Lupus pernio
Lupus pernio also called Besnier-Tenneson syndrome, nodular or plaque sarcoidosis or sarcoidosis lupus pernio type, is a chronic non-life threatening type of cutaneous sarcoidosis that can be related to chronic fibrotic sarcoidosis, hyperglobulinemia and hypercalcemia 1. The name is derived from the Latin name for ‘wolf’ (lupus) and for ‘chilblain’ (pernio). This is because it was thought to be related to lupus vulgaris (cutaneous tuberculosis) by Besnier (1889) 2.
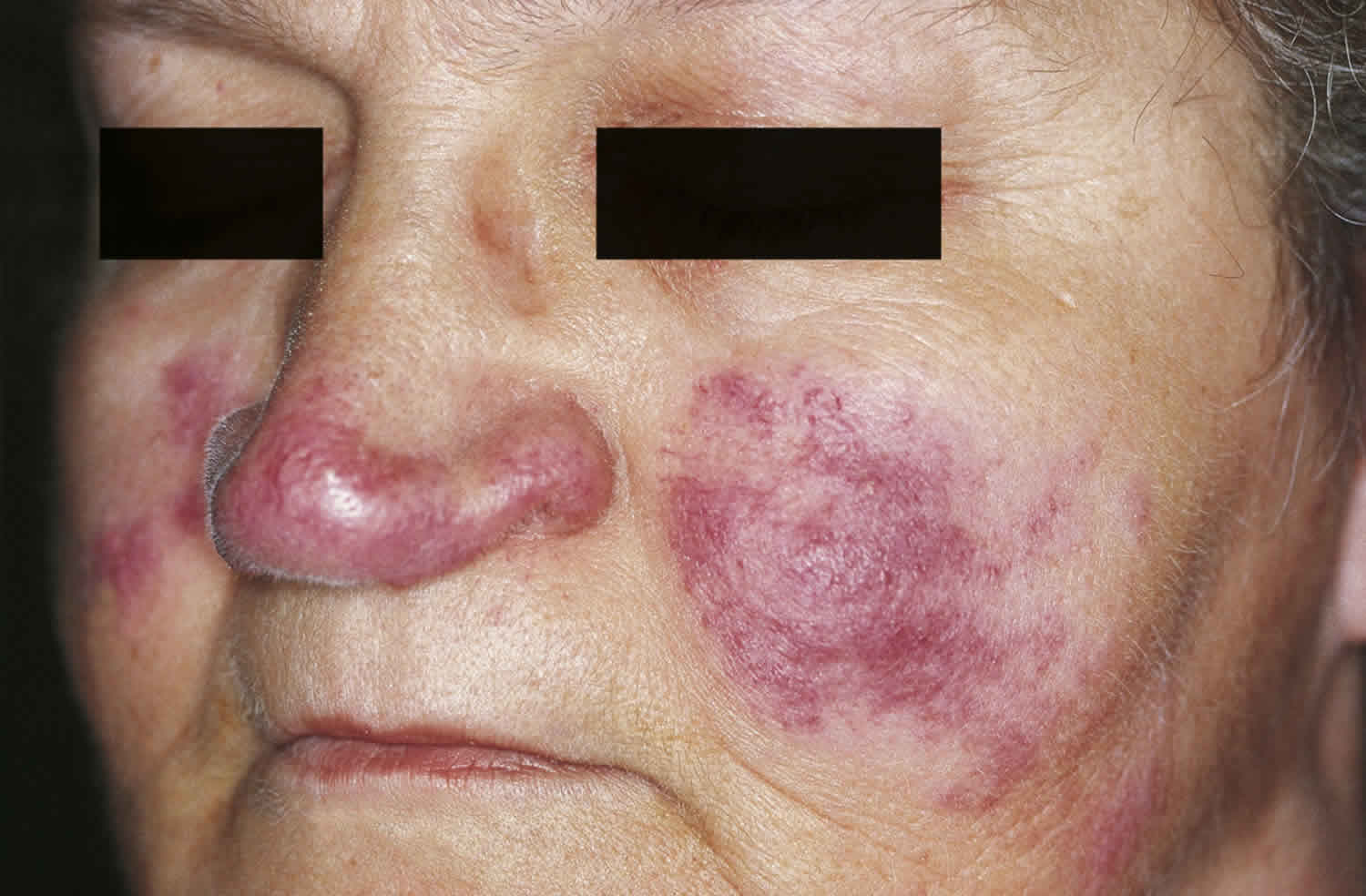
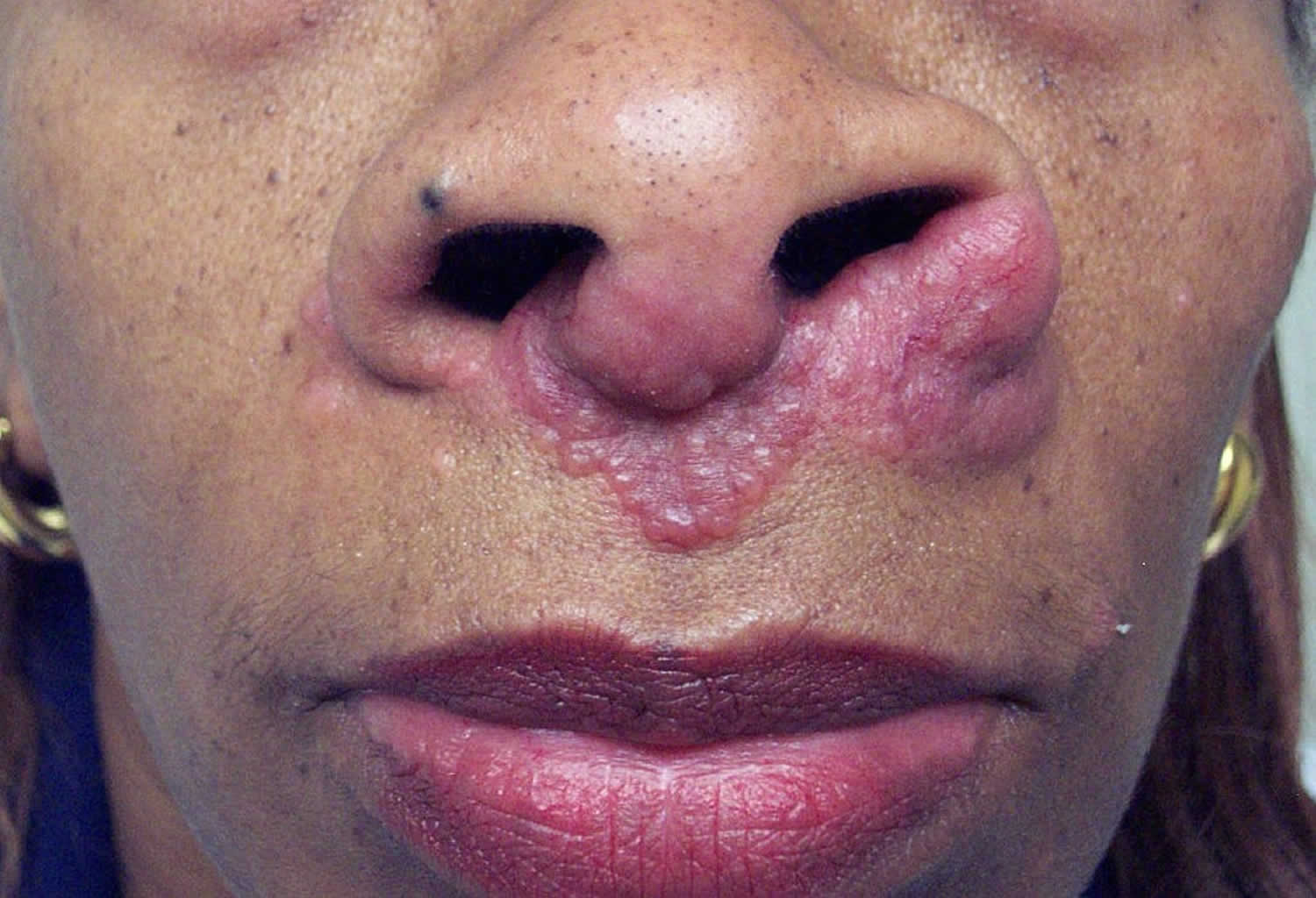
Lupus pernio is an indicator of chronic sarcoidosis. Sarcoidosis is a multisystemic granulomatous condition characterized by collection of non-caseating epithelioid granulomas. It can affect the pulmonary, reticuloendothelial, skin, gastrointestinal, cardiac, musculoskeletal, endocrine, or central nervous system. Sarcoidosis can be divided into two broad categories: systemic or cutaneous 3. Lupus pernio presents as blue red to violet smooth shiny nodules and plaques on the head and neck, predominantly on the nose, ears, lips, and cheeks 4. Lupus pernio rarely resolves spontaneously and may cause cosmetic disfigurement, nasal obstruction and fibrotic pulmonary complications due to extensive involvement of the nasal cavity and maxillary sinus 5. There is a 50% risk of developing lupus pernio if the patient has upper respiratory tract sarcoidosis, although each can present separately 6. Cutaneous sarcoidosis can be the presenting sign of systemic sarcoidosis, and work-up is indicated in all patients with cutaneous manifestations.
Annual incidence of lupus pernio is thought to be between 1 and 64 per 100,000. It is more common among some populations of African origin, women and ages between 45 and 65 7.
Some populations are at greater risk of developing lupus pernio:
- The age of onset is most often between 45 and 65 years of age.
- Lupus pernio is twice as common in women as in men.
- Lupus pernio is more common and more severe in African ethnic groups than in Caucasians.
- There are genetic/HLA associations.
The cause of cutaneous sarcoidosis is unknown, although some theories exist. In literature, it has been proposed that it could be due to the unusual host reaction to Mycobacterium paratuberculosis, fungi, histoplasmosis or other infective agents. Other studies refer to it as a cell mediated immune response were granulomas are formed as a result of activation of CD4 T lymphocytes and macrophages which release cytokines 7. Sarcoidal inflammation has been related to multiple factors, including infectious antigens, genetics and environmental triggers, and the immune system. The immune system is thought to be related in that it involves Th1 predominant response with interferon-gamma and tumor necrosis factor. In addition, there is evidence in literature suggesting a role of Th17 inflammation and interplay with the innate immune system 7.
Lupus pernio rarely resolves spontaneously and may cause cosmetic disfigurement, nasal obstruction and fibrotic pulmonary complications due to extensive involvement of the nasal cavity and maxillary sinus 5.
Lupus pernio in all cases requires treatment due to its destructive nature. Despite the lack of evidence for treatment of lupus pernio, topical corticosteroid therapy has shown favorable responses. Systemic corticosteroids are used for thick plaques unresponsive to topical corticosteroids and where intralesional corticosteroids would be impractical and painful 8. Systemic glucocorticosteroids (prednisolone 30-40 mg per day) has been associated with great results and almost complete resolution. Intralesional therapy also proved better than local therapy in such cases. Antimalarials, methotrexate and tetracycline derivatives are glucocorticoid sparing agents that are used either as alternatives or in order to decrease the dose of corticosteroid 8.
Figure 1. Lupus pernio nose
[Source 1 ]Figure 2. Lupus pernio nose
[Source 9 ]Lupus pernio causes
Despite intensive investigation, the cause of lupus pernio and other forms of cutaneous sarcoidosis is unknown. Sarcoidosis is recognized as a chronic cell-mediated immune response to an unknown antigen, in which activated macrophages and CD4 T-lymphocytes release cytokines that trigger the formation of granulomas.
At least some cases of cutaneous sarcoidosis may be due to an unusual host reaction to one or more infective agents, such as Mycobacterium paratuberculosis, histoplasmosis, other infective agents and other fungi. Lupus pernio itself is not infectious.
Other studies refer to it as a cell mediated immune response were granulomas are formed as a result of activation of CD4 T lymphocytes and macrophages which release cytokines 7. Sarcoidal inflammation has been related to multiple factors, including infectious antigens, genetics and environmental triggers, and the immune system. The immune system is thought to be related in that it involves Th1 predominant response with interferon-gamma and tumor necrosis factor. In addition, there is evidence in literature suggesting a role of Th17 inflammation and interplay with the innate immune system 7.
It is uncertain why lupus pernio affects sites where the skin is cool.
The histopathological changes are similar in all organs affected by sarcoidosis. The gold standard feature in histology is non-caseating granuloma with sparse lymphocytic component known as naked granuloma. The granulomas are usually observed in the dermis but can extend in some cases to the subcutaneous tissue. At the center of the granuloma, CD helper cells or induced T lymphocytes are present, whereas at the periphery small proportion of CD8 suppressor and cytotoxic T lymphocytes can be present. Granulomas can contain few or no giant cells 10.
Lupus pernio symptoms
Lupus pernio is usually asymptomatic, and it rarely causes itch or pain. Cosmetic disfigurement is the most common complaint.
It presents as indolent reddish-purple plaques and nodules on the nose, cheeks, lips, ears and digits. Lesions may ulcerate and later heal with telangiectatic scars.
Lesions on the nasal rim are associated with granulomatous inflammation of the upper respiratory tract. The skin lesions may extend to the nasal septum leading to nosebleeds and crusting.
Lupus pernio diagnosis
Lupus pernio diagnosis is based on the results of clinical and histological studies. Lupus pernio may be recognized by its typical clinical appearance and history, but the diagnosis may difficult to establish and delayed.
Examination of the edge of the skin lesion using diascopy, or pressure with a glass slide, shows apple-jelly appearance typical of granulomatous inflammation.
Biopsy of the skin, lymph nodes or lungs confirms the diagnosis by revealing sarcoidal non-caseating granulomas. Histologically, lupus pernio is characterized by the presence of naked epithelial cell granulomas that are, without inflammatory reaction around and inside the granuloma, without caseosa (fibrinoid necrosis); presence of different numbers of giant cells of type of Pirogov-Langhans type and foreign body unchanged or atrophic epidermis.
As lupus pernio is associated with sarcoidosis in the lungs (75% of patients) and upper respiratory tract (50%), the following tests should also be performed at diagnosis and for monitoring:
- Lung function tests
- Chest X-ray
- Electrocardiogram (ECG) or echocardiogram
- Blood tests, which may show elevated angiotensin-converting enzyme (ACE), alkaline phosphatase, calcium, gamma globulin (polyclonal) and reduced lymphocyte count
It is important to exclude tuberculosis. Tuberculin skin test and QuantiFERON® gold blood test are negative in sarcoidosis.
Laboratory investigations usually show no significant changes, except for hypercalcemia, serum angiotensin converting enzyme level >2-3 times the upper limit of normal, and Kveim-Siltzbach skin test positive in about 91% of patients with lupus pernio, compared with a positivity of 65% o in sarcoidosis overall 1. The main radiological manifestation of pulmonary sarcoidosis is bilateral increase of intrathoracic lymph nodes. Enlarged lymph nodes are clear of polycyclic outlines. In the early stages of the disease, there is increased pulmonary pattern due to peribronchial and perivascular mesh. Later there is development of focal shadows (original marmoristeria) of various size, round shape, two-way, spread in all lung fields, but predominant in the lower and middle parts of the lungs. With the progression of the process, there is an intense proliferation of connective tissue diffuse pneumosclerosis changes (honeycomb lung). X-rays may reveal bone destruction in the form of multiple foci rarefaction of bone tissue, mainly in the phalanges of hands and feet. In this form of limited emptiness round or oval, clearly seen in x-rays is so-called custody osteitis, symptom of osteitis Morozova Yunglinga. More rarely, bones of the skull and long bones are involved in the process. The eye may be affected by sarcoidosis mainly the anterior and posterior uveitis (the most common form of disease), conjunctivitis, corneal opacity, cataracts or glaucoma, changes of the iris, or decreased visual acuity.
Lupus pernio differential diagnosis
Lupus pernio differential diagnosis includes the following 11:
- malignant and benign tumors (lymphoma and cutaneous pseudolymphoma, benign, Kaposi’s sarcoma, mastocytosis, melanoma, histiocytoma, etc.),
- granuloma faciale,
- specific infections (leprosy, skin tuberculosis, and leishmaniasis),
- cutaneous manifestations of metabolic disorders (xanthomas, necrobiosis lipoidica, etc.),
- lupus erythematosus,
- lichen planusand others.
Lupus pernio treatment
Treatment is required for lupus pernio due to the risk of disease progression or cosmetic disfigurement implying physical, psychological and social impairment that may be acquired. The goal of the treatment of lupus pernio is to improve the patient’s appearance and prevent scarring. Nevertheless, treatment is difficult and complicated due to the unpredictable course of the condition 8.
The treatment chosen may depend on the severity of systemic symptoms.
The treatment has varying success. Options include:
- Topical corticosteroids
- Intralesional steroid injections
- Laser treatment (pulsed dye and carbon dioxide lasers)
- Systemic therapies, which include systemic corticosteroids, hydroxychloroquine, methotrexate and biologic agents (infliximab, adalimumab)
Cosmetic camouflage may be used to disguise skin lesions.
Numerous therapeutic options are available in literature on the treatment of sarcoidosis but few randomized trials are available addressing the treatment options of various cutaneous manifestations and no treatment for sarcoidosis is yet approved by the United States Food and Drug Administration (FDA). The first line therapy is local then systemic glucocorticosteroid. For limited skin involvement, intralesional injections of triamcinolone acetonide is used. Several other management modalities which are given in literature include chloroquine, hydroxychloroquine, methotrexate, azathioprine, cyclophosphamide, thalidomide, and infliximab 12.
Lupus pernio may fail to respond to the above and disease modifying drugs may be of benefit. Infliximab used as monotherapy or combination has been shown in some trials to be superior in the treatment of lupus pernio, which is administered IV 3 to 5 mg/kg initially then subsequent doses at 2, 4,6,10 and 14 weeks 13. Other studies showed that halobetasol propionate 0.05% ointment resulted in significant flattening of the lesions and is given twice a day for approximately 10 weeks 14.
Another drug which has shown good results in a case studied is Lenalidomide 10mg daily for approximately 3 months 15. Some research articles have concluded with promising results using either pulsed dye laser or photodynamic therapy 16. Lastly, minocycline has been shown to have good results but needs more research to prove its efficacy 17.
Lupus pernio prognosis
Lupus pernio tends to persist for several years and seldom resolves spontaneously. Lung and cardiac function should be monitored.
References- Hubail A, Belkharoeva R, Tepluk N, Belerosova T. Lupus pernio (Besnier-Tenneson syndrome): A rare form of sarcoidosis. Dermatol Reports. 2018;10(2):7696. Published 2018 Oct 1. doi:10.4081/dr.2018.7696 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6250080
- Scadding JG, Mitchell DN. Sarcoidosis. London, UK: Eyre & Spottiswoode; 1967
- Gopikrishnan A, Rita V. Lupus pernio without systemic involvement. Indian Dermatol Online J 2013;4:314-7.
- Howard A. Non-infectious granulomas. Bolognia J, ed. Textbook Dermatology. Vol 2. London, UK: Mosby; 2008.
- Amor K. Plaques and papules on the nose. Am Fam Physician 2006;73:1431-2.
- Wanat AK, Rosenbach M. Cutanous Sarcoidosis. Clin Chest Med 2015;36:685-702.
- Gawkrodger DJ. Sarcoidosis. Burns T, Breathnach S, Cox N, Griffiths C, eds. Rooks Textbook of Dermatology. Vol. 5. Massachusetts: Blackwell Science Ltd; 2016. pp 98.1-98.13.
- Baughman RP, Lower EE. Evidence-based therapy for cutaneous sarcoidosis. Clin Dermatol 2007;25:334.
- Successful long-term management of refractory cutaneous and upper airway sarcoidosis with periodic infliximab infusion. Dermatology Online Journal 13 (3): 14 https://escholarship.org/uc/item/3n87w6h3
- Paller A, Gilcrest Bam Leffell DJ, et al. Fitzpatrick dermatology in general medicine. London; McGraw Hill Medical; 2012.
- Peter S, Kim M, Maor S, et al. Pulmonary arterial hypertension. Clin Chest Med 2013;34:799-857.
- Anjaneyan G, Vora R. Lupus pernio without systemic involvement. Indian Dermatol Online J 2013;4:314-7.
- Stagaki E, Mountford WK, Lackland DT, et al. The treatment of lupus pernio: results of 116 treatment courses in 54 patients. Chest 2009;135:468-76.
- Dalm VA, van Hagen PM. Efficacy of lenalidomide in refractory lupus pernio. JAMA Dermatol 2013;149:493-4.
- Ashinoff R, Dosik JS. Treating lupus pernio with the 585 nm pulsed dye laser. Skin Aging 1999;7:93.
- Roos S, Raulin C, Ockenfels HM, et al. Successful treatment of cutaneous sarcoidosis lesions with the flashlamp pumped pulsed dye laser: a case report. Dermatol Surg 2009;35:1139-40.
- Bachelez H, Senet P, Cadranel J, et al. The use of tetracyclines for the treatment of sarcoidosis. Arch Dermatol 2001;137:6973.