parts of the body, or also have MDS (myelodysplastic syndromes) or AML (acute myeloid leukemia), may have a shorter lifespan.
The good news is that good treatments are available, and new treatments are being developed that help people with PNH live longer. You may have seen older research saying that patients with PNH live an average of 15 to 20 years, but more recent research shows that life expectancy has been steadily climbing over the past 20 years. It is even possible that PNH patients will soon live just as long as the average person of the same age.
Paroxysmal cold hemoglobinuria
Paroxysmal cold hemoglobinuria (PCH) is a very rare subtype of autoimmune hemolytic anemia caused by the presence of cold-reacting autoantibodies in the blood and characterized by the premature destruction of healthy red blood cells by autoantibodies and the sudden presence of hemoglobinuria, typically after exposure to cold temperatures 25. While rare, paroxysmal cold hemoglobinuria is nevertheless one of the most common causes of acute autoimmune hemolytic anemia in young children 26. Paroxysmal cold hemoglobinuria is thought to account for at most 2-10% of cases of autoimmune hemolytic anemia, whose annual incidence is estimated to be between 1/35,000-1/80,000 in North America and Western Europe.
Paroxysmal cold hemoglobinuria is classified as an autoimmune hemolytic anemia, an uncommon group of disorders in which the immune system mistakenly attacks healthy red blood cells. Autoimmune diseases occur when the body’s natural defenses against foreign organisms destroy healthy tissue for unknown reasons. Normally, red blood cells have a life span of approximately 120 days before they get removed by the spleen. In individuals with paroxysmal cold hemoglobinuria, red blood cells are destroyed prematurely and sometimes suddenly (paroxysmally). Many reports emphasize that paroxysmal cold hemoglobinuria is an unusual disease. However, in recent years, paroxysmal cold hemoglobinuria has become recognized as one of the most common causes of acute autoimmune hemolytic anemia in young children. The reason why acute transient paroxysmal cold hemoglobinuria appears to be a more common type of childhood autoimmune hemolytic anemia than it was thought to be several decades ago is uncertain, but probably relates to greater awareness of the disorder and more frequent use of the Donath-Landsteiner test (see Diagnosis section ), especially in children with acute autoimmune hemolytic anemia with hemoglobinuria.
A majority of cases of paroxysmal cold hemoglobinuria recorded in the early medical literature were associated with late syphilis or congenital syphilis. In the early 1900s over 90 percent of patients with chronic paroxysmal cold hemoglobinuria had a positive test for syphilis and approximately 30 percent showed clinical evidence of the disease. With the effective treatment of syphilis and the virtual elimination of the congenital form, “classical” syphilitic paroxysmal cold hemoglobinuria is now an extremely rare disorder, as is chronic paroxysmal cold hemoglobinuria. It was in patients with the chronic form of paroxysmal cold hemoglobinuria that exposure to cold resulted in a paroxysm of hemoglobinuria.
In modern times, paroxysmal cold hemoglobinuria cases almost exclusively affect children and are often preceded by symptoms of viral illness, so that paroxysms resulting from cold exposure are rarely encountered. Thus, although this type of autoimmune hemolytic anemia is known as paroxysmal cold hemoglobinuria, the words paroxysmal and cold are generally not relevant to paroxysmal cold hemoglobinuria as it is manifest in the modern era. As children with paroxysmal cold hemoglobinuria do not usually have hemolysis directly related to exposure to the cold (e.g., they continue hemolysis when in a warm hospital environment), it has been suggested that a better term might be Donath-Landsteiner test positive hemolytic anemia.
Chronic idiopathic paroxysmal cold hemoglobinuria cases also occur but are extremely rare. Acute cases of paroxysmal cold hemoglobinuria are characterized by an abrupt onset with features of severe intravascular hemolysis including high fever, chills, back and/or leg pain. Other symptoms may include nausea, headache, vomiting and diarrhea. Typically hemoglobinuria occurs, producing dark red to black urine. Hemolysis can be severe and even life-threatening and results from exposure to cold, which may even be localized (eg from drinking cold water, from washing hands in cold water). Chronic forms of paroxysmal cold hemoglobinuria are characterized by recurrent episodes of hemolysis precipitated by cold exposure.
Autoimmune hemolytic anemias as a group are estimated to affect 1-3 people per 100,000 in the general population. Both the syphilitic and non-syphilitic forms of chronic paroxysmal cold hemoglobinuria are exceedingly rare. The prevalence and incidence rates are unknown. Anyone may acquire paroxysmal cold hemoglobinuria, but it is more common among children than among adults. An individual with a viral infection is at higher risk of contracting the disorder. No known genetic, sex, or racial risk factors exist, although the disease has been reported in families.
Paroxysmal cold hemoglobinuria causes
In most affected children, paroxysmal cold hemoglobinuria occurs as an acute hemolytic anemia, following an infection, mainly upper respiratory and the causative agent is often not identified and spontaneously resolves once the infection subsides. Usually, paroxysmal cold hemoglobinuria does not recur (self-limited) in children, but recurrent cases have been reported in the medical literature. In most adults the cause of paroxysmal cold hemoglobinuria is unknown (idiopathic) and is usually a chronic disease. With the dramatic decline in the prevalence of syphilis, paroxysmal cold hemoglobinuria in adults has declined, and the current understanding of the adult form of the disease is less clear.
Paroxysmal cold hemoglobinuria is an autoimmune disorder, a disorder in which the body’s natural defenses against invading organisms destroy healthy tissue for unknown reasons. In paroxysmal cold hemoglobinuria, antibodies mistakenly attack red blood cells causing the cells to breakdown prematurely, a condition called (hemolysis). When antibodies attack healthy tissue, they are referred to as autoantibodies.
Antibodies (which are also known as immunoglobulins) are specialized proteins that bind to invading organisms and bring about their destruction. There are five main classes of antibodies – IgA, IgD, IgE, IgG, and IgM. In paroxysmal cold hemoglobinuria, a specific autoantibody known as the Donath-Landsteiner autoantibody is produced often in response to a viral infection. This autoantibody binds to red blood cells during exposure to cold temperatures. The Donath-Landsteiner autoantibody is a type of IgG antibody; its target is the P blood group antigen, present on the red cells of almost all individuals.
Paroxysmal cold hemoglobinuria symptoms
Acute paroxysmal cold hemoglobinuria cases almost exclusively affect children and are often preceded by symptoms of infection. Chronic idiopathic paroxysmal cold hemoglobinuria cases also occur but are extremely rare.
Acute cases of paroxysmal cold hemoglobinuria typical presentation is that of a child who during the preceding 1-2 weeks had suffered from what appeared to be an undefined or “flu-like” illness. Usually the onset of intravascular hemolysis is signaled by a recurrence of high fever, chills, back and/or leg pain and then the passage of red-brown urine. Hemolysis can be severe and even life-threatening and results from exposure to cold, which may even be localized (eg from drinking cold water, from washing hands in cold water). Other symptoms may include nausea, headache, abdominal pain, vomiting and diarrhea. The urine contains the iron bearing, oxygen transporting, protein pigment of blood called hemoglobin, which is released when red blood cells are prematurely destroyed. The presence of hemoglobin in the urine (hemoglobinuria) causes the dark brown color of the urine. Hemoglobinuria, hemoglobinemia (hemoglobin in the plasma), jaundice and pallor are common clinical findings in acute paroxysmal cold hemoglobinuria and, of particular significance is that hemoglobinuria is found in almost all acute cases in childhood.
Approximately 25 percent of cases have palpable liver and spleen. Although hemoglobinuria may be induced by exposure to cold, such an occurrence is rare in acute paroxysmal cold hemoglobinuria. In acute paroxysmal cold hemoglobinuria, hemolysis typically lasts for a few days only and recovery is usually uninterrupted.
The older medical literature describes chronic syphilitic paroxysmal cold hemoglobinuria as a rather benign disease that rarely caused severe chronic anemia. Chronic forms of paroxysmal cold hemoglobinuria are characterized by recurrent episodes of hemolysis precipitated by cold exposure. However, acute attacks of hemolysis and hemoglobinuria were well known and were characterized by the sudden onset of shaking chills, fever, malaise, abdominal distress, aching pains in the back or legs, arid nausea. Usually, hemoglobin was present in the first specimen of urine passed after the onset of symptoms, and the interval between chilling and the development of symptoms ranged from a few minutes to eight hours. The extent of cold exposure could be surprisingly slight and, in some cases, a history of undue exposure to cold was not elicited.
Individuals with paroxysmal cold hemoglobinuria often develop the classic symptoms of anemia- the medical term for low levels of circulating red blood cells. These symptoms may include fatigue, difficulty breathing upon exertion (dyspnea) and abnormal or extreme paleness of the skin (pallor). In addition, affected individuals may develop chills, fever, abdominal pain, and pain or aching in the legs or lower back. Less common findings associated with paroxysmal cold hemoglobinuria include headaches, vomiting and diarrhea.
Following an episode, affected individuals usually develop the signs of hemolysis including yellowing of the skin, whites of the eyes and mucous membranes (jaundice). In some cases additional symptoms may occur including tingling in the hands and feet, a condition marked by a feeling of coldness or numbness of the hands, nose and ears in response to cold temperatures (Raynaud’s phenomenon), or a skin condition marked by reddening and itching of the skin in response to cold temperatures (cold urticaria). In extremely rare cases, the kidney may become involved and kidney (renal) failure has been reported in a few cases.
Paroxysmal cold hemoglobinuria diagnosis
A diagnosis of paroxysmal cold hemoglobinuria may be suspected in some individuals with anemia. In particular, the diagnosis should be suspected in any acutely ill child with hemoglobinuria. Paroxysmal cold hemoglobinuria diagnosis is based upon a thorough clinical evaluation, a detailed patient history, identification of characteristic symptoms and a variety of specialized tests such as a direct antiglobulin test (Coombs) test, which is used to detect certain antibodies that act against red blood cells.
A diagnosis of paroxysmal cold hemoglobinuria is confirmed by the results of a Donath-Landsteiner test, which can distinguish paroxysmal cold hemoglobinuria from other forms of hemolytic anemia and evidence of anti-P specificity of the IgG autoantibodies. The Donath-Landsteiner test consists of incubating a sample of the patient’s serum with normal red blood cells (RBCs) in the cold for 30 minutes and then warming the mixture to body temperature (37 °C). Hemolysis of the RBCs in this “bi-phasic” test indicates a diagnosis of paroxysmal cold hemoglobinuria.
Paroxysmal cold hemoglobinuria differential diagnosis
The main differential diagnosis is acute cold autoimmune hemolytic anemia induced by an infection, for example Mycoplasma pneumoniae or the Epstein Barr virus, due to the presence of IgM autoantibodies which are cold agglutinins.
Paroxysmal cold hemoglobinuria treatment
Most cases of paroxysmal cold hemoglobinuria are self-limited (resolve spontaneously without treatment) so treatment is usually symptomatic for a few days to weeks after onset, including keeping the patient warm. Strict avoidance of cold temperatures is recommended to protect against the premature breakdown of red blood cells and loss of hemoglobin (hemolysis). In some cases, severe anemia may require a red blood cell transfusion. In such cases, a transfusion should not be delayed. Use of a blood warmer during transfusion is sometimes recommended. Patients with few clinical symptoms and slight anemia may not require drug therapy. Corticosteroids and splenectomy are usually ineffective and should not be considered. In cases of life-threatening paroxysmal cold hemoglobinuria, plasmapheresis can temporarily dampen the hemolysis. Some patients may respond to rituximab, although responses are usually short-lived. If syphilis is present, treatment with antibiotics generally eliminates the concurrent hemolysis.
Due to the temporary (transient) nature of the disease in children in most cases, affected children are often in the recovery phase of the illness at the time symptoms become apparent. Most cases that involve children and are linked to a viral infection require only supportive therapy, bed rest, and protection of the affected individual from cold temperatures.
Investigational therapies
In some cases of chronic paroxysmal cold hemoglobinuria additional therapies may be tried to help manage the disease. Steroids have been used but often with ineffective results. Researchers are studying other drugs that suppress the immune system (immunosuppressive agents) such as Rituximab for the treatment of chronic paroxysmal cold hemoglobinuria that does not respond to other therapies (refractory paroxysmal cold hemoglobinuria). More research is necessary to determine the long-term safety and effectiveness of immunosuppressive drugs for the treatment of individuals with refractory paroxysmal cold hemoglobinuria.
Paroxysmal cold hemoglobinuria prognosis
Acute episodes are generally transitory and rarely recur. The prognosis in paroxysmal cold hemoglobinuria is excellent with supportive therapy.
The chronic idiopathic forms may persist for years with variable morbidity.
Paroxysmal cold hemoglobinuria usually ameliorates if the underlying disease responds to specific therapy.
References- Hemolytic Anemia. https://emedicine.medscape.com/article/201066-overview
- Renard D, Rosselet A. Drug-induced hemolytic anemia: Pharmacological aspects. Transfus Clin Biol. 2017 Sep. 24 (3):110-114.
- Chiao EY, Engels EA, Kramer JR, Pietz K, Henderson L, Giordano TP, et al. Risk of immune thrombocytopenic purpura and autoimmune hemolytic anemia among 120 908 US veterans with hepatitis C virus infection. Arch Intern Med. 2009 Feb 23. 169(4):357-63.
- Zamvar V, McClean P, Odeka E, Richards M, Davison S. Hepatitis E virus infection with nonimmune hemolytic anemia. J Pediatr Gastroenterol Nutr. 2005 Feb. 40(2):223-5.
- Rink BD, Gonik B, Chmait RH, O’Shaughnessy R. Maternal hemolysis after intravenous immunoglobulin treatment in fetal and neonatal alloimmune thrombocytopenia. Obstet Gynecol. 2013 Feb. 121(2 Pt 2 Suppl 1):471-3.
- Mayer B, Leo A, Herziger A, Houben P, Schemmer P, Salama A. Intravascular immune hemolysis caused by the contrast medium iomeprol. Transfusion. 2013 Jan 24.
- Acharya D, McGiffin DC. Hemolysis after Mitral Valve Repair. J Card Surg. 2013 Jan 13. 1-4.
- Hill A, Hill QA. Autoimmune hemolytic anemia. Hematology Am Soc Hematol Educ Program. 2018 Nov 30. 2018 (1):382-389.
- Sanz J, Arriaga F, Montesinos P, Ortí G, Lorenzo I, Cantero S, et al. Autoimmune hemolytic anemia following allogeneic hematopoietic stem cell transplantation in adult patients. Bone Marrow Transplant. 2007 May. 39(9):555-61.
- Singh A, Mandal A, Patel A, Mishra S. Autoimmune Haemolytic Anaemia-A Spectrum of Presentation in Children. J Clin Diagn Res. 2017 Sep. 11 (9):SR01-SR02.
- Moreira M, Brás R, Gonçalves D, Alencoão I, Inocêncio G, Rodrigues M, et al. Fetal Splenomegaly: A Review. Ultrasound Q. 2017 Nov 29.
- Lechner K, Obermeier HL. Cancer-related microangiopathic hemolytic anemia: clinical and laboratory features in 168 reported cases. Medicine (Baltimore). 2012 Jul. 91 (4):195-205.
- Paroxysmal nocturnal hemoglobinuria. https://ghr.nlm.nih.gov/condition/paroxysmal-nocturnal-hemoglobinuria
- Paroxysmal Nocturnal Hemoglobinuria. https://emedicine.medscape.com/article/207468-overview
- Paroxysmal Nocturnal Hemoglobinuria (PNH). https://www.aamds.org/diseases/pnh
- Parker CJ. The pathophysiology of paroxysmal nocturnal hemoglobinuria. Exp Hematol. 2007;35:523-33. https://doi.org/10.1016/j.exphem.2007.01.046
- Dulau-Florea A, Maric I, Calvo KR, Braylan RC. Detection of paroxysmal nocturnal hemoglobinuria (PNH) in bone marrow aspirates☆. Semin Hematol. 2019 Jan. 56 (1):65-68.
- Paroxysmal Nocturnal Hemoglobinuria Treatment & Management. https://emedicine.medscape.com/article/207468-treatment
- Sicre de Fontbrune F, Peffault de Latour R. Ten Years of Clinical Experience With Eculizumab in Patients With Paroxysmal Nocturnal Hemoglobinuria. Semin Hematol. 2018 Jul. 55 (3):124-129.
- Hillmen P, Lewis SM, Bessler M, Luzzatto L, Dacie JV. Natural history of paroxysmal nocturnal hemoglobinuria. N Engl J Med. 1995 Nov 9. 333(19):1253-8.
- Griffin M, Munir T. Management of thrombosis in paroxysmal nocturnal hemoglobinuria: a clinician’s guide. Ther Adv Hematol. 2017 Mar. 8 (3):119-126.
- Risitano AM, Marotta S. Toward complement inhibition 2.0: Next generation anticomplement agents for paroxysmal nocturnal hemoglobinuria. Am J Hematol. 2018 Aug. 93 (4):564-577.
- Notaro R, Sica M. C3-mediated extravascular hemolysis in PNH on eculizumab: Mechanism and clinical implications. Semin Hematol. 2018 Jul. 55 (3):130-135.
- Yuan X, Gavriilaki E, Thanassi JA, Yang G, Baines AC, Podos SD, et al. Small-molecule factor D inhibitors selectively block the alternative pathway of complement in paroxysmal nocturnal hemoglobinuria and atypical hemolytic uremic syndrome. Haematologica. 2017 Mar. 102 (3):466-475.
- Paroxysmal Cold Hemoglobinuria. https://rarediseases.org/rare-diseases/paroxysmal-cold-hemoglobinuria
- Paroxysmal Cold Hemoglobinuria. https://emedicine.medscape.com/article/200947-overview