What is iron binding capacity
Total iron-binding capacity (TIBC) measures the total amount of iron that can be bound by proteins in your blood. Since transferrin is the primary iron-binding protein, the total iron-binding capacity (TIBC) test is a good indirect measurement of transferrin availability—the amount of transferrin that is available to bind to iron. Though total iron-binding capacity (TIBC) is a reflection of the amount of transferrin available, total iron-binding capacity (TIBC) and transferrin are not synonymous. In healthy individuals, transferrin is one-third saturated with iron. This means that there is about two-thirds held in reserve. In iron deficiency, all of the stored iron is used and the body tries to compensate by producing more transferrin to increase iron transport. While the serum iron level continues to decrease, the transferrin level increases. Thus, the amount of transferrin available to bind iron (TIBC) increases and the amount of transferrin saturated with iron (i.e., percent transferrin saturation) decreases.
Transferrin saturation is calculated as follows:
- Transferrin saturation calculation (%) = [Serum iron level (µg/dL)/total iron-binding capacity (TIBC) (µg/dL)] x 100
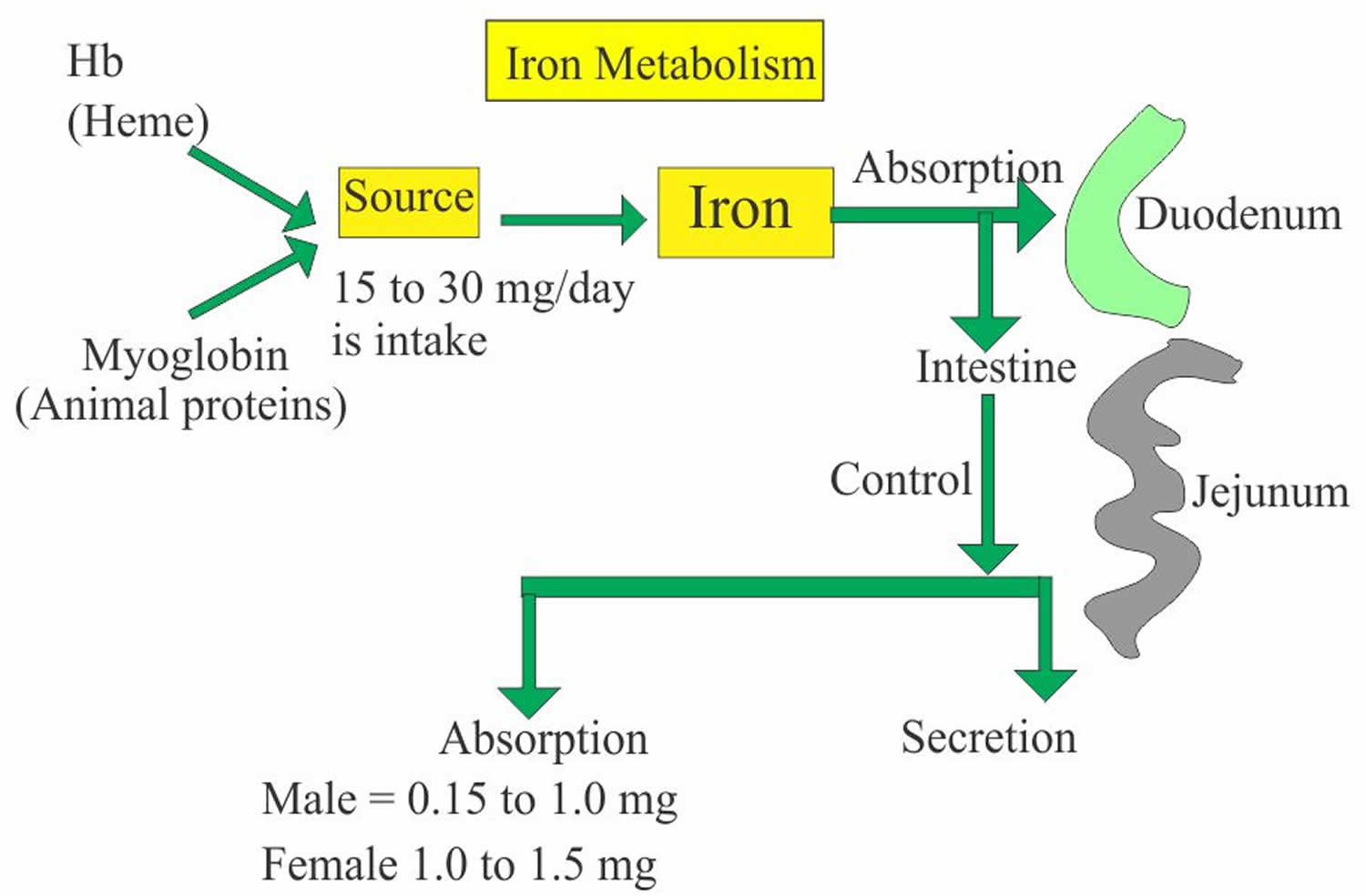
Iron is a most abundant trace element in your body and iron is an essential nutrient that, among other functions, is necessary for the production of healthy red blood cells (RBCs). Iron is a critical part of hemoglobin, the protein in red blood cells that binds oxygen in the lungs and releases oxygen as blood circulates to other parts of the body. The body cannot produce iron and must absorb it from the foods you eat or from supplements.
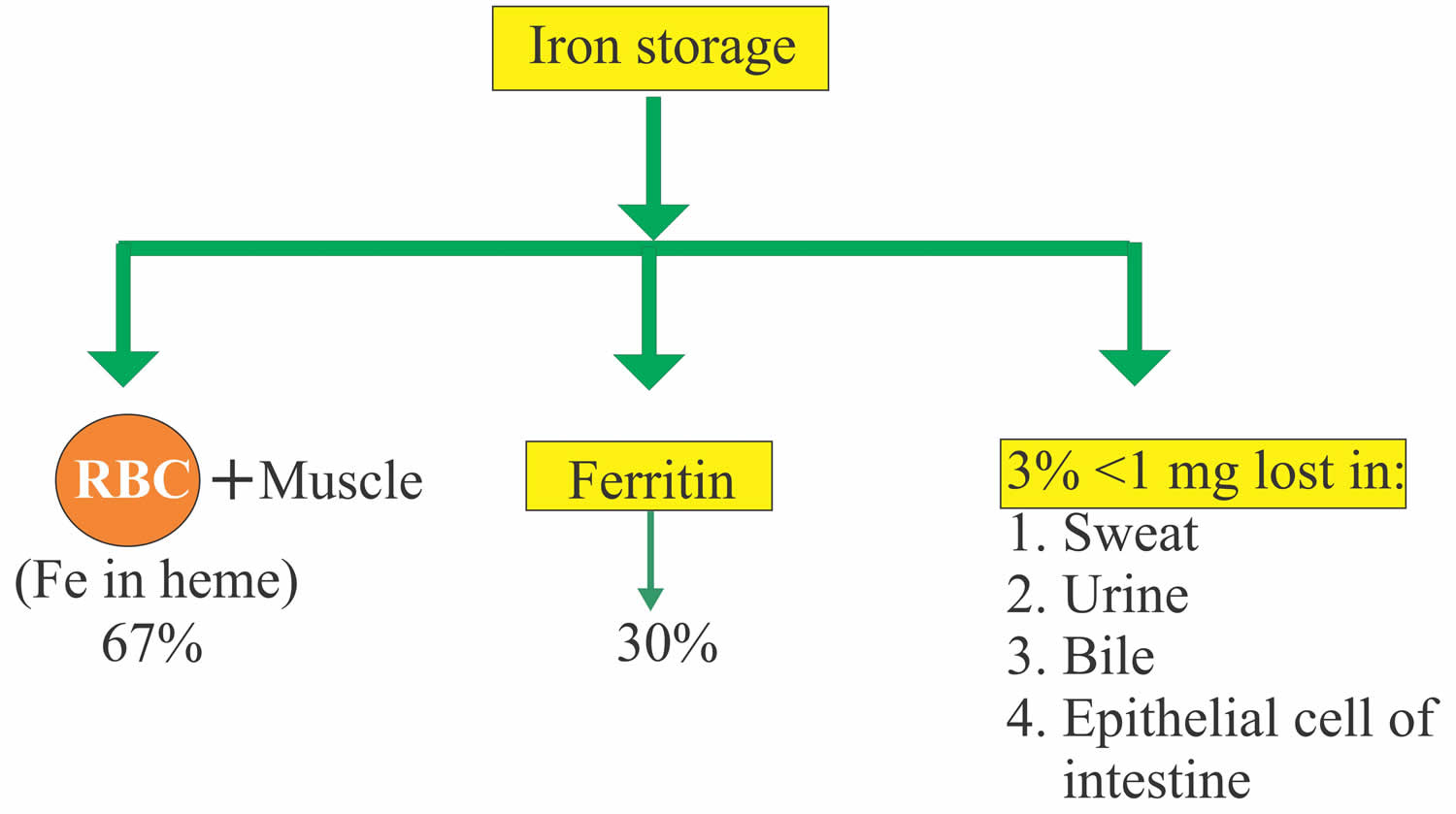
Iron in the food is absorbed by the intestinal epithelium and is temporarily stored in the mucosal cells as ferritin (Fe3+ ferric iron). Ferritin provides a soluble protein shell to encapsulate a complex of insoluble ferric hydroxide-ferric phosphate. On demand, iron is released into the blood by mechanisms that are not clearly understood, to be transported as Fe3+ (ferric iron)-transferrin. Iron is ingested as Fe3+ (ferric iron) form and is converted to Fe2+ (ferrous iron) form for the absorption. The conversion of Fe3+ (ferric iron) to Fe2+ (ferrous iron) form takes place in the stomach where gastric hydrochloric acid provides the acidity to reduce the iron. Ferric (Fe3+) iron is reduced to Ferrous (Fe2+) iron by vitamin C and this ferrous (Fe2+) iron form is absorbed very easily. Milk and antacid bind iron and reduce its absorption. Iron 1 mg/day is lost in the urine, sweat, bile and epithelial cells. In the blood, this absorbed Ferric (Fe3+) iron attaches with the transport protein (Transferrin). So transferrin may indirectly represent the total iron-binding capacity (TIBC).
Normally, iron is transported throughout the body by transferrin, the primary plasma iron transport protein, which is produced by the liver and binds iron strongly at physiological pH. In healthy people, most iron is incorporated into the hemoglobin within red blood cells. The remainder is stored in the tissues as ferritin or hemosiderin, with additional small amounts used for other purposes (e.g., to produce other proteins such as myoglobin and some enzymes). Transferrin is generally only 25% to 30% saturated with iron. The additional amount of iron that can be bound is the unsaturated iron-binding capacity (UIBC). The total iron-binding capacity (TIBC) can be indirectly determined using the sum of the serum iron and unsaturated iron-binding capacity (UIBC). Knowing the molecular weight of the transferrin and that each molecule of transferrin can bind 2 atoms of iron, total iron-binding capacity (TIBC) and transferrin concentration is interconvertible.
Transferrin saturation percentage is usually normal or decreased in persons who are iron deficient, pregnant, or are taking oral contraceptive medications. Persons with chronic inflammatory processes, hemochromatosis, or malignancies generally display low transferrin.
Transferrin is a protein that may decrease during any inflammatory process and is referred to as a negative acute phase reactant. Chronic inflammation, infections, and malignancies may cause changes in transferrin levels.
Serum iron, total iron-binding capacity, and percent saturation are widely used for the diagnosis of iron deficiency. However, serum ferritin is a much more sensitive and reliable test for demonstration of iron deficiency.
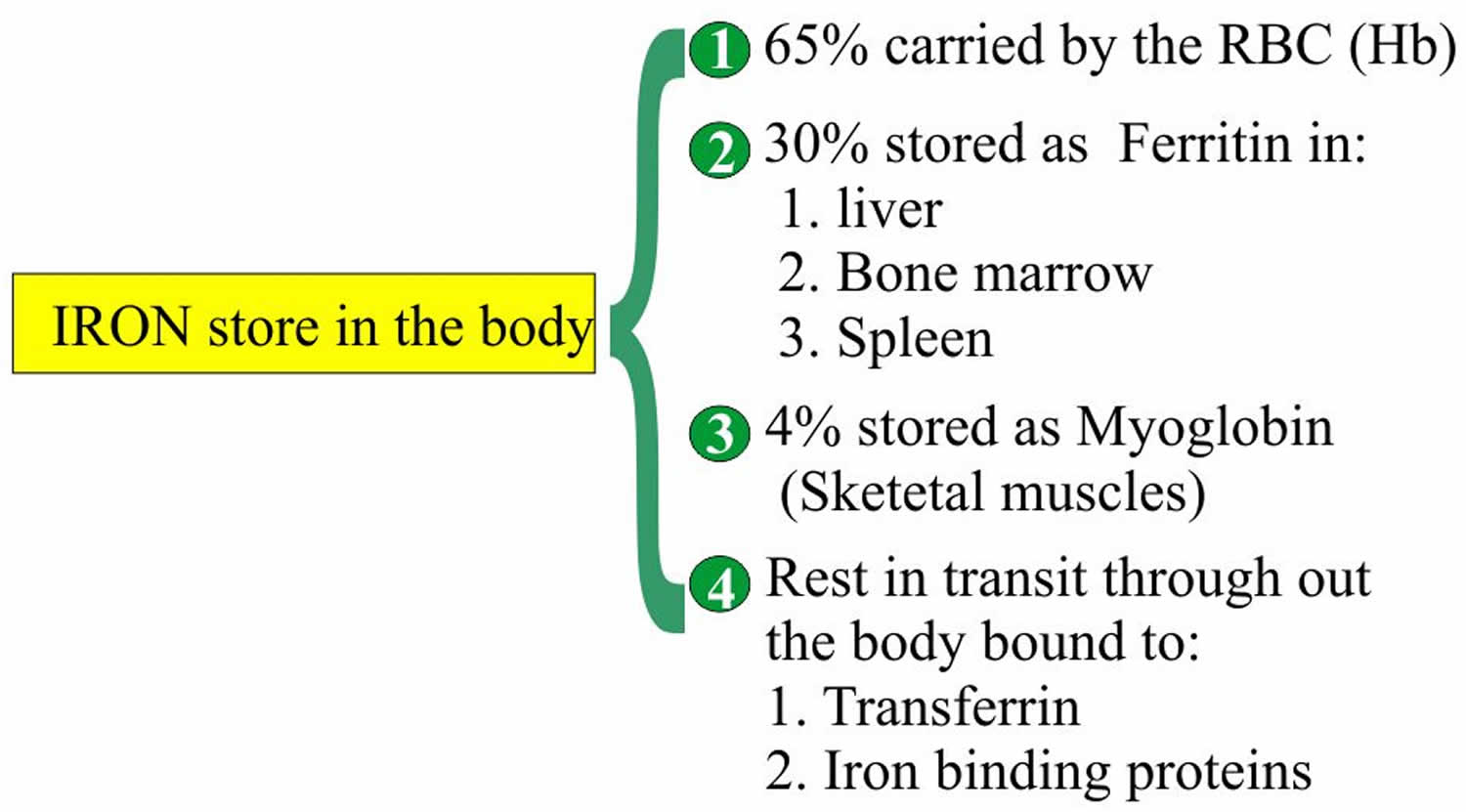
- Iron is 65% bound to Heme.
- Measurement of the iron concentration refers specifically to the Fe3+ (ferric iron) bound to the transferrin and not to the iron circulating as free hemoglobin in the blood.
- Iron is constituents of:
- Heme.
- Hemoglobin.
- Methemoglobin.
- Myoglobin.
- Several enzymes.
Total iron binding capacity (TIBC) is the capacity of transferrin to bind to iron:
- Total iron binding capacity (TIBC) is an indirect measurement of Transferrin concentration.
- TIBC measure the total amount of iron that apotransferrin has the capacity to bind.
- TIBC refer to the amount of iron that could be bound by saturation of transferrin and other minor iron-binding proteins present in the serum or plasma.
- TIBC is the sum of all protein bound to iron.
- TIBC increases in 70% of the patients with iron deficiency anemia.
- When serum iron falls then the total iron binding capacity (TIBC) increases.
- TIBC is increased in the presence of iron deficiency but may be normal or low in chronic diseases.
- TIBC may be calculated from the direct measurement of serum transferrin by the following formula:
- TIBC µg/dL = serum transferrin mg/dL x 1.25.
- Total iron binding capacity (TIBC) in Adult = 250 to 425 µg/dL (this value varies from one reference to other)
- Total iron binding capacity (TIBC) decreases in the older people around = 250 µg/dL (this value varies from one reference to other)
- TIBC µg/dL = serum transferrin mg/dL x 1.25.
- TIBC may be calculated from the direct measurement of serum transferrin by the following formula:
- A small proportion of the iron is bound to other proteins, so the above equation underestimates the total iron binding capacity (TIBC).
- The unsaturated iron-binding capacity, the amount of apotransferrin is still available to bind the iron, can be measured.
- Increased total iron binding capacity (TIBC) is seen in:
- Pregnancy.
- Iron deficiency.
- Iron deficiency anemia.
- Acute hepatitis.
- Acute and chronic blood loss.
- The decreased total iron binding capacity (TIBC) is seen in:
- Hemochromatosis.
- Hypoproteinemia in malabsorption.
- Burns.
- Cirrhosis.
- Renal diseases like nephrosis etc.
- Thalassemia.
- Hyperthyroidism.
- Chronic diseases.
- Non-iron deficiency anemia. Anemia due to red blood cells being destroyed too quickly (hemolytic anemia).
- Decrease in red blood cells from the intestines not properly absorbing vitamin B12 (pernicious anemia)
- Sickle cell anemia
- Inflammation.
Ferritin represents stored iron.
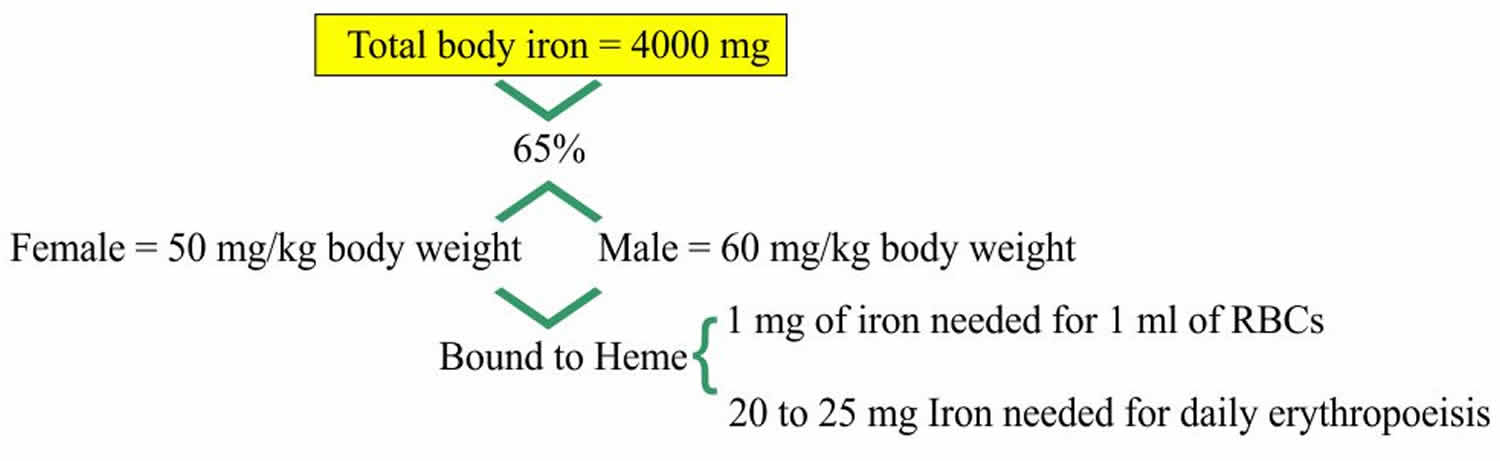
- 10 to 20% to 30% of the total iron is stored as Ferritin.
- Ferritin Adult male = 12 to 300 ng/mL (12 to 300 µg/L).
- Ferritin Adult female = 10 to 150 ng/mL (10 to 150 µg/L).
- Ferritin Children
- Newborn = 25 to 200 ng/mL.
- One month old = 200 to 600 ng/mL.
- 2 to 5 months old = 50 to 200 ng/mL.
- 6 months = 7 to 142 ng/mL.
- Iron is stored as ferritin in the body in liver, spleen and bone marrow.
- Or stored as Ferric (Fe3+) iron bound to an apoferritin protein molecule.
- When iron is needed then it is released from the Ferritin and is then bound to β1 globulin molecule, transferrin.
- Serum Ferritin is the best diagnostic test for the iron deficiency anemia.
- Because ferritin is the measure of the iron stores in the body.
- In an iron deficiency anemia, the ferritin level is <15 µg/L as compared to the normal level of 20 to 250 µg/L.
- In children <6 µg/L compared to the normal value of 7 to140 µg/L.
- In baby <12 µg/L compared to the normal values of 50 to 200 µg/L.
- Ferritin is the acute phase protein, so its value may increase in infections, systemic lupus erythematosus (SLE), liver diseases, malignancies, and chronic renal failure.
Transferrin represents the major protein which binds to iron. Majority of the iron is bound to transferrin.
- Transferrin is a beta-globulin (β1-globulin).
- Transferrin capacity to bind iron in normal plasma is 240 to 360 µg/dL.
- Transferrin also acts as an acute phase protein.
- This is a transport protein synthesized in the liver.
- This regulates iron absorption.
- Transferrin also called siderophilin.
- Total iron + total iron binding capacity (TIBC) + Transferrin when done together help in the differential diagnosis of anemia.
- The cellular uptake of iron is mediated by the cell surface transferrin receptor.
- The number of transferrin receptors depends upon the needs of the cell for the iron.
- In the case of apoferritin deficiency, an excess of the iron is deposited as small granules as Iron-oxide, called hemosiderin.
Transferrin saturation is the percentage of transferrin and other iron binding proteins.
- Transferrin saturation is calculated as follows.
- Transferrin saturation calculation (%) = [Serum iron level (µg/dL)/total iron-binding capacity (TIBC) (µg/dL)] x 100
- Normal value for transferrin saturation is 20 to 50%. This may vary with age and sex.
- Male transferrin saturation = 20 to 50 %.
- Female transferrin saturation = 15 to 50 %.
- Transferrin saturation is helpful to find the cause of abnormal iron and total iron binding capacity (TIBC) level.
- Transferrin saturation is decreased below 15% in a patient with iron deficiency anemia.
- Transferrin saturation is increased in patients:
- Hemolytic anemia.
- Sideroblastic anemia.
- Megaloblastic anemia.
- Patient with iron overload or iron poisoning.
- Hemochromatosis.
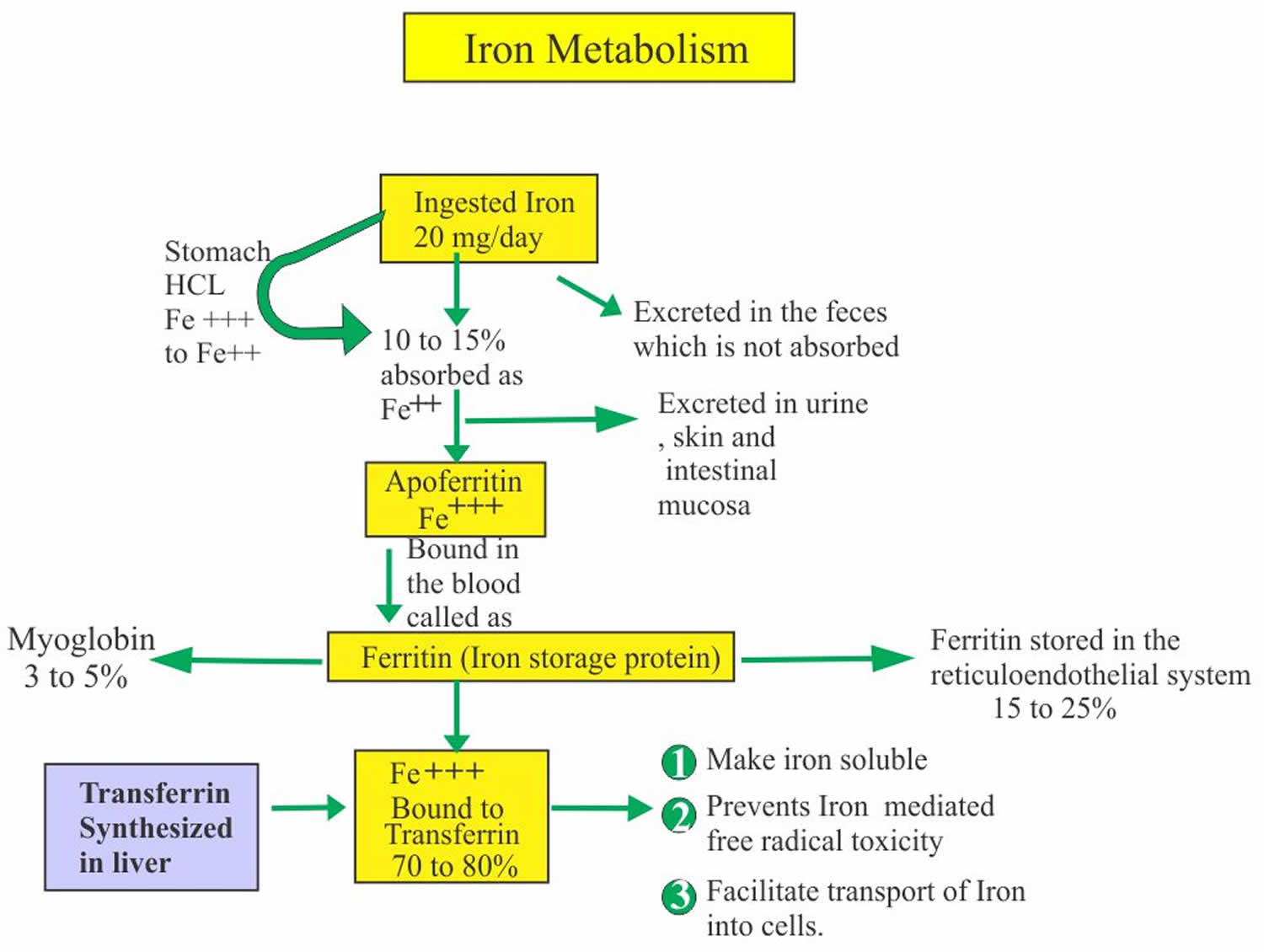
Figure 1. Iron storage in the body
Figure 2. Ferritin iron storage
Figure 3. Iron absorption and excretion
Figure 4. Iron metabolism
Total iron binding capacity test
Total iron-binding capacity (TIBC), unsaturated iron binding capacity (UIBC), transferrin test and transferrin saturation, along with other iron tests, help to evaluate the amount of iron circulating in your blood, the total capacity of your blood to transport iron, and the amount of stored iron in your body. These tests are often ordered at the same time and the results interpreted together to help diagnose and/or monitor iron deficiency, iron deficiency anemia or too much iron in the body (iron overload). Testing may also help differentiate various causes of anemia.
- Serum iron test—measures the total amount of iron in the liquid portion of the blood, nearly all of which is bound to transferrin.
- Transferrin test—directly measures the level of transferrin in the blood. The level depends upon liver function and a person’s nutritional status. Transferrin is a protein that may decrease during any inflammatory process and is referred to as a negative acute phase reactant.
- TIBC (total iron-binding capacity)—measures the total amount of iron that can be bound by proteins in the blood. Since transferrin is the primary iron-binding protein, the total iron-binding capacity (TIBC) test is a good indirect measurement of transferrin availability—the amount of transferrin that is available to bind to iron. Note: Though total iron-binding capacity (TIBC) is a reflection of the amount of transferrin available, total iron-binding capacity (TIBC) and transferrin are not synonymous.
- UIBC (unsaturated iron-binding capacity)—Unsaturated iron binding capacity (UIBC) test determines the reserve capacity of transferrin, i.e., the portion of transferrin that has not yet been saturated with iron.
- Transferrin saturation— dividing the iron concentration by the total iron-binding capacity (TIBC) produces an estimate of how many of transferrin iron-binding sites are occupied; this is called the transferrin saturation. Under normal conditions, transferrin is typically one-third saturated with iron. This means that about two-thirds of its capacity is held in reserve. Less commonly, the iron concentration may be divided by the transferrin concentration, not the total iron-binding capacity (TIBC). This similar estimate is usually called the transferrin index.
- Ferritin—measures the level of ferritin, a protein made by almost all cells in response to increased iron. The ferritin level reflects the total body iron. It will be low when there is iron deficiency and high when there is an excess of iron in the body.
When the level of iron is insufficient to meet the body’s needs, the level of iron in the blood drops and iron stores are depleted. This may occur because:
- There is an increased need for iron, for example during pregnancy or childhood, or due to a condition that causes chronic blood loss (e.g., peptic ulcer, colon cancer)
- Not enough iron is consumed (either foods or supplements)
- The body is unable to absorb iron from the foods eaten in conditions such as celiac disease
Insufficient levels of circulating and stored iron may eventually lead to iron deficiency anemia (decreased hemoglobin and hematocrit, smaller and paler red cells). In the early stage of iron deficiency, no physical effects are usually seen and the amount of iron stored may be significantly depleted before any signs or symptoms of iron deficiency develop. If a person is otherwise healthy and anemia develops over a long period of time, symptoms may not appear before the hemoglobin in the blood drops below the lower limit of normal.
However, as the iron deficiency progresses, symptoms eventually begin to appear. The most common symptoms of anemia include fatigue, weakness, dizziness, headaches and pale skin.
Conversely, too much iron can be toxic to the body. Iron storage and ferritin levels increase when more iron is absorbed than the body needs. Absorbing too much iron over time can lead to the progressive buildup of iron compounds in organs and may eventually cause their dysfunction and failure. An example of this is hemochromatosis, a rare genetic disease in which the body absorbs and builds up too much iron, even on a normal diet. Additionally, iron overload can occur when a person undergoes repeated blood transfusions.
When is total iron binding capacity test ordered?
Total iron-binding capacity (TIBC), unsaturated iron binding capacity (UIBC), transferrin test and transferrin saturation test may be ordered along with other iron tests when results from a routine complete blood count (CBC) show that a person’s hemoglobin and hematocrit are low and their red blood cells are smaller and paler than normal (microcytic and hypochromic), suggesting iron deficiency anemia even though other clinical symptoms may not have developed yet.
Iron tests may be ordered when a person develops signs and symptoms of anemia such as:
- Chronic fatigue/tiredness
- Dizziness
- Weakness
- Headaches
- Pale skin (pallor)
Testing may be ordered when iron overload is suspected. Signs and symptoms of iron overload will vary from person to person and tend to worsen over time. They are due to iron accumulation in the blood and tissues. These may include:
- Joint pain
- Fatigue, weakness
- Weight loss
- Lack of energy
- Abdominal pain
- Loss of sex drive
- Organ damage, such as in the heart and/or liver
Testing is also ordered when there is a case of suspected iron poisoning. This is most common in children who accidentally overdose with vitamins or other supplements containing iron.
What does the total iron binding capacity test results mean?
The results of total iron-binding capacity (TIBC), unsaturated iron binding capacity (UIBC) and transferrin tests are usually evaluated in conjunction with other iron tests.
Recent blood transfusions can affect test results as can iron injections or transfused iron. Multiple blood transfusions can sometimes lead to iron overload.
A high total iron-binding capacity (TIBC), unsaturated iron binding capacity (UIBC) or transferrin usually indicates iron deficiency, but they are also increased in pregnancy and with the use of oral contraceptives.
A low total iron-binding capacity (TIBC), unsaturated iron binding capacity (UIBC) or transferrin may also occur if someone has malnutrition, inflammation, liver disease, or nephrotic syndrome. However, the tests are usually not used to assess these conditions.
A summary of the changes in iron tests seen in various diseases of iron status is shown in the table below.
| Disease | Iron | Total iron-binding capacity (TIBC)/Transferrin | Unsaturated iron binding capacity (UIBC) | %Transferrin Saturation | Ferritin |
| Iron Deficiency | Low | High | High | Low | Low |
| Hemochromatosis/Hemosiderosis | High | Low | Low | High | High |
| Chronic Illness | Low | Low/Normal | Low/Normal | Low/Normal | High/Normal |
| Hemolytic Anemia | High | Normal/Low | Low/Normal | High | High |
| Sideroblastic Anemia | Normal/High | Normal/Low | Low/Normal | High | High |
| Iron Poisoning | High | Normal | Low | High | Normal |
Iron deficiency
The early stage of iron deficiency is the slow depletion of iron stores. This means there is still enough iron to make red cells but the stores are being used up without adequate replacement. The serum iron level may be normal in this stage, but the ferritin level will be low.
As iron deficiency continues, all of the stored iron is used and the body tries to compensate by producing more transferrin to increase iron transport. The serum iron level continues to decrease and transferrin and total iron-binding capacity (TIBC) and unsaturated iron binding capacity (UIBC) increase. As this stage progresses, fewer and smaller red blood cells are produced, eventually resulting in iron deficiency anemia. Transferrin saturation is decreased with iron deficiency.
Iron overload
If the iron level and transferrin saturation are high, the total iron-binding capacity (TIBC), unsaturated iron binding capacity (UIBC) and ferritin are normal and the person has a clinical history consistent with iron overdose, then it is likely that the person has iron poisoning. Iron poisoning occurs when a large dose of iron is taken all at once (acute) or over a long period of time (chronic). Iron poisoning in children is almost always acute, occurring in children who ingest their parents’ iron supplements. In some cases, acute iron poisoning can be fatal.
A person who has mutations in the HFE gene is diagnosed with hereditary hemochromatosis. However, while many people who have hemochromatosis will have no symptoms for their entire life, others will start to develop symptoms such as joint pain, abdominal pain, and weakness in their 30’s or 40’s. Men are affected more often than women because women lose blood during their reproductive years through menstruation.
Iron overload may also occur in people who have hemosiderosis and in those who have had repeated transfusions. This may occur with sickle cell anemia, thalassemia major, or other forms of anemia. The iron from each transfused unit of blood stays in the body, eventually causing a large buildup in the tissues. Some persons with alcoholism and with chronic liver disease also develop iron overload.
Are there other things that cause anemia besides iron deficiency?
Yes, there are numerous causes of anemia. However, iron deficiency is one of the most common. If iron tests rule out iron deficiency, another source for the anemia must be found.
High total iron binding capacity
Elevated total iron binding capacity (TIBC) is seen in:
- Pregnancy.
- Iron deficiency.
- Iron deficiency anemia
- Acute hepatitis.
- Acute and chronic blood loss.
Low total iron binding capacity
Low total iron binding capacity (TIBC) is seen in:
- Hemochromatosis.
- Lower-than-normal level of protein in the blood (hypoproteinemia) due to malabsorption.
- Malnutrition.
- Burns.
- Cirrhosis.
- Renal diseases like nephrosis etc.
- Thalassemia.
- Hyperthyroidism.
- Chronic diseases.
- Non-iron deficiency anemia. Anemia due to red blood cells being destroyed too quickly (hemolytic anemia).
- Decrease in red blood cells from the intestines not properly absorbing vitamin B12 (pernicious anemia)
- Sickle cell anemia
- Inflammation.