What is lamellar ichthyosis
Lamellar ichthyosis is a very rare autosomal recessive skin disease. Lamellar ichthyosis is a sub-type of non-bullous congenital ichthyosis. Lamellar ichthyosis appears at birth and continues throughout life. In lamellar ichthyosis, the skin cells are produced at a normal rate, but they do not separate normally at the surface of the outermost layer of skin (stratum corneum) and are not shed as quickly as they should be. The result of this retention is the formation of scale.
Infants with lamellar ichthyosis are typically born with a tight, clear sheath covering their skin called a collodion membrane. This membrane usually dries and peels off during the first few weeks of life, and then it becomes obvious that affected babies have scaly skin, and eyelids and lips that are turned outward. People with lamellar ichthyosis typically have large, dark, plate-like scales covering their skin on most of their body. Infants with lamellar ichthyosis may develop infections, an excessive loss of fluids (dehydration), and respiratory problems. Affected individuals may also have hair loss (alopecia), abnormally formed fingernails and toenails (nail dystrophy), a decreased ability to sweat (hypohidrosis), an increased sensitivity to heat, and a thickening of the skin on the palms of the hands and soles of the feet (keratoderma). Less frequently, affected individuals have reddened skin (erythema) and joint deformities (contractures).
Lamellar ichthyosis is a very rare disorder occurring in less than one in 200,000 people 1. Lamellar ichthyosis is more common in Norway, where an estimated 1 in 91,000 individuals are affected 2. Lamellar ichthyosis is not limited by gender, race or ethnicity; it occurs in all populations.
Figure 1. Lamellar ichthyosis baby
Lamellar ichthyosis causes
Lamellar ichthyosis may be caused by mutations affecting several different genes (ABCA12, ALOXE3, ALOX12B, CERS3, CYP4F22, NIPAL4/ICHTHYIN, PNPLA1, and TGM1 gene). Three of these genes have been identified; they are the gene encoding the epidermal enzyme Transglutaminase 1 (TGM1 gene) and two genes (ABCA12) encoding two distinct but related enzymes, 12(R)-lipoxygenase and lipoxygenase-3. There is also evidence for more genes that are yet to be identified. Mutations in the TGM1 gene are responsible for approximately 90 percent of cases of lamellar ichthyosis. The TGM1 gene provides instructions for making an enzyme called transglutaminase 1. Transglutaminase 1 is an important enzyme responsible for cross-linking epidermal proteins during the formation and maturation of the stratum corneum (outermost layer of the skin), which is a structure that surrounds skin cells and helps form a protective barrier between the body and its environment. The skin abnormalities associated with lamellar ichthyosis disrupt the normal formation of the epidermis, resulting in impaired regulation of body temperature, water retention, and resistance to infections.
Mutations in other genes associated with lamellar ichthyosis are each responsible for only a small percentage of cases. In some people with lamellar ichthyosis, the cause of the disorder is unknown. Researchers have identified multiple chromosome regions that contain genes that may be associated with lamellar ichthyosis, although the specific genes have not been identified.
Lamellar ichthyosis inheritance pattern
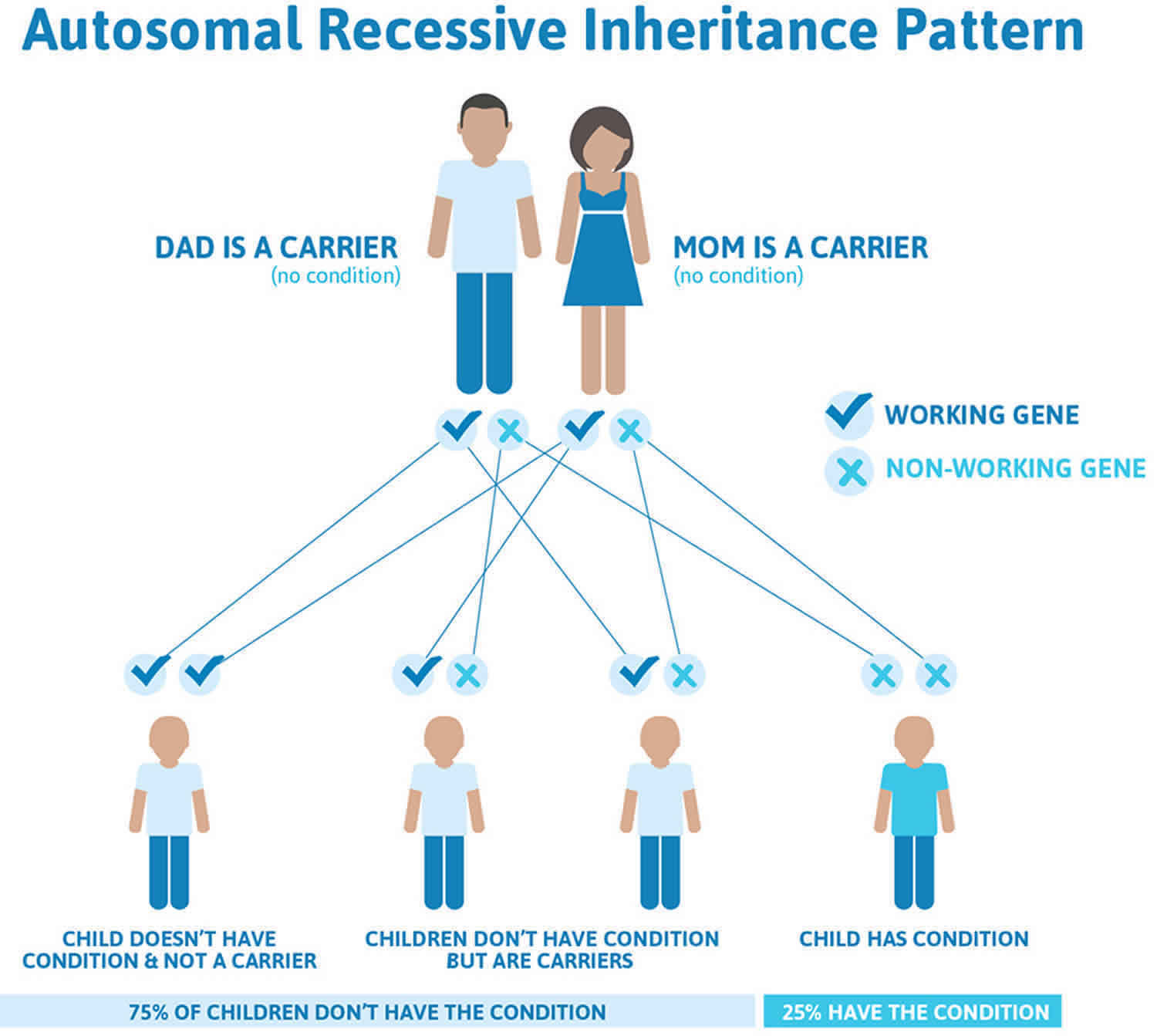
This condition is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figure 2 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 2. Lamellar ichthyosis autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Lamellar ichthyosis symptoms
Lamellar ichthyosis is present at birth with many babies with lamellar ichthyosis are born with a clear, shiny, waxy layer of skin. Many babies born with lamellar ichthyosis are born as “collodion babies”, so called because they are covered with a clear membrane called collodion membrane. The membrane sheds within the first 2 weeks of life. The skin underneath the membrane is red and scaly. It resembles the surface of a fish. Sometimes described as having a shellacked appearance, these newborns have skin that can be red or dark, tight and split. Often the eyelids and lips are forced open by the tightness of the skin, and there may be contractures around the fingers. Problems with temperature regulation, water loss, secondary infections, and systemic infection can occur in the newborn with lamellar ichthyosis.
The collodion membrane is shed a few days to a few weeks after birth, leaving the newborn covered with broad, dark, plate-like scales separated by fissures that may be superficial or deep. People with lamellar ichthyosis often have trouble closing their eyes completely because of the tightness of the skin around the eyes and eyelids. In some cases, the skin around the eyes pulls so tightly it causes they eyelids to turn outward exposing the inner red lid and causing continuous irritation. This condition is called ectropion. Some physicians recommend plastic surgery to correct it because if left untreated, damage to the cornea can develop leading to impaired vision. People with lamellar ichthyosis may also have thickened nails and hair loss due to the thickness of the scales on their scalp. They may also have reddened skin (erythroderma), thickened skin on the palms of the hands and soles of the feet, and decreased sweating with heat intolerance.
With lamellar ichthyosis, the outer layer of skin called the epidermis is not normal and cannot protect the body like the healthy epidermis can. As a result, a baby with lamellar ichthyosis may have the following health problems:
- Difficulty in feeding
- Loss of fluid dehydration
- Loss of balance of minerals in the body (electrolyte imbalance)
- Breathing problems
- Body temperature that is not stable
- Skin or body-wide infections
Older children and adults with lamellar ichthyosis may have these symptoms:
- Very large scales that cover most of the body
- Decreased ability to sweat causing sensitivity to heat
- Hair loss
- Abnormal finger and toenails
- Skin of the palms and soles is thickened.
Lamellar ichthyosis diagnosis
There is currently no diagnostic test for amellar ichthyosis, it is generally determined by the presence of the collodion membrane or collodion baby.
Doctors frequently use genetic testing to help define which ichthyosis a person actually has. This may help them to treat and manage the patient. Another reason to have a genetic test is if you or a family member wants to have children. Genetic testing, which would ideally be performed first on the person with ichthyosis, is often helpful in determining a person’s, and their relative’s, chances to have a baby with ichthyosis. Genetic testing may be recommended if the inheritance pattern is unclear or if you or a family member is interested in reproductive options such as genetic diagnosis before implantation or prenatal diagnosis.
Results of genetic tests, even when they identify a specific mutation, can rarely tell how mild or how severe a condition will be in any particular individual. There may be a general presentation in a family or consistent findings for a particular diagnosis, but it’s important to know that every individual is different. The result of a genetic test may be “negative,” meaning no mutation was identified. This may help the doctor exclude certain diagnoses, although sometimes it can be unsatisfying to the patient. “Inconclusive” results occur occasionally, and this reflects the limitation in our knowledge and techniques for doing the test. But we can be optimistic about understanding more in the future, as science moves quickly and new discoveries are being made all the time.
Lamellar ichthyosis treatment
Collodion babies usually need to stay in the neonatal intensive care unit (NICU). They are placed in a high-humidity incubator. They will need extra feedings. Moisturizers need to be applied to the skin. After the collodion membrane is shed, babies can usually go home.
Lifelong care of the skin involves keeping the skin moist to minimize the thickness of the scales. Measures include:
- Moisturizers applied to the skin
- Medicines called retinoids that are taken by mouth in severe cases
- High-humidity environment
- Bathing to loosen scales
Lamellar ichthyosis is treated topically with skin barrier repair formulas containing ceramides or cholesterol, moisturizers with petrolatum or lanolin, and mild keratolytics (products containing alpha-hydroxy acids.. Severe lamellar ichthyosis can be treated systemically with oral synthetic retinoids. Retinoids are only used in severe cases of lamellar ichthyosis due to their known bone toxicity and other complications.
Lamellar ichthyosis prognosis
Patients with lamellar ichthyosis have normal life spans.
In the neonatal period, following the shedding of the collodion membrane, the newborn is at risk for secondary sepsis and hypernatremic dehydration.
As the child ages, the hyperkeratosis can interfere with normal sweat gland function, which can predispose to heat intolerance and possible heat shock. Ectropion may result in the inability to fully close the eyelids and can cause exposure keratitis.
External auditory canal stenosis and tympanic membrane blunting may result in a conductive hearing loss. Osseointegrated hearing devices may effectively bypass this hearing defect.
Less common associations include orthopedic abnormalities such as genu valgum, other ocular problems such as corneal perforation, and rickets 3.
Like other ichthyoses, lamellar ichthyosis may be especially prone to widespread, severe, and chronic Trichophyton rubrum infections and viral infections 4.
References- Lamellar ichthyosis. https://rarediseases.org/rare-diseases/ichthyosis-lamellar/
- Lamellar ichthyosis. https://ghr.nlm.nih.gov/condition/lamellar-ichthyosis
- Angmo D, Patil B, Agarwal R, Mohanty K, Singh A. A Unique Case of JOAG With Lamellar Ichthyosis With Rickets: A Case Report and Review of the Literature. J Glaucoma. 2016 Mar. 25 (3):e280-3.
- Damsky WE, Leventhal JS, Khalil D, Vesely MD, Craiglow BG, Milstone LM, et al. Recurrent Coxsackievirus Infection in a Patient with Lamellar Ichthyosis. Pediatr Dermatol. 2016 Mar-Apr. 33 (2):e140-2