What is intervertebral disc
Intervertebral discs are found between the bodies of adjacent vertebrae from the second cervical vertebra to the sacrum and account for about 25% to 33% of the
height of the vertebral column. There are 25 intervertebral discs (7 cervical, 12 thoracic, 5 lumbar, and 1 sacral). There is no intervertebral disc between C1 and C2, which is unique in the spine 1. Each intervertebral disc has an outer fibrous ring consisting of fibrocartilage called the annulus fibrosus (annulus = ringlike) and an inner soft , pulpy, highly elastic substance called the nucleus pulposus (pulposus = pulplike). The superior and inferior surfaces of the intervertebral disc consist of a thin plate of hyaline cartilage endplates that anchor the discs to adjacent vertebrae 2. The intervertebral discs form strong joints, permit various movements of the vertebral column, and absorb vertical shock. Under compression, they flatten and broaden. Degenerative changes in the anulus fibrosus can lead to herniation of the nucleus pulposus. Posterolateral herniation can impinge on the roots of a spinal nerve in the intervertebral foramen.
- The anulus fibrosus is a ring-shaped disc of fibrous connective tissue that surrounds the nucleus pulposus. This structure is highly organized, consisting of 15 to 25 stacked sheets, or “lamellae,” of predominantly collagen, with interspersed proteoglycans, glycoproteins, elastic fibers, and the connective tissue cells that secrete these extracellular matrix products. Each lamella contains collagen uniformly oriented in a plane that differs in orientation to adjacent lamella by about 60 degrees. This alignment leads to the parallel orientation of alternate lamella. This “radial-ply” formation provides exceptional strength compared to an entirely longitudinal setup and has been mimicked in the construction of products such as car tires. The lamellae are interconnected through translamellar bridges. The number of translamellar bridges per unit area is set to achieve a balance between strength and flexibility. A greater number of bridges would provide greater resistance to compressive forces, but would limit flexibility, and vice-versa. The anulus fibrosus contains an inner and an outer portion. They differ primarily in their collagen composition. While both are primarily collagen, the outer annulus contains mostly type I collagen, while the inner has predominantly type II. The inner annulus also contains more proteoglycans than the inner. The ratio of type I to type II changes gradually; as the distance from the nucleus pulposus increases, the amount of type II collagen decreases, while the amount of type I increases. Another major difference between the two segments is the morphology of the connective tissue cells that secrete extracellular matrix. The cells of the inner annulus are described as round, while the outer annulus has a more oblong, fibroblast-like appearance 3.
- The nucleus pulposus fills the center of the intervertebral disc, is gelatinous, and absorbs compression forces between vertebrae. The nucleus pulposus is a gel-like structure that sits at the center of the intervertebral disc and accounts for much of the strength and flexibility of the spine. It is made of 66% to 86% water with the remainder consisting of primarily type II collagen (it may also contain type VI, IX, and XI) and proteoglycans. The proteoglycans include the larger aggrecan and versican that bind to hyaluronic acid, as well as several small leucine-rich proteoglycans. Aggrecan is largely responsible for retaining water within the nucleus pulposus. This structure also contains a low density of cells. While sparse, these cells produce the extracellular matrix (ECM) products (aggrecan, type II collagen, etc.) and maintain the integrity of the nucleus pulposus.
During the course of a day the discs compress and lose water from their cartilage so that we are a bit shorter at night. While you are sleeping there is less compression and rehydration occurs, so that you are taller when you awaken in the morning. With age, the nucleus pulposus hardens and becomes less elastic. Decrease in vertebral height with age results from bone loss in the vertebral bodies and not a decrease in thickness of the intervertebral discs.
Intervertebral disc thickness generally increases from rostral to caudal, except for a nadir at T3-T4. The thickness of the intervertebral discs relative to the size of the vertebral bodies is highest in the cervical and lumbar regions. This reflects the increased range of motion found in those regions.
In the cervical and lumbar regions, the intervertebral discs are thicker anteriorly. This creates the secondary curvature of the spine – the cervical and lumbar lordoses.
Since intervertebral discs are avascular, the annulus fibrosus and nucleus pulposus rely on blood vessels from the bodies of vertebrae to obtain oxygen and nutrients and remove wastes. Certain stretching exercises, such as yoga, decompress discs and increase general blood circulation, both of which speed up the uptake of oxygen and nutrients by discs and the removal of wastes.
While only the outer third of the anulus fibrosus is vascular and innervated in a non-pathologic state, in aging and states of inflammation, nerve growth and granulation tissue growth are stimulated. Additionally, the granulation tissue secretes inflammatory cytokines, which further increases sensitivity to pain sensations.
Two major ligaments support the intervertebral discs. The anterior longitudinal ligament is a broadband that covers the anterolateral surface of the spine from the foramen magnum in the skull to the sacrum. This ligament assists the spine in preventing hyperextension and prevents intervertebral disc herniation in the anterolateral direction. The posterior longitudinal ligament covers the posterior aspect of the vertebral bodies, within the vertebral canal, and serves mainly to prevent a posterior herniation of the intervertebral discs, and is therefore responsible for the most herniations being in the postero-lateral direction.
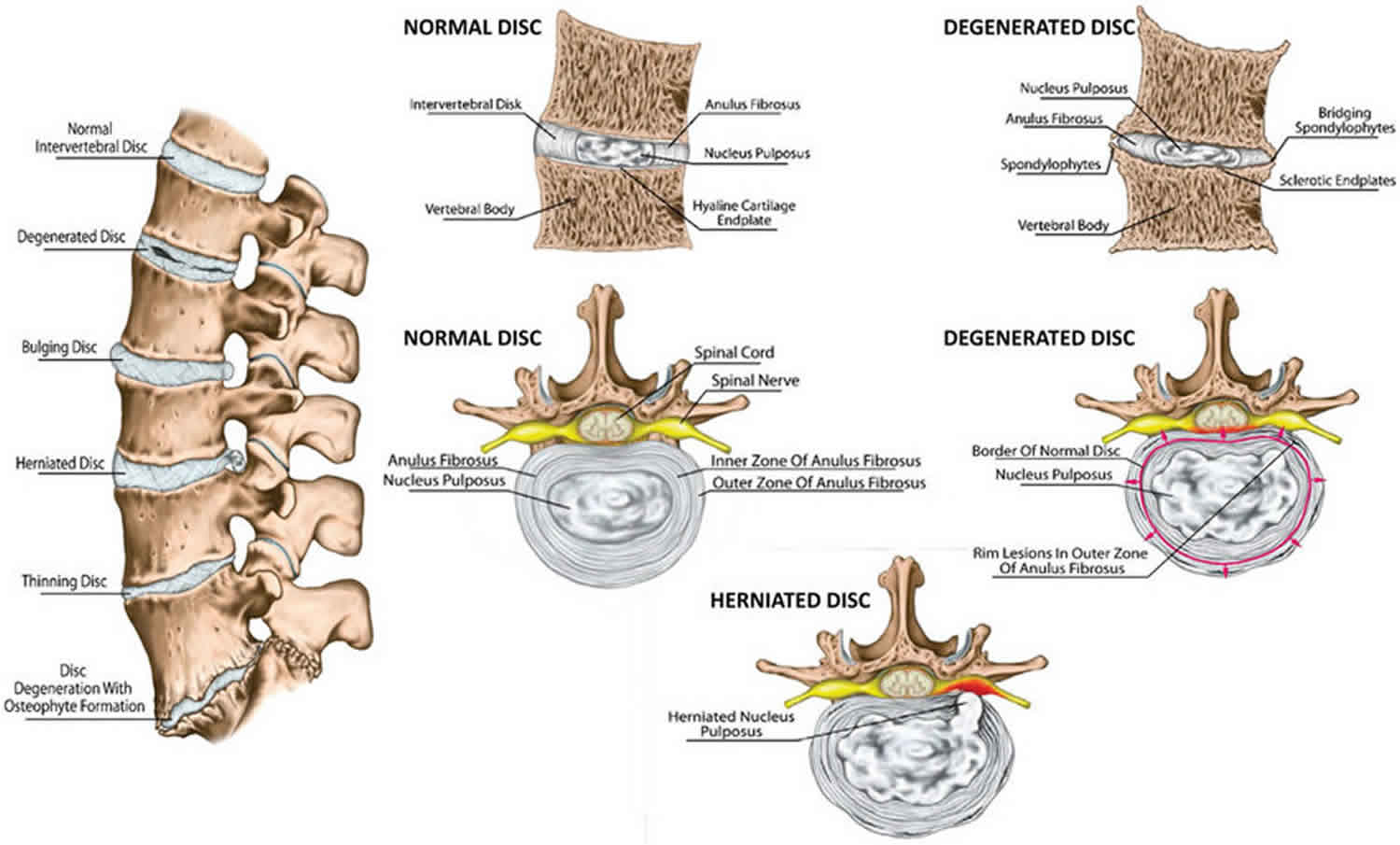
Figure 1. Intervertebral disc disease
Intervertebral disc function
Intervertebral discs serve a number of vital functions in the form structural support and locomotion. Intervertebral discs allow the spine to be flexible without sacrificing a great deal of strength. Intervertebral discs also provide a shock-absorbing effect within the spine and prevent the vertebrae from grinding together. Within the intervertebral disc, itself, the separate components serve different purposes. The nucleus pulposus serves to distribute hydraulic pressure throughout the intervertebral disc. By virtue of its high water content, the nucleus pulposus can disperse the forces placed on one aspect of a vertebral body to the entire structure. A solid nucleus pulposus, in contrast, would transmit a force placed on one aspect of a vertebral body directly to the corresponding aspect of the inferior vertebral body, thus increasing the risk of trauma. The annulus fibrosus serves, for one, to encircle the nucleus pulposus as a “cage” to provide structure to the gelatinous form. The aforementioned “radial-ply” configuration allows for increased resistance to the compressive forces exerted upon it by the nucleus pulposus. Given the general rostral-caudal direction of the fibers, the annulus fibrosus also resists torsion, flexion and extension movements of the spine.
Holistically, the intervertebral discs first allow for the spine to be both a supportive, yet flexible structure. They provide separation and connectivity between vertebrae and counteract forces that act to lengthen or compress the spine or affect it in a torsional or shear manner. They also sufficiently separate the vertebrae to allow spinal nerves to exit the intervertebral foramina.
In a similar vein to the flexibility created by the intervertebral discs, they also have a protective effect on vertebrae. This “shock-absorbing” feature distributes forces throughout the spine – lessening the load on any one vertebra, thus reducing the risk of fracture and degenerative changes.
Intervertebral disc disorder
There are several terms to describe disc disorders.
In intervertebral disc bulge, the circumference of disc extends beyond the vertebral bodies. A intervertebral disc bulge may be circumferential, involving the entirety of the disc circumference, or an asymmetric bulge, which only affects one portion of the disc 4.
A intervertebral disc herniation involves the nucleus pulposus. Disc herniation is significant in that it may compress an adjacent spinal nerve. A herniated disc impinges upon the nerve associated with the inferior vertebrae (e.g., L4/L5 herniation affects the L5 nerve root). The most common site of disc herniation is at L5-S1, which may be due to the thinning of the posterior longitudinal ligament towards its caudal end.
There are three subtypes of herniated intervertebral disc:
- Intervertebral disc protrusion is characterized by the width of the base of the protrusion is wider than the diameter of the disc material that is herniated.
- In intervertebral disc extrusion, the anulus fibrosus is damaged, allowing the nucleus pulposus to herniate beyond the normal bounds of the disc. In this case, the herniated material produces a mushroom-like dome that is wider than the neck connecting it to the body of the nucleus pulposus. The herniation may extend superior or inferiorly relative to the disc level.
- In intervertebral disc sequestration, the herniated material breaks off from the body of the nucleus pulposus.
Intervertebral disc desiccation is common in aging. It is brought about by the death of the cells that produce and maintain the extracellular matrix, including proteoglycans, such as aggrecan. The nucleus pulposus shrinks as the gelatinous form is replaced with fibrotic tissue, reducing its functionality, and leaves the anulus fibrosus supporting additional weight. This increased stress leads the anulus fibrosus to compensate by increasing in size. The resulting flattened disc reduces mobility and may impinge on spinal nerves leading to pain and weakness. It is thought to be due to proteoglycan breakdown, which reduces the water-retaining properties of the nucleus pulposus.
Significant research has been put into means of replacing/re-growing the intervertebral discs. The various methods include the replacement of discs with synthetic materials, stem cell therapy, and gene therapy.
Herniated intervertebral disc
A common source of back or neck pain is a herniated intervertebral disc. Sometimes called a “slipped” or “ruptured” disc, this condition most often occurs in the lower back, as well as the smaller intervertebral discs in the neck. The incidence of herniated intervertebral disc is about 5 to 20 cases per 1000 adults annually and is most common in people in their third to the fifth decade of life, with a male to female ratio of 2:1.
Intervertebral disc herniation is more likely to occur posterolaterally, where the annulus fibrosus is thinner and lacks the structural support from the anterior or posterior longitudinal ligaments. Because of the proximity to the nerve roots, a posterolateral herniation is more likely to compress the nerve root and to produce radiculopathies in the associated dermatome. On the other hand, spinal cord compression and clinical myelopathy can occur if there is herniation of a large midline disc. The localized back pain is a combination of the herniated disc pressure on the longitudinal ligament, and chemical irritation due to local inflammation.
Although a herniated intervertebral disc can sometimes be very painful, most people feel much better with just a few months of simple, nonsurgical treatments.
Over 85% patients with symptoms associated with acute herniated disc will resolve within 8 to 12 weeks without any specific treatments 5. However, patients who have an abnormal neurological examination or refractory to conservative treatments will need further evaluation and treatments.
Herniated intervertebral disc cause
A intervertebral disc herniates or ruptures when part of the center nucleus pushes through the outer edge of the disk and back toward the spinal canal. This puts pressure on the nerves. Spinal nerves are very sensitive to even slight amounts of pressure, which can result in pain, numbness, or weakness in one or both legs.
While the biological causes of intervertebral disc herniation itself are well known, the biological causes of the symptoms of intervertebral disc herniations are still under investigation. The pathophysiology of herniated intervertebral discs is believed to be a combination of the mechanical compression of the nerve by the bulging nucleus pulposus and the local increase in inflammatory chemokines. Current thought is that while mechanical compression of spinal nerves is an important cause of pain in intervertebral disc herniation, another possible factor on the perception of pain is the effect of the nucleus pulposus on nervous tissue 6. The theory is that the leakage of the nucleus pulposus can cause an inflammatory reaction that in turn causes changes in the nerve roots themselves.
A recent study showed that when peripheral nerves and dorsal root ganglia suffered exposure to the contents of the nucleus pulposus, there was a considerable increase in neuronal activity in these neuronal tissues starting at 9 hours and lasting for up to a couple of days. Similar changes also showed in the spinal cord in this same study. This study also revealed that when applying the nucleus pulposus in the absence of mechanical compression, the neural activity in the ventral posterolateral nucleus of the thalamus increased quickly 6. The ventral posterolateral is an endpoint for the spinothalamic tract which sends pain signals from the periphery to the brain. These neurons are excited in response to painful mechanical stimuli as well as visceral nociception 7. This study helps to show that the painful symptoms of intervertebral disc herniation have two primary contributing factors: mechanical compression and inflammatory response to the nucleus pulposus 8.
Risk factors for herniated intervertebral disc
In children and young adults, disks have high water content. As people age, the water content in the discs decreases and the discs become less flexible. The discs begin to shrink and the spaces between the vertebrae get narrower. Conditions that can weaken the disc include:
- Improper lifting
- Smoking
- Excessive body weight that places added stress on the disks (in the lower back)
- Sudden pressure (which may be slight)
- Repetitive strenuous activities
Herniated intervertebral disc symptoms
Lower Back
Low back pain affects many people. Pain alone is not enough to recognize a herniated intervertebral disc. See your doctor if back pain results from a fall or a blow to your back. The most common symptom of a herniated intervertebral disc is sciatica—a sharp, often shooting pain that extends from the buttocks down the back of one leg. It is caused by pressure on the spinal nerve. Other symptoms include:
- Back pain
- Weakness in the leg and/or foot
- Tingling (a “pins-and-needles” sensation) or numbness in the leg and/or foot
- Loss of bladder or bowel control (This is rare and may indicate a more serious problem called cauda equina syndrome. This condition is caused by the spinal nerve roots being compressed. It requires immediate medical attention.)
Neck
As with pain in the lower back, neck pain is also common. When pressure is placed on a nerve in the neck, it causes pain in the muscles between your neck and shoulder (trapezius muscles). The pain may shoot down the arm. Other symptoms include:
- Weakness in one arm
- Tingling (a “pins-and-needles” sensation) or numbness in one arm
- Burning pain in the shoulders, neck, or arm
Herniated intervertebral disc diagnosis
To determine whether you have a herniated intervertebral dis, your doctor will ask you for a complete medical history and conduct a physical examination.
A physical examination will help determine which nerve roots are affected.
To help confirm a diagnosis of herniated disc, your doctor may recommend a magnetic resonance imaging (MRI) scan. This test can create clear images of soft tissues like intervertebral discs.
Herniated intervertebral disc treatment
Nonsurgical treatment
Nonsurgical treatment is effective in treating the symptoms of herniated discs in the majority of patients. Most neck or back pain will resolve gradually with simple measures.
- Rest and over-the-counter pain relievers may be all that is needed.
- Muscle relaxers, analgesics, and anti-inflammatory medications are also helpful.
- Cold compresses or ice can also be applied several times a day for no more than 20 minutes at a time.
- After any spasms settle, gentle heat applications may be used.
Any physical activity should be slow and controlled, especially bending forward and lifting. This can help ensure that symptoms do not return, as can taking short walks and avoiding sitting for long periods. For the lower back, exercises may also be helpful in strengthening the back and abdominal muscles. For the neck, exercises or traction may also be helpful. To help avoid future episodes of pain, it is essential that you learn how to properly stand, sit, and lift.
If these nonsurgical treatment measures fail, epidural injections of a cortisone-like drug may lessen nerve irritation and allow more effective participation in physical therapy. These injections are given on an outpatient basis over a period of weeks.
Surgical treatment
Only a small percentage of patients with disc herniations require surgery. Spine surgery is typically recommended only after a period of nonsurgical treatment has not relieved painful symptoms.
- Lumbar microdiscectomy. This is the most common procedure for a herniated disc in the lower back. Microdiscectomy involves removing the herniated part of the disc and any fragments that are putting pressure on the spinal nerve.
- Cervical discectomy and fusion. Cervical discectomy is a procedure for the herniated disc in the neck. To relieve pressure, the entire herniated disc is removed. Bone is placed in the disc space and a metal plate may be used to help support the spine.
Intervertebral disc degeneration
Intervertebral disc degeneration is directly correlated with increasing patient age 9. Interestingly, while it is thought that men likely start this degeneration almost ten years earlier than women, women with disc degeneration are likely to be more susceptible to the effects (e.g., malalignment, instability) 10.
Traditionally, dating back to the early 1990s, the traditional views regarding the causes of intervertebral disc degeneration focused on environmental exposures such as smoking, vehicular vibration, and occupation. More recent research has highlighted the genetic components associated with disc disease and shifted the paradigm away from the aforementioned social, occupational, and environmental factors.
The contemporary general consensus advocates the importance of these genetic factors as the most important predictors of intervertebral disc degeneration, and the environmental factors are recognized as additional, minor contributors to disease onset 9. The effects of smoking also have been questioned with more recent research only finding weak correlations with cigarette use and intervertebral disc disease. Similarly, while occupational aspects (e.g., heavy lifting, forceful bending) may have some contributions to lumbar degeneration, it is now thought that socioeconomic factors likely confound these studies, and occupational exposure is, at most, a minor contributor to intervertebral disc disease.
A disruption of the normal architecture of these round intervertebral discs can lead to a disc herniation or a protrusion of the inner nucleus pulposus, possibly applying pressure to the spinal cord or nerve root and resulting in radiating pain and specific locations of weakness. Slightly more than 90% of herniated discs occur at the L4-L5 or the L5-S1 disc space, which will impinge on the L4, L5 or S1 nerve root. This compression produces a radiculopathy into the posterior leg and dorsal foot.
If the intervertebral disc injury progresses to the point of neurologic compromise or limitations with activities of daily living, then surgical intervention may be required to decompress and stabilize the affected segments. In the absence of motor deficits, a nonoperative course of analgesia, activity modification, and injections should be tried for several months. The surgical results for the primarily sciatic pain that has failed conservative treatment are predictable and favorable 11.
Most intervertebral disc degenerations are asymptomatic, making a true understanding of the prevalence difficult. Additionally, due to the lack of uniformity in the definitions of intervertebral disc degenerations and intervertebral disc herniations, the actual prevalence of the intervertebral disc degeneration is difficult to review across multiple studies. In a meta-analysis of 20 studies evaluating the MRI of asymptotic individuals, the reported intervertebral disc abnormalities at any level were: 20% to 83% for reduction in signal intensity, 10% to 81% for disc bulges, 3% to 63% for disc protrusion (versus 0% to 24% for disc extrusion), 3% to 56% for disc narrowing, and 6% to 56% with annular tears. This study supports that the mere incidental finding of intervertebral disc disease is common and should not necessitate specialist evaluation in the absences of pain or limitations 12.
The radiation of back pain associated with disc disease is thought to be due to the compression of the nerve roots in the spinal canal from either one, or a combination of, the following elements:
Disc herniation material (i.e. herniated nucleus pulposus)
- Varying degrees of herniated nucleus pulposus is recognized, from disc protrusion (annulus remains intact), extrusion (annular compromise, but herniated material remains continuous with disc space), to sequestered (free) fragments
- Herniated nucleus pulposus material predictably is resorbed over time, with the sequestered fragment demonstrating the highest degree of resorption potential
- In general, 90% of patients will have symptomatic improvement in radicular symptoms within 3 months following nonoperative protocols alone
Hypertrophy/expansion of degenerative tissues
- Common sources include ligamentum flavum and the facet joint. The facet joint itself undergoes degenerative changes (just like any other joint in the body) and synovial hypertrophy and/or associated cysts can compromise surrounding nerve roots.
In a 2010 study by Suri et al. 662% of 154 consecutive patients presenting with new lumbar intervertebral disc herniation noted spontaneous symptoms compared to just 26% who reported the symptoms starting after a specific household task or seemingly common non-lifting activity. Contrary to popular belief, fewer than 8% reported acute sciatica after heavy lifting or physical trauma 13.
The many tiny blood vessels surrounding the spinal cord and nerve roots are paramount to delivering nutrition, oxygen, and chemomodulators. Compression of these structures limits the ability of these vessels to deliver vital nutrients, resulting in an ischemic effect of the structure. The subsequent inflammation from intervertebral disc compression results in (ischemic) pain along the path of this nerve root. This nerve compression from the disc causes an increase in cytokines, TNF-alpha, and recruitment of macrophages. Interestingly, the extent of the histologic changes within the intervertebral disc has a positive correlation with body mass index, indicating that those with obesity may be more prone to degeneration.
Intervertebral disc degeneration signs and symptoms
Classically, patients complain of pain radiating down both buttocks and lower extremities. It is helpful to determine if the pain is localized to the lower back or if there is radiation into the leg(s). A presentation of radiating pain correlates with canal stenosis. Radiating pain as the main issue has a much more predictable surgical outcome compared to a presentation of non-specific lower back pain that likely is related to muscle fatigue and strain. A mechanical component to the back pain (i.e., pain only with certain movements) may indicate instability or a degenerative pars fracture. It also is important in any evaluation of extremity issues to inspect circulation, as vascular claudication may mirror or mimic the neurogenic issues.
An evaluation of the patient walking is critical to better assess the daily impact the pain/deficit is causing. Having the patient arise from the chair, walk on his or her heels and toes, and then sit on the examination table for testing of strength, reflex, and straight leg testing is one systematic order. The gait assessment should include ruling out a trendelenburg gait, which can reveal underlying weakness in gluteus medius, innervated by the L5 nerve root.
All physical examinations will include evaluation of the neurologic function of the arms, legs, bladder, and bowels. The keys to a thorough exam are organization and patience. One should not only evaluate strength, but also sensation and reflexes. It is also important to inspect the skin along the back and document the presence of tenderness to compression or any prior surgical scars.
The straight leg raise (SLR) test consists of a supine patient having his/her fully extended leg passively stretched from 0 to about 80 degrees. The onset of radiating back pain in either leg supports a diagnosis of a stenotic canal. A herniation compressing the L5 nerve root will present as a weakness of ankle dorsiflexion and an extension of the great toe. This deficit also may diminish the Achilles tendon reflex. An L4 radiculopathy may present with weakness at the quadriceps and a decreased patellar tendon reflex.
Documentation is paramount, as these initial findings likely will be used as a baseline for all future evaluations.
Wadell Signs
A comprehensive examination should also include ruling out non-organic causes of low back pain/symptoms. When the clinician suspects potential malingering, consideration should be given to the following:
- Nonspecific description of symptoms or inconsistency, including superficial/non-anatomic sites of tenderness on exam
- Pain with axial load/rotational movements
- Negative straight leg raise with patient distraction (one approach includes having the patient sitting in a chair and reproducing the straight leg raise “environment”)
- Non-dermatomal patterns of distribution of symptoms
- Pain out of proportion on the exam
Intervertebral disc degeneration diagnosis
Evaluation of patients with low back pain typically includes anterior-posterior (AP) and lateral radiographs of the impacted area. Some physicians will obtain radiographs of the entire spine. An MRI should not be ordered at initial presentation of suspected acute disc herniations in patients lacking “red flags,” because these patients will initially trial a 6-week course of physical therapy and frequently improve. An MRI likely is an unnecessary financial and utilization burden in the initial presentation. If at follow-up the symptomology is still present, then an MRI can be obtained at that time. The focus should be directed to the T2 weighted sagittal, and axial images as these will illustrate any compression of neurologic elements. Over time, both symptomatic and asymptomatic disc herniations will decrease in size on MRI. The finding of disc disease (degeneration or herniation) on MRI does not correlate with the likelihood of chronic pain or the future need for surgery 14.
Intervertebral disc degeneration treatment
In the setting of “red-flags,” aggressive diagnosis and likely surgical options should be explored. Examples of these red flags include:
- Cauda equina syndrome (issues controlling bowel/bladder, difficulty starting urination)
- Infection (high suspicion in IV drug user, history of fever, nighttime chills)
- Tumor suspected (known history of cancer; new onset weight loss)
- Trauma (fall, assault, collision)
Fortunately, the majority of patients will improve without surgical treatment. A course of at least 6 weeks of physical therapy with an emphasis on core strengthening and stretching should be attempted. Non-surgical intervention includes modification of the activity that may exacerbate the pain, non-steroidal anti-inflammatory medications (NSAIDs), and epidural injections. Epidural injections may provide moderate, short-term relief of pain due to disc herniations; but the literature regarding the usefulness of injections for chronic non-radiating back pain is less certain. Certainly, the literate does not advocate against injections as a non-operative treatment option.
Future studies on the inhibition of molecular mediators of degeneration are promising. Similarly, while it is known that TNF-alpha is a major contributor to the degeneration and pain associated with disc disease, placebo-controlled, randomized, controlled studies with TNF-alpha inhibitors showed negative outcome in those treated patients, which shows that more research is needed to determine the best molecular strategies for treatment.
Unfortunately, many patients do not respond to conservative treatment. With a failed conservative course the patient has three options: (1) continued pain, (2) complete avoidance of activities that elicit pain, or (3) surgical intervention. Again, the surgical options for disc herniations, as well as degenerative spinal stenosis, should be reserved for those with either neurologic deficits, degenerative spondylolisthesis, or pain limiting daily functions.
One of the most cited guides on the outcomes of surgical versus conservative management for lumbar disc herniations comes from the Spine Patient Outcomes Research Trial (SPORT). In their report, patients electing for surgery had better outcomes at 3 months, years, and 4 years compared to patients who did not elect surgery. The literature regarding the optimal surgical procedure, approach, and roles for decompression/instrumentation continue to expand. Literature shows that a traditional open surgery compared to a microdiscectomy are broadly similar in outcomes and effectiveness. In regards to the amount of disc removed during a discectomy, while a “limited” discectomy provides better pain relief and patient satisfaction compared to a subtotal discectomy, they have a higher risk of repeat herniations. Patient outcomes and satisfaction are similar in repeat/revision microdiscectomies as compared to their initial discectomy. The operation, at times, requires an overnight hospitalization; but frequently these surgeries are designed to be outpatient procedures.
It is important for the patient to understand that while surgical intervention has favorable outcomes for relieving radicular pains, the results are less predictable for non-radiating lower back pain 15.
Surgical complications:
- Bleeding
- Recurrence of disease or symptoms
- Infection
- Worsening neurological deficits
- Failed operation
Postoperative and rehabilitation care:
- Ambulation and resumption of exercise is key
- Pain control
- Maintain healthy weight
In regards to microdiscectomy postoperative rehabilitation, one study showed superior results when neuromuscular exercise programs were started 2 weeks post-surgery (compared to those starting at the traditional 6-week mark). Furthermore, at 4 to 6 weeks postoperatively, evidence shows that intensive exercise programs result in the more rapid short-term improvement of function as well as a return to work when compared to mild intensity programs. Most importantly, these studies show that the more aggressive and sooner-onset therapies did not alter the rates of re-herniation or reoperation.
Intervertebral disc degeneration prognosis
The majority of patients who are treated conservatively do have a good outcome provided they change lifestyle. For those who undergo surgery, the outcomes do vary from poor to fair. In fact, poor results are universal. Many outcome studies have been misrepresented because they have been published by the surgeon or the orthopedic manufacturer or sponsorer. Long-term reduction is radicular pain is seen in some patients, but the numbers vary from 30-60%. For those who do not undertake changes in lifestyle, recurrence of symptoms is very common 16.
References- Waxenbaum JA, Futterman B. Anatomy, Back, Intervertebral Discs. [Updated 2018 Dec 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470583
- Huang YC, Hu Y, Li Z, Luk KDK. Biomaterials for intervertebral disc regeneration: Current status and looming challenges. J Tissue Eng Regen Med. 2018 Nov;12(11):2188-2202
- van Uden S, Silva-Correia J, Oliveira JM, Reis RL. Current strategies for treatment of intervertebral disc degeneration: substitution and regeneration possibilities. Biomater Res. 2017;21:22
- Waxenbaum JA, Futterman B. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Dec 6, 2018. Anatomy, Back, Cervical Vertebrae
- Ngnitewe Massa R, Mesfin FB. Herniation, Disc. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822
- Nilsson E, Brisby H, Rask K, Hammar I. Mechanical compression and nucleus pulposus application on dorsal root Ganglia differentially modify evoked neuronal activity in the thalamus. Biores Open Access. 2013 Jun;2(3):192-8
- Ab Aziz CB, Ahmad AH. The role of the thalamus in modulating pain. Malays J Med Sci. 2006 Jul;13(2):11-8
- Nedresky D, Singh G. Anatomy, Back, Nucleus Pulposus. [Updated 2018 Dec 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535373
- Donnally III CJ, Varacallo M. Lumbar Degenerative Disk Disease. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448134
- Solomou A, Kraniotis P, Rigopoulou A, Petsas T. Frequent Benign, Nontraumatic, Noninflammatory Causes of Low Back Pain in Adolescents: MRI Findings. Radiol Res Pract. 2018;2018:7638505
- Bozzio AE, Johnson CR, Fattor JA, Kleck CJ, Patel VV, Burger EL, Noshchenko A, Cain CMJ. Stand-alone Anterior Lumbar Interbody, Transforaminal Lumbar Interbody, and Anterior/Posterior Fusion: Analysis of Fusion Outcomes and Costs. Orthopedics. 2018 Sep 01;41(5):e655-e662
- Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU. Lumbar Diskography and Failed Back Syndrome in Patients Receiving Workers’ Compensation. Orthopedics. 2015 Nov;38(11):e951-8
- Yao Q, Wang S, Shin JH, Li G, Wood KB. Lumbar facet joint motion in patients with degenerative spondylolisthesis. J Spinal Disord Tech. 2013 Feb;26(1):E19-27
- Shah LM, Ross JS. Imaging of Degenerative and Infectious Conditions of the Spine. Neurosurgery. 2016 Sep;79(3):315-35
- Mostofi K, Khouzani RK. Preliminary results of lumbar disk herniation surgery by Endoscopic Destandau Method. J Clin Orthop Trauma. 2018 Mar;9(Suppl 1):S149-S151
- Malham GM, Parker RM, Blecher CM, Chow FY, Seex KA. Choice of Approach Does Not Affect Clinical and Radiologic Outcomes: A Comparative Cohort of Patients Having Anterior Lumbar Interbody Fusion and Patients Having Lateral Lumbar Interbody Fusion at 24 Months. Global Spine J. 2016 Aug;6(5):472-81