What is a runny nose
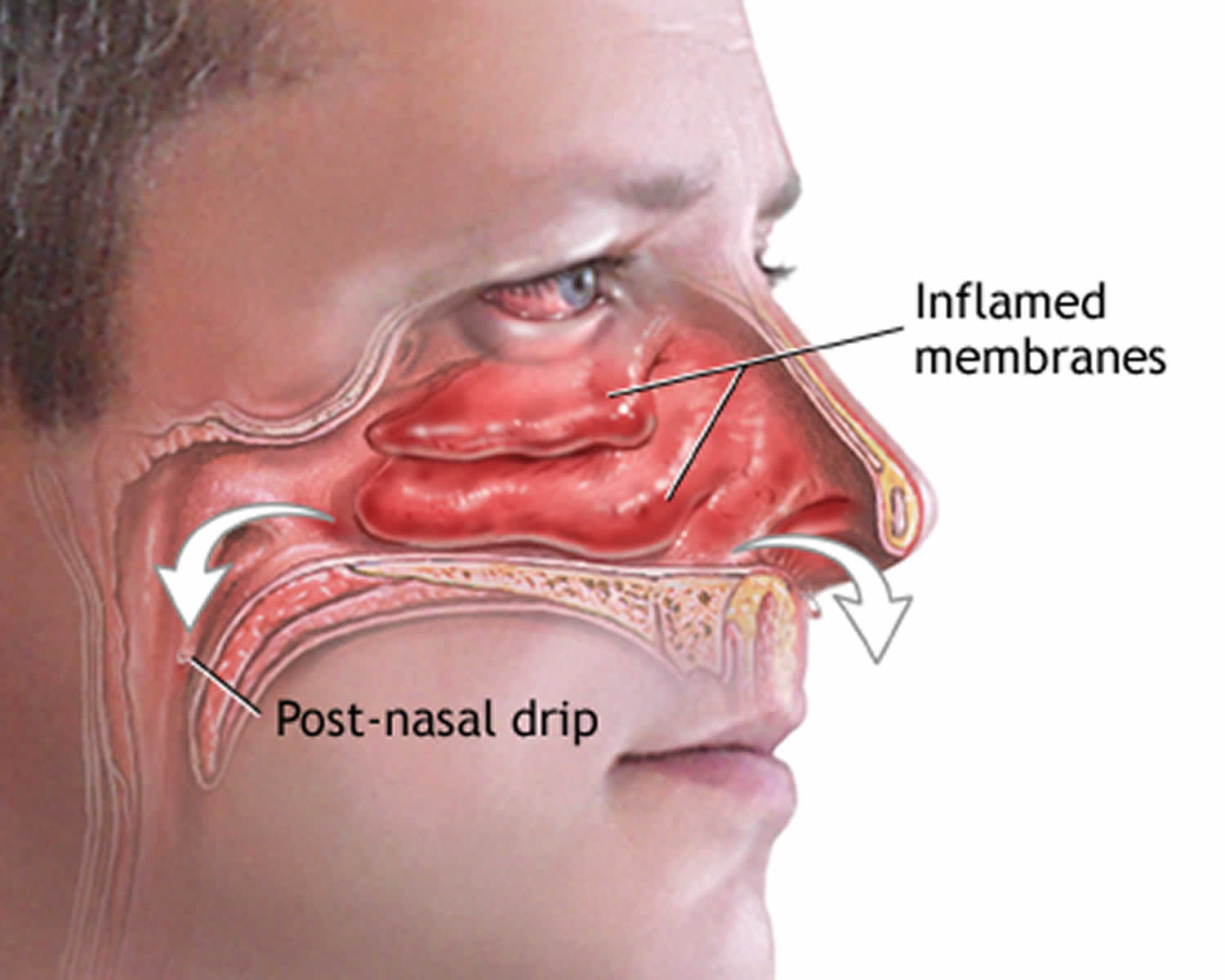
Runny nose also called rhinorrhea or rhinitis, is excess nasal discharge produced by nasal and adjacent tissues and blood vessels in the nose. Runny nose may range from a clear fluid to thick mucus. Runny nose drainage may run out of your nose, down the back of your throat (postnasal drip) or both and it may cause a cough or sore throat.
Strictly speaking, rhinorrhea refers to a thin, relatively clear nasal discharge. Rhinitis refers to inflammation of the nasal tissues from a number of causes, which usually results in a runny nose.
Nasal congestion may or may not accompany runny nose.
The mucus drainage may plug up the eustachian tube between the nose and the ear, causing an ear infection and pain. The mucous drip may also plug the sinus passages, causing sinus infection and pain.
See the doctor if you or your child has any of the following:
- A stuffy nose with swelling of the forehead, eyes, side of the nose, or cheek, or that occurs with blurred vision
- More throat pain, or white or yellow spots on the tonsils or other parts of the throat
- Discharge from the nose that has a bad smell, comes from only one side, or is a color other than white or yellow
- Cough that lasts longer than 10 days, or produces yellow-green or gray mucus
- Symptoms that last more than 3 weeks
- Nasal discharge with fever
What causes a runny nose
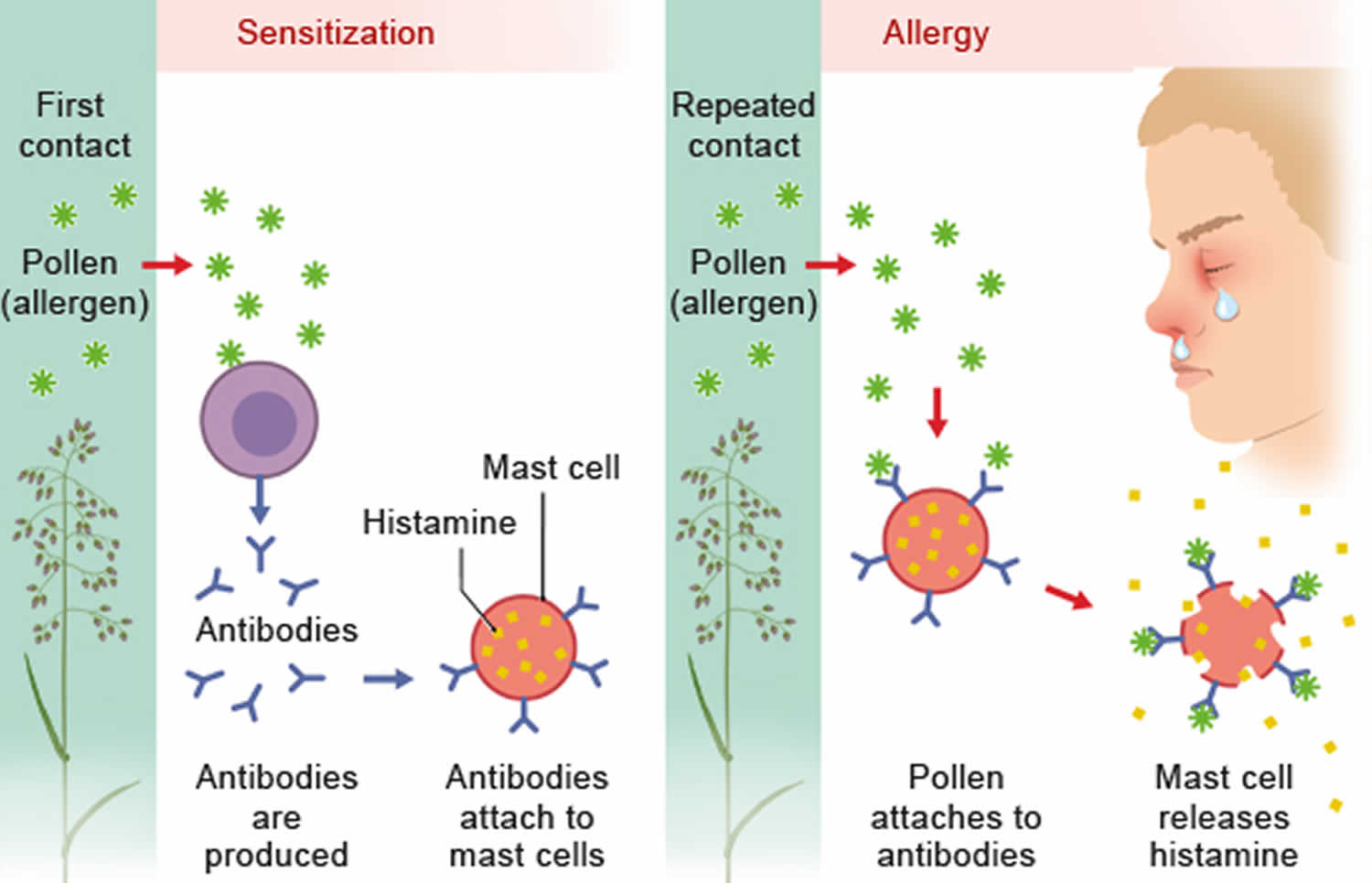
Runny nose can be caused by anything that irritates or inflames the nasal tissues. Infections — such as the common cold and influenza — allergies and various irritants may all cause a runny nose. Some people have a chronically runny nose for no apparent reason — a condition called nonallergic rhinitis or vasomotor rhinitis.
Less commonly, runny nose can be caused by polyps, a foreign body, a tumor or migraine-like headaches.
Causes of runny nose include:
- Acute sinusitis (sinus infection)
- Allergies
- Cerebrospinal fluid (CSF) leak 1
- Chronic sinusitis
- Churg-Strauss syndrome
- Common cold
- Decongestant nasal spray overuse or use of some nasal sprays or drops bought without a prescription for more than 3 days (may make nasal stuffiness worse)
- Deviated septum
- Drug addiction (substance use disorder)
- Dry air
- Granulomatosis with polyangiitis (Wegener’s)
- Hay fever
- Hormonal changes
- Influenza (flu)
- Lodged object in the nostril or nose
- Medications
- Nasal polyps
- Nonallergic rhinitis (chronic congestion or sneezing not related to allergies)
- Occupational asthma
- Pregnancy
- Respiratory syncytial virus (RSV)
- Tobacco smoke
Table 1. Know the difference between Cold, Flu and Allergy
| Symptoms | Common Cold | Flu | Airborne Allergy |
|---|---|---|---|
| Fever | Rare | Usual, high (100-102 °F), sometimes higher, especially in young children); lasts 3-4 days | Never |
| Headache | Uncommon | Common | Uncommon |
| General Aches, Pains | Slight | Usual; often severe | Never |
| Fatigue, Weakness | Sometimes | Usual, can last up to 3 weeks | Sometimes |
| Extreme Exhaustion | Never | Usual, at the beginning of the illness | Never |
| Stuffy, Runny Nose | Common | Sometimes | Common |
| Sneezing | Usual | Sometimes | Usual |
| Sore Throat | Common | Sometimes | Sometimes |
| Cough | Common | Common, can become severe | Sometimes |
| Chest Discomfort | Mild to moderate | Common | Rare, except for those with allergic asthma |
| Treatment | Get plenty of rest. Stay hydrated. (Drink plenty of fluids.) Decongestants. Aspirin (ages 18 and up), acetaminophen, or ibuprofen for aches and pains | Get plenty of rest. Stay hydrated. Aspirin (ages 18 and up), acetaminophen, or ibuprofen for aches, pains, and fever Antiviral medicines (see your doctor) | Avoid allergens (things that you’re allergic to) Antihistamines Nasal steroids Decongestants |
| Prevention | Wash your hands often. Avoid close contact with anyone who has a cold. | Get the flu vaccine each year. Wash your hands often. Avoid close contact with anyone who has the flu. | Avoid allergens, such as pollen, house dust mites, mold, pet dander, cockroaches. |
| Complications | Sinus infection middle ear infection, asthma | Bronchitis, pneumonia; can be life-threatening | Sinus infection, middle ear infection, asthma |
What is respiratory syncytial virus (RSV)?
Respiratory syncytial virus (RSV) is the most common cause of respiratory and breathing infections in children. It is a virus that causes infection of the lungs and breathing passages, and is one of the most frequent causes of the common cold.
Respiratory syncytial virus (RSV) can affect people of all ages. Most children aged under two years have been infected by RSV at some stage, and it is possible to get respiratory syncytial virus (RSV) over and over again. Good hygiene habits can reduce the chance of your child getting the virus or passing it on to others.
Key points to remember
- Respiratory syncytial virus (RSV) is the most common cause of respiratory and breathing infections in children.
- Respiratory syncytial virus (RSV) is a common cause of bronchiolitis and pneumonia in children under one year old, and may trigger symptoms in children with asthma.
- Your child can go to school if they feel OK and are not spreading the virus via coughing or sneezing.
- Respiratory syncytial virus (RSV) is very infectious, so good hygiene is important to avoid spreading the virus.
- Try to keep infected children away from newborn babies and people with weakened immune systems.
What’s the difference between a cold and RSV?
Respiratory syncytial virus (RSV) is one of many viruses that causes the common cold, and it can be hard to tell which virus your child has. It doesn’t really matter if we know which virus it is, because treatment is the same – plenty of rest and fluids, and no antibiotics, because antibiotics don’t work on viruses. However, respiratory syncytial virus (RSV) can lead to other problems in some children, including bronchiolitis and pneumonia. It can also worsen existing problems, like asthma.
Is there a vaccine to prevent RSV?
There is currently no vaccine to prevent respiratory syncytial virus (RSV). However, researchers are working towards developing vaccines and antiviral therapies to help protect infants and young children, as well as pregnant women, from severe respiratory syncytial virus (RSV) infection. If your child were to contract respiratory syncytial virus (RSV) a second time in the same season, their illness is likely to be more mild than the first episode.
How is respiratory syncytial virus (RSV) spread?
Children with respiratory syncytial virus (RSV) are usually infectious (able to pass the virus onto others) for eight days from the start of their symptoms. Respiratory syncytial virus (RSV) is very contagious and can live on surfaces for several hours, and on unwashed hands for 30–60 minutes. Respiratory syncytial virus (RSV) spreads quickly and easily among children through coughing and sneezing, and sharing cups and other objects that have been in contact with the infected child’s mouth, nose or eyes.
It can be difficult to stop the spread of respiratory syncytial virus (RSV); however, practising good hygiene will help avoid passing any virus onto others.
- Don’t allow children to share drinks, cutlery or toys (whenever possible) and ensure these items are cleaned thoroughly with soap and water between uses.
- Encourage your child to cough and sneeze into a tissue, then throw the tissue away.
- It is very important that you and/or your child wash their hands once they have blown their nose to stop the germs from spreading.
- Wash your hands after having any contact with someone who has symptoms of a cold.
If your child has RSV (or cold-like symptoms), it is important to keep them away from newborn babies or people who are immunocompromised (have a weakened immune system).
Signs and symptoms of respiratory syncytial virus (RSV):
After exposure to the virus, your child may only develop symptoms around five days later. Respiratory syncytial virus (RSV) in children is normally associated with mild to moderate cold-like symptoms, which generally last between eight and 15 days. If your child has RSV they may have some or all of the following symptoms:
- runny nose
- coughing
- wheezing
- fever.
Respiratory syncytial virus (RSV) is a common cause of bronchiolitis and pneumonia in children under one year old. If your child has asthma, RSV is likely to trigger their asthma symptoms.
Care at home
Most cases of respiratory syncytial virus (RSV) are mild and can be treated with rest at home. If your child has RSV:
- Keep them home if they feel unwell. If they feel well and are not coughing and sneezing, they can continue with their normal activities (kindergarten, school etc.).
- Encourage your child to drink small amounts of fluids more frequently. If an infant has RSV, give them small amounts of fluid (breastmilk, formula or water) regularly.
- See our fact sheet Fever in children for advice on managing your child’s fever if it is causing them discomfort.
When to see a doctor
Take your child to the doctor if:
- they have a high temperature (fever) and do not look well
- their nose is filled with mucus and they are having difficulty feeding
- the cough becomes worse, or your child starts coughing up mucus
- your child is dehydrated
- they are a baby and refusing to breast or bottle feed and are irritable.
Call an ambulance or go to your nearest hospital emergency department if your child is turning blue, having trouble breathing, or is breathing very quickly.
After seeing your child, the doctor may ask to review your child again the following day. Take them back sooner if your child:
- is having more difficulty breathing or breathing faster
- is looking more unwell
- is not taking at least half of their normal fluids
- has a cough that is getting worse.
Runny nose diagnosis
Your healthcare provider may perform a physical exam that focuses on the ears, nose, throat, and airways.
Tests that may be done include:
- Allergy tests skin and blood tests
- Blood tests (such as complete blood count or blood differential)
- Sputum culture and throat culture
- X-rays of the sinuses and chest x-ray
- CT scan of the head
How to stop a runny nose
Treatment depends on the causes of your runny nose. A health professional can help you choose the best therapy.
Common Cold
- Symptoms last up to 2 weeks
- Stuffy, runny nose; sore throat; cough
- Treated with rest, fluids and over-the-counter (OTC) medicines to ease symptoms. Viruses cannot be treated with antibiotics. The best treatment is rest at home to allow your child’s immune system to fight the virus. Here are some simple measures that can make you or your child more comfortable:
- Give your child small amounts to drink frequently when awake, such as a mouthful of water every 15 minutes or so. This helps to ease a sore throat by keeping it moist, and replaces the fluid lost due to having a fever, vomiting or diarrhea. Water is best, but rehydrating icy poles are also a good way of providing fluids to your child.
- Giving enough fluid is particularly important in infants – this should be breastmilk or formula, or rehydration fluids such as pedialyte.
- Do not be concerned if your child does not eat for a few days. When they feel better they will start eating again.
- Allow your child to rest.
- Use saline nasal (nose) drops to help clear a blocked nose in babies. A baby with a clear nose will find it easier to feed.
- Give your child paracetamol or ibuprofen for pain, or if your child is miserable, irritable or lethargic. See our fact sheet Pain relief for children. Do NOT give your child aspirin. Carefully check the label for the correct dose and make sure you are not already giving your child any other products containing paracetamol or ibuprofen (such as some cough medicines and cold-and-flu preparations).
- Do not use paracetamol or ibuprofen just to reduce fever. Fever helps the body get better naturally.
- Do not use other remedies unless advised by a doctor or health care professional.
- Your child is likely to feel better in a few days, but may be unwell for up to two weeks. A cough can linger for several weeks.
- Most rashes are mild and do not cause your child any distress, although some rashes can cause a lot of itching. Talk to your local pharmacist about treatments that can help relieve itchy rashes. A rash often lasts a few days before going away on its own. Sometimes a rash appears when a fever goes away. When this rash appears, it means the child is getting better.
Seasonal Flu
- Symptoms usually last 1-2 weeks
- High fever (100-102 °F [37.8-39 °C] or higher in youngsters), headache, aches and pains, weakness, exhaustion, cough, chest discomfort
- Treated with rest, fluids, over-the-counter medicines, prescription antiviral drugs
Airborne Allergy
- Lasts as long as allergens (such as pollen, pet dander) are present
- Stuffy, runny nose; itchy, watery eyes
- Treated with non-sedating antihistamines, decongestants and low-dose steroid nasal sprays.
Home care for infants and young children
Tips to help infants and younger children include:
- Raise the head of your child’s bed. Put a pillow underneath the head of the mattress. Or, place books or boards under the legs at the head of the bed.
- Older children may drink extra fluids, but those fluids should be sugar-free.
- You can try a cool-mist vaporizer, but avoid putting too much moisture in the room. Clean the vaporizer every day with bleach or Lysol.
- You can also steam up the bathroom shower and bring your child in there before bed.
A nasal wash can help remove mucus from your child’s nose:
- You can buy a saline spray at a drugstore or make one at home. To make one, use 1 cup (240 milliliters) of warm water, 1/2 teaspoon (3 grams) of salt, and a pinch of baking soda.
- Use gentle saline nasal sprays 3 to 4 times per day.
If your child has allergies:
- Your health care provider may also prescribe nasal sprays that treat allergy symptoms.
- Learn how to avoid triggers that make allergies worse.
Nasal sprays are not recommended for children under age 2. Don’t use over-the-counter nasal sprays more often than 3 days on and 3 days off, unless told to by your provider.
You can buy cough and cold medicines without a prescription. They do not seem to be effective in children.
Home care for adults
Finding ways to keep mucus thin will help it drain from your nose and sinuses and relieve your symptoms. Drinking plenty of clear fluids is one way to do this. You can also:
- Apply a warm, moist washcloth to your face several times a day.
- Inhale steam 2 to 4 times a day. One way to do this is to sit in the bathroom with the shower running. Do not inhale hot steam.
- Use a vaporizer or humidifier.
A nasal wash can help remove mucus from your nose:
- You can buy a saline spray at a drugstore or make one at home. To make one, use 1 cup (240 milliliters) of warm water, 1/2 teaspoon (3 grams) of salt, and a pinch of baking soda.
- Use gentle saline nasal sprays 3 to 4 times per day.
Congestion is often worse when lying down. Keep upright, or at least keep the head elevated.
Some stores sell adhesive strips that can be placed on the nose. These help widen the nostrils, making breathing easier.
Medicines you can buy at the store without a prescription can help your symptoms:
- Decongestants are drugs that shrink and dry up your nasal passages. They may help dry up a runny or stuffy nose.
- Antihistamines are drugs that treat allergy symptoms. Some antihistamines make you drowsy so use with care.
- Nasal sprays can relieve stuffiness. Don’t use over-the-counter nasal sprays more often than 3 days on and 3 days off, unless told to by your health care provider.
Many cough, allergy, and cold medicines you buy have more than one medicine inside. Read the labels carefully to make sure you don’t take too much of any one medicine. Ask your provider which cold medicines are safe for you.
If you have allergies:
- Your healthcare provider may also prescribe nasal sprays that treat allergy symptoms.
- Learn how to avoid triggers that make allergies worse.
- Common allergens include the following:
- Pollen
- House dust mites
- Pets and farm animals
- The venom (poison) in insect stings and bites
- Foods
- Medication
- Contact allergens (e.g. metals or fragrance ingredients)
- Mold
- Common allergens include the following:
- Yadav YR, Parihar V, Janakiram N, Pande S, Bajaj J, Namdev H. Endoscopic management of cerebrospinal fluid rhinorrhea. Asian Journal of Neurosurgery. 2016;11(3):183-193. doi:10.4103/1793-5482.145101. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4849285/
- https://newsinhealth.nih.gov/2014/10/cold-flu-or-allergy