Nevus of Ota
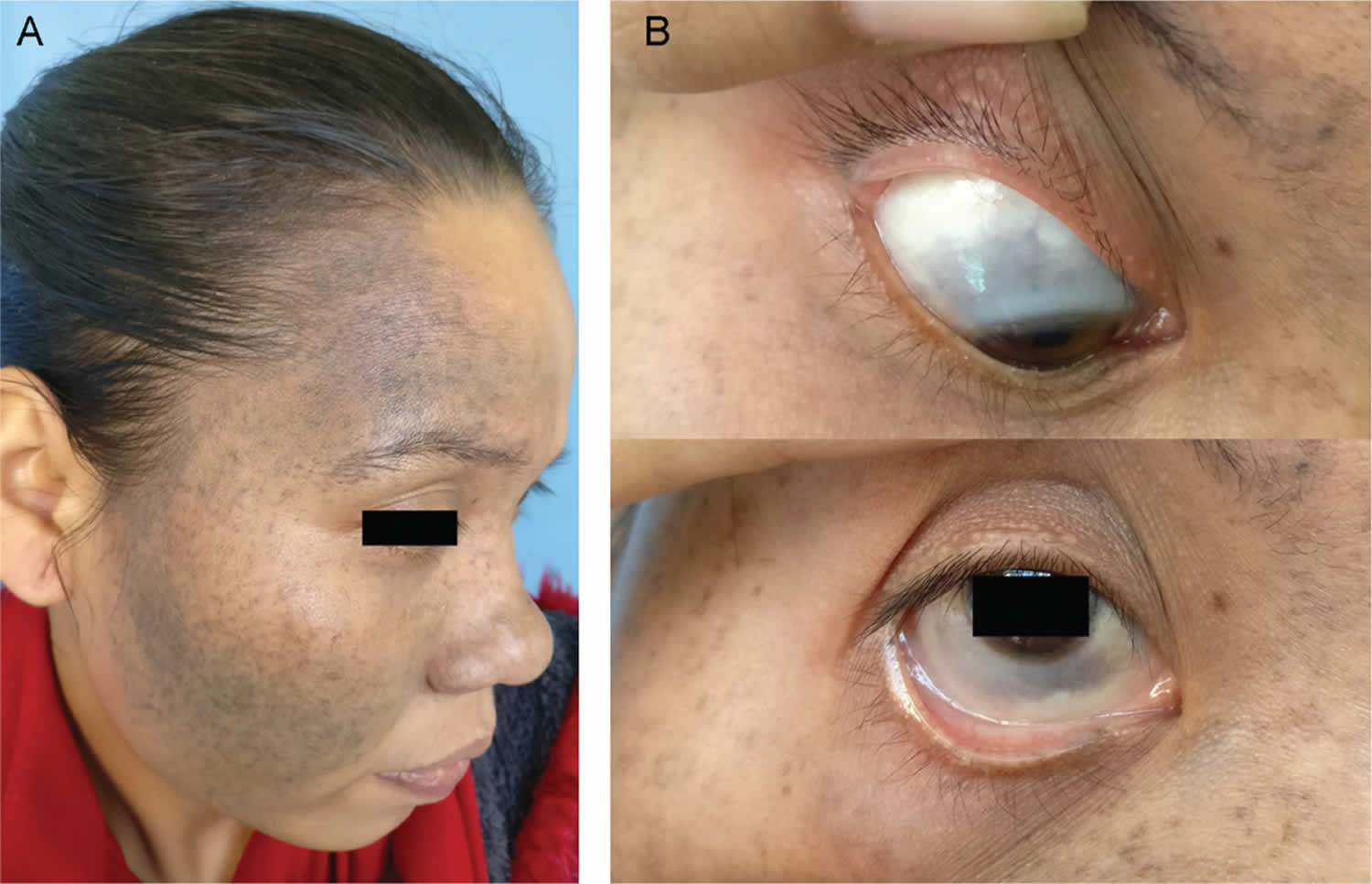
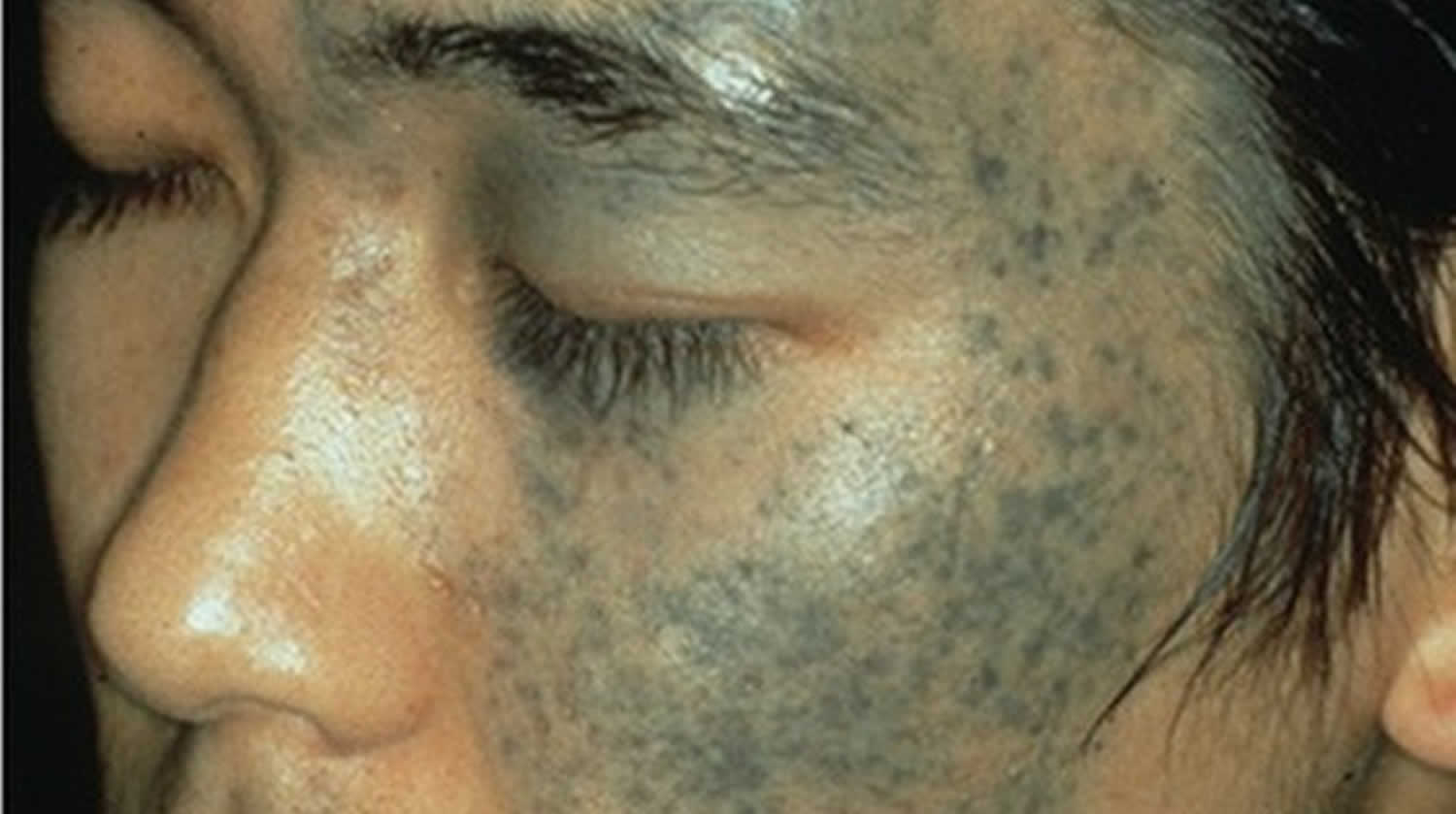
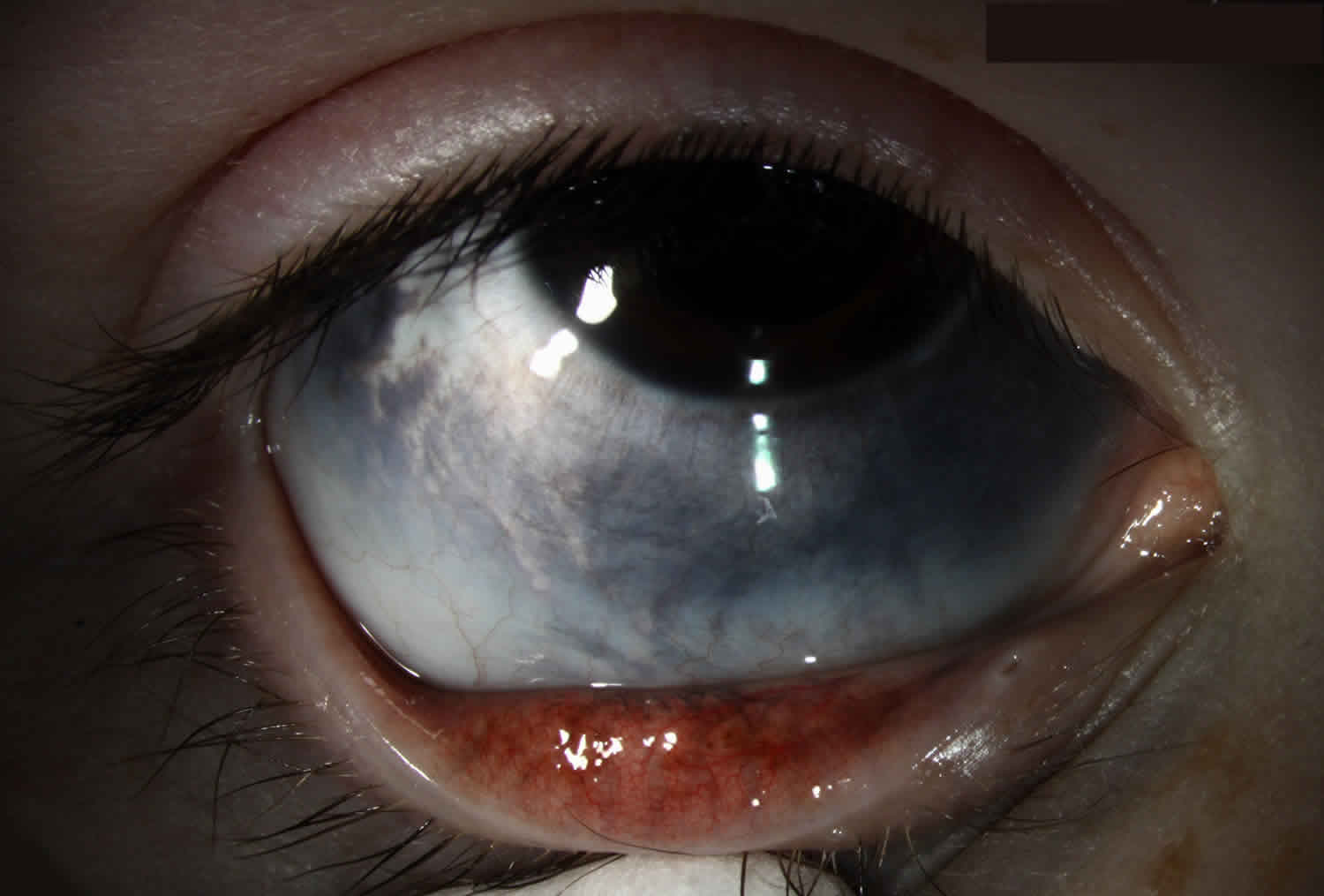
Nevus of Ota also called oculodermal melanocytosis, is a pigmented birthmark that is slate-brown or blue/grey in color. Nevus of Ota is usually a unilateral, patchy dermal melanosis that affects the skin of the face along the distribution of the ophthalmic and maxillary divisions of the trigeminal nerve 1. Nevus of Ota usually involves the periorbital region, the temple, the forehead, the malar area and the nose. Nevus of Ota rye is a condition of excessive pigmentation of the uvea, sclera, episclera, and eyelids secondary to an increase in the number of normal melanocytes. In about two third cases the ipsilateral sclera is affected with a bluish discoloration 2. When the eyelids are not involved, it is called ocular melanocytosis 3. When examined under a microscope, the pigmented nevus cells are found in the deep layer of the skin (dermis).
Nevus of Ota is a dermal melanosis 4. Nevus of Ota occurs more commonly in Asians and blacks though cases in whites have also been reported 5. Though rare in white population, nevus of Ota affects near about 0.014-0.034% of the Asian population 6. Nevus of Ota is usually unilateral in 90% of cases though at times bilateral cases may occur. Females are affected five times more than the males 7. The onset is usually at birth but may appear at puberty in a small percentage of cases 8. The intensity of the lesion may be influenced by the onset of puberty, fatigue, menstruation, insomnia and even weather 9. The typical lesion is unilateral though bilateral involvement may occur 10. The extracutaneous lesions may occur in sclera, cornea, eyelids, retina and other sites like tympanum (55%), nasal mucosa (30%), pharynx (25%), palate (20%) etc 5.
Nevus of Ota may occur simultaneously with nevus of Ito. Nevus of Ito usually manifests as unilateral, asymptomatic, blue, gray or brown lesions 11. Nevus of Ito was first described by Minor Ito in 1954 12. Nevus of Ito differs from the nevus of Ota only by its area of distribution and rarity. Nevus of Ito affects the area of distribution of the posterior supraclavicular and lateral cutaneous brachial nerves that encompass the supraclavicular, scapular or deltoid regions 5. Bilateral nevus of Ito is an extremely rare condition. In exceptional cases nevus of Ito may be present simultaneously with the nevus of Ota 13.
Nevus of Ota, nevus of Ito, mongolian spot, and dermal melanocyte hamartoma are the morphological forms of dermal melanosis 14.
Treatment of a melanocytosis may include cosmetic camouflage to cover the disfiguring markings, and laser treatment (usually using 1064nm Q switched Nd:YAG, Alexandrite or QS ruby laser) or intense pulsed light (IPL):
- Picosecond laser may be the most effective device.
- Laser and light devices work by destroying the dermal melanocytes.
- Multiple treatments are necessary, often with a combination of devices.
- Laser treatment is more effective in treating melanocytosis in light skinned individuals compared to those with dark skin.
- Recurrence is common after laser clearance, sometimes resulting in a darker hue than prior to treatment.
If the eye is affected, regular eye examinations should be arranged to detect glaucoma. Any change in a nevus should be assessed by a dermatologist.
Figure 1. Nevus of Ota
Figure 2. Nevus of Ota eye
Nevus of Ota classification
A number of classifications have been suggested depending on different parameters and utility 15. The classification laid down by Tanino in 1939 has remained the most useful clinical classification and in this classification nevus of Ota has been classified into four major subtypes 16:
Type-1
- 1A: Mild orbital type-Distribution over the upper and lower eyelids, periocular and temple region.
- 1B: Mild zygomatic type-Infrapalpebral fold, nasolabial fold and zygomatic regions are affected.
- 1C: Mild forehead type-Only forehead is affected.
- 1D: Ala nasi alone is affected.
Type-2
- Moderate type-The lesions affect upper and lower eyelids, periocular, zygomatic, cheek and temple regions.
Type-3
- The condition is distributed over the scalp, forehead, eyebrows and nose.
Type 4
Bilateral type Nevus of Ito, also known as nevus fuscocaeruleus acromiodeltoideus is another dermal melanosis. This usually manifests as unilateral, asymptomatic, blue, gray or brown lesions 11. It was first described by Minor Ito in 1954 12. Nevus of Ito differs from the nevus of Ota only by its area of distribution and rarity. It affects the area of distribution of the posterior supraclavicular and cutaneous brachii lateralis nerves that encompass the supraclavicular, scapular or deltoid regions 5. Bilateral nevus of Ito is an extremely rare condition. In exceptional cases nevus of Ito may be present simultaneously with the nevus of Ota 13.
Type 5
- 5A: Unilateral nevus of Ito without nevus of Ota.
- 5B: Bilateral nevus of Ito without nevus of Ota.
Type 6
- 6A: Unilateral nevus of Ota with unilateral nevus of Ito (ipsilateral and contralateral)
- 6B: Bilateral nevus of Ota with unilateral nevus of Ito (ipsilateral and contralateral)
- 6C: Unilateral nevus of Ota (ipsilateral and contralateral) with bilateral nevus of Ito
As the nevi may be associated with extra cutaneous manifestations a letter “E” may be suffixed with the class (e.g., type 6C-E etc.) wherever it is applicable.
This proposed classification will put both nevi in a common platform as the underlying pathogenesis and pathology is same though the area of distribution is different. This will help to avoid a separate classification for the nevus of Ito. The addition of the letter “E” for extra cutaneous associated features will also give a complete idea regarding the disease and its magnitude of affection. Also the physician will be more vigilant while dealing with either of the nevi as far as the prognosis and management strategy is concerned as malignant transformation may rarely occur in both the nevi 17.
Nevus of Ota causes
The precise cause of Nevus of Ota is unknown. However, GNAQ or GNA11 mutations have been found in the dermal melanocytes seen in this condition. Researchers have suggested that hormones play a part in their development. The role of ultraviolet radiation is thought to be small, as it does not reach deep dermal melanocytes.
Nevus of Ota is much more common than nevus of Ito. These nevi are present at birth in 50% of cases but may appear during adolescence or adult life.
Nevus of Ota and Ito are most commonly found in Asian populations; 0.2–0.6% of Japanese people have a nevus of Ota. They appear more frequently in females. Both forms of nevi are uncommon in Caucasians.
Nevus of Ota symptoms
Nevus of Ota and nevus of Ito are all smooth, non-scaly blue-grey, blue-brown spots. They are usually small spots that connect to form larger continuous areas of pigmentation.
Nevus of Ota refers to a lesion, usually present at birth or young adulthood, on one side of the forehead and around the eye. Some people may also have pigment on the sclera (eyeball), cornea and inside the mouth including the palate.
Nevus of Ito occurs on the shoulder and upper arm region and is present at birth in the majority of instances. It may coexist with Nevus of Ota.
Nevus of Hori is a different condition but is similar to Nevus of Ota when examined under the microscope. Nevus of Hori is spotty rather than continuous and located on both sides of the face. It occurs more commonly in women and in Asian populations (especially East Asian). Small pinpoint discrete brown macules typically affect the prominence of the cheek but the lateral temples, eyelids and the nose may also be involved. Nevus of Hori is not present at birth and is therefore a form of acquired melanocytosis.
In all forms of dermal melanocytosis:
- Color may vary to include brown-violet, violet-blue or blue-green hues
- Nevi present in childhood may slowly grow and darken until adulthood is reached
- Color or perceived colour of naevi may change according to personal and environmental conditions, e.g. fatigue, menstruation, hot weather
- If affecting the eye, melanocytosis rarely causes glaucoma
- Malignant melanoma very rarely develops within dermal melanocytosis, and has usually been reported in Caucasians. Ocular melanoma has rarely been reported in the choroid, brain, orbit, iris, ciliary body, and optic nerve in association with a nevus of Ota.
Nevus of Ota diagnosis
Nevus of Ota is usually diagnosed after examining the color and pattern of the pigment. A small sample of skin (biopsy) may be taken to confirm the diagnosis and exclude other causes of pigmentation such as melasma, medication-induced pigmentation, lichen planus pigmentosus and post-inflammatory pigmentation.
Nevus of Ota treatment
Laser is the mainstay of treatment for Nevus of Ota. Quality(Q)-switched lasers [Neodymium:YAG (1064nm and/or 532nm), Ruby (694nm) or Alexandrite (755nm)] are usually used. Several treatments 2 to 3 months apart are required to lighten pigmentation. Risks involved with the treatment are low. Ten or more treatments are usually needed.
Newer picosecond laser technology may be helpful for this condition but further studies are required to prove this type of laser has any advantages over the abovementioned methods.
Photographs are taken at baseline and to assess progress during treatment.
If the eye is affected with pigmentation, review with an ophthalmologist should be arranged.
While camouflage with makeup is often cited as a treatment for this condition, cosmetically acceptable skin color matching is hard to achieve.
References- Cohen AB. 3rd ed. Philadelphia: Elsevier Mosby; 2005. Pediatric Dermatology; pp. 45–146.
- Paller AS, Mancini AJ. 3rd ed. Philadelphia: Elsevier Saunders; 2006. Hurwitz Clinical Pediatric Dermatology; pp. 297–9.
- Oculodermal melanocytosis (nevus of Ota). https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/oculodermal-melanocytosis/index.htm
- Mukhopadhyay AK. Unilateral Nevus of Ota with Bilateral Nevus of Ito and Palatal Lesion: A Case Report with a Proposed Clinical Modification of Tanino’s Classification. Indian J Dermatol. 2013;58(4):286–289. doi:10.4103/0019-5154.113943 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3726875
- Barnhill RL, Rabinovitz H. Benign melanocytic neoplasms. In: Bolognia JL, Jorizzo JL, Rapini R, editors. Dermatology. 2nd ed. Philadelphia: Mosby Elsevier; 2008. pp. 1720–2.
- Aurangabadkar S. QYAG5 Q-switched Nd: YAG laser treatment of nevus of Ota: An Indian study of 50 patients. J Cutan Aesth Surg. 2008;1:80–4.
- Hidano A, Kajima H, Ikeda S, Miyasato H, Nimamura M. Natural history of nevus of Ota. Arch Dermatol. 1967;95:187–95.
- Park JH, Lee MH. Acquired, bilateral nevus of Ota-like macules associated with Ota’s nevus: Case report. J Korean Med Sci. 2004;19:616–8.
- Tronnier M. Melanotic spots and melanocytic nevi. In: Burgdorf WH, Plewig G, Wolff HH, Landthaler M, editors. Braun-Falco’s Dermatology. 3rd ed. Heidelberg: Springer; 2009. pp. 1402–3.
- Gangopadhyay AK. Bilateral nevus of Ota. Indian J Dermatol Venereol Leprol. 1997;63:50–2.
- Mataix J, López N, Haro R, González E, Angulo A, Requena L. Late-onset Ito’s nevus: An uncommon acquired dermal melanocytosis. J Cutan pathol. 2007;34:640–3.
- Ito M. Nevus fusco-ceruleus acromio-deltoideus. Tohoku Exp Med. 1954;60:10.
- Mukhopadhyay AK. Nevus of Ota associated with nevus of Ito. Indan J Dermatol Venereol Leprol. 2004;70:112–3.
- Lapeere H, Boone B, Schepper SD, Verheghee E, Ongenae K, Geel NV, et al. Hypomelanoses and hypermelanoses. In: Wolf K, Goldsmith LA, Katz IS, Gilchrest BA, Paller A, Leffell DJ, editors. Fitzpatrick’s Dermatology in General Medicine. 7th ed. New York: McGraw-Hill; 2008. pp. 632–3.
- Chan HH, Lam LK, Wong DS. Nevus of Ota: A new classification based on the response to laser treatment. Lasers Surg Med. 2001;28:267–72.
- Tanino H. Nevus fuscocaeruleus ophthalmomaxillaris Ota. Jpn J Dermatol. 1939;46:435–51.
- Wise SR, Capra G, Martin P, Wallace D, Miller C. Malignant melanoma transformation within a nevus of Ito. J Am Acad Dermatol. 2010;62:869–74.