What is cutis verticis gyrata
Cutis verticis gyrata (CVG) refers to a scalp condition with convoluted folds and deep furrows look similar to the folds of the brain 1. Cutis verticis gyrata is a progressive condition. It is mainly troublesome due to the cosmetic appearance. Rarely, it can be complicated by malignant melanoma developing within a melanocytic nevus 2. Primary cutis verticis gyrata occurs more commonly in males, and most commonly develops after puberty, but before age 30. The primary form of cutis verticis gyrata has a reported male-to-female ratio of 5:1. The incidence of cutis verticis gyrata may be reported as lower in women because longer hair may camouflage the condition. The estimated prevalence of cutis verticis gyrata is 1 in 100,000 in males 0.026 in 100,000 in females 3. Cutis verticis gyrata may occur alone where it is called isolated cutis verticis gyrata or in association with a variety of underlying conditions or treatments, including neuropsychiatric disorders, eye abnormalities, or inflammatory conditions 2. Some secondary forms of cutis verticis gyrata, like cerebriform intradermal nevus, can be present at birth. While most isolated cases of unknown cause are sporadic, autosomal recessive and autosomal dominant inheritance with varying degrees of severity have been described. In cases associated with underlying conditions, the cause depends on the underlying condition. Management may include keeping areas within the folds clean, and/or surgery if requested for psychological or cosmetic reasons 1.
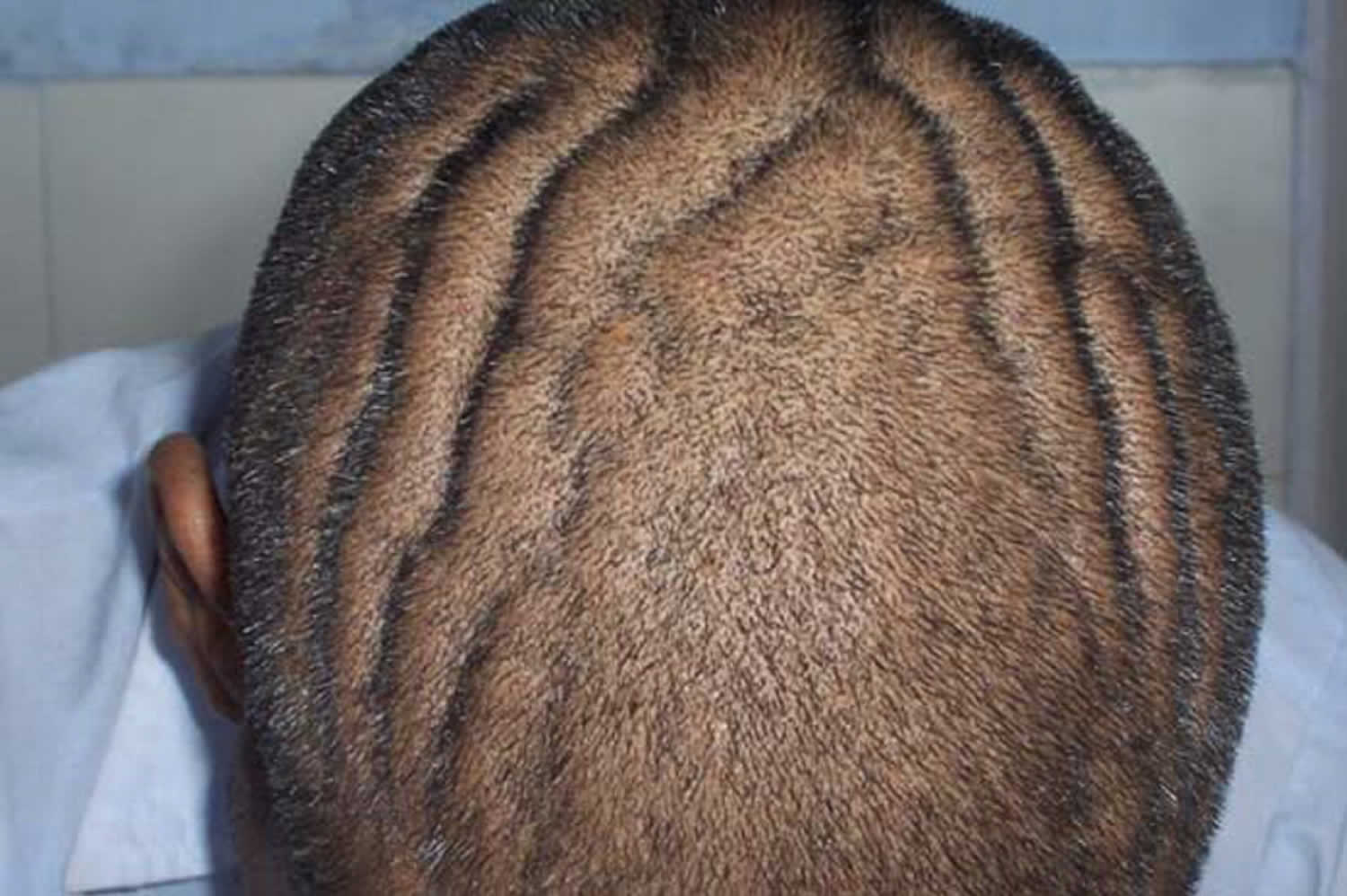
Figure 1. Cutis verticis gyrata
Classification of cutis verticis gyrata
Cutis verticis gyrata is classified according to the underlying cause as primary essential, primary nonessential and secondary.
Primary means the cause of the condition is unknown. Primary essential cutis verticis gyrata has no other associated abnormalities. Primary nonessential cutis verticis gyrata can be associated with neuropsychiatric disorders including cerebral palsy, epilepsy, seizures and ophthalmologic abnormalities, most commonly cataracts.
Secondary cutis verticis gyrata occurs as a consequence of a number of diseases that produce changes in scalp structure. These conditions include:
- Acromegaly (excessive growth hormone, due to pituitary gland tumour)
- Melanocytic nevi (moles)
- Birthmarks, including Connective tissue nevi, fibromas and nevus lipomatosus
- Inflammatory processes (eczema, psoriasis, Darier disease, folliculitis, impetigo, atopic dermatitis, acne).
Cutis verticis gyrata causes
The cause of cutis verticis gyrata is unknown in primary cases, although genetic and endocrinologic factors are suspected to participate in the etiology. Systemic diseases, inflammatory dermatoses, underlying nevoid abnormalities, and trauma are most common in secondary cases. Cutis verticis gyrata‒like lesions have been described in melanoma patients undergoing treatment with vemurafenib and whole-brain radiotherapy, but not with each of the treatments alone 4.
Secondary causes of cutis verticis gyrata are associated with the following underlying diseases and treatments:
- Acanthosis nigricans
- Acromegaly 5
- Amyloidosis 6
- Autosomal dominant insulin-resistant syndrome 7
- Beare-Stevenson syndrome
- Connective tissue nevus
- Cretinism
- Cutaneous leiomyomatosis 8
- Cylindroma
- Dermatofibroma
- Diabetes mellitus
- Ehlers-Danlos syndrome
- Fallopian tube carcinoma
- Fibroma
- Focal mucinosis
- Graves disease 9
- Hereditary neuralgic amyotrophy 10
- HIV-related lipodystrophy 11
- Hyperimmunoglobulin E syndrome 12
- Inflammatory processes (eg, eczema, psoriasis, Darier disease, folliculitis, impetigo, erysipelas, atopic dermatitis, acne conglobata) 13
- Intracranial aneurysm 14
- Intraventricular ependymoma 14
- Leukemia 15
- Melanocytic nevi or hamartomas (cerebriform intradermal nevus, giant cellular blue naevus, cutaneous neurocristic hamartoma) 16
- Myxedema 9
- Neurofibroma 17
- Nevus lipomatosus
- Noonan syndrome 18
- Pachydermoperiostosis 19
- Posttraumatic (eg, traction alopecia) 20
- Pseudoacromegaly 21
- Scleromyxedema without monoclonal gammopathy 22
- Supernumerary X chromosome syndromes (including Klinefelter syndrome) 23
- Syphilis
- Systemic T-cell lymphoma 24
- Tuberous sclerosis
- Turner syndrome
- Vemurafenib and whole-brain radiotherapy combination treatment in melanoma patients 25
Cutis verticis gyrata symptoms
Cutis verticis gyrata typically affects the central and back of the scalp, but some forms can involve the entire scalp. The folds are typically soft and spongy. The folds are unable to be corrected with pressure. The skin color is not affected. The number of folds can vary from 2 to more than 10.
Cutis verticis gyrata treatment
The management of cutis verticis gyrata includes good scalp hygiene to avoid accumulations of secretions in the furrows of the scalp. Definitive treatment by surgery may be requested for appearance reasons. Small localized lesions can be excised in one procedure. Larger lesions can be removed with serial excision, requiring multiple procedures.
In cases of cerebriform intradermal nevus, early diagnosis, wide surgical excision, and plastic reconstruction should be always considered 26.
Cutis verticis gyrata prognosis
The prognosis of primary cutis verticis gyrata is good, although the condition does not regress without surgical intervention and progression of cutis verticis gyrata may be observed. In secondary cases, the prognosis depends on the underlying process 27.
Cutis verticis gyrata is long lasting and progressive. It is often found to be unacceptable because of cosmetic reasons. It can be complicated by malignant melanoma developing within a congenital melanocytic nevus 26.
References- Cutis Verticis Gyrata. https://emedicine.medscape.com/article/1113735-overview
- Cutis verticis gyrata. https://www.dermnetnz.org/topics/cutis-verticis-gyrata
- Schenato LK, Gill T, Carvalho LA, et al. Essential primary cutis vertices gyrata. J Pediatr 2002;78:75–80.
- Lang N, Sterzing F, Enk AH, Hassel JC. Cutis verticis gyrata-like skin toxicity during treatment of melanoma patients with the BRAF inhibitor vemurafenib after whole-brain radiotherapy is a consequence of the development of multiple follicular cysts and milia. Strahlenther Onkol. 2014 Oct. 190 (11):1080-1.
- Zangeneh F, Carpenter PC. Visual vignette. Cutis verticis gyrata (GVG) in acromegaly. Endocr Pract. 2002 Nov-Dec. 8(6):475.
- Saoji V, Chaudhari S, Gohokar D. Primary systemic amyloidosis: three different presentations. Indian J Dermatol Venereol Leprol. 2009 Jul-Aug. 75(4):394-7.
- Woollons A, Darley CR, Lee PJ, Brenton DP, Sonksen PH, Black MM. Cutis verticis gyrata of the scalp in a patient with autosomal dominant insulin resistance syndrome. Clin Exp Dermatol. 2000 Mar. 25(2):125-8.
- Marque M, Gardie B, Bressac de Paillerets B, Rustin P, Guillot B, Richard S, et al. Novel FH mutation in a patient with cutaneous leiomyomatosis associated with cutis verticis gyrata, eruptive collagenoma and Charcot-Marie-Tooth disease. Br J Dermatol. 2010 Dec. 163(6):1337-9.
- Bilen H, Atasoy M, Akcay G, Akcay M, Capoglu I, Gursan N, et al. Elephantiasic pretibial myxedema and cutis verticis gyrata caused by graves’ disease. Thyroid. 2006 Aug. 16(8):815-6.
- Jeannet PY, Watts GD, Bird TD, Chance PF. Craniofacial and cutaneous findings expand the phenotype of hereditary neuralgic amyotrophy. Neurology. 2001 Dec 11. 57(11):1963-8.
- Khanijow K, Unemori P, Leslie KS, Mulligan K, Schambelan M, Maurer T. Cutis Verticis Gyrata in Men Affected by HIV-Related Lipodystrophy. Dermatol Res Pract. 2013. 2013:941740.
- Harish V, Clarke F. Isolated cutis verticis gyrata of the glabella and nasal bridge: a case report and review of the literature. J Plast Reconstr Aesthet Surg. 2013 Oct. 66(10):1421-3.
- Larsen F, Birchall N. Cutis verticis gyrata: three cases with different aetiologies that demonstrate the classification system. Australas J Dermatol. 2007 May. 48(2):91-4.
- Kolawole TM, al Orainy IA. Cutis verticis gyrata (case reports of rare causes). West Afr J Med. 1999 Apr-Jun. 18(2):130-2.
- Passarini B, Neri I, Patrizi A, Masina M. Cutis verticis gyrata secondary to acute monoblastic leukemia. Acta Derm Venereol. 1993 Apr. 73(2):148-9.
- Rao AG, Koppada D, Haritha M. Giant Cerebriform Congenital Cellular Blue Nevus Presenting as Cutis Verticis Gyrata. Indian J Dermatol. 2016 Jan-Feb. 61 (1):126.
- Commens CA, Greaves MW. Cutis verticis gyrata due to an intradermal naevus with an underlying neurofibroma. Clin Exp Dermatol. 1978 Sep. 3(3):319-22.
- Fox LP, Geyer AS, Anyane-Yeboa K, Garzon MC. Cutis verticis gyrata in a patient with Noonan syndrome. Pediatr Dermatol. 2005 Mar-Apr. 22(2):142-6.
- Arikan S, Sen I, Bahceci M, Tuzcu A, Ayli M. An interesting case of pachydermoperiostosis with idiopathic myelofibrosis associated with monosomy 22. Int J Dermatol. 2009 Aug. 48(8):882-5.
- Kanwar AJ, Ghosh S, Thami GP, Kaur S. Alopecia and cutis verticis gyrata due to traction presenting as headache. Int J Dermatol. 1992 Sep. 31(9):671-2.
- Nguyen KH, Marks JG Jr. Pseudoacromegaly induced by the long-term use of minoxidil. J Am Acad Dermatol. 2003 Jun. 48(6):962-5.
- Koregol S, Yatagiri RV, Warad SR, Itagi NR. A rare association of scleromyxedema with cutis verticis gyrata. Indian Dermatol Online J. 2016 May-Jun. 7 (3):186-9.
- Keller K, Williams C, Seagle B. Klinefelter syndrome and cutis verticis gyrata. Am J Med Genet. 2001 Oct 15. 103(3):249-51.
- George AA, George L, Mahabal G, Bindra M, Pulimood S. Systemic T cell lymphoma presenting as cutis verticis gyrata. Indian J Dermatol Venereol Leprol. 2015 Nov-Dec. 81 (6):631-3.
- Harding JJ, Barker CA, Carvajal RD, Wolchok JD, Chapman PB, Lacouture ME. Cutis verticis gyrata in association with vemurafenib and whole-brain radiotherapy. J Clin Oncol. 2014 May 10. 32 (14):e54-6.
- Hayashi Y, Tanioka M, Taki R, Sawabe K, Kore-eda S, Utani A, et al. Malignant melanoma derived from cerebriform intradermal naevus. Clin Exp Dermatol. 2009 Dec. 34(8):e840-2.
- Beauregard S. [Cutis verticis gyrata and pachydermoperiostosis. Several cases in a same family. Initial results of the treatment of pachyderma with isotretinoin]. Ann Dermatol Venereol. 1994. 121(2):134-7.