Lymph node infection
Lymph node infection also known as lymphadenitis, is the medical term for enlargement in one or more lymph nodes, usually due to infection. Lymph node infection is a complication of certain bacterial infections. Lymph nodes are small, ovoid nodules normally ranging in size from a few millimeters to 2 cm. Lymph nodes are distributed in clusters along the course of lymphatic vessels located throughout the body. The primary function of lymph nodes is to filter out microorganisms and abnormal cells that have collected in lymph fluid 1. Lymph nodes are filled with white blood cells that help your body fight infections. When lymph nodes become infected, it’s usually because an infection started somewhere else in your body. Rarely, lymph nodes can enlarge due to cancer.
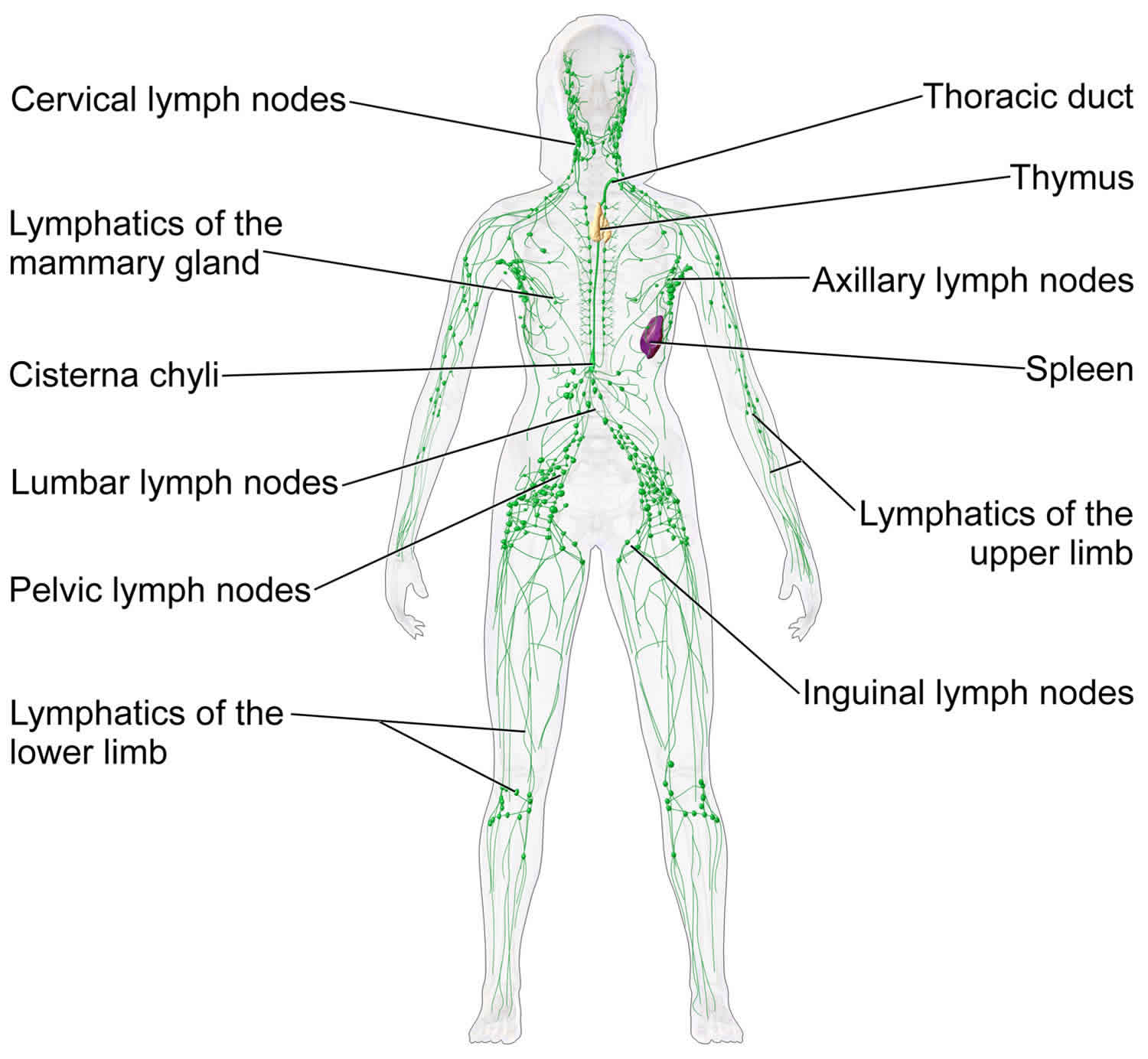
You have about 600 lymph nodes in your body, but normal lymph nodes may only be felt below your jaw, under your arms, and in your groin area.
A normal lymph node is small and firm. When lymph nodes become infected, they usually increase in size, become tender, and may be felt in other areas of your body during a physical exam.
Infections that spread to lymph nodes are usually caused by bacteria, a virus, or a fungus. It is important to learn how the infection spread into your lymph nodes so that the right treatment can be started.
Increased lymph node size may be caused by the following:
- Multiplication of cells within the node, including lymphocytes, plasma cells, monocytes, or histiocytes
- Infiltration of cells from outside the node, such as malignant cells or neutrophils
- Draining of an infection (eg, abscess) into local lymph nodes
Lymph node infection can be one of two types:
- Localized lymphadenitis. This is the most common type. Localized lymphadenitis involves one or just a few nodes that are close to the area where the infection started. For example, nodes enlarged because of a tonsil infection may be felt in the neck area.
- Generalized lymphadenitis. This type of lymph node infection occurs in two or more lymph node groups and may be caused by an infection that spreads through the bloodstream or another illness that affects the whole body.
Lymphadenitis key points
- Lymphadenitis is an infection in one or more lymph nodes.
- When lymph nodes become infected, it’s usually because an infection started somewhere else in your body.
- Lymphadenitis can cause lymph nodes to become enlarged, red, or tender.
- Treatment may include antibiotics, and medications to control pain and fever.
- Early treatment of infections can prevent the development of lymphadenitis.
Lymph node infection causes
The lymph system (lymphatics) is a network of lymph nodes, lymph ducts, lymph vessels, and organs that produce and move a fluid called lymph from tissues to the bloodstream.
The lymph glands, or lymph nodes, are small structures that filter the lymph fluid. There are many white blood cells in the lymph nodes to help fight infection. When lymph nodes become infected, it’s usually because an infection started somewhere else in your body.
Lymphadenitis occurs when the lymph glands become enlarged by swelling (inflammation), often in response to bacteria, viruses, or fungi. The swollen glands are usually found near the site of an infection, tumor, or inflammation.
Lymphadenitis may occur after skin infections or other infections caused by bacteria such as streptococcus or staphylococcus. Sometimes, it is caused by rare infections such as tuberculosis or cat scratch disease (bartonella).
Infectious agents causes and lymphadenitis characteristics are as follows 2:
- Bartonella henselae (catscratch disease) – Single-node involvement determined by scratch site; discrete, mobile, nontender
- Coccidioides immitis (coccidioidomycosis) – Mediastinal
- Cytomegalovirus – Generalized
- Dental caries/abscess – Submaxillary
- Epstein-Barr virus (mononucleosis) – Anterior cervical, mediastinal, bilateral; discrete, firm, nontender
- Francisella tularensis (tularemia) – Cervical, mediastinal, or generalized; tender
- Histoplasma capsulatum (histoplasmosis) – Mediastinal
- Atypical Mycobacterium – Cervical, submandibular, submental (usually unilateral); most commonly in immunocompetent children aged 1-5 years 3
- Mycobacterium tuberculosis – Mediastinal, mesenteric, anterior cervical, localized disease (discrete, firm, mobile, tender); generalized hematogenous spread (soft, fluctuant, matted, and adhere to overlying, erythematous skin)
- Parvovirus – Posterior auricular, posterior cervical, occipital
- Rubella – Posterior auricular, posterior cervical, occipital
- Salmonella – Generalized
- Seborrheic dermatitis, scalp infections – Occipital, postauricular
- Staphylococcus aureus adenitis – Cervical, submandibular; unilateral, firm, tender
- Group A streptococcal pharyngitis – Submandibular and anterior cervical; unilateral, firm, tender
- Toxoplasma gondii – Generalized, often nontender
- Viral pharyngitis – Bilateral postcervical; firm, tender
- Yersinia enterocolitica – Cervical or abdominal
- Yersinia pestis (plague) – Axillary, inguinal, femoral, cervical; extremely tender with overlying erythema
Immunologic or connective tissue disorders causing lymphadenitis are as follows:
- Juvenile rheumatoid arthritis
- Graft versus host disease
Primary diseases of lymphoid or reticuloendothelial tissue causing lymphadenitis are as follows:
- Acute lymphoblastic leukemia
- Lymphosarcoma
- Reticulum cell sarcoma
- Non-Hodgkin lymphoma
- Malignant histocytosis or histocytic lymphoma
- Nonendemic Burkitt tumor
- Nasopharyngeal rhabdomyosarcoma
- Neuroblastoma
- Thyroid carcinoma, chronic lymphocytic thyroiditis
- Histiocytosis X
- Kikuchi disease
- Benign sinus histiocytosis
- Angioimmunoblastic or immunoblastic lymphadenopathy
- Chronic pseudolymphomatous lymphadenopathy (chronic benign lymphadenopathy)
Immunodeficiency syndromes and phagocytic dysfunction causing lymphadenitis are as follows:
- Chronic granulomatous disease of childhood
- Acquired immunodeficiency syndrome
- Hyperimmunoglobulin E (Job) syndrome
Metabolic and storage diseases causing lymphadenitis are as follows:
- Gaucher disease
- Niemann-Pick disease
- Cystinosis
Hematopoietic diseases causing lymphadenitis are as follows:
- Sickle cell anemia
- Thalassemia
- Congenital hemolytic anemia
- Autoimmune hemolytic anemia
Miscellaneous disorders causing lymphadenitis are as follows:
- Kawasaki disease
- PFAPA (periodic fever, aphthous stomatitis, pharyngitis, and adenitis) syndrome
- Sarcoidosis
- Castleman disease (also known as benign giant lymph node hyperplasia)
Medications causing lymphadenitis are as follows:
- Mesantoin – most commonly causes cervical lymphadenitis
- Hydantoin – Generalized lymphadenopathy.
Regional lymphadenitis
In a patient with regional lymphadenitis, knowledge of lymphatic drainage patterns and pathologic processes most likely to affect these areas can facilitate diagnostic investigation 4.
Cervical lymph nodes
Cervical lymph nodes receive lymphatic drainage from the head, neck, and oropharyngeal cavities.
Infections associated with cervical lymph nodes are as follows 5:
- Skin and soft tissue infections of the face
- Dental abscesses
- Otitis externa
- Bacterial pharyngitis
- Cytomegalovirus
- Adenovirus infection
- Rubella
- Toxoplasmosis
Malignancies associated with cervical lymph nodes are as follows:
- Hodgkin lymphoma
- Non-Hodgkin lymphomas
- Squamous cell carcinomas of nasopharyngeal or laryngeal structures
Axillary lymph nodes
Axillary lymph nodes receive lymphatic drainage from upper extremities and breasts.
Infections associated with axillary lymph nodes are as follows:
- Bartonella henselae infection (catscratch disease)
- Sporotrichosis
- Tularemia
- Staphylococcal or streptococcal skin infections
Malignancies associated with axillary lymph nodes are as follows:
- Lymphoma
- Melanoma
- Carcinoma of the breast
Epitrochlear lymph nodes
Epitrochlear lymph nodes receive lymphatic drainage from the hands.
Infections associated with epitrochlear lymph nodes are as follows:
- Skin and soft tissue infections from local trauma
Malignancies associated with epitrochlear lymph nodes are as follows:
- Lymphoma
Supraclavicular lymph nodes
Supraclavicular lymph nodes receive lymphatic drainage from the chest and mediastinum.
Infections associated with supraclavicular lymph nodes are as follows:
- Intrathoracic mycobacterial, fungal infections (not bacterial pneumonias or bronchial infections)
Malignancies associated with supraclavicular lymph nodes are as follows (Note: supraclavicular lymphadenitis is an ominous sign of malignancy):
- Intrathoracic and intra-abdominal malignancies (Note: left-sided supraclavicular sentinel node or the Virchow node is highly suggestive of an occult abdominal neoplasm.)
- Breast cancer
Other diseases associated with supraclavicular lymph nodes are as follows:
- Sarcoidosis
Inguinal lymph nodes
Inguinal lymph nodes receive lymphatic drainage from the lower extremities and skin of the lower abdomen, genitals, and perineum 6.
Infections associated with inguinal lymph nodes are as follows:
- Cellulitis of the lower extremities
- Venereal infections – Syphilis, chancroid, herpes simplex virus infection, lymphogranuloma venereum
Malignancies associated with inguinal lymph nodes are as follows:
- Lymphomas
- Metastatic melanomas from lower extremity primary site
- Squamous cell carcinomas from genital primary site
Note: lymphatic drainage from internal pelvic organs and testes drain via iliac nodes into the para-aortic chain. Therefore, deep pelvic infections or malignancies do not present as inguinal lymphadenitis.
Hilar or mediastinal lymph nodes
Hilar or mediastinal lymph nodes receive lymph drainage from local structures and are usually found on radiologic examination.
Infections associated with hilar or mediastinal lymph nodes are as follows:
- Tuberculosis
- Fungal infections
Malignancies associated with hilar or mediastinal lymph nodes are as follows:
- Bronchogenic carcinoma
- Lymphoma
- Hodgkin lymphoma
Other diseases associated with hilar or mediastinal lymph nodes are as follows:
- Sarcoidosis
Intra-abdominal or retroperitoneal lymph nodes
Intra-abdominal or retroperitoneal lymph nodes receive lymph drainage from local structures, these are typically detected by finding a palpable mass on physical examination or by obstructive/pressure effects on surrounding structures.
Infections associated with intra-abdominal or retroperitoneal lymph nodes are as follows:
- Tuberculosis 7
- Yersinia enterocolitica infection
- Deep abscess
Malignancies associated with intra-abdominal or retroperitoneal lymph nodes are as follows:
- Hodgkin lymphoma (pelvic and retroperitoneal nodes)
- Non-Hodgkin lymphoma (mesenteric nodes)
Generalized lymphadenitis
In a patient with generalized lymphadenitis, the differential includes systemic conditions.
Associated medication toxicities are as follows:
- Hydralazine
- Allopurinol
Associated infections are as follows:
- Epstein-Barr virus infection
- Cytomegalovirus infection
- Toxoplasmosis
- HIV disease
- Tuberculosis (advanced)
- Histoplasmosis
- Coccidioidomycosis
- Brucellosis
- Bacterial endocarditis
- Hepatitis
- Syphilis (secondary)
Associated immunologic diseases are as follows:
- Sarcoidosis
- Rheumatoid arthritis
- Lupus
Associated malignancies are as follows:
- Acute lymphoblastic leukemia
- Chronic lymphocytic leukemia
- Lymphomas
- Angiofollicular lymph node hyperplasia (Castleman disease)
Lymph node infection symptoms
The symptoms of lymphadenitis may look like other medical conditions or problems. Always see your healthcare provider for a diagnosis.
The main symptom of lymphadenitis is enlarged lymph nodes. A lymph node is considered enlarged if it is about one-half inch wide. Symptoms caused by an infected lymph node or group of nodes may include:
- Lymph nodes that increase in size
- Lymph nodes that are painful to touch
- Lymph nodes that are soft or matted together
- Redness or red streaking of the skin over lymph nodes
- Lymph nodes that are filled with pus (an abscess)
- Fluid that drains from the lymph nodes to the skin
- Swollen, tender, or hard lymph nodes
- Fever
Lymph nodes may feel rubbery if an abscess (pocket of pus) has formed or they have become inflamed.
Cervical lymphadenitis can lead to neck stiffness and torticollis.
Preauricular adenopathy is associated with several forms of conjunctivitis, including unilocular granulomatous conjunctivitis (catscratch disease, chlamydial conjunctivitis, listeriosis, tularemia, or tuberculosis), pharyngeal conjunctival fever (adenovirus type 3 infection) and keratoconjunctivitis (adenovirus type 8 infection).
Retropharyngeal node inflammation can cause dysphagia or dyspnea.
Mediastinal lymphadenitis may cause cough, dyspnea, stridor, dysphagia, pleural effusion, or venous congestion.
Intra-abdominal (mesenteric and retroperitoneal) adenopathy can manifest as abdominal pain.
Iliac lymph node involvement may cause abdominal pain and limping.
Lymph node infection possible complications
Untreated lymph node infection may lead to:
- Abscess formation
- Cellulitis (a skin infection)
- Fistulas (seen in lymphadenitis that is due to tuberculosis)
- Sepsis (bloodstream infection)
Lymph node infection diagnosis
If you have lymphadenitis, the most important parts of your diagnosis are usually your history and the physical exam done by your healthcare provider. You may be asked about your symptoms, such as chills and fever, any recent travel, any breaks in your skin, and recent contact with cats or other animals. Then, during the physical exam, your healthcare provider will look for signs of infection near the enlarged lymph nodes. This includes feeling your lymph nodes and looking for signs of injury or infection around any swollen lymph nodes.
These tests may be needed to help make the diagnosis 8:
- Blood tests to look for infection.
- Blood cultures may reveal spread of infection (often bacteria) to the bloodstream.
- A biopsy (taking a sample of tissue) from the lymph node or fluid from inside the lymph node to study under a microscope
- Culture of aspirated tissue or biopsy specimen – To determine the causative organism and its sensitivity to antibiotics
- Gram stain of aspirated tissue – to evaluate bacterial causes
- Monospot or Epstein-Barr virus (EBV) serologies – to confirm the diagnosis of infectious mononucleosis
- Bhenselae serologies – to confirm the diagnosis of catscratch disease (if exposed to cats)
- Skin testing or purified protein derivative (PPD) – to confirm the diagnosis of tuberculous lymphadenopathy; alternative is interferon-gamma release assays (IGRA) 9
- Complete blood cell count (CBC count) – elevated white blood cell count may indicate an infectious etiology
- Erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) – elevated ESR and CRP are nonspecific indicators of inflammation
- Liver function tests – may indicate hepatic or systemic involvement; elevated transaminase levels can be seen in infectious mononucleosis
Imaging studies
Ultrasonography may be useful for verifying lymph node involvement and taking accurate measurements of enlarged nodes. A study by Wang et al 10 indicated that endobronchial ultrasonography can aid in differentiating between nonmalignant intrathoracic lymphadenopathies, including tuberculosis, sarcoidosis, and reactive lymphadenitis. The investigators found that the presence of reactive lymphadenitis is predicted by the existence of central hilar structure and a lack of clustered formation, as well as by vascular pattern (hilar perfusion or avascularity). Best diagnostic accuracies of 77.1%, 89.2%, and 87.1% were found for tuberculous nodes, sarcoid nodes, and reactive lymphadenitis, respectively 10.
Chest radiography may be helpful in determining pulmonary involvement or spread of lymphadenopathy to the chest.
Lymph node infection treatment
Lymphadenitis may spread within hours. Treatment should begin right away. However, the exact type of treatment depends on what type of infection has spread into your lymph nodes. Once an infection has spread into some lymph nodes, it can spread quickly to others and to other parts of your body, so it’s important to find the cause of the infection and start treatment quickly.
Treatment for lymphadenitis may include:
- Antibiotics given by mouth or injection to fight an infection caused by bacteria
- Medicine to control pain and fever e.g., analgesics or painkillers
- Anti-inflammatory medicines to reduce inflammation and swelling
- Cool compresses to reduce inflammation and pain
- Surgery may be needed to drain a lymph node that has filled with pus.
Antimicrobial therapy is used when nodes are greater than 2-3 cm, are unilateral, have overlying erythema, and are tender. Antibiotics should target common infectious causes of lymphadenopathy, including Staphylococcus aureus and group A Streptococcus. Owing to the increasing prevalence of community-acquired methicillin-resistant Staphylococcus aureus (MRSA), empiric therapy with clindamycin should be considered 11. Trimethoprim-sulfamethoxazole is often effective for methicillin-resistant Staphylococcus aureus (MRSA) infection, but it is not appropriate for group A Streptococcus infections.
Chemotherapy and radiotherapy are used for treatment of cancers.
Lymph node infection prognosis
Prompt treatment with antibiotics usually leads to a complete recovery. It may take weeks, or even months, for swelling to disappear.
References- Boldt DH. Lymphadenopathy and Splenomegaly, Internal Medicine, Stein. 5th Ed. 1998. Chapter 81.
- Pasternack MS, Marton NS. Lymphadenitis and Lymphangitis, Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. 2010. Chapter 92.
- Loizos A, Soteriades ES, Pieridou D, Koliou MG. Lymphadenitis by non-tuberculous mycobacteria in children. Pediatr Int. 2018 Dec. 60 (12):1062-1067.
- Friedmann AM. Evaluation and management of lymphadenopathy in children. Pediatr Rev. 2008 Feb. 29(2):53-60.
- Peters TR, Edwards KM. Cervical lymphadenopathy and adenitis. Pediatr Rev. 2000 Dec. 21(12):399-405.
- Sejben I, Rácz A, Svébis M, Patyi M, Cserni G. Petroleum jelly-induced penile paraffinoma with inguinal lymphadenitis mimicking incarcerated inguinal hernia. Can Urol Assoc J. 2012 Aug. 6(4):E137-9.
- Raoot A, Dev G. Assessment of Status of rpoB Gene in FNAC Samples of Tuberculous Lymphadenitis by Real-Time PCR. Tuberc Res Treat. 2012. 2012:834836
- Leung AK, Davies HD. Cervical lymphadenitis: etiology, diagnosis, and management. Curr Infect Dis Rep. 2009 May. 11(3):183-9.
- Willemse SH, Oomens MAEM, De Lange J, Karssemakers LHE. Diagnosing nontuberculous mycobacterial cervicofacial lymphadenitis in children: A systematic review. Int J Pediatr Otorhinolaryngol. 2018 Sep. 112:48-54.
- Wang L, Wu W, Teng J, Zhong R, Han B, Sun J. Sonographic Features of Endobronchial Ultrasound in Differentiation of Benign Lymph Nodes. Ultrasound Med Biol. 2016 Sep 7.
- Guss J, Kazahaya K. Antibiotic-resistant Staphylococcus aureus in community-acquired pediatric neck abscesses. Int J Pediatr Otorhinolaryngol. 2007 Jun. 71(6):943-8.