What is lichen striatus
Lichen striatus is an uncommon, benign, self-limiting linear skin rash that occurs mainly in children. Lichen striatus presents as pink raised spots that join together to form one or more dull red slightly scaly linear bands. Lichen striatus is clinically diagnosed on the basis of its appearance and characteristic developmental pattern following the lines of Blaschko 1.
The skin is the primary organ system affected by lichen striatus. However, lichen striatus also may involve the nails 2.
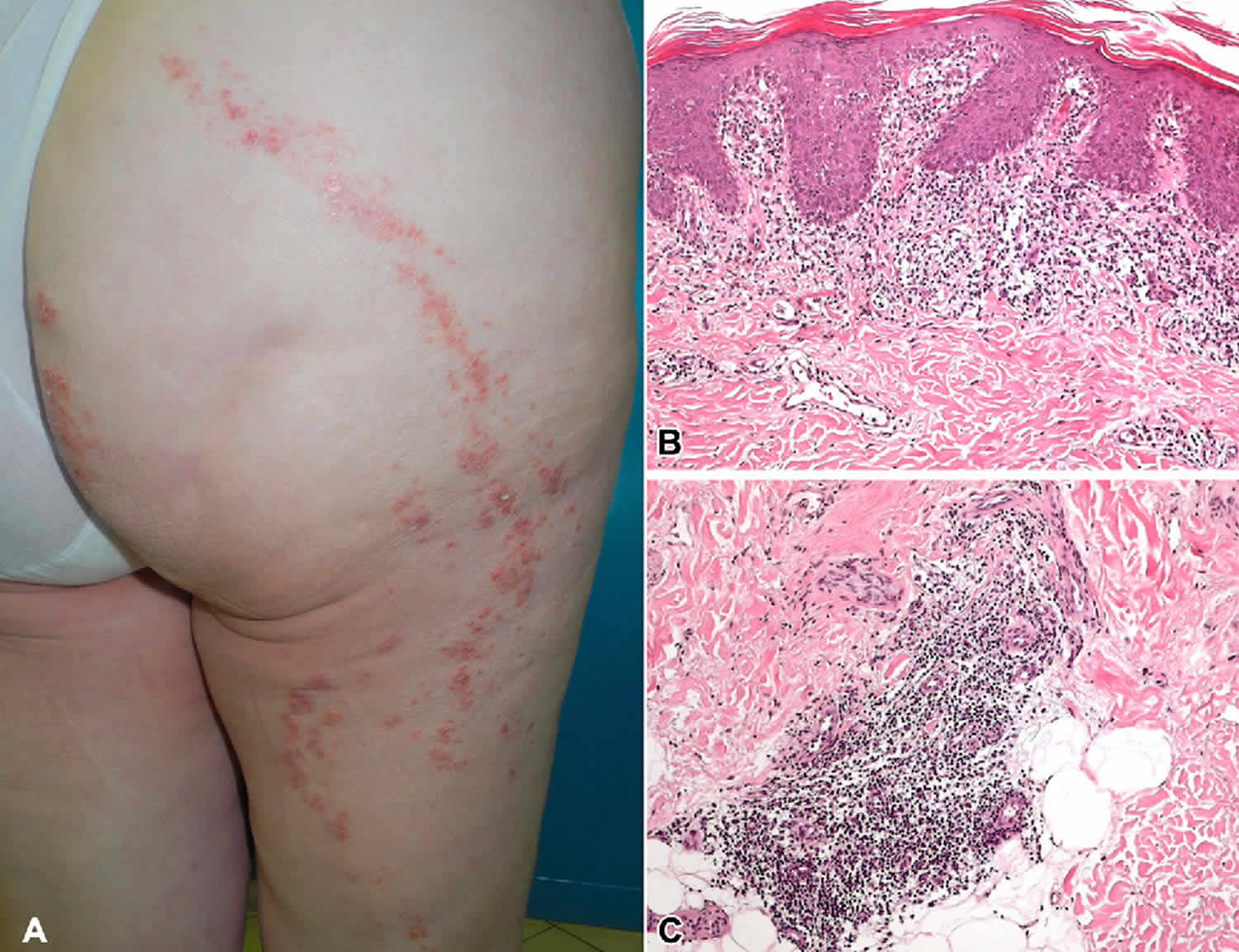
Figure 1. Lichen striatus
Footnote: Lichen striatus. A, Erythematous, scaly, papular eruption following the lines of Blaschko on the right leg. B, Detail of lichenoid lymphocytic interface dermatitis. C, Lymphocytic infiltrate involving eccrine gland coils (B and C, Hematoxylin-eosin stain; original magnifications: 3100).
[Source 3 ]Lichen striatus cause
The cause of lichen striatus is unknown. Possibly genetic factors or environmental triggers have a role to play in its development. The most commonly accepted hypothesis is the combination of genetic predisposition with environmental stimuli. The eruption affects the lines of Blaschko, which are thought to be embryonic in origin.
Over 50% of cases occur in children aged between 5 and 15 years. Lichen striatus appears in females two or three times as often as in males. Lichen striatus is rare in adults when it is sometimes known as acquired blaschkoid dermatitis or blaschkitis.
Atopy may be a predisposing factor. One group reported that 85% of patients with lichen striatus have a family history of atopic dermatitis, asthma, or allergic rhinitis. However, another report disputes this claim, stating that the incidence of atopy is no greater than that of the general population.
An autoimmune response may also be involved in lichen striatus. A case of lichen striatus has been reported during pregnancy, and it has been postulated that the pregnancy may have triggered an autoimmune response leading to the appearance of the eruption 4. Lichen striatus has also been reported concurrently with vitiligo 5 and after adalimumab 6 and etanercept 7. Some reports simply suggest that lichen striatus is an inflammatory skin disease mediated by T cells. It has been reported 17 months after allogenic peripheral blood stem cell transplantation 8.
An environmental (infectious or trauma) etiology has also been suggested 9. Familial cases 10, outbreaks among unrelated children in a shared living environment, and a possible seasonal variation suggest an environmental agent, such as a virus. Support of infectious involvement includes elevations of interleukin 1-beta in lichen striatus biopsy specimens 11. However, results of viral testing have not conclusively proven this association. In addition, familial episodes of lichen striatus are not always simultaneous, signifying a possible genetic predisposition as a second explanation. Lichen striatus has been reported to occur shortly following immunization with BCG and hepatitis B vaccination, after UV exposure from a tanning bed 12, following a prick from a pineapple leaf, after a bite by a bumblebee 13 and after varicella and influenza infection 14.
One group of authors has suggested that epigenetic mosaicism may be involved. They hypothesize that lichen striatus is triggered by an immunologic reaction to an infection, which triggers methylation or demethylation of a partially silenced genomic element in predisposed patients 11. A report of concurrent pityriasis rosea and lichen striatus may lend support to this theory. Human herpes viruses 6 and 7 have been implicated in the etiology of pityriasis rosea. The concurrent lichen striatus eruption may have manifested after being triggered by this viral infection 15.
Lesions of lichen striatus follow the lines of Blaschko 16. Blaschko lines are thought to be embryologic in origin. They are believed to be the result of the segmental growth of clones of cutaneous cells or the mutation-induced mosaicism of cutaneous cells. In lichen striatus, an acquired event (eg, viral infection) may allow an aberrant clone of cutaneous cells to express a new antigen, resulting in the phenotypic skin changes.
Lichen striatus symptoms
Lichen striatus starts as small pink, red or flesh colored spots that over the course of one or two weeks join together to form a dull red slightly scaly linear band. The band is usually 2 mm to 2 cm in width and may be a few centimeters in length or may extend the entire length of the limb. Sometimes there are two parallel bands. Lesions occur most commonly on one arm or leg but can affect the neck, face, or trunk. Sometimes a band may extend from the leg onto the buttock or abdomen. Usually, there are no symptoms but some patients may complain of slight or intense itching.
Occasionally nails may be affected, sometimes without any skin lesions. They become thick, ridged, split and may rarely fall off altogether.
Lichen striatus diagnosis
Lichen striatus is diagnosed by its typical clinical appearance. Findings on histopathology of a skin biopsy may also be helpful.
Lichen striatus treatment
There is no effective treatment for lichen striatus and in most cases none is necessary. Lichen striatus usually resolves within 6 months but may leave temporary pale or dark marks (hypopigmentation or hyperpigmentation).
Emollients may be used to help treat dryness or itching, if present. Topical steroids or pimecrolimus cream may clear the lesions although they may take some weeks to be effective.
Lichen striatus prognosis
The prognosis of patients with lichen striatus is excellent. Recovery is complete. Lichen striatus lesions usually regress spontaneously within 1 year, with a range of 4 weeks to 3 years. Relapses of lichen striatus may occur, but these are uncommon.
Lichen striatus of the nail may take a protracted course, lasting from 6 months to 5 years 17. Nail involvement resolves spontaneously without deformity.
References- Suárez-Peñaranda JM, Figueroa O, Rodríguez-Blanco I, Aliste C, Casas L. Unusual Interface Dermatoses Distributed Along Blaschko’s Lines in Adult Patients. Am J Dermatopathol. 2017 Feb. 39 (2):144-149.
- Kim M, Jung HY, Eun YS, Cho BK, Park HJ. Nail lichen striatus: report of seven cases and review of the literature. Int J Dermatol. 2015 Nov. 54 (11):1255-60.
- Lora, V., Kanitakis, J., Latini, A., & Cota, C. (2014). Lichen striatus associated with etanercept treatment of rheumatoid arthritis. Journal of the American Academy of Dermatology, 70 4, e90-e92
- Brennand S, Khan S, Chong AH. Lichen striatus in a pregnant woman. Australas J Dermatol. 2005 Aug. 46(3):184-6.
- Correia LD, Silva de Castro CC. Association between bilateral segmental vitiligo and lichen striatus: an expression of mosaicism?. Int J Dermatol. 2018 Mar 8.
- Monteagudo B, Cabanillas M, Suárez-Amor O, Ramírez-Santos A, Alvarez JC, de Las Heras C. [Adult blaschkitis (lichen striatus) in a patient treated with adalimumab]. Actas Dermosifiliogr. 2010 Dec. 101(10):891-2.
- Lora V, Kanitakis J, Latini A, Cota C. Lichen striatus associated with etanercept treatment of rheumatoid arthritis. J Am Acad Dermatol. 2014 Apr. 70 (4):e90-2.
- Mun JH, Park HJ, Kim HS, Kim SH, Ko HC, Kim BS. Lichen striatus occurring after allogenic peripheral blood stem cell transplantation in an adult with aplastic anemia. Ann Dermatol. 2012 Feb. 24(1):87-9.
- Shepherd V, Lun K, Strutton G. Lichen striatus in an adult following trauma. Australas J Dermatol. 2005 Feb. 46(1):25-8.
- Yaosaka M, Sawamura D, Iitoyo M, Shibaki A, Shimizu H. Lichen striatus affecting a mother and her son. J Am Acad Dermatol. 2005 Aug. 53(2):352-3.
- Racette AJ, Adams AD, Kessler SE. Simultaneous lichen striatus in siblings along the same Blaschko line. Pediatr Dermatol. 2009 Jan-Feb. 26(1):50-4.
- Ciconte A, Bekhor P. Lichen striatus following solarium exposure. Australas J Dermatol. 2007 May. 48(2):99-101.
- Unal E, Balta I, Bozkurt O. Lichen striatus: after a bite by bumblebee. Cutan Ocul Toxicol. 2015. 34 (2):171-2.
- Ishikawa M, Ohashi T, Yamamoto T. Lichen striatus following influenza infection. J Dermatol. 2014 Dec. 41 (12):1133-4.
- Verma P, Singal A, Yadav P, Sharma R. Concurrence of lichen striatus and localised pityriasis rosea: Cutaneous mosaicism. Australas J Dermatol. 2013 Feb. 54(1):41-2.
- Arias-Santiago SA, Sierra Giron-Prieto M, Fernandez-Pugnarie MA, Naranjo-Sintes R. [Lichen striatus following Blaschko lines]. An Pediatr (Barc). 2009 Jul. 71(1):76-7.
- Kim GW, Kim SH, Seo SH, Jung DS, Ko HC, Kim MB, et al. Lichen striatus with nail abnormality successfully treated with tacrolimus ointment. J Dermatol. 2009 Nov. 36(11):616-7.