Interrupted aortic arch
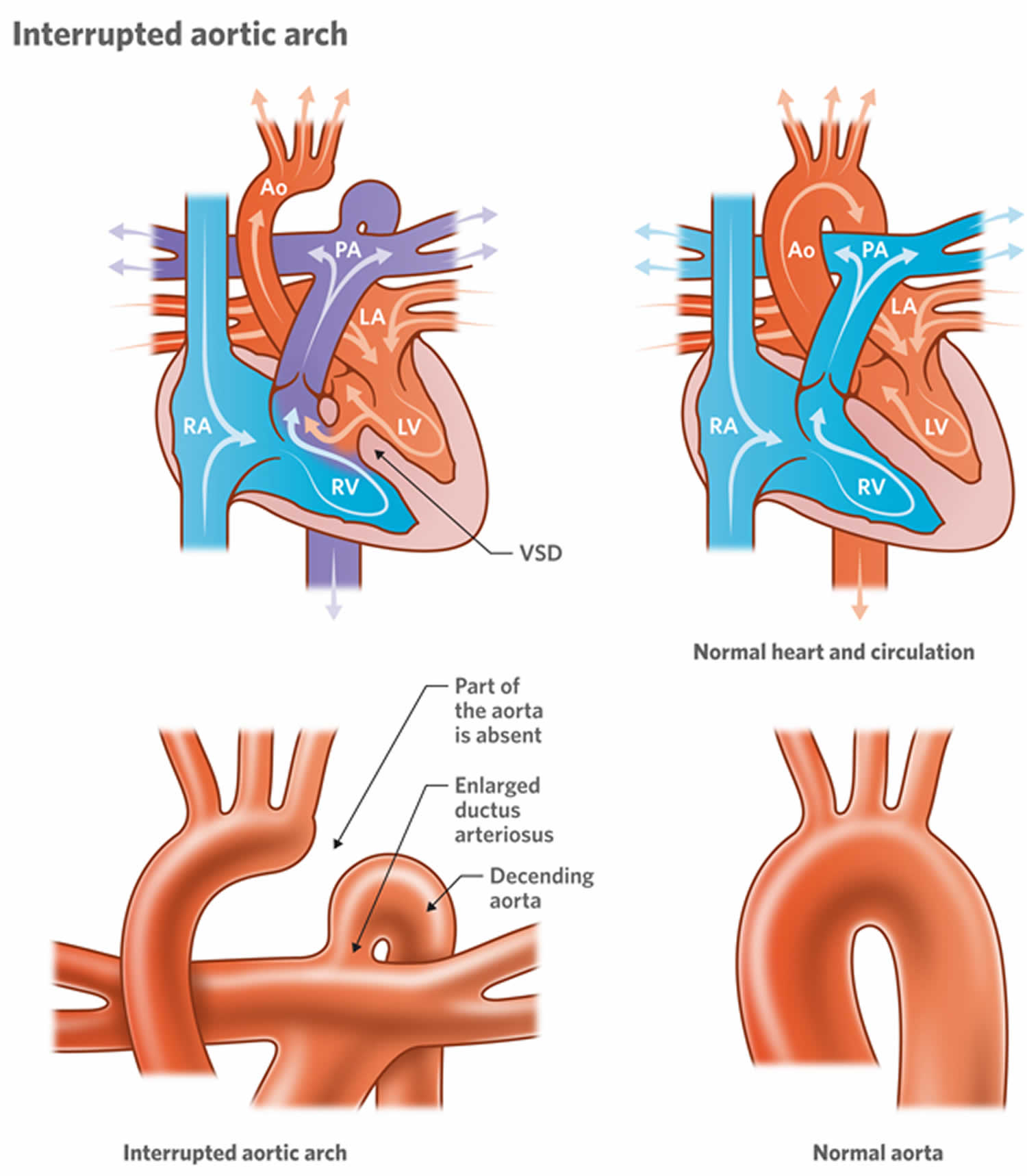
Interrupted aortic arch is a extremely rare congenital heart disease involving a loss of continuity between the ascending and descending aorta due to an absence or atresia of an aortic arch 1. In an interrupted aortic arch, there is an anatomical and luminal disruption between the ascending and descending aorta 2. Interrupted aortic arch is a patent ductus arteriosus dependent lesion since this is the only way the blood flow can travel to places distal to the disruption. There is posterior malalignment of the conal septum additional to the interrupted aortic arch, producing a ventricular septal defect as an associated lesion. Interrupted aortic arch is present is approximately 73% of all cases. Due to this malalignment, there could be left ventricular outflow tract obstruction. Besides a ventricular septal defect, interrupted aortic arch can be associated with other more complicated cardiac anomalies; for example, transposition of the great arteries, truncus arteriosus, aortopulmonary window, single ventricle, aortic valve atresia, right-sided ductus, and double-outlet right ventricle 3. Interrupted aortic arch is a rare type of congenital heart disease which affects approximately 1.5% of congenital heart disease patients 3. The incidence of interrupted aortic arch is about 2 cases per 100,000 live births.
Interrupted aortic arch is primarily considered to be a diagnosis in the neonatal period and clinical deterioration is often rapid and long-term prognosis is limited 4. Interrupted aortic arch might be associated with other anomalies including ventricular septal defects, single ventricle, truncus arteriosus, transposition of the great arteries, valvular abnormalities (eg, bicuspid aortic valve, aortic or mitral stenosis, etc.), DiGeorge Syndrome, among others 5. With anomaly it is highly unusual for a patient to survive without surgical interventional, because there would be no path for the blood to leave the heart and enter the systemic circulation [3]. Nonetheless, this condition has been identified later in adult life in rare cases 6. Patients with isolated interrupted aortic arch may survive until adulthood due to the development of significant collateral circulation ensuring the maintenance of a blood flow to the distal aorta 7. Clinical presentation of interrupted aortic arch in adults varies from absence of symptoms to hypertension, headache, malaise, differential blood pressure between arms and legs, claudication, limb swelling, and congestive heart failure. Most patients have refractory hypertension since adolescence or early adulthood 8.
About 37 cases of interrupted aortic arch in adults have been reported over the past 40 years 9, which has led to a better identification and description of this condition in adulthood. There have been some differences identified between neonatal interrupted aortic arch and adult interrupted aortic arch: in infants, interrupted aortic arch is usually associated with other congenital cardiovascular abnormalities, whereas in adults it is usually isolated; furthermore, in adults, type A interrupted aortic arch appears to be much more common in comparison with neonatal interrupted aortic arch, were type B and type C are more prevalent 6. Some hypotheses have been proposed for these differences. First, patients with type A interruptions are more likely to have adequate collateral flow to prevent severe symptoms. Second, patients with asymptomatic type B and C interrupted aortic arch have disparate upper extremities blood pressures, making diagnosis in childhood more common; and third, a subset of type A interruption may in fact represent the end point of a progressively narrowed aortic coarctation 9. This latter point could potentially mean that the adult form of interrupted aortic arch is altogether different from the neonatal form 6.
Gordon et al. 9 published a review of interrupted aortic arch in the adults, describing the 37 cases reported in the literature up until 2010. The average age of the cases reviewed was 39.4 years (range 18-72 years), and it was more commonly diagnosed among men (74%) than women (26%). Regarding clinical presentation, most patients had refractory hypertension as their presenting symptom, followed by claudication, congestive heart failure, and aortic insufficiency 9. Chest pain in our patient corresponded to aortic dissection and hemopericardium; associations of these serious complications have been reported in patients with bivalve aorta (>50 years; 17.4% [95% confidence interval 2.9%-53.6%]) with or without interrupted aortic arch 10. Chest pain has also been reported in patients with interrupted aortic arch and hypertensive crisis 11, a different type of interrupted aortic arch 12, or acute coronary syndrome 13.
The main treatment for interrupted aortic arch in the adult is the same as in infants, which is the reconstruction of the aortic continuity to enable appropriate blood flow, usually by surgical means (eg, end-to-end anastomosis, graft interposition, or extra-anastomotic bypass) or by percutaneous approach in selected patients 5. The main objective of the surgical intervention is to improve the patient’s symptomatology and to prevent potentially fatal complications 9. However, conventional surgical repair is typically a challenge because of the extent of collateral circulation in adult patients 6; therefore, the mortality rates can range from 15% to 20% 14. Unfortunately, even though if patient had a surgical intervention to correct the aortic arch, some died during the postoperative period within a week. Mortality in a case report may be secondary to the life-threatening complications present at initial presentation (aortic dissection plus hemopericardium), which might indicate that the initial clinical presentation of interrupted aortic arch in adults is an important factor in patient survival 4.
Figure 1. Interrupted aortic arch
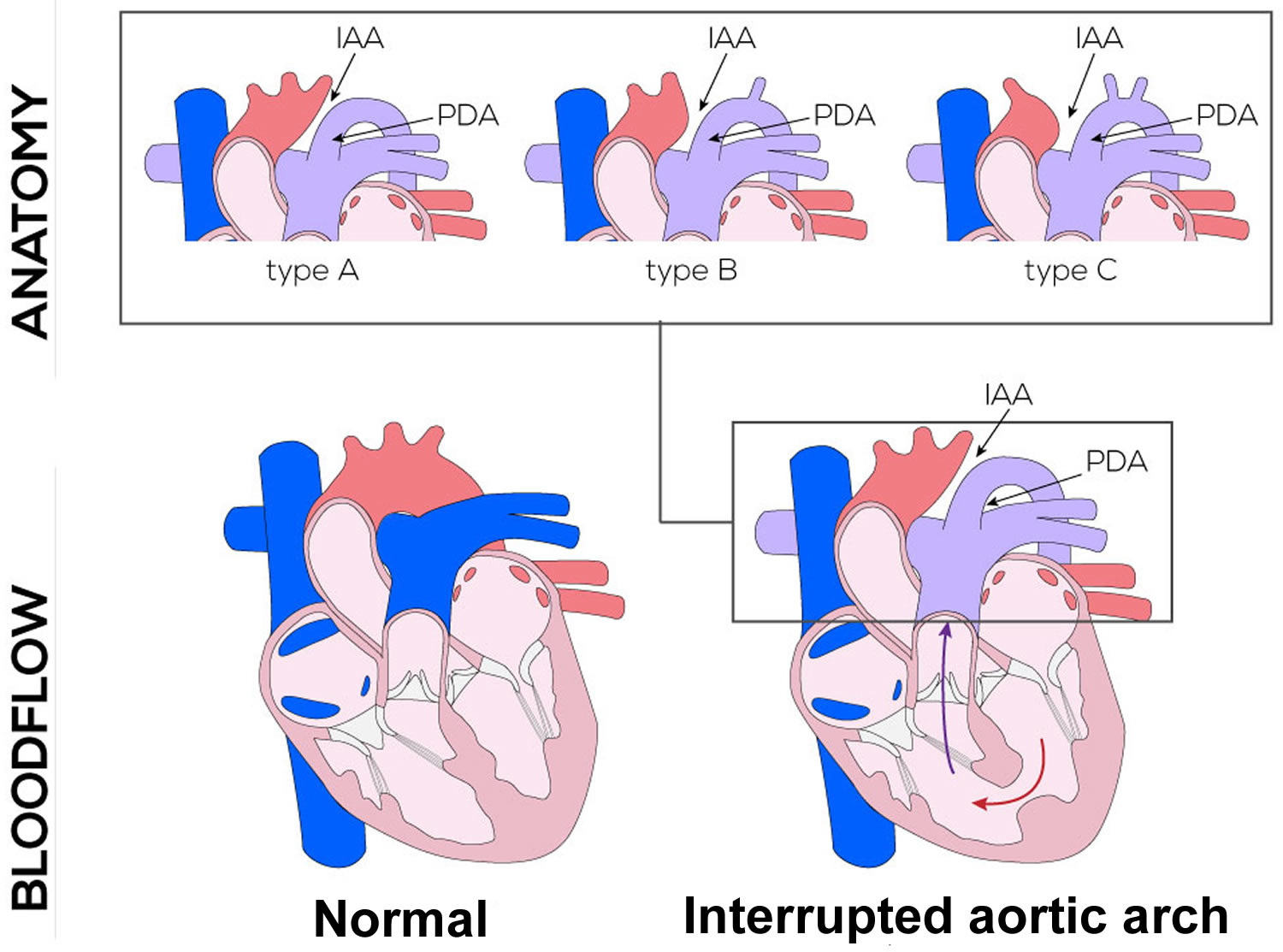
Interrupted aortic arch types
Interrupted aortic arch Celoria and Patton classification can be grouped into 3 anatomic types (ABC), depending on the site of the disruption 15:
- Interrupted aortic arch type A: the disruption is located distal to the left subclavian artery (interruption between the left subclavian artery and descending aorta; this is the second most common disruption represents approximately 13% of the cases.
- Interrupted aortic arch type B: the disruption is located between the left carotid artery and left subclavian artery; this is the most common anomaly, representing approximately 84% of the cases.
- Interrupted aortic arch type C: the disruption is located between the innominate artery and the left carotid artery; this is a rare type represents approximately 3% of all cases.
These three types of interrupted aortic arch can be sub-classified according to the origin of the subclavian artery:
- Type 1: Normal origin of the subclavian artery.
- Type 2: Aberrant right subclavian artery, found distal to the left subclavian artery.
- Type 3: Isolated right subclavian artery; found originating from a right patent ductus arteriosus.
All three types of interrupted aortic arch require that there be a patent ductus arteriosus to supply blood to the lower half of the body. During fetal circulation, the ductus arteriosus provides blood to the distal extremities of the fetus and the upper part of the body receives its blood supply from the left ventricle to the aorta. After birth, the pulmonary vascular resistance decreases, promoting the closure of the ductus arteriosus. This leads to the inability of the heart to provide blood to the distal part of the body and produces respiratory distress and cyanosis, leading to circulatory collapse, cardiogenic shock, metabolic acidosis and death if the necessary measures are not instated in time. The average infant born with an interrupted aortic arch is extremely ill and rarely survives more than a few weeks, typically only a few days.
Figure 2. Interrupted aortic arch types
Abbreviations: IAA = interrupted aortic arch; PDA = patent ductus arteriosus
Interrupted aortic arch causes
Almost 50% of patients with interrupted aortic arch have a 22q11.2 deletion; this cause of 22q11.2 deletion syndrome, also known as DiGeorge syndrome 2. Approximately 75% to 85% of patients with a 22q11.2 deletion have congenital heart disease that can range from asymptomatic to very severe that requires intervention in the newborn period. Besides an interrupted aortic arch, these patients can have other types of congenital heart diseases that can be classified into two groups, the branchial arch defects, and conotruncal defects. Branchial arch defects include interrupted aortic arch, coarctation of the aorta, and right aortic arch. Conotruncal defects include tetralogy of Fallot, sub-arterial ventricular septal defects, double-outlet right ventricle, and truncus arteriosus. Another syndrome associated with interrupted aortic arch is CHARGE syndrome.
Interrupted aortic arch symptoms
Nearly all patients with interrupted aortic arch present in the first 2 weeks of life when the ductus arteriosus closes. Most patients present in the first day of life. The baby may be asymptomatic until the ductus arteriosus closes and the patient develops tachypnea, feeding difficulties, respiratory distress, cyanosis, and anuria which, ultimately, can lead to shock and death. The physical exam will reveal absent pulses with a difference in blood pressure between the right arm and lower extremities. Sometimes, there may be an oxygen discrepancy between the left and right side of the body.
Interrupted aortic arch diagnosis
When the diagnosis is suspected, it is important as initial work up to perform a blood gas, chest radiograph, electrocardiogram, and echocardiogram. The blood gas will reveal metabolic acidosis. The chest radiograph will show cardiomegaly and increased pulmonary markings. The electrocardiogram, typically, has nonspecific findings which include biventricular hypertrophy or right ventricular predominance. The echocardiogram will define the site of the disruption. Other imaging modalities used for the diagnosis of this entity are cardiac angiography, computed tomography angiography of the chest, and magnetic resonance angiography. These modalities are used to get a more comprehensive understanding of the lesion’s anatomy before surgical repair 1.
In addition to the imaging studies, all patients should have a fluorescence in situ hybridization since there is a high association with chromosome 22q11 deletion, which is associated with DiGeorge syndrome. Serum calcium may be low in patients with DiGeorge syndrome 3.
Interrupted aortic arch treatment
Management of interrupted aortic arch begins with administration of prostaglandin E to maintain a patent ductus arteriosus and blood supply to the lower body, to avoid sudden cardiac collapse and death 16. The role of the prostaglandins is to maintain the patency of the ductus arteriosus, thus guaranteeing the perfusion of the lower part of the body until surgical correction is done. In the presence of shock, the patient should be managed with inotrope support, and treatment should be adjusted depending on the clinical response of the patient.
It is recommended that surgical correction take place as soon as metabolic acidosis is controlled. The objective of the surgery is to form unobstructed continuity between the ascending and descending aorta and to repair associated defects with the most common atrial and/or ventricular septum defect. The repair is done using either native arterial tissue, a homograph, or autograph vascular patch. For ventricular septal defect, repairs are closed with a synthetic patch. This synthetic patch is made up of polyester or polytetrafluoroethylene (ePTFE). A median sternotomy, cardiopulmonary bypass, and hypothermia are utilized for this procedure. Excision of the ductal tissue and re-anastomosis of the aortic arch are performed to create unobstructed continuity between the parts of the aorta. The anastomosis consists either entirely of native arterial tissue or requires an additional homograft/autograft patch. Any additional defects such as a ventricular septum defect will be repaired contemporarily.
An alternative route to a definitive single-operation repair of the arch is to implement a two-stage approach. This approach consists of the reconstruction and placement of a pulmonary artery band in stage 1, postponing the placement of the ventricular septal defect closure to a later time. For the second stage procedure of the procedure, the pulmonary band is removed 17.
In cases of significant outflow tract obstruction, it may be necessary to perform a complex combination of the Norwood and Rastelli procedures 17. In the Norwood-Rastelli procedure, an interventricular baffle allows left ventricular blood to reach not only the aortic outflow but also the pulmonary annulus (Rastelli), and the main pulmonary artery is transected 18. The proximal portion is anastomosed to the ascending aorta (Norwood) while the distal portion is connected to the right ventricle via a conduit (Rastelli).
Following surgical reconstruction, echocardiographic and Doppler evaluation of the adequacy of the repair should be performed.
Interrupted aortic arch survival rate
The prognosis of these infants is dependent on birth weight, associated heart defects and time of surgery. The outlook for most infants is guarded and multiple heart surgeries are often needed. In most cases of interrupted aortic arch, with good surgical repair, the prognosis is excellent.
About 37 cases of interrupted aortic arch in adults have been reported over the past 40 years 9, which has led to a better identification and description of this condition in adulthood. There have been some differences identified between neonatal interrupted aortic arch and adult interrupted aortic arch: in infants, interrupted aortic arch is usually associated with other congenital cardiovascular abnormalities, whereas in adults it is usually isolated; furthermore, in adults, type A interrupted aortic arch appears to be much more common in comparison with neonatal interrupted aortic arch, were type B and type C are more prevalent 6. Some hypotheses have been proposed for these differences. First, patients with type A interruptions are more likely to have adequate collateral flow to prevent severe symptoms. Second, patients with asymptomatic type B and C interrupted aortic arch have disparate upper extremities blood pressures, making diagnosis in childhood more common; and third, a subset of type A interruption may in fact represent the end point of a progressively narrowed aortic coarctation 9. This latter point could potentially mean that the adult form of interrupted aortic arch is altogether different from the neonatal form 6.
Gordon et al. 9 published a review of interrupted aortic arch in the adults, describing the 37 cases reported in the literature up until 2010. The average age of the cases reviewed was 39.4 years (range 18-72 years), and it was more commonly diagnosed among men (74%) than women (26%). Regarding clinical presentation, most patients had refractory hypertension as their presenting symptom, followed by claudication, congestive heart failure, and aortic insufficiency 9. Chest pain in our patient corresponded to aortic dissection and hemopericardium; associations of these serious complications have been reported in patients with bivalve aorta (>50 years; 17.4% [95% confidence interval 2.9%-53.6%]) with or without interrupted aortic arch 10. Chest pain has also been reported in patients with interrupted aortic arch and hypertensive crisis 11, a different type of interrupted aortic arch 12, or acute coronary syndrome 13.
References- Patel DM, Maldjian PD, Lovoulos C. Interrupted aortic arch with post-interruption aneurysm and bicuspid aortic valve in an adult: a case report and literature review. Radiol Case Rep. 2015 Oct;10(3):5-8.
- Ramirez Alcantara J, Mendez MD. Interrupted Aortic Arch. [Updated 2019 Feb 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532902
- Varghese R, Saheed SB, Omoregbee B, Ninan B, Pavithran S, Kothandam S. Surgical Repair of Interrupted Aortic Arch and Interrupted Pulmonary Artery. Ann. Thorac. Surg. 2015 Dec;100(6):e139-40.
- Pérez TM, García SM, Velasco ML, Sánchez AP. Interrupted aortic arch diagnosis by computed tomography angiography and 3-D reconstruction: A case report. Radiol Case Rep. 2017;13(1):35–38. Published 2017 Nov 17. doi:10.1016/j.radcr.2017.10.001 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851190
- Liping C., Pradhan D., Jing Z., Hongwei Z., Shrestha R. Isolated interrupted aortic arch in a 42-year-old adult—case report. J Clin Ultrasound. 2013;41:521–523.
- Borgohain S., Gupta A., Grover V., Gupta V.K. Isolated interrupted aortic arch in an 18-year-old man. Texas Hear Inst J. 2013;40:79–81.
- Kimura-Hayama E.T., Meléndez G., Mendizábal A.L., Meave-González A., Zambrana G.F.B., Corona-Villalobos C.P. Uncommon congenital and acquired aortic diseases: role of multidetector CT angiography. Radiographics. 2010;30:79–98.
- Ponte M., Dias A., Dias Ferreira N., Fonseca C., Mota J.C., Gama V. Interrupted aortic arch: a misdiagnosed cause of hypertension. Rev Port Cardiol. 2014;33:389.e1–389.e5.
- Gordon E.A., Person T., Kavarana M., Ikonomidis J.S. Interrupted aortic arch in the adult. J Card Surg. 2011;26:405–409.
- Michelena H.I., Khanna A.D., Mahoney D., Margaryan E., Topilsky Y., Suri R.M. Incidence of aortic complications in patients with bicuspid aortic valves. JAMA. 2011;306:1104–1112.
- Maier J.M., Scheffold N., Cyran J. Primary diagnosis of an interrupted aortic arch in a 65-year old woman with hypertension. Dtsch Med Wochenschr. 2005;130:2893–2896.
- Sim M.-M., Chen C.-C. Transthoracic echocardiographic diagnosis of a type C interrupted aortic arch in an adult. J Am Soc Echocardiogr. 2007;20:1418.e1–1418.e4.
- Riess F.-C., Danne M., Stripling J.-H., Bergmann H., Bleese N. Surgical treatment of interrupted aortic arch with extraanatomical bypass simultaneous to coronary artery bypass grafting and aortic valve replacement. Heart Surg Forum. 2004;7:E394–E397.
- Sandhu S.K., Pettitt T.W. Interrupted aortic arch. Curr Treat Options Cardiovasc Med. 2002;4:337–340.
- Mendoza Díaz PM, Herrera Gomar M, Rojano Castillo J. Interrupted Aortic Arch in an Adult and Myocardial Infarction. Rev Esp Cardiol (Engl Ed). 2016 Feb;69(2):212.
- Hu XJ, Ma XJ, Zhao QM, Yan WL, Ge XL, Jia B, Liu F, Wu L, Ye M, Liang XC, Zhang J, Gao Y, Zhai XW, Huang GY. Pulse Oximetry and Auscultation for Congenital Heart Disease Detection. Pediatrics. 2017 Oct;140(4).
- Alsoufi B, Schlosser B, McCracken C, Sachdeva R, Kogon B, Border W, Mahle WT, Kanter K. Selective management strategy of interrupted aortic arch mitigates left ventricular outflow tract obstruction risk. J. Thorac. Cardiovasc. Surg. 2016 Feb;151(2):412-20.
- Steger V, Heinemann MK, Irtel von Brenndorff C. Combined Norwood and Rastelli procedure for repair of interrupted aortic arch with subaortic stenosis. Thorac Cardiovasc Surg. 1998 Jun. 46(3):156-8.