What is leukotriene
Leukotrienes are a group of potent inflammatory mediators that belong to the eicosanoid family 1. Leukotrienes were initially identified in the 1970s, and the biosynthetic pathways involved in leukotriene formation were elucidated around the same time 2. Leukotrienes synthesis, primarily by leukocytes, is spurred by a variety of immunologic and nonimmunologic stimuli including antigens, immune complexes, complement, cytokines, osmotic challenges, and pollutants among others. Leukotriene molecules collectively serve a variety of purposes aimed at furthering the inflammatory cascade via alterations in vascular permeability, effects on leukocytes, and constriction of smooth muscle. Most notably, the bronchoconstriction that results from the action of leukotrienes plays an important role in the pathophysiology of asthma 3. Leukotrienes have also been shown to be upregulated in several other diseases, including aspirin-exacerbated respiratory disease 4, allergic rhinitis 5, inflammatory bowel disease 6, and acute respiratory distress syndrome (ARDS) 7. This creates opportunity in the utilization of targeted pharmacotherapy to treat asthma and similar diseases 8. Several leukotriene receptors (B leukotriene receptor 1 and 2 [BLT1 and BLT2], and type 1 and type 2 cysteinyl leukotriene receptor [CysLT1, CysLT2]) have also been discovered and small molecules were developed that inhibited leukotriene synthesis either by targeting 5-lipoxygenase, 5-lipoxygenase activating protein (FLAP), cytosolic phospholipase A2 (cPLA2), or molecules, such as leukotriene receptor antagonists, that interfere with the ability of leukotrienes to mediate their effects 9.
However, with rare exceptions, such as aspirin-exacerbated respiratory disease 10, leukotriene modifiers have shown only a modest beneficial effect on diseases in which leukotrienes would be expected to play an important role 9. Several explanations, including differences in leukotriene levels in individual patients, the heterogeneity of disease phenotypes, and differences in drug pharmacokinetics, pharmacodynamics, and pharmacogenomics, have been proposed for why targeting leukotrienes does not benefit leukotriene-related diseases 11; however, there has not been a clear explanation for why antileukotriene drugs have not worked as expected 9. There are noted differences in the incidence of leukotriene-mediated diseases in males and females, but sex as a factor in the response to leukotriene inhibitors has not been fully explored 9.
One possible explanation comes from the study of diseases associated with elevated leukotriene levels and the response of these conditions to antileukotriene drugs. Several of these diseases have a female predominance and have been associated with sex hormone levels (e.g., asthma in adults, aspirin-exacerbated respiratory disease) 12. Based on these data, it is possible that leukotriene modifiers would have a greater effect in those with the highest leukotriene levels. In this issue, Pace and colleagues 13 build on their previous work and address a potential mechanism that may be responsible for the relatively limited response to leukotriene modifiers in several disease states. Pace et al. 13 exposed male and female mice and rats as well as peripheral blood cells from male and female human volunteers to inflammatory stimuli and administered different leukotriene synthesis inhibitors. The results from this study confirmed their previous findings that there are sex-dependent differences in leukotriene biosynthesis and the effects of leukotriene modifiers and that these differences are mediated at least in part by androgens 14. Pace and colleagues also note that females are more likely than males to have 5-lipoxygenase/5-lipoxygenase activating protein (FLAP) complex assembly at the nuclear membrane, the site where this complex mediates its effects. Additionally, androgens inhibited the tight assembly, and drugs that directly interfered with 5-lipoxygenase activating protein (FLAP) and 5-lipoxygenase/5-lipoxygenase activating protein (FLAP) assembly were most likely to result in a sex-specific effect. One area that Pace and colleagues 13 did not explore is how androgens may alter the interaction between 5-lipoxygenase and 5-lipoxygenase activating protein (FLAP). Nonetheless, their experiments highlight the complexity of trying to understand the role of sex in the differences in leukotriene synthesis and response to leukotriene-targeting drugs, as the results were influenced by the specific stimulus and model system, the type of inflammatory cell (human peripheral blood neutrophils and monocytes and mouse and rat peritoneal macrophages), and the leukotriene modifier selected. Even the use of structurally dissimilar 5-lipoxygenase inhibitors showed different effects.
Leukotriene synthesis
The synthesis of leukotrienes primarily occurs in leukocytes 1. Different leukocytes tend to predominantly produce a specific leukotriene, either leukotriene B4 or the cysteinyl class of leukotrienes called cysteinyl-leukotrienes (i.e., leukotriene C4, leukotriene D4 and leukotriene E4) 2. Neutrophils are the primary synthesizers of leukotriene B4 and produce little of the cysteinyl leukotrienes. Eosinophils, basophils, and mast cells are the primary producers of the cysteinyl leukotrienes and have minimal capacity to produce leukotriene B4. Macrophages and monocytes serve as intermediaries, having adequate capacity to produce both leukotriene B4 and the cysteinyl leukotrienes. Other cells typically do not produce significant levels of leukotrienes as they often do not express 5-lipoxygenase or 5-lipoxygenase activating protein (FLAP). However, it is possible for cells to take up leukotriene A produced by leukocytes and then synthesize bioactive leukotrienes if they express more distal enzymes in the metabolic pathway. This process has been termed “transcellular biosynthesis” 8.
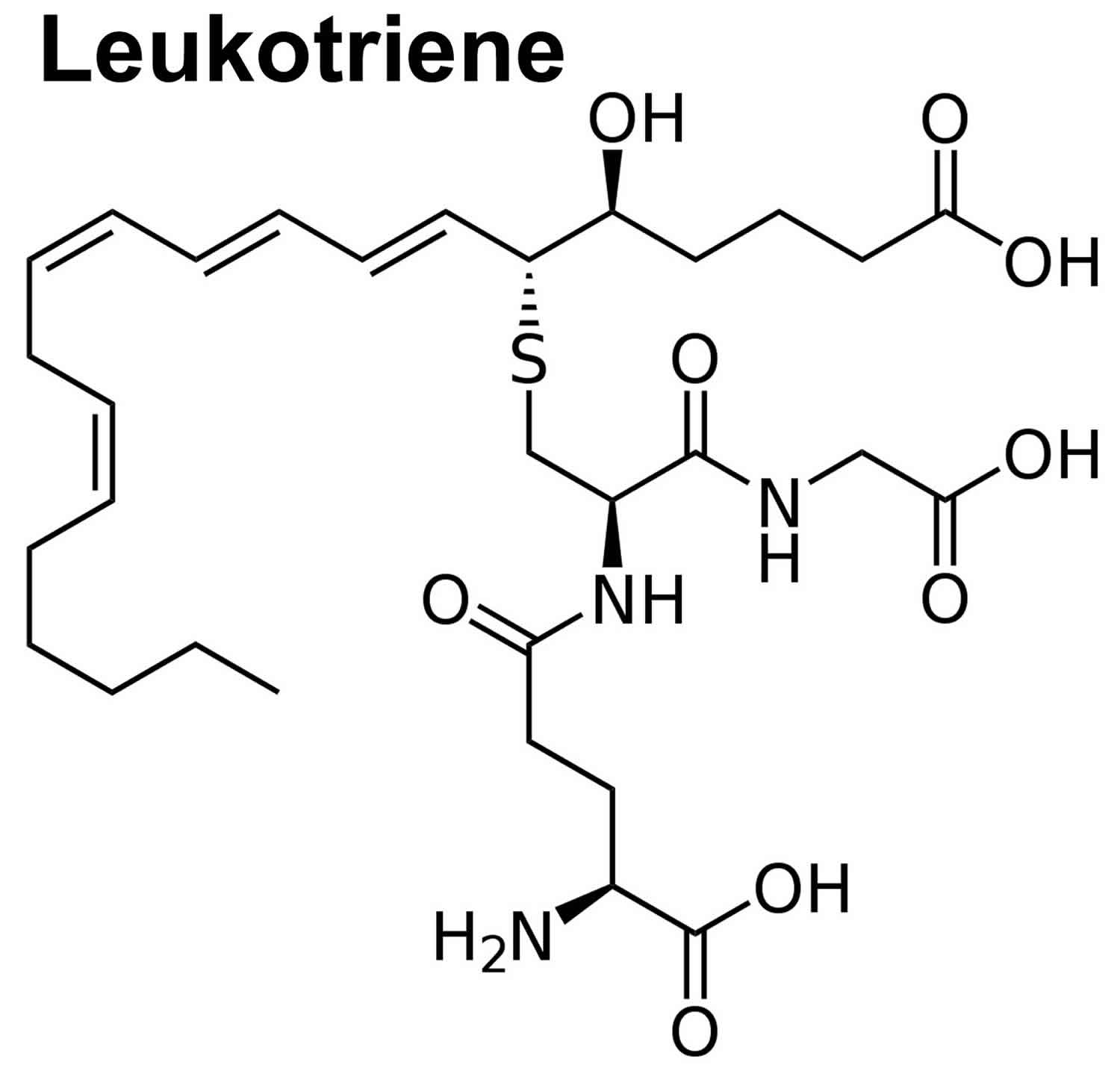
Leukotrienes are synthesized via the 5-lipoxygenase pathway of arachidonic acid metabolism (see Figure 1). Arachidonic acid is a fatty acid found within the phospholipids that constitute cell membranes. When a stimulus arrives that calls for the production of leukotrienes, phospholipid within our cell membranes is metabolized to arachidonic acid via phospholipase A. The arachidonic acid is then acted on by 5-lipooxygenase in concert with 5-lipoxygenase activating protein (FLAP) to yield leukotriene A. Within the cell, leukotriene A is used as the substrate for production of leukotriene B via hydrolysis or leukotriene C via conjugation with glutathione. At this point, leukotriene B and leukotriene C are exported out of the cell via separate transport proteins. Extracellularly, leukotriene C can be subsequently hydrolyzed to produce leukotriene E. Leukotriene C, leukotriene D (an intermediate in leukotriene E synthesis), and leukotriene E are termed cysteinyl leukotrienes 8.
Figure 1. Leukotriene synthesis
[Source 2 ]Leukotriene function
Leukotrienes are proinflammatory lipid mediators that have been shown to be upregulated in several diseases, including asthma, allergic rhinitis, aspirin-exacerbated respiratory disease, inflammatory bowel disease, and acute respiratory distress syndrome (ARDS).
Leukotrienes exert their effects by binding receptors in an autocrine or paracrine fashion. These receptors are G protein-coupled receptors that, once bound, activate a G protein. Leukotriene receptors either activate the Gq protein, which leads to increases in intracellular calcium, or the Gi protein, which leads to decreases in the intracellular cAMP. Either of these G proteins then signals a cascade of kinase reactions, leading to changes in both transcriptional activity and cellular motility.
The different types of leukotrienes exert both common and distinctive effects. In general, leukotriene B and the cysteinyl-leukotrienes (i.e., leukotriene C4, leukotriene D4 and leukotriene E4) exert different effects by separate binding classes of receptors. Leukotriene B binds to B leukotriene receptor 1 and 2 [BLT1 and BLT2] respectively. Leukotriene B most notably acts as a potent neutrophil chemotactic receptor. This action emphasizes the inflammatory propellant nature of leukotrienes as neutrophils are the primary produces of leukotriene B as well. The cysteinyl leukotrienes bind to type 1 and type 2 cysteinyl leukotriene receptor (CysLT1 and CysLT2) respectively). CysLT1 primarily mediates airway changes including bronchoconstriction, airway edema, and mucus secretion. cysLT2, on the other hand, is principally an inflammatory stimulator as it evokes increases in vascular permeability and tissue fibrosis but has little effect on the airways. It is worth noting that leukotriene mediated increases in vascular permeability are 3 to 4 times more potent than histamine 15.
Collectively, the different types of leukotrienes also exert common effects. Leukotrienes promote the movement of almost all leukocyte types into tissues and amplify the effects of type 2 T helper cells. Additionally, it has been proposed that leukotrienes also exert a negative inotropic effect on the heart, stimulate prostaglandin synthesis in macrophages, and induce gastrointestinal smooth muscle constriction.
Leukotriene asthma
Leukotrienes have been revealed to play a crucial role in several diseases, most notably asthma. Leukotrienes have a number of effects that lead to the production of asthma symptoms. First, they promote bronchiole constriction leading to narrowing of the airways. In regards to this, they also promote smooth muscle proliferation, leading to increased responsiveness in airway constriction. Second, they promote leukocyte recruitment and subsequent cytokine release, leading to further inflammation of the airways. Third, they act directly on airway goblet cells to promote mucus secretion. Collectively, these actions produce many of the symptoms seen in asthma. Given the ability of leukotrienes to lead to airway remodeling with increases in goblet cell and smooth muscle proliferation, it has been suggested that those suffering from chronic asthma especially will benefit from anti-leukotriene therapy 16.
Key points
Leukotriene receptor antagonists are:
- no more effective than beclomethasone 400 microgram per day
- less effective than beta agonists at preventing exercise-induced asthma
- probably useful in aspirin-sensitive asthma
- suitable for patients who are unable to take inhaled steroids
In addition to asthma, leukotrienes have been found to play a role in the development of cardiovascular disease. It has been noted that atherosclerotic vascular lesions express the entire biochemical machinery necessary for leukotriene production including 5-lipooxygenase, 5-lipoxygenase activating protein (FLAP), and other distal enzymes important for leukotriene synthesis. Moreover, it has been shown that levels of 5-lipooxygenase within atherosclerotic vessels correlates with disease severity. Based on animal models, it is believed that increases in leukotrienes promote the attraction of macrophages as well as their differentiation into foam cells. Globally, it has been found that several different ethnic populations with variants of leukotriene-related genes that lead to overproduction of leukotrienes have an increased incidence of stroke and myocardial infarction. Although anti-leukotriene therapy is not currently standard in the care of cardiovascular disease, increasing evidence supports the role of leukotrienes in its pathogenesis 17.
Lastly, leukotrienes have been noted to have a connection to various cancers. It is known that chronic inflammation leads to an increased risk of certain cancers. For example, the chronic inflammation provoked by inflammatory bowel disease (IBD) is believed to promote transformation to colorectal adenocarcinoma. In such patients, it has been found that these cancers have increased expression of cysLT. It has also been shown that leukotriene D promotes the up-regulation of Bcl-2, an anti-apoptotic protein that promotes cell survival. Similar findings have also been shown in other cancers including leukemia, lymphomas, esophageal, lung, and skin cancers. These malignancies have been shown to express increased amounts of 5-lipooxygenase, 5-lipoxygenase activating protein (FLAP), and other enzymes in the leukotriene synthesis pathway. Cell models and animal studies have suggested that anti-leukotriene therapies decrease cancer cell survival and decrease the incidence of certain malignancies 8.
Leukotriene receptor antagonist
Two leukotriene receptor antagonists also called leukotriene modifiers, are montelukast and zafirlukast, have been approved for use in the US to prevent asthma symptoms 18, 19. Montelukast and zafirlukast have only mild to moderate beneficial effects at best, but are very safe. Montelukast and zafirlukast are taken in pill form; chewable and sprinkle forms are available for young children and can be used together with a steroid inhaler. These drugs afford a degree of protection against antigen challenge and exercise-induced bronchospasm. They are particularly effective for patients with asthma who are sensitive to aspirin. While regular use can control asthma, they are no more effective than 400 microgram/day of beclomethasone dipropionate. Montelukast and zafirlukast are oral preparations. They may be useful for patients who prefer tablets or cannot tolerate inhaled beclomethasone because of local adverse effects.
These compounds (i.e., montelukast and zafirlukast) act by decreasing the effects of an inflammatory chemical made by the body known as leukotrienes.
Types of anti-leukotriene drugs
Four classes of drugs that interfere with leukotriene synthesis or activity have been developed. To date, no significant clinical differences have been observed between drugs of these classes, so the term anti-leukotriene drug has been coined for these compounds.
The 5-lipoxygenase inhibitors block the activity of 5-lipoxygenase. The 5-lipoxygenase activating protein (FLAP) inhibitors displace arachidonic acid from its binding site on the FLAP molecule and prevent this substrate from being presented to 5-lipoxygenase. These two classes of drugs block the synthesis of both cysteinyl leukotrienes (leukotriene C4, leukotriene D4, leukotriene E4) and leukotriene B4. The third class of drugs is the cysteinyl leukotriene receptor antagonists. The fourth class is the leukotriene B4 receptor antagonists.
Efficacy in acute challenge
Leukotriene D4-induced bronchoconstriction
In a study of mild asthmatics, a 10-fold shift in the leukotriene D4 dose-response curve was evident 12 hours after an oral dose of zafirlukast 40 mg. That is, higher doses of leukotriene D4 were required to induce bronchospasm because zafirlukast blocked the bronchoconstrictor response to leukotriene D4. The patients who had higher plasma concentrations of the drug at 12 hours had greater shifts in their dose-response curves than patients with lower plasma concentrations. A similar response was observed in studies of montelukast.
Exercise challenge
Exercise-induced asthma is partially inhibited by anti-leukotriene drugs. Zafirlukast, 20 mg taken orally two hours before exercise, had variable efficacy, ranging from complete protection in some individuals to little or no protection in others. The mean maximum percent falls in FEV1 after exercise were 36% for placebo and 21.6% for zafirlukast. Montelukast (10-50 mg) ameliorated asthma when the exercise challenge was performed at the end of the once daily dosing interval, immediately before the next dose. The protective effect of the anti-leukotriene drugs is less than that of the inhaled beta agonists, which abolish exercise-induced asthma in the majority of patients.
Antigen challenge
A challenge with inhaled antigens causes an early asthmatic response, peaking at 15 minutes with recovery over the next hour or so. In about 50% of patients, this early asthmatic response is followed after 6-8 hours by a late asthmatic response. This late reaction is accompanied by swelling of the airway wall and infiltration by inflammatory cells, together with increased airway response to methacholine and histamine (i.e. increased airway reactivity).
Zafirlukast (40 mg) given two hours before antigen challenge attenuates the early response by 80% and the late response by 50%. It partially reduces the associated increase in airway reactivity 6 hours after the challenge. In another study, a single 40 mg oral dose of zafirlukast reduced the response to inhaled cat allergen compared to placebo.
There was considerable inter patient variability in these studies. This variability in effectiveness is probably not due to pharmacokinetic differences. There may well be heterogeneity in the relative importance of leukotrienes in the pathogenesis of asthma in different people.
Some studies have used a bronchoscope to deliver an allergen challenge to a lung segment. The patients took zafirlukast 20 mg twice daily for 5 days before the challenge. Bronchial fluid was then collected 5 minutes and 48 hours after the antigen challenge. After 5 minutes, there were no statistically significant differences, in cell counts in the broncho-alveolar lavage fluid, between zafirlukast and placebo. By 48 hours, the basophil and lymphocyte counts and the histamine concentrations were reduced in the patients given zafirlukast. Studies of this type provide direct evidence that the oral administration of anti-leukotriene drugs reduces the magnitude of the lung’s inflammatory response to an antigen challenge.
Airway hyper reactivity
Allergen-induced hyper reactivity may be an important mechanism in the continuing symptoms and progression of disease. The ability of drugs to prevent this effect would be an important component of long-term drug therapy. Zafirlukast has been found to attenuate the antigen-induced increase in hyper reactivity, but similar studies with montelukast have not been reported. Oral treatment with pranlukast (not available in America) for 5 days also attenuates the allergen-induced hyper reactivity suggesting that this is a class effect.
Routes of administration
Most of the currently available asthma therapies are inhaled. This delivers the drugs more effectively to target sites in the lung and reduces the risk of systemic activity. The inhaled route of administration does have some problems, particularly with non-compliance or poor inhalation technique. Montelukast and zafirlukast have been developed as oral formulations, largely because of patient preference for this type of medication in the world’s two largest asthma markets, the U.S.A. and Japan. While tablets eliminate the problem of variable dose delivery due to poor inhalation technique, their systemic bioavailability may increase the risk of adverse events.
Pharmacokinetics
Zafirlukast is well absorbed with a mean oral bioavailability of 80%. Peak plasma concentrations are achieved by 2-3 hours and the plasma half-life is approximately 10 hours. Montelukast has a mean oral bioavailability of approximately 65%. Peak plasma concentrations are achieved by 2-3 hours and the plasma half-life is 5-6 hours. Both drugs undergo liver metabolism to several products that are thought to be inactive.
Use in chronic asthma
Large-scale clinical trials have studied zafirlukast (20 mg twice daily) in patients with mild asthma requiring treatment with beta agonists only. Compared with placebo, patient-reported endpoints, such as daytime asthma scores, night wakenings and use of beta agonists, have improved with zafirlukast.
In another large clinical trial, montelukast 10 mg daily was compared with placebo in patients who usually only used beta agonists for their mild asthma. In this study, there was an increase in FEV1, quality of life and parental global evaluation. In these trials, montelukast decreased the eosinophil counts in blood and in sputum.
Comparison with other drugs
In a 13-week comparative trial between zafirlukast 20 mg twice daily and sodium cromoglycate (1600 microgram daily), both drugs reduced symptom scores and improved lung function compared with placebo. Direct comparison with inhaled corticosteroids shows that both zafirlukast and montelukast are no more potent than beclomethasone dipropionate 400 microgram daily.
A 6-week double-blind study randomized patients with mild to moderate asthma to take beclomethasone dipropionate 200-250 microgram or zafirlukast 20 mg or 80 mg. Each drug was taken twice daily. Neither dose of zafirlukast was as effective as beclomethasone dipropionate. The most revealing finding in this study was the fact that there was a significant proportion of patients who did not respond to inhaled corticosteroids and a similar proportion who did not respond to zafirlukast. As there were 3 parallel treatment groups, there was no crossover to determine if the patients who did not respond to steroids may respond to the anti-leukotriene drugs. Such studies will be important in determining where the anti-leukotriene drugs fit in the treatment of asthma.
Aspirin-sensitive asthma
A small minority of asthmatic patients (2-5%) cannot tolerate aspirin. It can induce bronchospasm, naso-ocular and gastrointestinal reactions. These patients have an abnormally high leukotriene production, as measured by urinary leukotriene E4. An aspirin challenge further increases the leukotriene E4 concentration. Several studies have shown that the anti-leukotriene drugs diminish the bronchoconstrictor response in patients with aspirin-sensitive asthma.
Steroid sparing effect
In a randomized, double-blind, placebo-controlled trial of 79 patients with asthma requiring inhaled beclomethasone (1500 microgram daily or more), the inhaled dose of beclomethasone dipropionate was halved. The patients were then randomised to take pranlukast (not available in America) or placebo for 6 weeks.1 In the placebo group, there was a decrease in FEV1 and morning and evening peak flows. In contrast, these measures remained above baseline values (those recorded before randomisation) in patients taking pranlukast. The use of this leukotriene receptor antagonist had allowed a reduction in inhaled corticosteroids.
In another study, patients with stable asthma treated with 400-750 microgram of beclomethasone dipropionate were randomised to treatment with zafirlukast 20 mg twice daily or placebo. Both placebo and treated groups were able to reduce their dose of inhaled corticosteroids without loss of control of asthma. There was no statistical difference between the groups with respect to daytime symptoms, daily use of beta2 agonist or morning peak flows at the end of the study.
Where do anti-leukotriene drugs fit?
The majority of trials showing clinical efficacy of anti-leukotriene drugs have studied patients with mild asthma, requiring only beta-2 agonists. In these patients, the drugs are no more effective than 400 microgram beclomethasone dipropionate 20. The anti-leukotriene drugs may have a role in patients whose asthma would be controlled with modest doses of inhaled corticosteroids, if they were unable to tolerate the local adverse effects. The oral drugs may also be useful in patients who comply poorly with inhaler devices or have difficulty using an inhaler. Oral medications may also be useful in children, although neither montelukast nor zafirlukast is currently approved in the US for use in children under 6 years of age. Current evidence suggests that the anti-leukotriene drugs are likely to be effective in some individuals whose asthma is much more dependent upon leukotriene generation than others e.g. aspirin-sensitive asthma.
It is premature to state that the anti-leukotriene drugs are genuinely `steroid sparing’. If clinical trials to specifically address this question show that this is the case, then these drugs could be used in a similar fashion to long-acting beta agonists to cap the dose of inhaled corticosteroids.
In United States, doctors have a tradition of prescribing inhaled medications for the treatment of asthma. With the advent of the orally effective anti-leukotriene drugs, doctors now have an alternative approach to prescribing regular therapy. When prescribing these drugs, doctors must be mindful of the possibility of drug interactions because zafirlukast has the potential to affect (or be affected by) the hepatic metabolism of several other drugs.
Leukotriene modifiers side effects
Montelukast has been generally well tolerated in clinical trials. The adverse effects that have been reported more frequently than placebo in these clinical trials include abdominal pain and headache. Zafirlukast may cause drug interactions because it inhibits cytochrome P450, e.g. doses of warfarin may need to be reduced. Both erythromycin and theophylline reduce the plasma concentrations of zafirlukast by approximately 30-40%.
A rare disorder called Churg Strauss syndrome has occurred in 8 patients treated with zafirlukast 21. It is characterised by blood eosinophilia and eosinophilic infiltration of various organs, including skin and lung. The precise mechanism for this phenomenon is unclear, but it has been proposed that the patients had a primary eosinophilic disorder which was unmasked by the cessation (or reduction in one case) of corticosteroids when the patients began treatment with zafirlukast. Vigilance is necessary to determine if this syndrome occurs with other anti-leukotriene drugs.
References- Cuzzo B, Lappin SL. Physiology, Leukotrienes. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526114
- The discovery of the leukotrienes. Samuelsson B. Am J Respir Crit Care Med. 2000 Feb; 161(2 Pt 2):S2-6. https://www.atsjournals.org/doi/pdf/10.1164/ajrccm.161.supplement_1.ltta-1
- Effects of 6 weeks of therapy with oral doses of ICI 204,219, a leukotriene D4 receptor antagonist, in subjects with bronchial asthma. ACCOLATE Asthma Trialists Group. Spector SL, Smith LJ, Glass M. Am J Respir Crit Care Med. 1994 Sep; 150(3):618-23.
- Bronchial aspirin challenge causes specific eicosanoid response in aspirin-sensitive asthmatics. Szczeklik A, Sladek K, Dworski R, Nizankowska E, Soja J, Sheller J, Oates J. Am J Respir Crit Care Med. 1996 Dec; 154(6 Pt 1):1608-14.
- Cysteinyl leukotrienes: multi-functional mediators in allergic rhinitis. Peters-Golden M, Gleason MM, Togias A. Clin Exp Allergy. 2006 Jun; 36(6):689-703.
- 5-Lipoxygenase inhibitors for the treatment of inflammatory bowel disease. Rask-Madsen J, Bukhave K, Laursen LS, Lauritsen K. Agents Actions. 1992; Spec No():C37-46.
- Possible prognostic value of leukotriene B(4) in acute respiratory distress syndrome. Masclans JR, Sabater J, Sacanell J, Chacon P, Sabin P, Roca O, Planas M. Respir Care. 2007 Dec; 52(12):1695-700.
- Peters-Golden M, Henderson WR. Leukotrienes. N. Engl. J. Med. 2007 Nov 01;357(18):1841-54.
- Smith LJ. Leukotrienes and sex: strange bedfellows?. J Clin Invest. 2017;127(8):2895-2896. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5531399/
- Improvement of aspirin-intolerant asthma by montelukast, a leukotriene antagonist: a randomized, double-blind, placebo-controlled trial. Dahlén SE, Malmström K, Nizankowska E, Dahlén B, Kuna P, Kowalski M, Lumry WR, Picado C, Stevenson DD, Bousquet J, Pauwels R, Holgate ST, Shahane A, Zhang J, Reiss TF, Szczeklik A. Am J Respir Crit Care Med. 2002 Jan 1; 165(1):9-14.
- Pharmacogenetic association between ALOX5 promoter genotype and the response to anti-asthma treatment. Drazen JM, Yandava CN, Dubé L, Szczerback N, Hippensteel R, Pillari A, Israel E, Schork N, Silverman ES, Katz DA, Drajesk J. Nat Genet. 1999 Jun; 22(2):168-70.
- Gender differences in asthma development and progression. Postma DS. Gend Med. 2007; 4 Suppl B():S133-46.
- Androgen-mediated sex bias impairs efficiency of leukotriene biosynthesis inhibitors in males. Pace S, Pergola C, Dehm F, Rossi A, Gerstmeier J, Troisi F, Pein H, Schaible AM, Weinigel C, Rummler S, Northoff H, Laufer S, Maier TJ, Rådmark O, Samuelsson B, Koeberle A, Sautebin L, Werz O. J Clin Invest. 2017 Aug 1; 127(8):3167-3176.
- ERK-mediated regulation of leukotriene biosynthesis by androgens: a molecular basis for gender differences in inflammation and asthma. Pergola C, Dodt G, Rossi A, Neunhoeffer E, Lawrenz B, Northoff H, Samuelsson B, Rådmark O, Sautebin L, Werz O. Proc Natl Acad Sci U S A. 2008 Dec 16; 105(50):19881-6.
- Hammarström S. Leukotrienes. Annu. Rev. Biochem. 1983;52:355-77.
- Montuschi P. Role of Leukotrienes and Leukotriene Modifiers in Asthma. Pharmaceuticals (Basel). 2010 Jun 02;3(6):1792-1811
- Colazzo F, Gelosa P, Tremoli E, Sironi L, Castiglioni L. Role of the Cysteinyl Leukotrienes in the Pathogenesis and Progression of Cardiovascular Diseases. Mediators Inflamm. 2017;2017:2432958
- Montelukast. https://medlineplus.gov/druginfo/meds/a600014.html
- Zafirlukast. https://medlineplus.gov/druginfo/meds/a697007.html
- Ind PW. Anti-leukotriene intervention: is there adequate information for clinical use in asthma? Respir Med 1996;90:575-86.
- Wechsler ME, Garpestad E, Flier SR, Kocher O, Weiland DA, Polito AJ, et al. Pulmonary infiltrates, eosinophilia, and cardiomyopathy following corticosteroid withdrawal in patients with asthma receiving zafirlukast. JAMA 1998;279:455-7.