Hypoplastic right heart syndrome
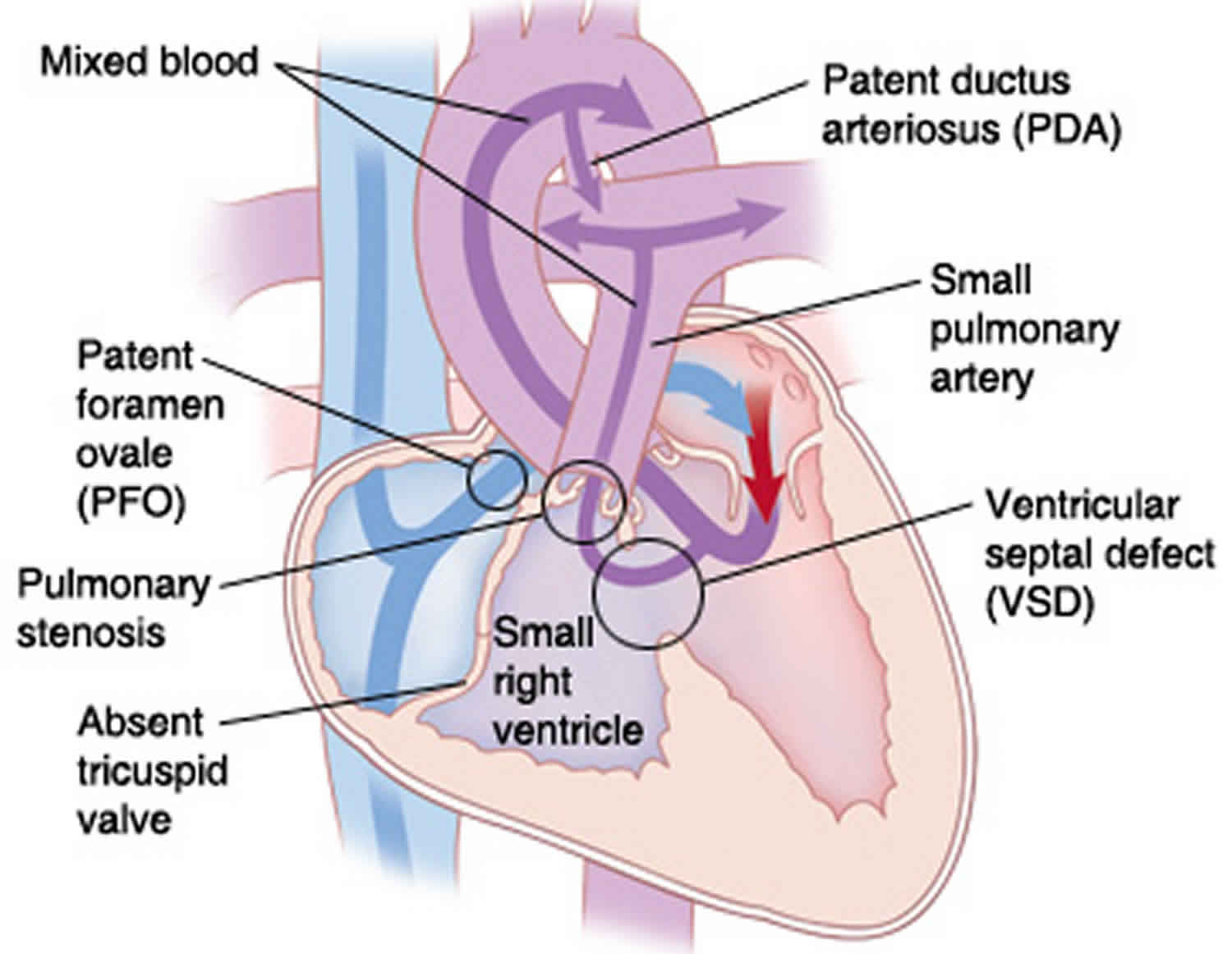
Hypoplastic right heart syndrome is a rare cyanotic congenital (present at birth) heart disease with under-development of the right ventricle, tricuspid valve, pulmonary valve and pulmonary artery leading to right-to-left shunting of the blood through inter-atrial septal defect 1. The underdeveloped right side of the heart is unable to provide enough blood flow to the body, leading to low blood oxygen and cyanosis 2. Hypoplastic right heart syndrome differs from hypoplastic left heart syndrome which involves the underdevelopment of the structures on the left side of the heart.
The main issue involving hypoplastic right heart syndrome is pulmonary valve atresia where the child is born without the pulmonary valve that is essential in the opening and closing the heart chamber to allow the flow of blood to enter the pulmonary artery. However, there also secondary issues associated with hypoplastic right heart syndrome that include:
- Hypoplastic (small) Right Ventricle – Normally developed lower chamber of the heart pumps blood to the lungs
- Hypoplastic (small) Tricuspid Valve – The small bowel restricts the flow of blood into the right ventricle
- Hypoplastic (small) Pulmonary Artery
- The flow of blood from the heart to the coronary arteries can be restricted and cause considerable damage to the heart muscle
Without treatment, the condition can be fatal.
Normally, the right ventricle pushes blood out of the heart and to the lungs where it can pick up oxygen. The blood with oxygen then moves to the left side of the heart which pumps the blood to the rest of the body.
Hypoplastic right heart syndrome makes it difficult or impossible to pass blood to the lungs. This decreases the amount of oxygen for the rest of the body. The underdeveloped muscle of the right ventricle can also be easily exhausted by normal heart functions.
Hypoplastic right ventricle syndrome may be present in around 1.1% of stillbirths and is rarer than the hypoplastic left heart syndrome.
The treatments for hypoplastic right ventricle syndrome have developed substantially in the last few decades and are tailored to each baby’s needs.
Who is at risk for hypoplastic right heart syndrome?
Mothers who previously birthed the child with hypoplastic right heart syndrome are at greater risk of birthing another baby with a similar condition. Doctors have yet to determine the exact cause of the condition but it is likely the result of environmental factors and genetics.
Hypoplastic right heart syndrome causes
The causes of heart defects such as hypoplastic right ventricle syndrome are unknown. It may be a combination of genetic and environmental factors, such as things the mother comes in contact with in the environment or what the mother eats or drinks or the medicines the mother uses.
Hypoplastic right heart syndrome is caused by decreased blood flow in and out of the right ventricle during fetal heart development. The most common right-sided defect to cause hypoplastic right ventricle syndrome is pulmonary atresia with an intact ventricular septum. Coronary arterial supply may be also abnormal. It is unclear why the heart does not develop as expected.
A family history of similar heart defects is a potential risk factor.
Hypoplastic right heart syndrome symptoms
Some congenital heart defects in the range of hypoplastic right ventricle syndrome are:
- Tricuspid stenosis: The tricuspid valve between the right atrium and right ventricle is too small
- Tricuspid atresia: The tricuspid valve between the right atrium and right ventricle is not formed
- Pulmonary stenosis: The pulmonary valve between the right ventricle and pulmonary artery is too small
- Pulmonary atresia: The pulmonary valve between the right ventricle and pulmonary artery is not formed
Babies are cyanotic at birth. A child most often has severe symptoms shortly after birth. The most common symptoms associated with hypoplastic right heart syndrome can include:
- Skin, lips, and nails look blue (cyanosis)
- Trouble breathing or rapid breathing
- Poor feeding
- Poor weight gain and growth
- Tiredness
- Child becomes gray and cold, and the heart may stop beating (circulatory collapse).
Certain structures of the heart and related blood vessels are present before birth. These structures decrease blood flow to the lungs. After birth, the baby will need to supply its own oxygen through the lungs. These structures gradually close over the first few weeks of life to increase the flow of blood to the lungs. Structures include:
- Ductus arteriosus—a connection between the pulmonary artery and the aorta (a large blood vessel that carries blood with oxygen away from the heart to the body)
- Foramen ovale—opening between the right and left side of the heart
These structures can decrease the efficiency of a normal heart. However, these structures actually help compensate for shortcomings created by hypoplastic right heart syndrome. Symptoms of hypoplastic right heart syndrome may worsen over the first few weeks of life as these structures close.
Hypoplastic right heart syndrome diagnosis
Hypoplastic right heart syndrome may be diagnosed during pregnancy or soon after the baby is born.
During pregnancy
During pregnancy, there are screening tests also called prenatal tests, to check for birth defects and other conditions. Hypoplastic right heart syndrome may be diagnosed during pregnancy with an ultrasound, which creates pictures of the body. Prenatal ultrasound may show a small right ventricle with hypertrophy and a small or absent pulmonary artery, with decreased or absent flow through the tricuspid valve and pulmonary valve 3. Some findings from the ultrasound may make your doctor suspect a baby may have hypoplastic right heart syndrome. If so, the health care provider can request a fetal echocardiogram, an ultrasound of the baby’s heart, to confirm the diagnosis. This test can show problems with the structure of the heart and how the heart is working with this defect.
Figure 1. Hypoplastic right heart syndrome ultrasound
Footnote: Four-chamber view shows small right ventricle (RV), with normal sized left ventricle (LV), consistent with hypoplastic right heart syndrome. LA = left atrium, RA = right atrium.
[Source 4 ]Figure 2. Tricuspid stenosis
Footnote: Four-chamber view show thickened leaflets of tricuspid valve (arrows), with restricted opening, consistent with tricuspid stenosis.
[Source 4 ]After the baby is born
Babies with hypoplastic right heart syndrome are cyanotic at birth.
During a physical examination, a doctor can see these signs or might hear a heart murmur (an abnormal whooshing sound caused by blood not flowing properly). If a murmur is heard or other signs are present, the health care provider might request one or more tests to make a diagnosis, the most common being an echocardiogram. Echocardiography also is useful for helping the health care provider follow the child’s health over time.
Hypoplastic right heart syndrome is a defect that also can be detected with newborn pulse oximetry screening. Pulse oximetry is a simple bedside test to determine the amount of oxygen in a baby’s blood. Low levels of oxygen in the blood can be a sign of a critical congenital heart defect. Newborn screening using pulse oximetry can identify some infants with a critical congenital heart defect, like hypoplastic right heart syndrome, before they show any symptoms.
Hypoplastic right heart syndrome treatment
Babies with hypoplastic right heart syndrome will need treatment shortly after birth. If hypoplastic right heart syndrome was detected before birth, a team of specialists will help monitor and treat the baby immediately after birth. Most babies with hypoplastic right heart syndrome can be delivered vaginally at full-term, unless there are obstetric indications for another mode of delivery. It is best for these babies to be delivered at a medical center where there is access to a team of pediatric cardiologists and neonatologists, along with an established neonatal intensive care unit (NICU).
After delivery, your baby will need prostaglandin, an intravenous medication that keeps the ductus arteriosus (a normal connection present in babies in the womb) open. The patent ductus arteriosus will allow blood to get to the lungs. In some cases, a cardiac catheterization may be required to perform a balloon atrial septostomy in the first few days of life. This x-ray guided procedure is typically done by placing a thin flexible tube, or catheter, through the umbilical vein (a vessel in the umbilical cord) and does not require an incision. A balloon atrial septostomy creates a larger hole between the top chambers of the heart.
The treatment for hypoplastic right ventricle syndrome vary depending on which structures are abnormal. In cases where the pulmonary valve is not opening well, cardiac catheterization may be performed to help open the valve. In less severe cases this may allow the right heart to function adequately.
In more severe cases, the right heart is too small to send enough blood to the lungs. Shortly after the baby’s birth, surgeons perform the first of a series of surgeries done to increase blood flow to the lungs and bypass the poorly functioning right side of the heart. These surgeries are not able to cure hypoplastic right ventricle syndrome, but provide for a functioning heart.
- Blalock-Taussig Shunt: This procedure usually occurs within the first few days of life. In this surgery, the surgeon inserts an artificial tube called a shunt is attached from the pulmonary artery to the aorta (major blood vessel that carries blood from the left side of the heart to the body). Some blood can then move from the aorta to the pulmonary artery which carries the blood to the lungs. This increases the amount of blood that passes the lungs. The oxygen available for the body will increase as a result. Blalock-Taussig Shunt is a temporary measure to improve oxygen supply to the body and relieve symptoms such as blue tint to skin. There is still mixing of oxygen poor and oxygen rich blood through the hole between the top chambers of the heart.
- Glenn Procedure: As the child ages, Blalock-Taussig shunt will not be able to provide enough blood flow to the lungs. The Glenn procedure typically occurs between 4 and 6 months of age. This surgery creates a direct connection between the pulmonary artery and the superior vena cava (vessel returning oxygen-poor blood from the upper part of the body to the heart). This reduces the amount of blood flow returning to the small right side of the heart by allowing blood returning from the upper body to flow directly to the lungs.
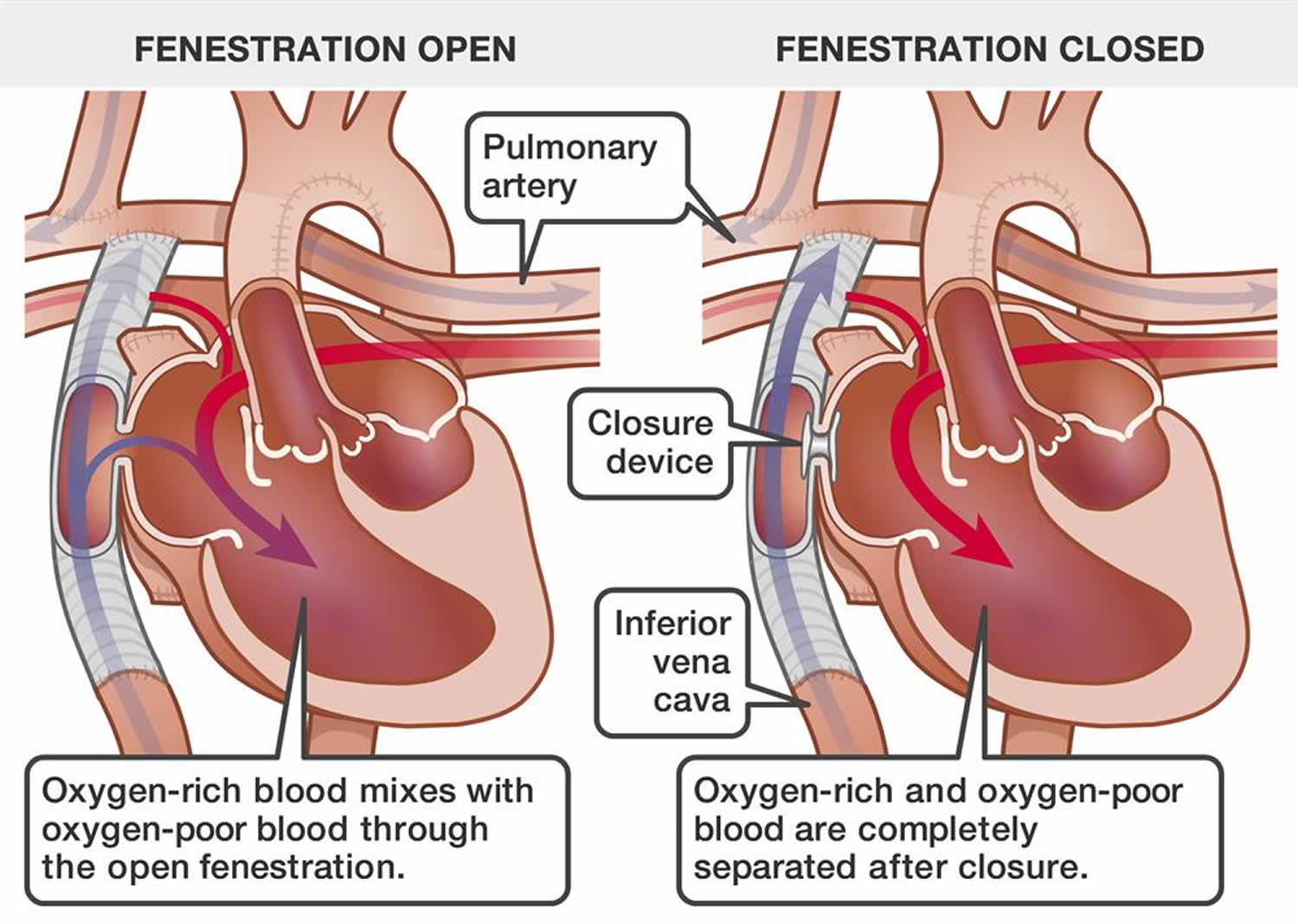
- Fontan Procedure or Fontan completion: The Fontan procedure typically occurs between 2 and 4 years of age. This surgery connects the pulmonary artery and the inferior vena cava (vessel returning oxygen-poor blood from the lower part of the body to the heart), allowing the blood coming back from the lower body to go to the lungs. Once the Fontan procedure is complete, oxygen-rich and oxygen-poor blood no longer mix in the heart. The surgeon may leave a small connection between the oxygen rich and oxygen poor chambers (a fenestration).
Heart transplant
The Blalock-Taussig shunt and Glenn and Fontan procedures will help improve the amount of oxygen in the blood and reduce symptoms. However, surgery cannot repair the damaged right ventricle. Eventually, the left side of the heart will have difficulty keeping up with the extra workload. The heart will eventually need to be replaced with a heart transplant.
A heart transplant may be done early in childhood instead of the Glenn and Fontan procedures or late in adulthood when the heart is no longer able to properly function.
Figure 3. Fontan procedure hypoplastic right heart
Hypoplastic right heart syndrome prognosis
The long-term prognosis of hypoplastic right ventricle syndrome varies depending on the severity of the initial defect. Children with hypoplastic right ventricle syndrome whose hearts become weak may eventually need heart transplants.
Hypoplastic right heart syndrome is a challenging heart problem to treat. After surgery, your child may have ongoing heart problems. They may need medicines to manage symptoms and improve heart function. Your child may also need more surgery. Your child needs follow-up visits with the cardiologist for the rest of their life.
In many cases, children with tricuspid atresia can be active. How active will vary with each child. Ask the cardiologist what activities your child can do safely.
Your child may need to take antibiotics before having any surgery or dental work. This is to prevent infection of the heart or valves. This is called infective endocarditis. The cardiologist will give you instructions for this.
Hypoplastic right heart syndrome life expectancy
The post-repair survival rate of a child who has undergone a Fontan procedure increases life longevity between 15 and 30 years. However, this outcome in no way meets the child will not succumb to the condition, but only that the child’s deteriorating heart function often means they will be listed for heart transplant.
In many cases, the parents will immediately opt in for a heart transplant after the child has been born instead of following normal treatment involving a Fontan procedure. Alternatively, some parents believe that medical advancements involving heart transplantation has yet to reach the level of surety of the child’s longevity and instead will choose the Fontan procedure to buy time.
That said, the child’s outlook for living a healthy life after being born with hypoplastic right heart syndrome has never been better. The condition was once considered to produce fatal certainty. However, in recent years, many children are now surviving the three stages of repair and go on to live active lives.
Special considerations
There are certain aspects of suffering from the congenital heart disease that requires specific care tips to avoid a heart infection that can easily develop without an apparent reason. Parents should consider following specific care tips of their child that include:
- Dental care – Any individual suffering from any form of heart disease has an increased potential risk of developing a heart infection. This is especially true when undergoing dental care where germs in the mouth can easily spread into the body’s bloodstream and eventually cause an infection in the heart.
- Exercise – Children of undergone a shunt operation are usually limited to light exercise.
- Vaccination scheduling – Children who have had a heart transplantation usually follow a variable vaccination schedule that is much different than children who have not had a heart transplant.
Before the doctor prescribes any medications, they should be fully aware of the child’s congenital heart defect and any repairs that have been made to minimize the potential for serious side effects or unusual symptoms caused by taking much-needed drugs.
References- Van der Hauwaert LG, Michaelsson M. Isolated right ventricular hypoplasia. Circulation. 1971;44(3):466-474. doi:10.1161/01.cir.44.3.466
- Hypoplastic Right-Heart Syndrome Presenting as Multiple Miscarriages. Tex Heart Inst J. 2012; 39(2): 249–254. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3384066
- Rajiah P, Mak C, Dubinksy TJ, Dighe M. Ultrasound of fetal cardiac anomalies. AJR Am J Roentgenol. 2011;197(4):W747-W760. doi:10.2214/AJR.10.7287
- Rajiah P, Mak C, Dubinksy TJ, Dighe M. Ultrasound of fetal cardiac anomalies. AJR Am J Roentgenol. 2011;197(4):W747-W760. doi:10.2214/AJR.10.7287 https://www.ajronline.org/doi/10.2214/AJR.10.7287