What is hydrocodone
Hydrocodone is an opioid agonist with analgesic (narcotic analgesic) and antitussive effects that is used to relieve severe pain and also used as cough suppressant. Opioids are sometimes called narcotics. Hydrocodone is only used to treat people who are expected to need medication to relieve severe pain around-the-clock for a long time and who cannot be treated with other medications or treatments. Hydrocodone extended-release (long-acting) capsules or extended-release tablets should not be used to treat pain that can be controlled by medication that is taken as needed. Hydrocodone is in a class of medications called opiate (narcotic) analgesics.
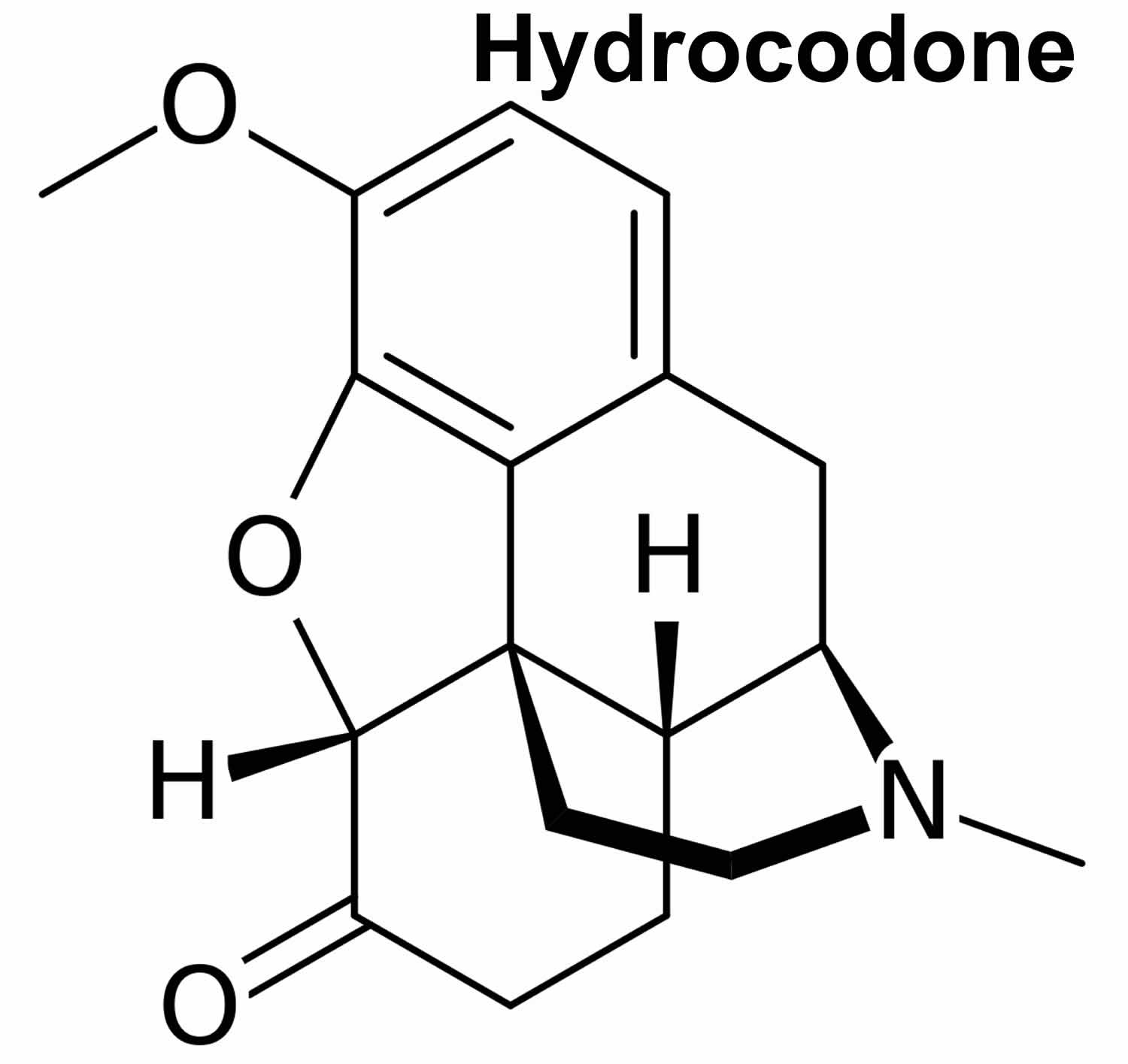
Hydrocodone is a semisynthetic hydrogenated codeine derivative, but more potent and more addicting by weight. Hydrocodone works by primarily binding to and activating the mu-opioid receptor in the central nervous system (CNS). This leads to analgesia, euphoria, respiratory depression, miosis (constricted or pinpoint pupil), decreased gastrointestinal motility, cough suppression and physical dependence. Hydrocodone is converted to hydromorphone by the cytochrome P450 enzyme CYP2D6. Hydrocodone may potentiate the effects of other opiate agonists, general anesthetics, tranquilizers, sedatives and hypnotics, tricyclic antidepressants, monoamine oxidase inhibitors, alcohol, and other CNS depressants 1.
When hydrocodone is used for a long time, it may become habit-forming, causing mental or physical dependence. Physical dependence may lead to withdrawal side effects if treatment is stopped suddenly.
Hydrocodone is available only with your doctor’s prescription.
Some commonly used hydrocodone products also contain other medications, such as acetaminophen. These include the brand names Lortab®, Norco®, Zydone® and Vicodin HP®.
Important information
Hydrocodone can slow or stop your breathing. Never use this medicine in larger amounts, or for longer than prescribed. Do not crush, break, or open an extended-release pill. Swallow it whole to avoid exposure to a potentially fatal dose. Hydrocodone may be habit-forming, even at regular doses. Never share this medicine with another person, especially someone with a history of drug abuse or addiction. Keep the medication in a place where others cannot get to it.
MISUSE OF NARCOTIC MEDICATION CAN CAUSE ADDICTION, OVERDOSE, OR DEATH, especially in a child or other person using the medicine without a prescription.
You should not use hydrocodone if you have severe asthma or breathing problems, or a blockage in your stomach or intestines.
Tell your doctor if you are pregnant. Hydrocodone may cause life-threatening withdrawal symptoms in a newborn if the mother has taken hydrocodone during pregnancy.
Do not drink alcohol. Dangerous side effects or death could occur when alcohol is combined with this medicine.
Hydrocodone can be habit forming, especially with prolonged use. Take hydrocodone exactly as directed. Do not take more of it, take it more often, or take it in a different way than directed by your doctor. While taking hydrocodone, discuss with your health care provider your pain treatment goals, length of treatment, and other ways to manage your pain. Tell your doctor if you or anyone in your family drinks or has ever drunk large amounts of alcohol, uses or has ever used street drugs, or has overused prescription medications, or if you have or have ever had depression or another mental illness. There is a greater risk that you will overuse hydrocodone if you have or have ever had any of these conditions. Talk to your health care provider immediately and ask for guidance if you think that you have an opioid addiction or call the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-4357.
Do not allow anyone else to take your medication. Hydrocodone may harm or cause death to other people who take your medication, especially children. Keep hydrocodone in a safe place so that no one else can take it accidentally or on purpose. Be especially careful to keep hydrocodone out of the reach of children. Keep track of how many capsules or tablets are left so you will know if any medication is missing.
Hydrocodone may cause slowed or stopped breathing, especially during the first 24 to 72 hours of your treatment and any time your dose is increased. Your doctor will monitor you carefully during your treatment. Your doctor will adjust your dose to control your pain and decrease the risk that you will experience serious breathing problems. Tell your doctor if you have or have ever had slowed breathing or asthma. Your doctor will probably tell you not to take hydrocodone. Also tell your doctor if you have or have ever had lung disease such as chronic obstructive pulmonary disease (COPD; a group of diseases that affect the lungs and airways), a head injury, or any condition that increases the amount of pressure in your brain. The risk that you will develop breathing problems may be higher if you are an older adult or are weakened or malnourished due to disease. If you experience any of the following symptoms, call your doctor immediately or get emergency medical treatment: slowed breathing, long pauses between breaths, or shortness of breath.
Taking certain medications or stopping treatment with certain other medications while you are taking hydrocodone may increase the risk that you will experience breathing problems, sedation, coma, or other serious, life-threatening side effects. Tell your doctor if you are taking, plan to take or plan to stop taking any of the following medications: certain antifungal medications including itraconazole (Onmel, Sporanox), ketoconazole (Extina, Nizoral, Xolegel), and voriconazole (Vfend); benzodiazepines such as alprazolam (Xanax), chlordiazepoxide (Librium), clonazepam (Klonopin), diazepam (Diastat, Valium), estazolam, flurazepam, lorazepam (Ativan), oxazepam, temazepam (Restoril), and triazolam (Halcion); carbamazepine (Carbatrol, Epitol, Equetro, Tegretol, others); cimetidine; clarithromycin (Biaxin, in Prevpac); erythromycin (E.E.S., Erythromycin, others); other narcotic pain medications; medications for mental illness or nausea; certain medications for human immunodeficiency virus (HIV) including ritonavir (Norvir, in Kaletra, in Viekira Pak); muscle relaxants; phenytoin (Dilantin, Phenytek); rifampin (Rifadin, Rimactane, in Rifamate, in Rifater); sedatives; sleeping pills; or tranquilizers. If you take hydrocodone with any of these medications and you develop any of the following symptoms, call your doctor immediately or seek emergency medical care: unusual dizziness, lightheadedness, extreme sleepiness, slowed or difficult breathing, or unresponsiveness. Be sure that your caregiver or family members know which symptoms may be serious so they can call the doctor or emergency medical care if you are unable to seek treatment on your own.
Drinking alcohol, taking prescription or nonprescription medications that contain alcohol, or using street drugs during your treatment with hydrocodone increases the risk that you will experience these serious, life-threatening side effects. Do not drink alcohol, take prescription or nonprescription medications that contain alcohol, or use street drugs during your treatment.
Swallow hydrocodone extended-release capsules or extended-release tablets whole; do not chew, break, divide, crush, or dissolve them. Hydrocodone extended-release capsules and extended-release tablets are difficult to crush, break or dissolve. If you swallow broken, chewed, or crushed extended-release capsules or extended-release tablets, you may receive too much hydrocodone at once. This may cause serious problems, including overdose and death.
Tell your doctor if you are pregnant or plan to become pregnant. If you take hydrocodone regularly during your pregnancy, your baby may experience life-threatening withdrawal symptoms after birth. Tell your baby’s doctor right away if your baby experiences any of the following symptoms: irritability, hyperactivity, abnormal sleep, high-pitched cry, uncontrollable shaking of a part of the body, vomiting, diarrhea, or failure to gain weight.
Your doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with hydrocodone and each time you refill your prescription. Read the information carefully and ask your doctor or pharmacist if you have any questions. You can also visit the Food and Drug Administration (FDA) website (https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm) or the manufacturer’s website to obtain the Medication Guide.
Talk to your doctor about the risks of taking hydrocodone.
Pregnancy Considerations
Prolonged maternal use of opioids during pregnancy can cause neonatal withdrawal syndrome in the newborn which may be life-threatening if not recognized and treated according to protocols developed by neonatology experts. If prolonged opioid therapy is required in a pregnant woman, ensure treatment is available and warn patient of risk to the neonate.
Opioids cross the placenta. Maternal use of opioids may be associated with birth defects, poor fetal growth, stillbirth, and preterm delivery. If chronic opioid exposure occurs in pregnancy, adverse events in the newborn (including withdrawal) may occur. Symptoms of neonatal abstinence syndrome (NAS) following opioid exposure may be autonomic (e.g, fever, temperature instability), gastrointestinal (e.g, diarrhea, vomiting, poor feeding/weight gain), or neurologic (e.g, high-pitched crying, hyperactivity, increased muscle tone, increased wakefulness/abnormal sleep pattern, irritability, sneezing, seizure, tremor, yawning). Mothers who are physically dependent on opioids may give birth to infants who are also physically dependent. Opioids may cause respiratory depression and psycho-physiologic effects in the neonate; newborns of mothers receiving opioids during labor should be monitored.
Agents other than hydrocodone are recommended to treat maternal pain during labor and immediately postpartum as well as chronic noncancer pain in pregnant women or those who may become pregnant.
How long does hydrocodone stay in your system?
Medications leave peoples’ bodies at different rates. In healthy, non-pregnant adults it usually takes about 24 hours for all of the hydrocodone to be gone from your body.
What should I avoid while taking hydrocodone?
Do not drink alcohol. Dangerous side effects or death can occur when alcohol is combined with hydrocodone. Check your food and medicine labels to be sure these products do not contain alcohol.
What does hydrocodone do
Hydrocodone works by primarily binding to and activating the mu-opioid receptor in the central nervous system (CNS). This leads to analgesia, euphoria, respiratory depression, miosis (constricted or pinpoint pupil), decreased gastrointestinal motility, cough suppression and physical dependence. Hydrocodone is converted to hydromorphone by the cytochrome P450 enzyme CYP2D6. Hydrocodone may potentiate the effects of other opiate agonists, general anesthetics, tranquilizers, sedatives and hypnotics, tricyclic antidepressants, monoamine oxidase inhibitors, alcohol, and other CNS depressants 1.
Hydrocodone and acetaminophen
Hydrocodone and acetaminophen combination is used to relieve moderate to moderately severe pain.
Acetaminophen is used to relieve pain and reduce fever in patients. It does not become habit-forming when taken for a long time. But acetaminophen may cause other unwanted effects when taken in large doses, including liver damage.
Hydrocodone belongs to the group of medicines called narcotic analgesics (pain medicines). It acts on the central nervous system (CNS) to relieve pain, and stops or prevents cough.
When hydrocodone is used for a long time, it may become habit-forming, causing mental or physical dependence. However, people who have continuing pain should not let the fear of dependence keep them from using narcotics to relieve their pain. Mental dependence (addiction) is not likely to occur when narcotics are used for this purpose. Physical dependence may lead to withdrawal side effects if treatment is stopped suddenly. However, severe withdrawal side effects can usually be prevented by gradually reducing the dose over a period of time before treatment is stopped completely.
This medicine is available only with your doctor’s prescription.
Hydrocodone and acetaminophen combination is available in the following dosage forms:
- Tablet
- Solution
- Syrup
- Elixir
- Capsule
- Liquid
In deciding to use hydrocodone and acetaminophen combination, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies have not been performed on the relationship of age to the effects of hydrocodone and acetaminophen capsules and tablets in the pediatric population. Safety and efficacy have not been established.
Appropriate studies performed to date have not demonstrated pediatric-specific problems that would limit the usefulness of hydrocodone and acetaminophen oral solution in children. However, safety and efficacy have not been established in children younger than 2 years of age.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of hydrocodone and acetaminophen combination in the elderly. However, elderly patients are more likely to have confusion and drowsiness, and age-related liver, kidney, or heart problems, which may require caution and an adjustment in the dose for patients receiving hydrocodone and acetaminophen combination.
Pregnancy Category C: Animal studies have shown an adverse effect and there are no adequate studies in pregnant women OR no animal studies have been conducted and there are no adequate studies in pregnant women.
Breastfeeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Naltrexone
How should hydrocodone be used?
Hydrocodone comes as an extended-release (long-acting) capsule and an extended-release (long-acting) tablet to take by mouth. The extended-release capsule is usually taken once every 12 hours. The extended-release tablet is usually taken once daily. Take hydrocodone at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take hydrocodone exactly as directed by your doctor.
Swallow the extended-release capsules or extended-release tablets one at a time with plenty of water. Swallow each capsule or tablet as soon as you put it in your mouth. Do not presoak, wet, or lick the extended-release tablets before you put them in your mouth.
Your doctor will probably start you on a low dose of hydrocodone and may gradually increase your dose, not more than once every 3 to 7 days if needed to control your pain. After your take hydrocodone for a period of time, your body may become used to the medication. If this happens, your doctor may increase your dose of hydrocodone or may prescribe a different medication to help control your pain. Talk to your doctor about how you are feeling during your treatment with hydrocodone.
Do not stop taking hydrocodone without talking to your doctor. If you suddenly stop taking hydrocodone, you may experience withdrawal symptoms such as restlessness, teary eyes, runny nose, yawning, sweating, chills, hair standing on end, muscle pain, widened pupils (black circles in the middle of the eyes), irritability, anxiety, back or joint pain, weakness, stomach cramps, difficulty falling asleep or staying asleep, nausea, loss of appetite, vomiting, diarrhea, fast breathing, or fast heartbeat. Your doctor will probably decrease your dose gradually.
Hydrocodone special precautions
Before taking hydrocodone:
- tell your doctor and pharmacist if you are allergic to hydrocodone, any other medications, or any of the ingredients in hydrocodone extended-release capsules or extended-release tablets. Ask your pharmacist or check the Medication Guide for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, and nutritional supplements you are taking or plan to take. Be sure to mention the medications listed in the IMPORTANT WARNING section and any of the following medications: antihistamines (found in cough and cold medications); amiodarone (Nexterone, Pacerone); azithromycin (Zithromax, Zmax); butorphanol; chlorpromazine; citalopram (Celexa); cyclobenzaprine (Amrix); dextromethorphan (found in many cough medications; in Nuedexta); dronedarone (Multaq); haloperidol (Haldol); laxatives such as lactulose (Cholac, Constulose, Enulose, others); levofloxacin (Levaquin); lithium (Lithobid); medications for irritable bowel disease, Parkinson’s disease, ulcers, and urinary problems; medications for migraine headaches such as almotriptan (Axert), eletriptan (Relpax), frovatriptan (Frova), naratriptan (Amerge), rizatriptan (Maxalt), sumatriptan (Imitrex, in Treximet), and zolmitriptan (Zomig); mirtazapine (Remeron); nalbuphine; pentazocine (Talwin); 5HT3 serotonin blockers such as alosetron (Lotronex), dolasetron (Anzemet), granisetron (Kytril), ondansetron (Zofran, Zuplenz), or palonosetron (Aloxi); selective serotonin-reuptake inhibitors such as citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac, Sarafem, in Symbyax), fluvoxamine (Luvox), paroxetine (Brisdelle, Prozac, Pexeva), and sertraline (Zoloft); serotonin and norepinephrine reuptake inhibitors such as desvenlafaxine (Khedezla, Pristiq), duloxetine (Cymbalta), milnacipran (Savella), and venlafaxine (Effexor); trazodone (Oleptro); or tricyclic antidepressants (‘mood elevators’) such as amitriptyline, clomipramine (Anafranil), desipramine (Norpramin), doxepin (Silenor), imipramine (Tofranil), nortriptyline (Pamelor), protriptyline (Vivactil), and trimipramine (Surmontil). Also tell your doctor or pharmacist if you are taking or receiving the following medications or have stopped taking them within the past two weeks: isocarboxazid (Marplan), linezolid (Zyvox), methylene blue, phenelzine (Nardil), rasagiline (Azilect), selegiline (Eldepryl, Emsam, Zelapar), or tranylcypromine (Parnate). Many other medications may also interact with hydrocodone, so be sure to tell your doctor about all the medications you are taking, even those that do not appear on this list. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor what herbal products you are taking, especially St. John’s wort and tryptophan.
- tell your doctor if you have any of the conditions mentioned in the IMPORTANT WARNING section, a blockage or narrowing of your stomach or intestines, or paralytic ileus (condition in which digested food does not move through the intestines). Your doctor may tell you not to take hydrocodone.
- tell your doctor if you have or have ever had low blood pressure, difficulty urinating, seizures, or thyroid, gall bladder, pancreas, liver, or kidney disease. If you are taking the extended-release tablets, also tell your doctor if you have or have ever had difficulty swallowing, colon cancer (cancer that begins in the large intestine), esophageal cancer (cancer that begins in the tube that connects the mouth and stomach), heart failure (condition in which the heart cannot pump enough blood to other parts of the body), or heart rhythm problems such long QT syndrome (condition that increases the risk of developing an irregular heartbeat that may cause fainting or sudden death).
- tell your doctor if you are breastfeeding.
- you should know that this medication may decrease fertility in men and women. Talk to your doctor about the risks of taking hydrocodone.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking hydrocodone.
- you should know that hydrocodone may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- you should know that hydrocodone may cause dizziness, lightheadedness, and fainting when you get up too quickly from a lying position. This is more common when you first start taking hydrocodone. To avoid this problem, get out of bed slowly, resting your feet on the floor for a few minutes before standing up.
- you should know that hydrocodone may cause constipation. Talk to your doctor about changing your diet and using other medications to treat or prevent constipation.
- Hydrocodone may be habit forming. Never share hydrocodone with another person, especially someone with a history of drug abuse or addiction. Keep hydrocodone in a place where others cannot get to it. Selling or giving away hydrocodone is against the law.
- Hydrocodone may impair your thinking or reactions. Avoid driving or operating machinery until you know how this medicine will affect you. Dizziness or severe drowsiness can cause falls or other accidents.
- Some medicines can interact with hydrocodone and cause a serious condition called serotonin syndrome. Be sure your doctor knows if you also take stimulant medicine, herbal products, or medicine for depression, mental illness, Parkinson’s disease, migraine headaches, serious infections, or prevention of nausea and vomiting. Ask your doctor before making any changes in how or when you take your medications.
Drug Interactions
Alcohol (Ethyl): May enhance the CNS depressant effect of HYDROcodone. Alcohol (Ethyl) may increase the serum concentration of HYDROcodone. Management: Patients using the Zohydro ER brand of extended-release hydrocodone must not consume alcohol or alcohol-containing products due to possibly fatal outcomes. Other hydrocodone products are also expected to interact, but to a less significant degree. Avoid combination
Alvimopan: Opioid Analgesics may enhance the adverse/toxic effect of Alvimopan. This is most notable for patients receiving long-term (i.e., more than 7 days) opiates prior to alvimopan initiation. Management: Alvimopan is contraindicated in patients receiving therapeutic doses of opioids for more than 7 consecutive days immediately prior to alvimopan initiation. Consider therapy modification
Amphetamines: May enhance the analgesic effect of Opioid Analgesics. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of Opioid Analgesics. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ceritinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of ceritinib with a narrow therapeutic index CYP3A substrate (eg, alfentanil, cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, tacrolimus) should be avoided when possible. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP2D6 Inhibitors (Strong): May decrease serum concentrations of the active metabolite(s) of HYDROcodone. Specifically, concentrations of hydromorphone may be decreased. Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of HYDROcodone. Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of HYDROcodone. Monitor therapy
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of HYDROcodone. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of HYDROcodone. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Desmopressin: Opioid Analgesics may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Diuretics: Opioid Analgesics may enhance the adverse/toxic effect of Diuretics. Opioid Analgesics may diminish the therapeutic effect of Diuretics. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (e.g., opioids, barbiturates) with concomitant use. Consider therapy modification
Eluxadoline: Opioid Analgesics may enhance the constipating effect of Eluxadoline. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gastrointestinal Agents (Prokinetic): Opioid Analgesics may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Minocycline: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the adverse/toxic effect of HYDROcodone. Management: Consider alternatives to this combination when possible. Consider therapy modification
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nalmefene: May diminish the therapeutic effect of Opioid Analgesics. Management: Avoid the concomitant use of nalmefene and opioid analgesics. Discontinue nalmefene 1 week prior to any anticipated use of opioid analgesics. If combined, larger doses of opioid analgesics will likely be required. Consider therapy modification
Naltrexone: May diminish the therapeutic effect of Opioid Analgesics. Management: Seek therapeutic alternatives to opioids. See full drug interaction monograph for detailed recommendations. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Ombitasvir, Paritaprevir, and Ritonavir: May increase the serum concentration of HYDROcodone. Management: Reduce the hydrocodone dose by 50% during concurrent use of ombitasvir, paritaprevir, and ritonavir; monitor closely for both analgesic effectiveness and for signs of toxicity or withdrawal. Consider therapy modification
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: May increase the serum concentration of HYDROcodone. Management: Reduce the hydrocodone dose by 50% during concurrent use of ombitasvir, paritaprevir, ritonavir, and dasabuvir; monitor closely for both analgesic effectiveness and for signs of toxicity or withdrawal. Consider therapy modification
Opioids (Mixed Agonist / Antagonist): May diminish the analgesic effect of Opioid Analgesics. Management: Seek alternatives to mixed agonist/antagonist opioids in patients receiving pure opioid agonists, and monitor for symptoms of therapeutic failure/high dose requirements (or withdrawal in opioid-dependent patients) if patients receive these combinations. Avoid combination
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pegvisomant: Opioid Analgesics may diminish the therapeutic effect of Pegvisomant. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pitolisant: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Combined use of pitolisant with a CYP3A4 substrate that has a narrow therapeutic index should be avoided. Other CYP3A4 substrates should be monitored more closely when used with pitolisant. Consider therapy modification
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Ramosetron: Opioid Analgesics may enhance the constipating effect of Ramosetron. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonin Modulators: Opioid Analgesics may enhance the serotonergic effect of Serotonin Modulators. This could result in serotonin syndrome. Exceptions: Nicergoline. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
St John’s Wort: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Succinylcholine: May enhance the bradycardic effect of Opioid Analgesics. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification.
Pregnancy and breastfeeding
Prolonged use during pregnancy can result in neonatal opioid withdrawal syndrome called neonatal abstinence syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.
I am taking hydrocodone, but I would like to stop taking it before becoming pregnant. How long does the drug stay in my body?
Talk with your healthcare provider before making any changes to your medications. Medications leave peoples’ bodies at different rates. In healthy, non-pregnant adults it usually takes about 24 hours for all of the hydrocodone to be gone from the body.
I take hydrocodone. Can it make it harder for me to get pregnant?
Hydrocodone has not been studied in women to see if using it could make it harder to get pregnant.
Should I stop taking my hydrocodone prescription if I find out that I am pregnant?
No. If you have been taking hydrocodone regularly (daily or almost daily) you should not stop suddenly (also called “cold turkey”). Stopping an opioid medication suddenly could cause you to go into withdrawal. More research is needed to know if going through withdrawal might hurt a pregnancy. Talk with your healthcare provider about the risks and benefits of continuing or stopping your medication. Any reduction in your hydrocodone needs to be done slowly, and under the direction of your healthcare provider.
Can taking hydrocodone in pregnancy increase the chance of miscarriage?
There are no published studies looking at whether hydrocodone increases the chance of miscarriage. This does not mean that there is an increased chance or no increased chance. It only means that this question has not been answered.
Can taking hydrocodone increase the chance of having a baby with a birth defect?
This is not yet known. Two studies reported that taking hydrocodone in the first trimester increased the chance of heart defects, and one of the studies reported a small increased chance of spina bifida (an opening in the spine and spinal cord) and gastroschisis (an opening in the wall of the abdomen). However, the number of women exposed to hydrocodone in these studies was small, so it is difficult to make an association between the medication and the birth defects. It is possible that other factors, such as other drugs the mothers took, or a combination of drugs, could have been responsible for the birth defects. In addition, two other studies on hydrocodone did not found an increased chance of birth defects.
Could hydrocodone cause other pregnancy complications?
Possibly. One study found that women who used hydrocodone and other opioids in pregnancy were more likely to have babies that were born smaller than expected. However, the women in this study who used opioids were also more likely to smoke during pregnancy, which can also cause babies to be born small. Other studies of women who used opioids throughout pregnancy also found an increased chance for smaller babies, as well as other adverse outcomes including stillbirth, premature delivery, and fetal distress during labor. This is more commonly reported in women who are using heroin or misusing hydrocodone (taking prescribed opioid pain medications in greater amounts or for longer than recommended by their health providers).
Will my baby have withdrawal (neonatal abstinence syndrome) if I continue to take hydrocodone?
Possibly. Neonatal abstinence syndrome is the term used to describe withdrawal symptoms in newborns from medications that a mother takes during pregnancy. Studies of pregnant women using prescribed hydrocodone and other opioid pain medications have reported an increased chance for neonatal abstinence syndrome. The chance of neonatal abstinence syndrome may be higher if these medications are used late in pregnancy.
For any opioid, symptoms can include difficulty breathing, extreme drowsiness (sleepiness), poor feeding, irritability, sweating, tremors, vomiting and diarrhea. Symptoms of neonatal abstinence syndrome may appear at birth and may last more than two weeks. If needed, babies can be treated for withdrawal while in the hospital. If you use an opioid in your pregnancy, it is important that your baby’s doctors know and check for symptoms of neonatal abstinence syndrome, so your newborn gets the best possible care.
Will taking hydrocodone during pregnancy affect my baby’s behavior or cause learning problems?
This is unknown. There are not enough studies on hydrocodone to know if there is a chance for long-term problems.
What do we know about misuse or abuse of opioid medications?
Studies find that pregnant women who take opioids in higher doses or for longer than recommended by their health care providers (i.e. misuse or “abuse” opioids) have an increased risk for pregnancy problems. These include poor growth of the baby, stillbirth, premature delivery, and c-section. Some women who misuse opioids also have other habits that can result in health problems for both the mother and the baby. For example, poor diet choices can lead to mothers not having enough nutrients to support a healthy pregnancy and could increase the chance of miscarriage and premature birth. Sharing needles to inject opioids increases the risk of getting diseases like hepatitis C and/or HIV, which can cross the placenta and infect the baby.
Can I take hydrocodone while I am breastfeeding?
Possibly. Small amounts of hydrocodone get into breast milk. Babies might have problems with even the small amounts of hydrocodone that could be in the breast milk. Speak to your healthcare provider about the best ways to manage your pain while you are breastfeeding.
Use of some opioids such as hydrocodone in breastfeeding may cause the baby to be very sleepy, have trouble latching on and have breathing difficulties. If you are using any opioid, your baby should be watched carefully. Contact your baby’s healthcare provider right away and stop breastfeeding if your baby has any of these problems while you are taking this medication.
What is hydrocodone used for
Hydrocodone is indicated for the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate.
Hydrocodone dosage
Hydrocodone is available in the following dosage forms:
- Capsule, Extended Release
- Tablet, Extended Release
- Liquid
- Syrup
- Tablet
Dose Adjustments
Abrupt discontinuation should be avoided in the physically dependent patient:
- Extended-release capsules: Titrate the dose down every 2 to 4 days; a more gradual titration may be needed in patients showing signs and symptoms of opioid withdrawal
- Extended-release tablets: Titrate the dose down every 2 to 4 days; the titrated dose should be at least 50% of the prior dose; after reaching 20 mg once a day for 2 to 4 days, the extended-release tablets can be discontinued.
Concomitant Use with CNS depressants: Lower the recommended starting dose by 20% to 30% and consider a lower dose of the concomitant CNS depressant.
CYP450 3A4 Inducers and Inhibitors: Dose adjustments may be necessary; closely monitor patients currently taking, or discontinuing CYP450 3A4 inducers and inhibitors
Increased Risk of Respiratory Depression: Consider lower initial doses, slower titrations, or alternative analgesics.
QTc Interval Prolongation: Reduce dose by 33% to 50%; consider alternative analgesics
Adult Dose for Chronic Pain
- The following dosing recommendations can only be considered suggested approaches to what is actually a series of clinical decisions over time; each patient should be managed individually.
- Use: For the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate.
As First Opioid Analgesic and For Patients who are NOT Opioid Tolerant:
- Extended-Release Capsules (Zohydro(R) ER): Initial dose: 10 mg orally every 12 hours
- Extended-Release Tablets (Hysingla(R) ER): Initial dose: 20 mg orally every 24 hours
Comments:
- Use of higher starting doses in patients who are not opioid tolerant may cause fatal respiratory depression; monitor patients closely for respiratory depression, especially during the first 24 to 72 hours.
- An opioid tolerant patient is one who has been receiving for 1-week or longer at least: oral morphine 60 mg/day, fentanyl transdermal patch 25 mcg per hour, oral oxycodone 30 mg/day, oral hydromorphone 8 mg/day, oral oxymorphone 25 mg/day, or an equianalgesic dose of another opioid.
TITRATION AND MAINTENANCE:
Individually titrate to a dose that provides adequate analgesia and minimizes adverse reactions.
- Dose adjustments to hydrocodone extended-release capsules should be made in 10 mg increments every 12 hours, every 3 to 7 days.
- Dose adjustments to hydrocodone extended-release tablets should be made in 10 to 20 mg increments every 24 hours, every 3 to 5 days.
- If unacceptable side effects occur, the dose may be reduced.
- Breakthrough Pain: If the level of pain increases after dose stabilization, attempt to identify the source before increasing dose; rescue medication with appropriate immediate-release analgesia may be helpful
DOSE CONVERSIONS
Dose conversions should be done carefully and with close monitoring due to large patient variability in regards to opioid analgesic response. Discontinue all other around the clock opioid drugs when initiating therapy with extended-release hydrocodone.
Hydrocodone Extended-Release (ER) CAPSULES:
- The 50 mg capsules, a single dose greater than 40 mg, or a total daily dose greater than 80 mg are reserved for opioid tolerant individuals.
CONVERSION FROM OTHER ORAL OPIOIDS:
- Published potency tables can be used to estimate a patient’s 24-hour oral hydrocodone requirement; however, due to substantial inter-patient variability, it is best to underestimate a patient’s 24-hour requirement and provide rescue medication as the dose is titrated.
- Alternatively, the following conversion factors (CF) may be used to convert selected oral opioids to the hydrocodone extended-release capsule: Hydrocodone, CF=1; Oxycodone, CF=1; Methadone, CF= 1, Oxymorphone, CF=2; Hydromorphone, CF=2.67; Morphine, CF=0.67; Codeine, CF=0.1.
- These conversion factors cannot be used to convert from hydrocodone extended-release to the selected oral opioid as doing so will result in overestimation of the oral opioid dose and may result in fatal respiratory depression.
- Example: Sum the total daily dose of prior oral opioid; multiply that sum by the CF to obtain 24-hour oral hydrocodone requirement; divide 24-hour requirement by 2 (round down, if necessary ) and give 1 dose orally every 12 hours.
- These conversion factors cannot be used to convert from hydrocodone extended-release to the selected oral opioid as doing so will result in overestimation of the oral opioid dose and may result in fatal respiratory depression.
CONVERSION FROM TRANSDERMAL FENTANYL
Remove the transdermal fentanyl patch and 18 hours later initiate hydrocodone extended-release capsules at 10 mg every 12 hours for each 25 mcg/hr fentanyl transdermal patch; monitor closely as there is limited documented experience with this conversion.
Hydrocodone Extended-Release (ER) TABLETS:
- Daily dose greater than or equal to 80 mg are reserved for use in opioid tolerant individuals.
CONVERSION FROM ORAL HYDROCODONE FORMULATIONS
- Administer patient’s total daily oral hydrocodone dose as extended-release tablet orally once a day.
CONVERSION FROM OTHER ORAL OPIOIDS
- Published potency tables can be used to estimate a patient’s 24-hour oral hydrocodone requirement; however, due to substantial inter-patient variability, it is best to underestimate a patient’s 24-hour requirement and provide rescue medication as the dose is titrated.
- To obtain the initial hydrocodone extended-release tablet dose, use the following conversion factors (CF) to convert selected oral opioids and then reduce that dose by 25%. Tramadol, CF=0.1; Oxycodone, CF=1; Methadone, CF= 1.5, Oxymorphone, CF=2; Hydromorphone, CF=4; Morphine, CF=0.5; Codeine, CF=0.15.
- These conversion factors cannot be used to convert from hydrocodone extended-release to the selected oral opioid as doing so will result in overestimation of the oral opioid dose and may result in fatal respiratory depression.
- Example: Sum the total daily dose of prior oral opioid; multiply that sum by the CF to obtain 24-hour oral hydrocodone requirement; reduce that hydrocodone requirement by 25% to account for interpatient variability, round down, if necessary; administer calculated dose orally once a day.
- These conversion factors cannot be used to convert from hydrocodone extended-release to the selected oral opioid as doing so will result in overestimation of the oral opioid dose and may result in fatal respiratory depression.
CONVERSION FROM TRANSDERMAL FENTANYL
Remove the transdermal fentanyl patch and 18 hours later initiate hydrocodone extended-release tablets at 20 mg every 24 hours for each 25 mcg/hr fentanyl transdermal patch; monitor closely as there is limited documented experience with this conversion.
CONVERSION FROM TRANSDERMAL BUPRENORPHINE
Patients receiving transdermal buprenorphine 20 mcg/hr or less should initiate extended-release hydrocodone tablets at 20 mg every 24 hours; monitor closely as there is limited documented experience with this conversion.
Comments:
- When converting from methadone, close monitoring is of particular importance due to methadone’s long half-life.
Renal Dose Adjustments
- Extended-release capsules: Initial dose should be lowered; monitor closely for respiratory depression and sedation
- Extended-release tablets: Lower the initial dose to one-half the normal starting dose; monitor closely for respiratory depression and sedation
Liver Dose Adjustments
Extended-release capsules:
- Mild to moderate hepatic impairment: No dose adjustment recommended
- Severe hepatic impairment: 10 mg orally every 12 hours; monitor closely for respiratory depression and sedation
Extended-release tablets:
- Lower the initial dose to one-half the normal starting dose; monitor closely for respiratory depression and sedation
What should I do if I forget a dose?
Skip the missed dose and continue your regular dosing schedule. Do not take more than one dose of hydrocodone extended-release capsules in 12 hours or extended-release tablets in 24 hours.
Hydrocodone side effects
When you take the correct or prescribed dose of hydrocodone, side effects may occur. In addition to relieving pain, you may be drowsy, confused and in a daze, constipated, and possibly nauseated.
The most commonly reported side effects included constipation, nausea, vomiting, fatigue, upper respiratory tract infection, dizziness, headache, and somnolence.
Hydrocodone may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- stomach pain
- dry mouth
- tiredness
- headache
- back pain
- muscle tightening
- difficult, frequent, or painful urination
- ringing in the ears
- difficulty falling asleep or staying asleep
- foot, leg, or ankle swelling
- uncontrollable shaking of a part of the body
Some side effects can be serious. If you experience any of these symptoms or those listed in the IMPORTANT WARNING or SPECIAL PRECAUTIONS sections, call your doctor immediately or get emergency medical treatment:
- chest pain
- agitation, hallucinations (seeing things or hearing voices that do not exist), fever, sweating, confusion, fast heartbeat, shivering, severe muscle stiffness or twitching, loss of coordination, nausea, vomiting, or diarrhea
- nausea, vomiting, loss of appetite, weakness, or dizziness
- inability to get or keep an erection
- irregular menstruation
- decreased sexual desire
- swelling of your eyes, face, lips, tongue, or throat
- hoarseness
- changes in heartbeat
- hives
- itching
- difficulty swallowing or breathing
Respiratory
- Common (1% to 10%): Upper respiratory tract infection, cough, bronchitis, nasopharyngitis, sinusitis, nasal congestion
- Uncommon (0.1% to 1%): Dyspnea
Cardiovascular
- Common (1 to 10%): Hot flush, hypertension, chest pain, peripheral edema
- Rare (less than 0.1%): Hypotension, orthostatic hypotension, palpitations, presyncope, syncope
- Frequency not reported: QTC interval prolongation
- QT interval prolongation has been observed in healthy subjects following daily dosing with hydrocodone extended-release tablets. The difference in QT interval at steady state was found to be 6 milliseconds, 7 milliseconds, and 10 milliseconds at doses of 80 mg, 120 mg and 160 mg, daily, respectively.
Gastrointestinal
- Very common (10% or more): Constipation (up to 11%), nausea (up to 10%)
- Common (1% to 10%): Dry mouth, vomiting, abdominal pain or discomfort, gastroesophageal reflux disease, diarrhea, dyspepsia
- Rare (less than 0.1%): Dysphagia, esophageal obstruction, retching, chocking
- Very rare (less than 0.01%): Difficulty swallowing tablet
- In clinical trials with extended release tablets, 11 or 2476 subjects reported difficulty swallowing the tablets. These reports included esophageal obstruction, dysphagia, and choking. One case required medical intervention to remove the tablet.
Nervous system
- Common (1% to 10%): Somnolence, fatigue, headache, tremor, dizziness, lethargy, migraine, paresthesia, sedation
- Uncommon (0.1% to 1%): Abnormal thinking
Other
- Common (1% to 10%): Pain, pyrexia, fatigue, tinnitus, chills
- Uncommon (0.1% to 1%): Asthenia, neonatal abstinence syndrome, drug withdrawal
Psychiatric
- Common (1 to 10%): Anxiety, depression, insomnia
- Uncommon (0.1% to 1%): Agitation, altered mood, irritability, libido decreased
Metabolic
- Common (1% to 10%): Dehydration, hypokalemia, increased blood cholesterol, decreased appetite
- Uncommon (0.1% to 1%): Thirst
Hepatic
- Common (1 to 10%): Increased gamma-glutamyltransferase
Musculoskeletal
- Common (1% to 10%): Back pain, muscle spasms , contusion, fall, foot fracture, joint injury or sprain, muscle strain, arthralgia, musculoskeletal pain, myalgia, neck pain, osteoarthritis, pain in extremity
- Uncommon (0.1% to 1%): Muscle twitching
Hypersensitivity
- Uncommon (0.1% to 1%): Drug hypersensitivity
Endocrine
- Uncommon (0.1% to 1%): Hypogonadism
Dermatologic
- Common (1% to 10%): Pruritus, skin laceration, hyperhidrosis, night sweats, rash
Genitourinary
- Common (1% to 10%): Urinary tract infection
- Uncommon (0.1% to 1%): Urinary retention
When you take too much hydrocodone, symptoms become much more serious. Symptoms of hydrocodone overdose may develop in many body systems:
Eyes, ears, nose, and throat:
- Pinpoint pupils
Gastrointestinal system:
- Constipation
- Nausea
- Spasms (pain) of the stomach or intestinal tract
- Vomiting
Heart and blood vessels:
- Low blood pressure
- Weak pulse
Nervous system:
- Coma (unresponsiveness)
- Drowsiness
- Possible seizures
Respiratory system:
- Difficulty breathing
- Slow breathing that requires more effort
- Shallow breathing
- No breathing
Skin:
- Bluish-colored fingernails and lips
Other symptoms:
- Muscle damage from being immobile while unresponsive
Hydrocodone may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
Hydrocodone withdrawal
Hysingla ER, Vantrela ER: For patients on long term opioid therapy, decrease dose by 25% to 50% every 2 to 4 days; monitor carefully for signs/symptoms of withdrawal. If patient displays withdrawal symptoms, increase dose to previous level and then reduce dose more slowly by increasing interval between dose reductions, decreasing amount of daily dose reduction, or both.
Zohydro ER: For patients on long term opioid therapy, gradually titrate the dose downward every 2 to 4 days to prevent signs and symptoms of withdrawal. If patient displays withdrawal symptoms, increase dose to previous level and then reduce dose more slowly by increasing interval between dose reductions, decreasing amount of daily dose reduction, or both.
Hydrocodone overdose
In case of overdose, call the poison control helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help. If the victim has collapsed, had a seizure, has trouble breathing, or can’t be awakened, immediately call your local emergency services number.
While you are taking hydrocodone, you may be told to always have a rescue medication called naloxone available (e.g., home, office). Naloxone is used to reverse the life-threatening effects of an overdose. It works by blocking the effects of opiates to relieve dangerous symptoms caused by high levels of opiates in the blood. You will probably be unable to treat yourself if you experience an opiate overdose. You should make sure that your family members, caregivers, or the people who spend time with you know how to tell if you are experiencing an overdose, how to use naloxone, and what to do until emergency medical help arrives. Your doctor or pharmacist will show you and your family members how to use the medication. Ask your pharmacist for the instructions or visit the manufacturer’s website to get the instructions. If someone sees that you are experiencing symptoms of an overdose, he or she should give you your first dose of naloxone, call 911 immediately, and stay with you and watch you closely until emergency medical help arrives. Your symptoms may return within a few minutes after you receive naloxone. If your symptoms return, the person should give you another dose of naloxone. Additional doses may be given every 2 to 3 minutes, if symptoms return before medical help arrives.
Serious overdose with hydrocodone is characterized by respiratory depression (a decrease in respiratory rate and/or tidal volume, Cheyne-Stokes respiration, cyanosis), extreme somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, and sometimes bradycardia and hypotension. In severe overdosage, apnea, circulatory collapse, cardiac arrest and death may occur. In severe overdose, apnea, circulatory collapse, cardiac arrest and death may occur. LD50 in rats = 375 mg/kg when given orally and 150 mg/kg for subcutaneous administration (lethal dose 50 is the dose where 50 percent of the test subject die) (subcutaneous, in mice).
Symptoms of overdose may include the following:
- slowed breathing
- sleepiness
- muscle weakness
- cold, clammy skin
- narrowed or widened pupils
- slowed heartbeat
- coma
- death
What to expect at the Emergency Room
Take the container with you to the hospital, if possible.
The health care provider will measure and monitor the person’s vital signs, including temperature, pulse, breathing rate, and blood pressure. Symptoms will be treated as appropriate. The health care team will closely monitor the person’s breathing. The person may receive:
- Activated charcoal
- Airway support, including oxygen, breathing tube through the mouth (intubation), and breathing machine (ventilator)
- Blood and urine tests
- Chest x-ray
- CT (computed tomography, or advanced imaging) scan
- EKG (electrocardiogram, or heart tracing)
- Fluids through a vein (intravenous or IV)
- Laxative
- Medicines to treat symptoms, including naloxone, an antidote to reverse the effect of the poison, many doses may be needed
Naloxone is a specific opioid antagonist with no agonist properties of its own; large doses may be given safely. The duration of effect of naloxone (1-2 hours) is shorter than that of many opioids. Therefore, do not release a patient who has awakened after naloxone treatment until at least 3-4 hours has passed since the last dose of naloxone. In general, if naloxone was required to reverse opioid-induced coma, it is safer to admit the patient for at least 6-12 hours of observation. 2. Nalmefene is an opioid antagonist with a longer duration of effect (3-5 hours).
Additional therapies may be needed if the person took hydrocodone with other drugs, such as Tylenol or aspirin.
Hydrocodone prognosis
A large overdose can cause a person to stop breathing and die if not treated right away. The person may need to be admitted to the hospital to continue treatment. Depending on the drug or drugs taken, multiple organs may be affected. This may affect the person’s outcome and chances of survival.
If you receive medical attention before serious problems with your breathing occur, you should have few long-term consequences. You will probably be back to normal in a day.
However, this overdose can be deadly or can result in permanent brain damage if treatment is delayed and a large amount of hydrocodone is taken.