What is a mandible
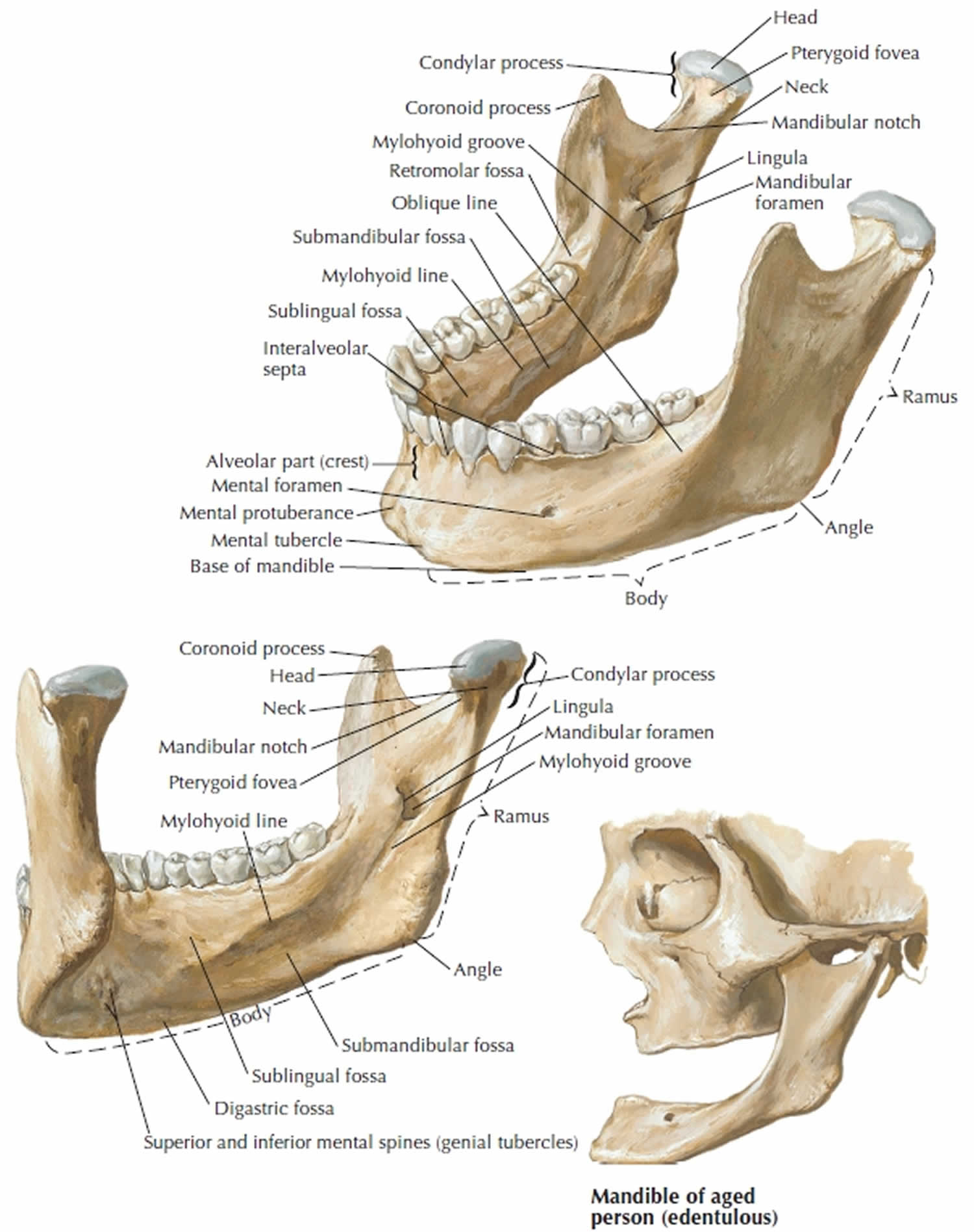
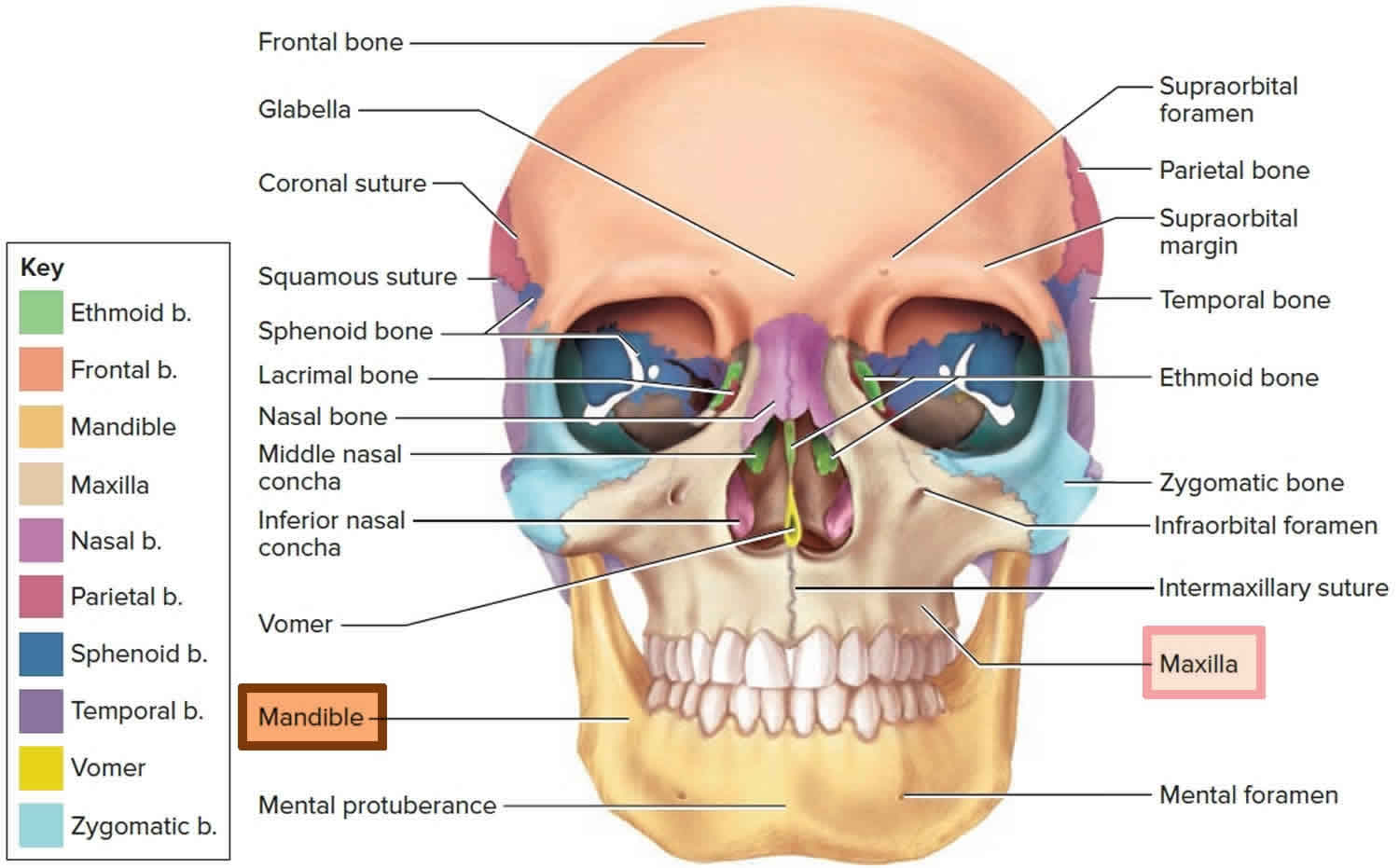
The mandible is a U-shaped lower jawbone and the largest, strongest bone in the face (Figures 1 and 2) and the only one that can move significantly. The mandible articulates with the neurocranium at the temporomandibular joints (TMJs). Mandible supports the lower teeth and provides attachment for muscles of mastication and facial expression. The mandible is a vital bone in terms of forensic evidence. Because the mandible progressively changes over an individual’s life, it is routinely used to determine the age of the deceased 1.
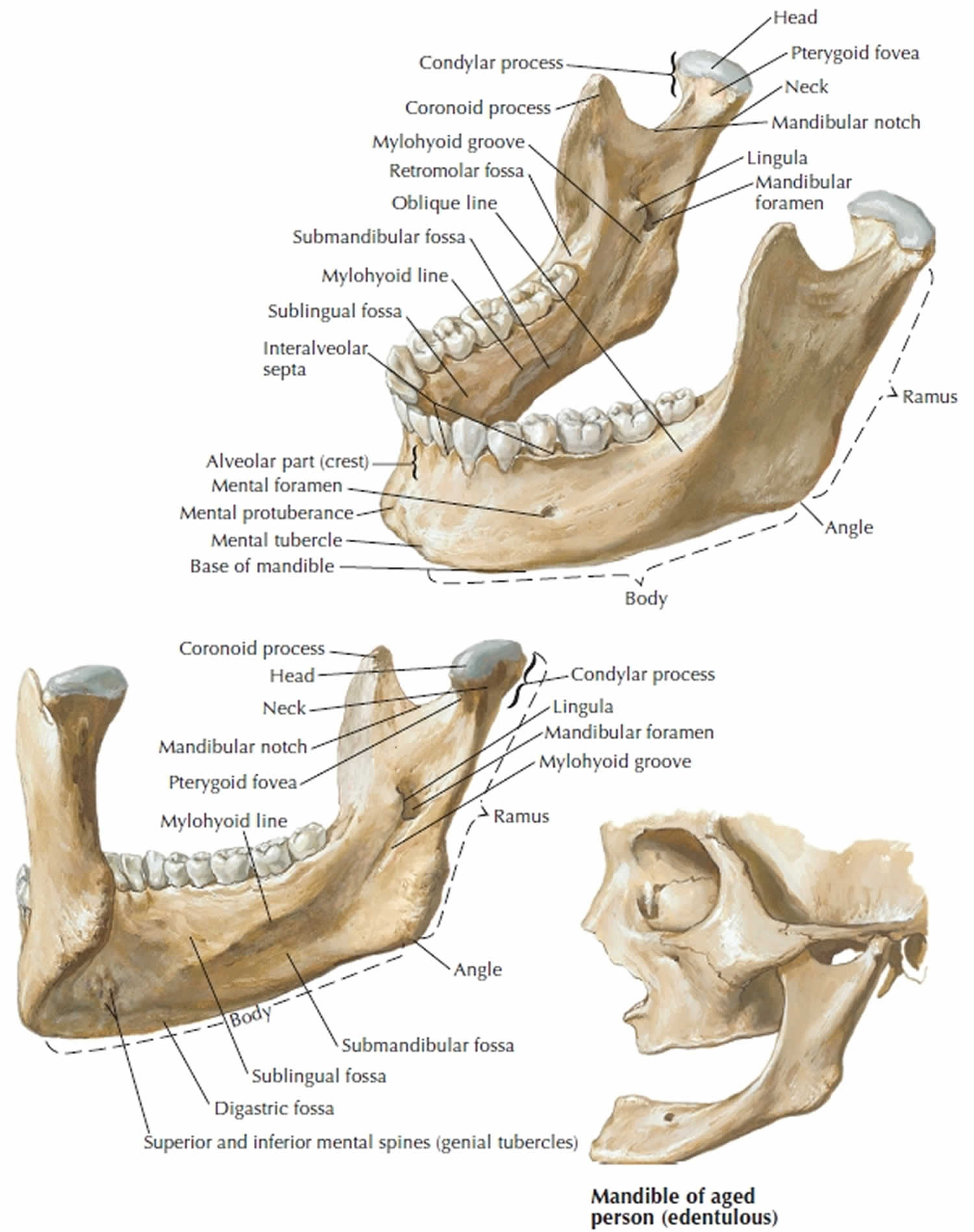
The horizontal portion, bearing the teeth, is called the body; the vertical to oblique posterior portion is the ramus (plural, rami); and these two portions meet at a corner called the angle of mandible. The mandible develops as separate right and left bones in the fetus, joined by a median cartilaginous joint called the mental symphysis at the point of the chin. This joint ossifies in early childhood, uniting the two halves into a single bone. The point of the chin itself is called the mental protuberance. The mental protuberance at this junction forms the chin. The inner (posterior) surface of the mandible in this region has a pair of small points, the mental spines, which serve for attachment of certain chin muscles (see Figure 1).
At the superior margin of each ramus are two processes. The anterior coronoid process (“crown-shaped”) is a flat, triangular projection. The temporalis muscle, which elevates the lower jaw during chewing, inserts here. The posterior condylar process enlarges superiorly to form the head of the mandible. It articulates with the temporal bone to form the temporomandibular joint. The coronoid and condylar processes are separated by the mandibular notch.
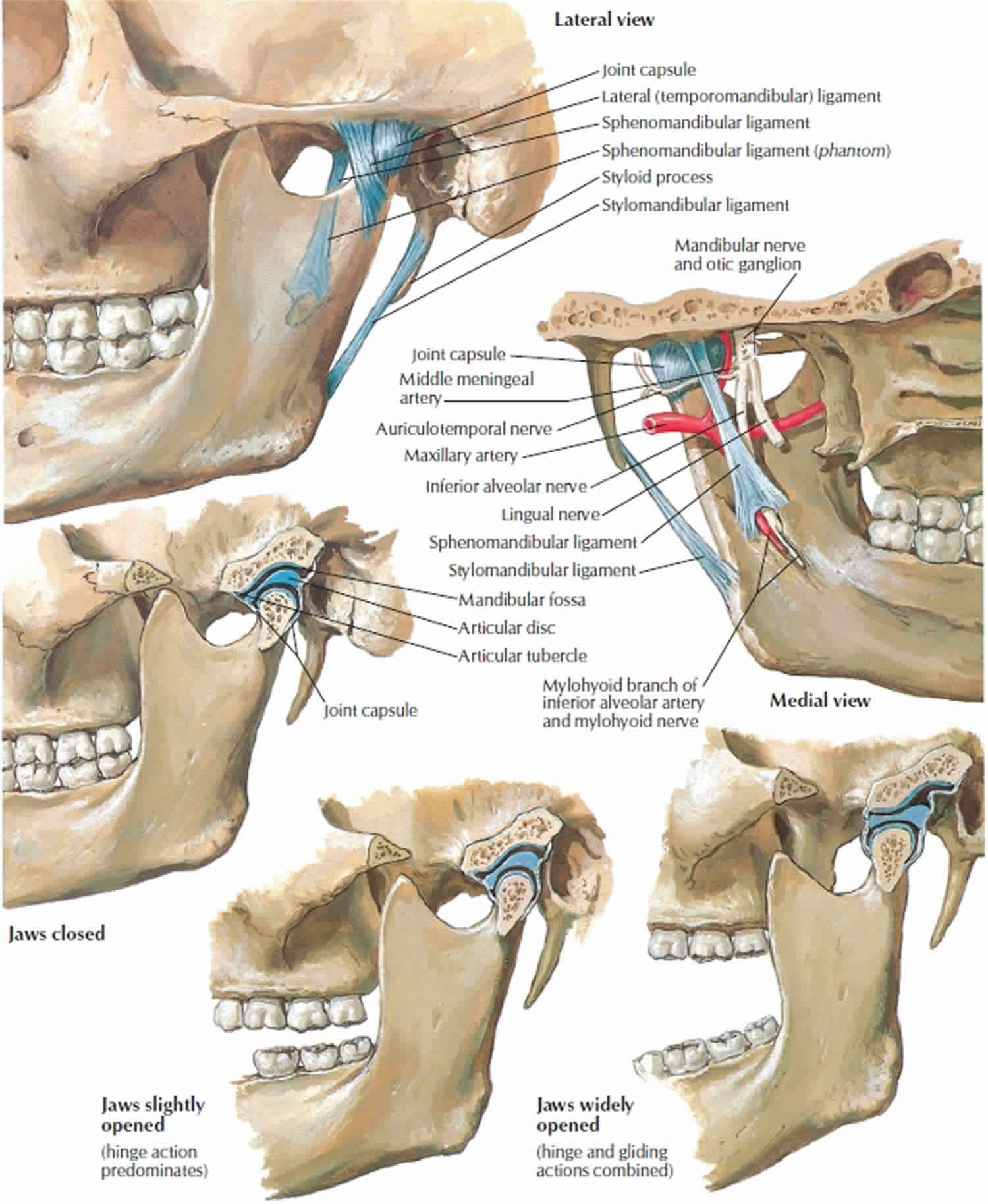
The temporomandibular joint is a specialized joint between the mandible and the temporal bone of the skull (see Figure 3 below). The condyle of the mandible articulates bilaterally in a concavity known as the glenoid fossa or the mandibular fossa. Biomechanics of the temporomandibular joint is under neuromuscular control, comprising the muscles of mastication, the ligaments associated with it, and neural transmission carried by the mandibular division of the trigeminal nerve (cranial nerve 5 or V).
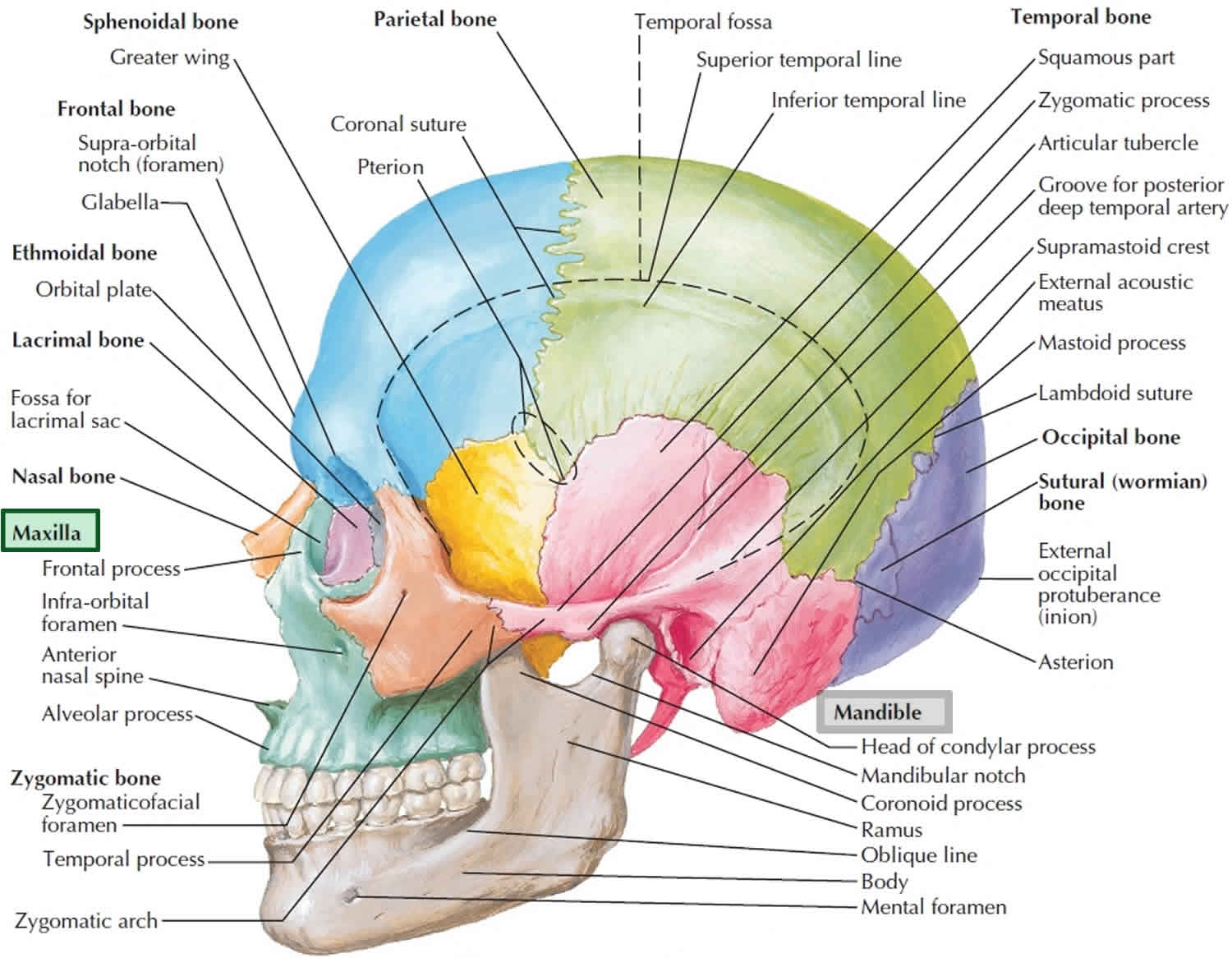
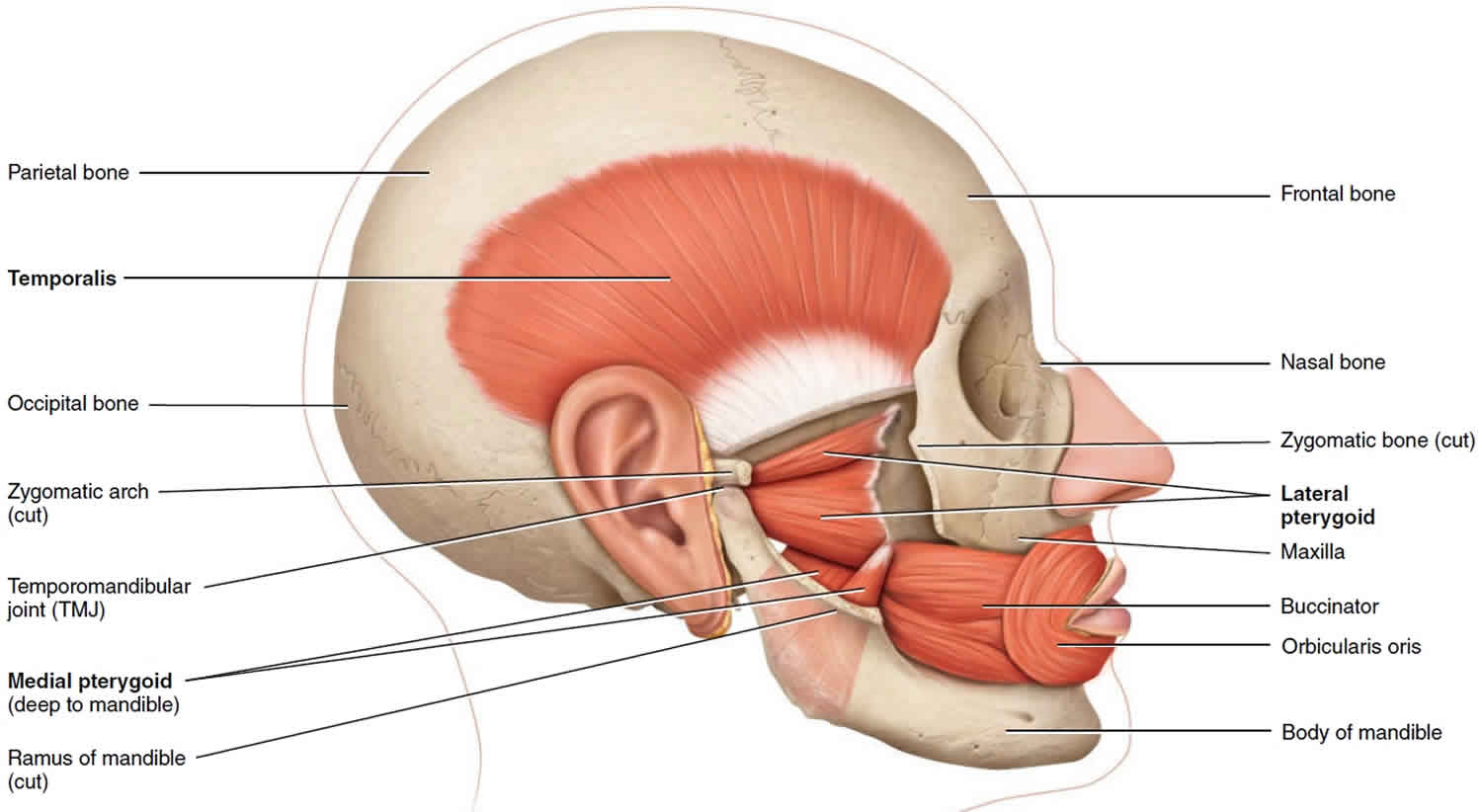
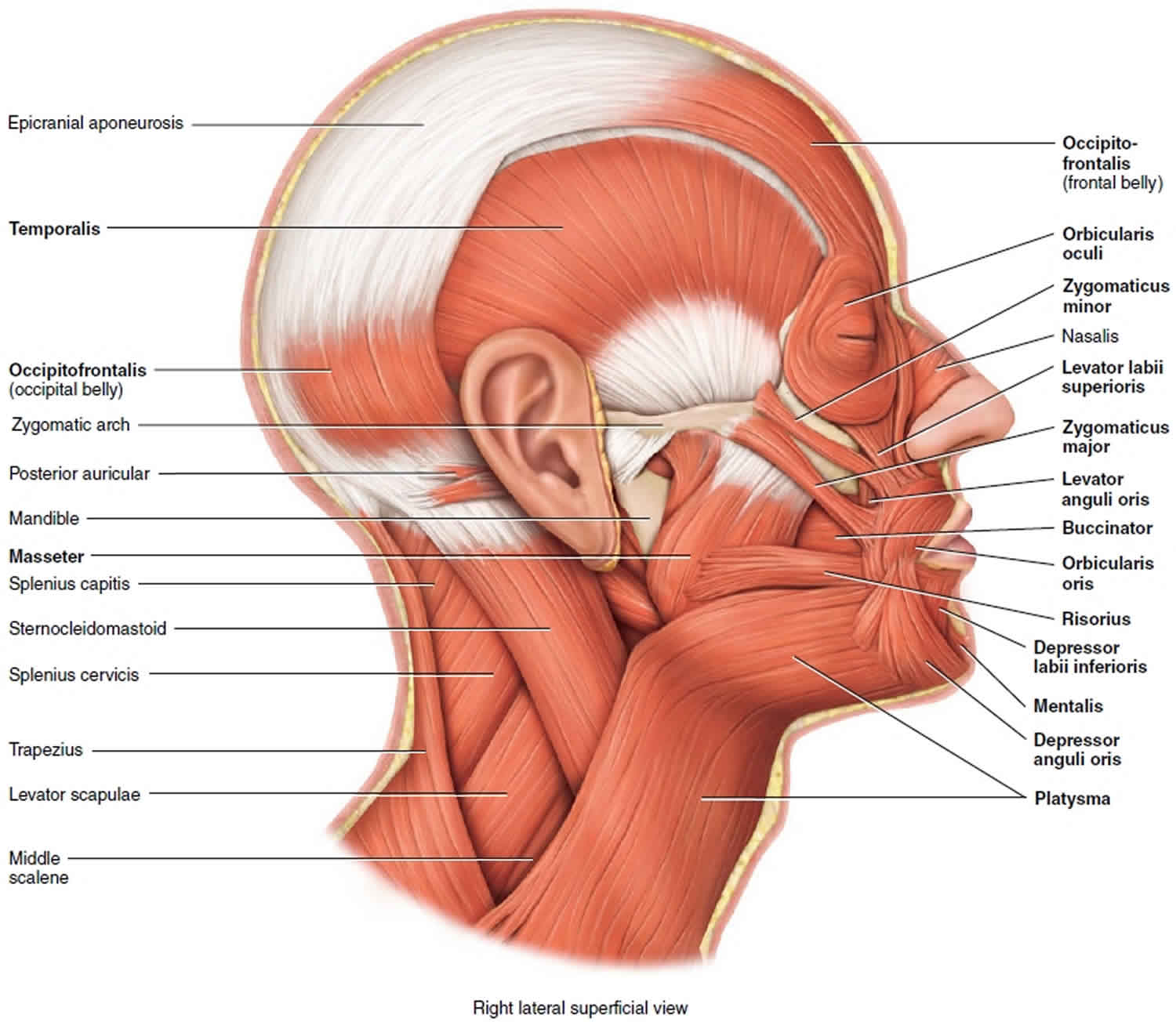
The muscles that move the mandible (lower jawbone) at the temporomandibular joint (TMJ) are known as the muscles of mastication (chewing) (Figure 4). Of the four pairs of muscles involved in mastication, three are powerful closers of the jaw and account for the strength of the bite: masseter, temporalis, and medial pterygoid. Of these, the masseter is the strongest muscle of mastication. The medial and lateral pterygoid muscles assist in mastication by moving the mandible from side to side to help grind food. Additionally, the lateral pterygoid muscles protract (protrude) the mandible. The masseter muscle has been removed in Figure 4 to illustrate the deeper pterygoid muscles; the masseter can be seen in Figure 5. Note the enormous bulk of the temporalis and masseter muscles compared to the smaller mass of the two pterygoid muscles.
Three of the four muscles of mastication close the mandible and only the lateral pterygoid opens the mouth. The force of gravity on the mandible off sets this imbalance. When the masseter, temporalis, and medial pterygoid muscles relax, the mandible drops. Now you know why the mouth of many persons, particularly the elderly, is open while the person is asleep in a chair. In contrast, astronauts in zero gravity must work hard to open their mouths.
The tongue is a highly mobile structure that is vital to digestive functions such as mastication (chewing), detection of taste, and deglutition (swallowing). It is also important in speech. The tongue’s mobility is greatly aided by its attachment to the mandible, styloid process of the temporal bone, and hyoid bone.
Physiologic Variants
Males generally have squarer, more prominent mandibles than females. This is due to the larger size of the mental protuberance in males and the decreased gonial angle. The gonial angle is 90 degrees in males, compared to 110 in females.
In rare instances, a bifid or trifid inferior alveolar canal may be present. This can be detected on X-ray as a second or third mandibular canal. Branches of the inferior alveolar nerve commonly run through these extra foramina and can confer a risk for inadequate anesthesia during surgical procedures involving the mandible 2.
A cleft chin can result from inadequate or absent fusion of the mandibular symphysis during embryonic development. This often results in a depression of the overlying soft tissue at the midline of the mandible. This is a genetic condition that is inherited in an autosomal dominant fashion and found more frequently in the male population 3.
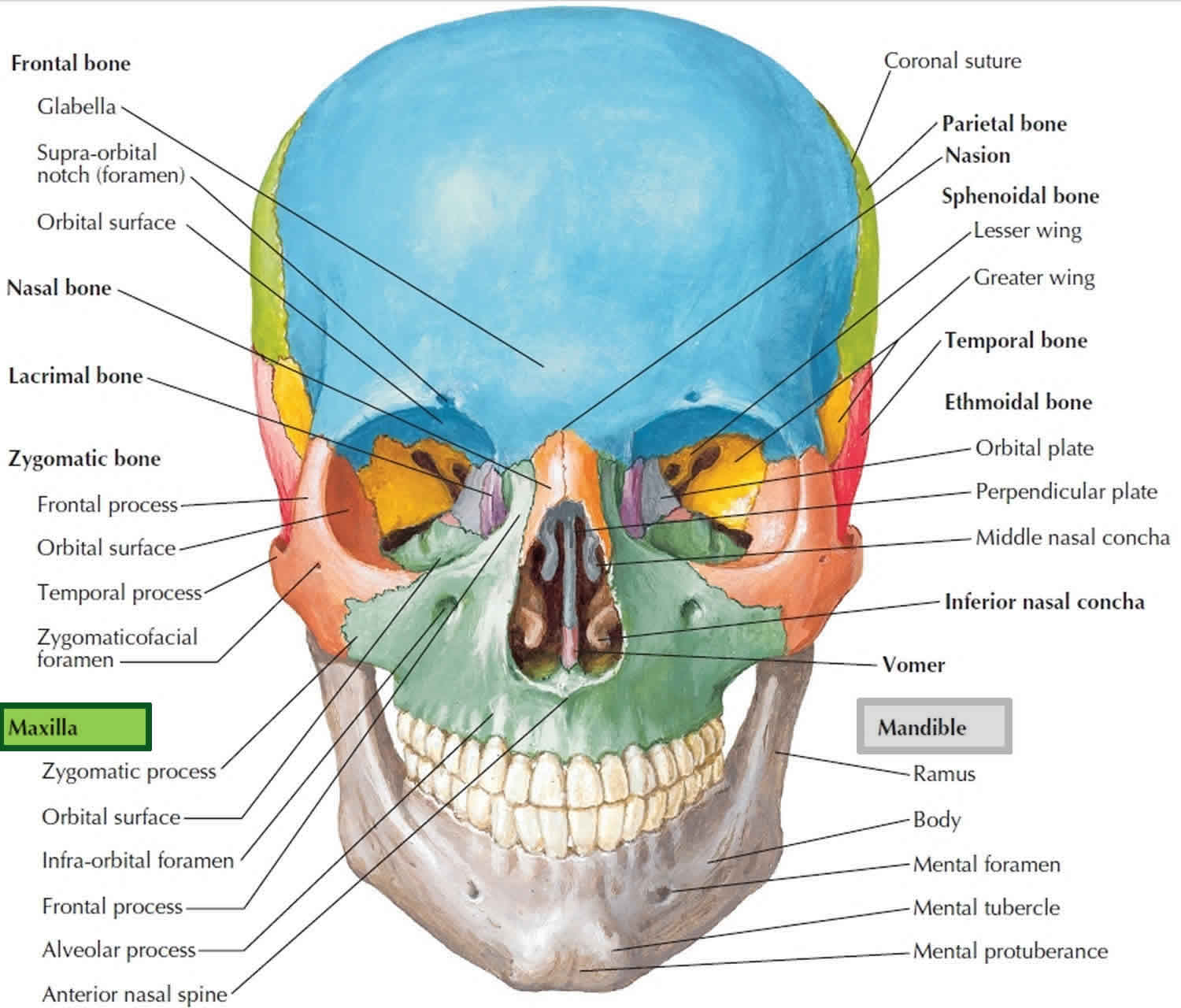
Figure 1. Mandible anatomy
Figure 2. Mandible and skull
Parts of mandible
The mandible is made up of the following parts: The body and two rami.
Body of mandible
The body is the anterior portion of the mandible and is bound by two surfaces and two borders. The body ends and the rami begin on either side at the angle of the mandible, also known as the gonial angle.
- External surface: The external surface contains the mandibular symphysis at midline, detected as a subtle ridge in the adult. The inferior portion of the ridge divides and encloses a midline depression called the mental protuberance. The edges of the mental protuberance are elevated, forming the mental tubercle. Laterally to the ridge and below the incisive teeth is a depression known as the incisive fossa. Below the second premolar is the mental foramen, in which the mental nerve and vessels exit. The oblique line courses posteriorly from the mental tubercle to the anterior border of the ramus.
- Internal surface: The internal surface contains the median ridge at midline and mental spines, which are just lateral to the ridge. The mylohyoid line begins at midline and courses superiorly and posteriorly to the alveolar border.
- Alveolar border: The alveolar border, which is the superior border, contains the hollow cavities in which the lower sixteen teeth reside.
- Inferior border: The inferior border creates the lower jawline and contains a small groove in which the facial artery passes.
Ramus of mandible
The ramus contributes to the lateral portion of the mandible on either side. The coronoid process and condyloid process are located at the superior aspect of the ramus. The coronoid process is anterior and the condyloid process is posterior; the two are separated by the mandibular notch. The ramus is bound by two surfaces and four borders and contains two processes.
- Lateral surface: The lateral surface contains a portion of the oblique line, which began on the external surface of the body. This surface also provides the origin for the masseter muscle.
- Medial surface: The medial surface contains the mandibular foramen through which the inferior alveolar nerve and inferior alveolar artery enter and subsequent course the mandibular canal. At the anterosuperior aspect of the mandibular foramen is a sharp process called the lingula of the mandible. At the posteroinferior aspect of the mandibular foramen is the mylohyoid groove, against which the mylohyoid vessels run.
- Superior border: The superior border which gives rise to the coronoid and condyloid processes.
Inferior border: The inferior border is continuous with the inferior border of the mandibular body and contributes to the jawline. - Posterior border: The posterior border is continuous with the inferior border of the ramus and is deep to the parotid gland. This border is used in conjunction with the inferior border of the mandibular body to determine the gonial angle.
- Anterior border: The anterior border is continuous with the oblique line of the external surface of the body.
Coronoid Process
The coronoid process is located at the superior aspect of the ramus. Its anterior border is continuous with that of the ramus, and its posterior border creates the anterior boundary of the mandibular notch. The temporalis muscle and masseter insert on its lateral surface.
Condyloid Process
The condyloid process is also located at the superior aspect of the ramus and is divided into two parts, the neck and the condyle. The neck is the thinner portion of the condyloid process that projects from the ramus. The condyle is the most superior portion and contributes to the temporomandibular junction by articulating with the articular disk.
Figure 3. Temporomandibular joints (TMJs)
Figure 4. Muscles that move the mandible
Figure 5. Muscles that move the mandible
Mandible anatomy
The body of the mandible anchors the lower teeth and forms the chin. Its superior border is the alveolar process. The tooth sockets, called alveoli, open onto this surface. Anteriorly, the two halves of the mandible fuse at the mandibular symphysis. The mental protuberance at this junction forms the chin. Several openings pierce the mandible. On the medial surface of each ramus is a mandibular foramen, through which a nerve responsible for tooth sensation (inferior alveolar nerve, a branch of cranial nerve V) enters the mandibular body and supplies the roots of the lower teeth. Dentists inject anesthetic into this foramen before working on the lower teeth. The mental (“chin”) foramen, which opens on the anterolateral side of the mandibular body, transmits blood vessels and nerves to the lower lip and the skin of the chin.
- Mental foramen: Mental nerve and vessels
- Mandibular foramen: Inferior alveolar nerves and vessels to the lower teeth
The inner surface of the body has a number of shallow depressions and ridges to accommodate muscles and salivary glands. The angle of the mandible has a rough lateral surface for insertion of the masseter, a muscle of mastication. Like the maxilla, the mandible has pointed alveolar processes between the teeth.
The ramus is somewhat Y-shaped. Its posterior branch, called the condylar process, bears the mandibular condyle—an oval knob that articulates with the mandibular fossa of the temporal bone. The meeting of this condyle with the temporal bone forms a hinge, the temporomandibular joint (TMJ). The anterior branch of the ramus is a blade called the coronoid process. It is the point of insertion for the temporalis muscle, which pulls the mandible upward when you bite. The U-shaped arch between the two processes is the mandibular notch. Just below the notch, on the medial surface of the ramus, is the mandibular foramen. The nerve and blood vessels that supply the lower teeth enter this foramen and then travel through the bone of the mandibular body, giving off branches to each tooth along the way. Dentists commonly inject lidocaine near the mandibular foramen to deaden sensation from the lower teeth.
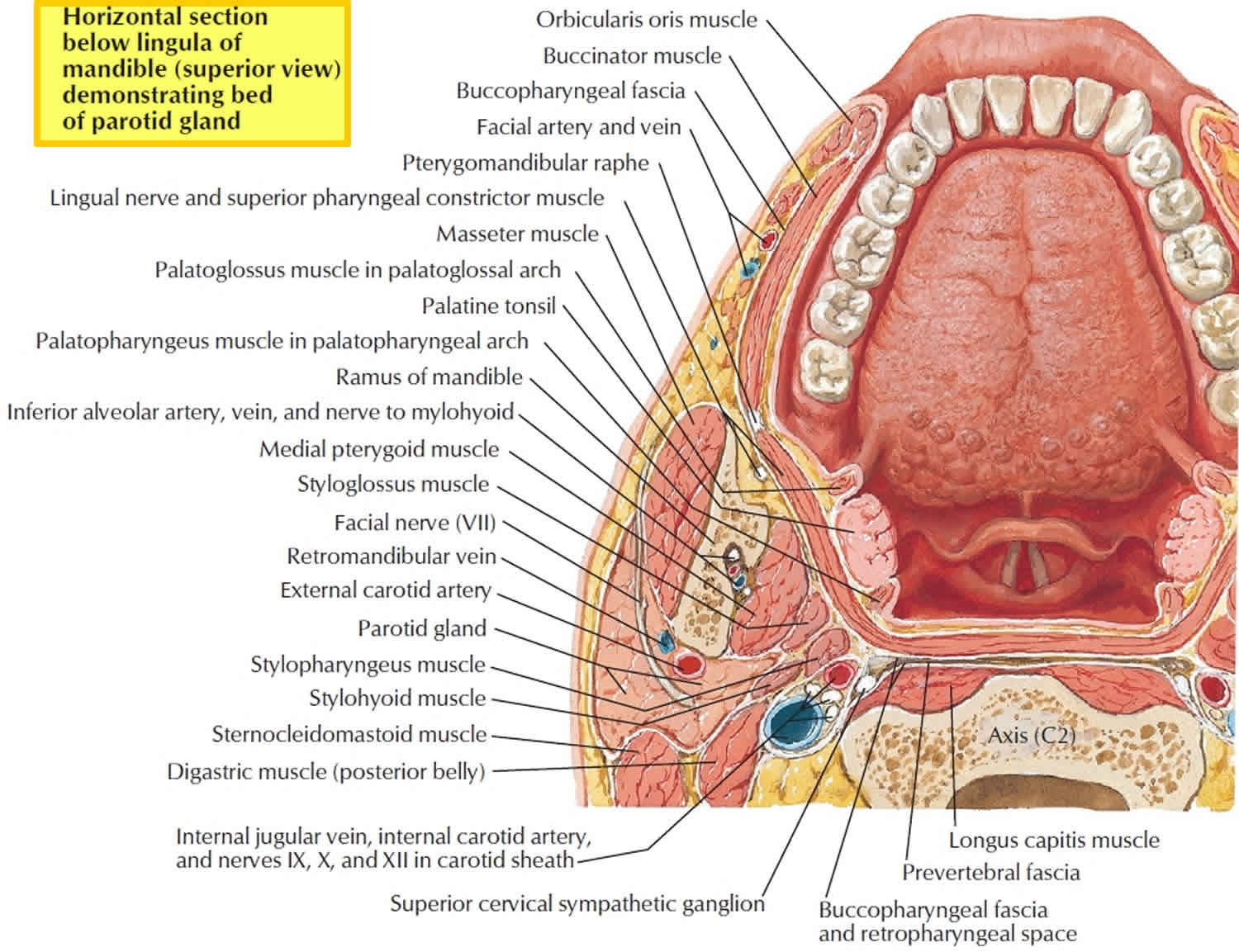
Figure 6. Mandible anatomy horizontal section
Blood Supply and Lymphatics
Blood supply to the mandible is via small periosteal and endosteal vessels. The periosteal vessels arise mainly from the inferior alveolar artery and supply the ramus of the mandible. The endosteal vessels arise from the perimandibular branches of the maxillary artery, facial artery, external carotid artery, and superficial temporal artery; these supply the body of the mandible 4. The mandibular teeth are supplied by dental branches from the inferior alveolar artery.
Lymphatic drainage of the mandible and mandibular teeth are primarily via the submandibular lymph nodes; however, the mandibular symphysis region drains into the submental lymph node, which subsequently drains into the submandibular nodes.
Nerves
The main nerve associated with the mandible is the inferior alveolar nerve, which is a branch of the mandibular division of the trigeminal nerve (cranial nerve 5). The inferior alveolar nerve enters the mandibular foramen and courses anteriorly in the mandibular canal where it sends branches to the lower teeth and provides sensation. At the mental foramen, the inferior alveolar nerve branches into the incisive and mental nerve. The mental nerve exits the mental foramen and courses superiorly to provide sensation to the lower lip. The incisive nerve runs in the incisive canal and provides innervation to the mandibular premolar, canine, and lateral and central incisors 5.
Muscles
Muscles Originating from the mandible:
- Mentalis – originates from the incisive fossa
- Orbicularis oris – originates from the incisive fossa
- Depressor labii inferioris – originates from the oblique line
- Depressor anguli oris – originates from the oblique line
- Buccinator – originates from the alveolar process
- Digastric anterior belly – originates from the digastric fossa
- Mylohyoid – originates from the mylohyoid line
- Geniohyoid – originates from the inferior portion of the mental spine
- Genioglossus – originates from the superior portion of the mental spine
- Superior pharyngeal constrictor – originates partially from the pterygomandibular raphe, which originates from the mylohyoid line
Muscles Inserting on the mandible:
- Platysma – inserts on the inferior border of the mandible
- Superficial masseter – inserts on the lateral surface of the ramus and angle of the mandible
- Deep masseter – inserts on the lateral surface of the ramus and angle of the mandible
- Medial pterygoid – inserts on the medial surface of the mandibular angle and ramus of the mandible
- Inferior head of the lateral pterygoid – inserts on the condyloid process
- Temporalis – inserts on the coronoid process
Mandible vs Maxilla
The maxillary bones, or maxillae are the largest facial bones and they form the upper jawbone and the central part of the facial skeleton (see Figure 2). The maxillae form the upper jaw and meet each other at a median intermaxillary suture. They are considered the keystone bones of the face because they articulate with all other facial bones except the mandible. The maxillary bones form the upper jaw and parts of the hard palate, orbits, and nasal cavity walls.
Small points of maxillary bone called alveolar processes grow into the spaces between the bases of the teeth. The root of each tooth is inserted into a deep socket, or alveolus. If a tooth is lost or extracted so that chewing no longer puts stress on the maxilla, the alveolar processes are resorbed and the alveolus fills in with new bone, leaving a smooth area on the maxilla.
Like the mandible, the maxillae have an alveolar process that contains teeth in alveoli. The palatine processes project medially from the alveolar margins to form the anterior region of the hard palate, or bony roof of the mouth (Figure 7). The frontal processes extend superiorly to reach the frontal bone, forming part of the lateral aspect of the bridge of the nose (Figure 1). The maxillae lie just lateral to the nasal cavity and contain the maxillary sinuses. These sinuses, the largest of the paranasal air sinuses, extend from the orbit down to the roots of the upper teeth. Laterally, the maxillae articulate with the zygomatic bones at the zygomatic processes.
The maxilla, along with several other bones, forms the borders of the inferior orbital fissure in the floor of the orbit. This fissure transmits several vessels and nerves, including the maxillary nerve (a branch of cranial nerve V) or its continuation, the infraorbital nerve. The infraorbital nerve proceeds anteriorly to enter the face through the infraorbital foramen.
Figure 7. Maxilla
The maxillary bones important structures:
- Alveolar process: sockets for teeth
- Zygomatic process: helps form the zygomatic arches
- Palatine process: forms the anterior part of the hard palate; the two processes meet medially in the intermaxillary suture
- Frontal process: forms part of lateral aspect of bridge of nose
- Incisive fossa: passageway for blood vessels and nerves through hard palate (fused palatine processes)
- Inferior orbital fissure: passageway for maxillary branch of cranial nerve V, the zygomatic nerve, and blood vessels
- Infraorbital foramen: passageway for infraorbital nerve to skin of face
Mandible function
Mandible supports the lower teeth and provides attachment for muscles of mastication (chewing and eating) and facial expression.
Mandible dislocation
Temporomandibular joint dislocation also called mandible dislocation, is an uncommon but debilitating condition of the facial skeleton. Mandible dislocation may be acute or chronic. Acute temporomandibular joint dislocation is common in clinical practice and can be managed easily with manual reduction 6. Chronic recurrent temporomandibular joint dislocation is a challenging situation to manage.
The pathophysiology of mandible dislocation is the movement of the condylar process in front of the articular eminence and an inability to descend back to its normal position. It can be partial (subluxation) or complete (luxation), bilateral or unilateral, acute, and chronic protracted or chronic recurrent 7. The most common mandible dislocation is anterior dislocation 6. The other types such as medial, lateral, superior into the middle cranial fossa, and posterior are rare and are mostly associated with trauma 8.
Dislocation of the temporomandibular joint is due to either imbalance in the neuromuscular function or structural deficit. Previous dislocation is the greatest risk factor. Alteration in the neuromuscular function occurs due to laxity of the articular disc and the capsular ligament, long-standing internal derangement, and spasm of the lateral pterygoid muscles. Structural deficit involves arthritic changes in the condyle, i.e., flattening or narrowing, decrease in the height of the articular eminence, morphological changes of the glenoid fossa, zygomatic arch, and squamotympanic fissure 9. Age and changes in the dentition also play definite role indislocation 10. Other causes include over function, i.e., forceful wide opening of the mouth while yawning, laughing, vomiting, or seizures, dental treatments like third molar extractions or root canal treatments, or endotracheal intubation, laryngoscopy, and trans oral fiber optic bronchoscopy 11. Certain antipsychotic medications may also lead to dislocation. Some syndromes are also associated with it such as the Ehlers-Danlos syndrome, orofacial dystonia, and the Marfan syndrome 10.
Mandible dislocation symptoms
The most common clinical symptom is the inability to close the oral cavity, i.e., “open lock,” difficulty in speech, drooling of saliva, and lip incompetency. The patient may present with the inability to close his or her mouth or with an asymmetric jawline. In acute dislocation, pain in the pre-auricular region is present, but chronic recurrent dislocation is rarely associated with it. Usually bilateral and at times unilateral dislocation may lead to deviation of the chin to the contralateral side. Palpation over the preauricular region may suggest emptiness in the joint space. The patient may look anxious 12.
Mandible dislocation diagnosis
Clinical history and examination are the most important tools in diagnosing temporomandibular joint dislocation. Other confirmatory diagnostic aids include plain and panoramic radiographies, showing the location of the condylar head anterior to the articular eminence. In patients with traumatic mandibular injuries, a standard four-view series of X-ray film may be obtained. In many cases, due to superimposed anatomy, mandibular series do not provide sufficient detail to accurately diagnose condylar fractures. This issue can be solved by using a reversed Towne view for imaging. Newer modalities such as CT scans have proven more sensitive than X-ray and are commonly employed 13. Three-dimensional computed tomography is the best in terms of its perfection to show this entity.
On the basis of the clinico-radiological evaluation, Akinbami 14 classified temporomandibular joint dislocation into the following three types:
- Type I – the head of the condyle is directly below the tip of the eminence
- Type II – the head of the condyle is in front of the tip of the eminence
- Type III – the head of the condyle is high-up in front of the base of the eminence.
Acute mandible dislocation
Acute mandible dislocation is a very painful clinical condition, but easy to manage. The conservative methods in its management include symptomatic pain relief with analgesics and manual reduction.
The manual reduction method is performed by first pressing the mandible downward, then backward, and finally upward as described by Hippo crates. In 1981, Lewis modified it in his way by stating that the patient should be made to sit down and the clinician should stand in front of him/her or at 11o’ clock position. Then, the thumb should be pressed down on the occlusal surface of the lower molar teeth. At the same time, the chin should be elevated with the fingers and the entire mandible should be pushed posteriorly 15. Few authors have further modified the technique by changing the position of the thumb from the occlusal surface of the teeth to the anterior border of the ramus 16. Sometimes, the manual reduction is complicated by the secondary reflex spasm of the lateral pterygoid muscle, followed by painful stimuli from the joint capsule. As the condition is very painful, it is always better to perform manual reduction under local anesthesia by giving auriculotemporal nerve block or local infiltration in the joint space. Role of the muscle relaxants in controlling the reflex muscle spasm is still debatable.
In 1987, Awang 17 described another simple, safe, and rapid method in managing acute dislocation. According to him, induction of the gag reflex by probing the soft palate creates a reflex neuromuscular action that resulted in the reduction 18.
Chronic recurrent mandible dislocation (Subluxation)
If this condition is long-standing or recurrent, it poses a challenge to the treating clinician. The management is divided into two stages, the conservative methods are opted; if the results are not satisfactory, then doctors go for the surgical methods.
The conservative method
The conservative method includes the use of various sclerosing agents like alcohol, sodium tetradecyl sulfate, sodium psylliate, morrhuate sodium, and platelet-rich plasma that has been injected into the joint space 19. In case of chronic protracted dislocation, elastic rubber traction with arch bars and ligature wires/intermaxillary fixation (IMF) with elastic bands are useful to achieve the reduction 19.
The use of autologous blood in recurrent dislocation was reported by Brachmann in 1964 and is very popular nowadays. It is based on the principle to restrict mandibular movements by inducing fibrosis in the upper joint space, the pericapsular tissues, or both 20. In an animal study, Gulses et al. 21, demonstrated that there are significant fibrotic changes histologically evident in bothretrodiscal and pericapsular tissues. The volume of blood to be used ranges 2-4 mL in the upper joint space and 1-1.5 m L in the pericapsular structures, repeated twice a week for 3 weeks. To further enhance the fibrosis, restriction of the mandibular movement with a head bandage is required for the period of 3-4 weeks 22. However, some authors have reported chances of degeneration in the articular cartilage and permanent joint destruction 23. But after inducing hem arthrosis in the temporomandibular joint of rats, Alons et al., reported that there is no noticeable damage to the cartilage and the interposing disc on histopathological examination 24. The only reported disadvantage of this technique is severe restriction in the mandibular range of motion 25. Machon et al. 22 advocated that the patient should start jaw rehabilitation by a gradual and controlled range of motion exercises after 2 weeks of the autologous blood injection therapy.
Another newer conservative method is the application of botulinum toxin-A in recurrent temporomandibular joint dislocation. Previously, botulinum toxin-A was used in the management of facial wrinkles, masseteric and temporalis muscle hypertrophies, strabismus, hyperhidrosis, hemifacial spasm, sialorrhea, and masticatory myalgia 26. There have been several anecdotal reports of the use of botulinum toxin-A as a treatment for temporomandibular joint dislocation, but a controlled clinical trial is needed to prove the evidence of its efficacy 27. It involves injecting the drug in the lateral pterygoid muscle, to prevent temporarily recurrent dislocation 28. It acts by causing temporary weakening of the skeletal muscle by blocking the Ca2+-mediated release of acetylcholine from the nerve endings of the neuromuscular junction 29. Because the effect is temporary, repeated administration is required after 2 weeks for better results. Botulinum toxin injection therapy is also an option in those patients who suffer from recurrent dislocation of the temporomandibular joint as a result of impaired muscle coordination, secondary to oromandibular dystonia, neuroleptically-induced early and late dyskinesias, epilepsy, and brainstem stroke syndromes 27. The adverse effect involves diffusion into the adjacent tissues, transient dysphagia, nasal speech, nasal regurgitation, painful chewing, and dysarthria. It is contraindicated in a few conditions like hypersensitivity to botulinum toxin and myasthenia gravis in pregnant and lactating women 30.
The surgical methods
The surgical methods are indicated in those cases where the patients have not responded well to the conservative methods.
In 1968, Rowe and Killey 19 used a bone hook that was passed over the sigmoid notch through a small incision below the angle of the mandible and downward traction was applied on the condyle. Traction with wires was done by applying the wires through the holes drilled in the angle of the mandible. In 1981, Lewis 15 used a technique in which the Bristow’s elevator was passed through the temporal fascia as in the Gillies technique of elevation of the depressed zygomatic bone. The tip of the elevator was used and strong force was applied in the downward and posterior directions. This method also facilitates open reduction by extending the incision as used for the preauricular approach to the joint.
Various other methods like condylotomy, modified condylotomy, and myotomy had been tried. Condylotomy was used as a blind approach using a modified Kostecka approach and a Gigli saw. It is an open approach, usually using the preauricular route 31. Myotomy with resection of the insertion of the external pterygoid muscle had been described by Bowman in 1949. It limits the mandibular translation and allows only rotational movement of the condyle 32. In 1973, Laskin proposed an intraoral surgical approach to the muscle via a coronoid incision to performa temporalis myotomy 33.
In 1976, Adekeya et al. 34 described a technique in which the occlusion was restored by means of the inverted L-shaped osteotomy of the ramus. Other authors have also recommended the use of vertical or oblique ramus osteotomy and bilateral sagittal split osteotomy for correction of the occlusion. But it did not get popularized due to many disadvantages like the risk of damage to the inferior alveolar bundle, less bone contact, and impingement/impaction of the coronoid process on the condyle 35.
Few authors have suggested surgical procedures that either remove the mechanical obstacle in the condylar path or create a mechanical obstacle by augmenting the articular eminence. In 1951, Myrhaug 36 first reported total eminectomy as a treatment for dislocation. The removal of the eminence will facilitate the return of the condyle without any interference into the glenoid fossa. Augmentation of the articular eminence can be done by autogenous bone grafts like the iliac crest or the calvarial bone 10. Various other materials have also been used like L-shaped pins, vitallium mesh implants, and mini implants to enhance the eminence 37. Silicone wedge blocks and coralline hydroxyapatite blocks have also been used by few authors 38. Looseness, displacement, and immune reactions are some of the adverse effects, especially for silicones.
Initially in 1933, Mayer described that downward displacement of the zygomatic arch acts by obstructing the path of the condylar translation. Later, Dautrey modified the technique in which the greenstick fracture was performed at the zygomaticotemporal suture and displaced the anterior segment downward and inward to serve as a stop to the forward and the upward movements of the condyle head. It cannot be performed in elderly people due to the brittleness of the bone; so, it is restricted to younger individuals 12.
Fascia lata, MERSILENE tapes (Dacron, Ethicon, Johnson and Johnson Ltd) anchored around the zygomatic arch and passed around the condyle have also been used to restrict its movement. Fascia lata can be readily harvested and the treatment is cheaper but accompanied with postoperative pain, swelling, minor gait disturbance, and movement of the lower limb 12. Surgical capsulorrhaphy also helps by reinforcing the lax capsule. Meniscoplasties and meniscectomies are relevant procedures done when the altered disc morphology and the position cause dislocation or prevent self-reduction. Total joint replacements should be considered when all the appropriate treatments fail in chronic protracted and chronic recurrent dislocations, especially those with associated degenerative joint diseases 18.
Mandible fractures
Seventy percent to 85% of mandibular fractures occur in males, with the majority occurring in individuals in their twenties and thirties 39. The most common causes are aggravated assaults and motor vehicle collisions in males, and falls and motor vehicle accidents in females 39. Other common causes include sporting activities and gunshot wounds. It may also result from assault. The mechanism of injury is important to take into consideration as it provides the physician with an index of suspicion for concomitant injuries, which may delay repair or necessitate a different treatment modality. Motor vehicle accidents and gunshot wounds, for example, because of the nature of the forces created, tend to be the most destructive to the craniofacial skeleton 40. Concomitant injuries are important in judging the gravity of the clinical scenario, because as one study showed, whereas the mortality of patients admitted for maxillofacial trauma with isolated mandibular fractures is fairly low (1.6%), when combined with fractures of regions of other areas of the face, the mortality is substantially higher (∼25%) 41.
Other injuries frequently occur with mandibular fractures as well. Studies have reported that the incidence of cervical-spine injuries in patients presenting with facial fractures ranges from ∼2 to 10% (whereas there is an inverse relationship between mandibular fractures and intracranial pathology) 42. Additionally, 32% of mandibular fractures are associated with abrasions or lacerations, 24% with neurologic injury, 20% with additional orthopedic injuries, and 12% with pulmonary, abdominal, or cardiac injury. Once again, though, the overall incidence of these accompanying injuries will differ based on the initial mechanism of injury 43.
Clinical evaluation
The most important factor in deciding whether or not a mandible fracture requires a surgical intervention is the status of the occlusion, which can be abnormal in more than 80% of mandibular fractures 44. The occlusion can be evaluated by asking the patient if his or her bite has changed since the injury. If this basic information cannot be obtained, examination of wear facets or assessing old dental records can be helpful. Determining the type of occlusion prior to trauma is important, because the subsequent goal of any surgical intervention will be to restore the preinjury occlusion, even if the preinjury occlusion was abnormal.
The patient’s occlusion can be systematically classified using the Angle classification system, the lingual-labial/buccal relationship, and the vertical relationship between the maxillary and mandibular teeth (Table 1). The vertical height of each hemi-mandible can then be assessed for shortening or cant by placing a tongue depressor between the teeth when in occlusion and examining the horizontal orientation of the tongue depressor.
A complete physical examination, including inspection, palpation, sensation, and range of motion, should also be performed. Abnormal changes in dentition need to be noted, as well as any associated injury to the mental nerve. The latter is particularly important to differentiate trauma-related injury from iatrogenic injury postoperatively. Other associated injuries need to be evaluated as well, including intraoral soft tissue injuries and the common concomitant injuries mentioned previously.
Table 1. The Occlusion Can Be Classified in a Systematic Manner Using the Angle Classification System, the Lingual-Labial/Buccal Relationship, and the Vertical Relationship between the Maxillary and Mandibular Teeth
| Classifying the Occlusion | |
|---|---|
| Angle classification | |
| Class 1 occlusion | Mesiobuccal cusp of 1st molar occludes into buccal groove |
| Class 2 occlusion | Mesiobuccal cusp of 1st molar lies mesial to the buccal groove |
| Class 3 occlusion | Mesiobuccal cusp of 1st molar lies distal to the buccal groove |
| Lingual-labial/buccal relationship | |
| Normal | Maxillary teeth are located slightly labial/buccal to mandibular teeth |
| Anterior crossbite | Anterior maxillary teeth located lingual to mandibular teeth |
| Posterior crossbite | Posterior maxillary teeth located lingual to mandibular teeth |
| Vertical relationship | |
| Normal | Incisal edges of the anterior maxillary teeth extend 2 to 3 mm below the incisal edges of the mandibular teeth |
| Open bite | Lack of occlusal contact between maxillary and mandibular dentition |
| Overbite | > 3 mm of vertical overlap |
Imaging studies
Imaging of the mandible for fractures is best performed with high-resolution computed tomography (CT) images, whereas for dentition-related injuries, the Panorex is the best. Panorex imaging has the ability to image the tooth roots, which will ultimately help in plate positioning for fixation. For patients that are unable to stand and obtain Panorex imaging, use of the “Zonarc” may be an alternative option 45. This equipment uses the same principles behind panoramic imaging to create an adequate imaging study for patients that are unable to stand or sit in an upright position. This is extremely beneficial in unstable patients (as often seen in the trauma setting) who require imaging. Magnetic resonance imaging also has a role in mandibular trauma, as it is particularly useful for evaluation of the temporomandibular joints and condyles.
Mandibular fractures treatment
The goal of treatment is proper alignment of the jaw bone so the upper and lower teeth come together normally. Surgery is often required for moderate to severe fractures to align and immobilize the bone so it can heal.
Optimal treatment timing must take into consideration the type and severity of injury. Concomitant injuries that require attention for patient stabilization need to be addressed in an expeditious manner, prior to management of mandibular fractures.
Studies looking at the relationship between timing of surgery and subsequent outcomes have demonstrated no difference in infectious/nonunion complications between treatment within or after 3 days status postinjury but did find that complications because of technical errors increased after this time.15 As a result, the authors commented that if surgery was to commence 3 or more days after the injury, a technically accurate surgery by the surgeon is necessitated to overcome factors such as tissue edema and inflammation. In cases where a delay in treatment is necessary, consideration should be given for temporary closed fixation to reduce fracture mobility and patient pain.
Treatment types
Treating mandibular fractures involves providing the optimal environment for bony healing to occur: adequate blood supply, immobilization, and proper alignment of fracture segments. As a result, most fractures require reduction and fixation to allow for primary or secondary bone healing. The one exception is the unilateral subcondylar fracture in the patient with a normal occlusion, which we shall discuss later.
Secondary bone healing occurs when fractured bone segments are placed in approximation, stabilized with allowance for some degree of micromotion, without significant devascularization of bone segments. Subsequently, bony healing occurs through a callous intermediate and ensuing ossification. This form of fixation can be performed with either intermaxillary fixation/maxillomandibular fixation (IMF/MMF) with arch bars, 4-point fixation, occlusal splints, or miniplates.
Primary bone healing with rigid fixation bypasses the callous intermediate by approximation and fixation, which inhibits micromotion of the fracture site. This is primarily performed via the application of plates (except for miniplates) and screws to the fracture site but ultimately results in a variable degree of periosteal undermining, which may compromise the vascularity of the injured bone segments.
There are advantages and disadvantages to both methods of fixation. Closed reduction does not traumatize the vascular envelope and is less expensive for the patient; however, it is associated with a significant period of immobilization and closure of the oral cavity, and requires intact dentition or some form of dental records. Open reduction and internal fixation (ORIF), in contrast, allows for direct visualization and reduction of fractured bone segments and restoration of the patient’s preinjury occlusion without complete fixation of the mandible and maxilla. This allows for bony healing in a shorter period of time, which gives rise to the patient’s earlier return to normal jaw function and better nutrition and oral hygiene. It is important to note, however, that potential foreign body infections are more likely with this technique.16 Additionally, studies that have examined the complications with both techniques have shown that open reduction and internal fixation (ORIF) is associated with increased morbidity, and although this can be explained by vascularity changes caused by the intervention, because there has not been a randomized study comparing the two. This could also be because open reduction and internal fixation (ORIF) is usually used in more severe injuries 46.
Another important factor to take into consideration is patient compliance. One study noted that up to 60% of patients being treated for facial fractures can be noncompliant in some form 47. Determining those who are likely to be noncompliant is important when deciding between intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) or open reduction and internal fixation (ORIF), as these patients are best treated with open reduction and internal fixation (ORIF) to reduce the risk of premature release of intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) and subsequent complications.
Intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) is also a reasonable option for those at an increased risk for complications with open reduction and internal fixation (ORIF); however, there is considerable overlap between this at-risk group for complications and the at-risk group for noncompliance, and intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) may not be the best option for long-term outcomes. At this point, a thorough assessment should be made and a thorough discussion held with the patient to determine the best treatment method. The decision regarding compliance and choice of reconstruction is extremely important as the cause of many facial fractures (aggravated assault, fights, alcohol/drugs, etc.) already indicates a high likelihood of noncompliance.
Closed Reduction
Intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) is a technique to immobilize the fractured segments of the mandible by externally locking the occlusion into place, using the dentition as a point of stability. The two terms refer to the same method of fixation, but the former is a vestige from a time when the mandible was considered the lower maxilla, and thus fixation occurred in an “intermaxillary” fashion.
Fixation with intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) can be performed in several ways. First, Kirschner wires can be used in either the Gilmer or Eyelet method to provide fixation. These methods differ in that the Eyelet method can allow for the removal of wires for inspection of the mandible without removing the intermaxillary ligatures. Erich arch bars provide the next level of intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) stability, alignment, and control and have become the standard of care for treatment with intermaxillary fixation (IMF)/maxillomandibular fixation (MMF), as they provide an additional structure for fixative support besides the dentition. In cases where supplemental fixation is necessary, however, adjacent structures can be used to fixate the occlusion.
Additional stability of the occlusion can be obtained by placing wires that fixate the maxilla superiorly around the pyriform aperture and inferiorly around the mandibular border. Additionally, screws can be used to provide “4-point” fixation in these regions as well. Screws can be placed into the maxilla and mandible in a bilateral fashion and wires subsequently used to fixate both the right and left hemi-mandibles using these fixation points. This technique is advantageous because it can be applied rapidly; however, it does not provide stabilization within the dental arch and also increases the risk of tooth injury. These additional forms of fixation are necessary, though, when inadequate stability is provided by the dentition, such as in the edentulous mandible in the elderly or the deciduous/transitioning dentition of the pediatric population.
Acrylic occlusal splints are also used to establish continuity of the dental arches in cases of discontinuity 48. Cases where these may be beneficial are when there are missing teeth or concomitant fractures of the alveolus that require stabilization within the maxillary or mandibular arch prior to intermaxillary fixation (IMF)/maxillomandibular fixation (MMF). These splints are wired into place and allow for accurate dental alignment while healing occurs.
A major downfall of any closed technique is the presence of soft tissue, bony fragments, or hematoma in the fracture site that prevents anatomic reduction. This may be less of an issue in the mandible as occlusion is the ultimate reduction measure, but if preinjury occlusion cannot be obtained with closed reduction, the fracture site may need to be cleaned of debris.
Open Reduction and Internal Fixation
Plates and screws function to rigidly fixate and prevent any motion of fracture segments by absorbing all or part of the functional load that is present at a fracture site. Subsequently, several principles underlie the decision-making process for mandibular fracture repair. Choices must be made regarding the proper plate length and thickness required, and what type and size of screws to use.
First, plate length is generally determined to allow for the placement of more than one screw on either side of the fracture to nullify the dynamic forces that act on the mandible. In ideal conditions, three screws are placed on either side of the fracture segments to allow for assurance against inadequate stabilization, with screws placed at least several millimeters from the fracture site.
Next, proper plate thickness is determined by the forces required to stabilize fractured bone segments. Options for stabilization can be divided into either load-sharing fixation (miniplates, 1.0-mm profile; universal fracture locking/nonlocking plates, 1.5-mm profile; lag screws) or load-bearing fixation (locking and nonlocking reconstruction (recon) plates, 1.5-, 2.0-, 2.5-, or 2.8-mm profile). These options differ in their internal screw diameter, thickness, surface area of in-contact bone (footprint), titanium grade, malleability, and in their ability to stabilize the bone segments against the intrinsic forces on the mandible. These characteristics, in general, increase as one progresses from miniplates, to normal fracture/locking plates, to recon plates.
Deciding between these forms of rigid fixation is based on both the bone quality of the fractured segments and the intrinsic forces on the mandible. If bone quality is poor, such as with significant comminution, defects, or atrophy, then load-bearing fixation will be needed for stabilization. For other situations, such as with young healthy male patients, stronger plates and extra screws will be necessary because of greater bite forces that are placed on the mandible. Miniplates, with decreased thickness, footprint, titanium grade, and increased malleability, are best used along areas of the mandible that are subjected to smaller degrees of forces. In 1978, Champy et al further defined these regions of the mandible that would only require monocortical plates to allow for stable fixation along the symphysis, parasymphysis, and angle of the mandible 49. These regions have subsequently been called Champy’s lines of tension, with the superior portion of lines also referred to as the tension band of the mandible.
More recently, locking plates have been introduced that allow for the screw head to be “locked” into the plate, thus turning the plate and screw apparatus into an internal-external fixator. There are both theoretical and biomechanical advantages to this technique, including a lower risk of malocclusion secondary to inappropriate plate contouring, a lower frequency of screw loosening, ease of use, and reduced time for application 50. Additionally, studies have demonstrated its use and clinical safety 51; however, a clear benefit over nonlocking plates and screws has not been definitively demonstrated 52. Although this technique of rigid fixation has become the status quo for fracture fixation, it is worth noting that one downside is that surgeons may get decreased sensory feedback regarding adequate bone purchase because of the design of the plate and screws.
As touched upon earlier, prior to open reduction and internal fixation (ORIF) complete cleaning of the fracture site is an essential and often overlooked first step. This can be accomplished by recreating the fracture after retracting the soft tissue and stripping the periosteum with elevators, synovial rongeurs, or a simple curved hemostat. A few minutes spent removing debris, soft tissue, hematoma, and fracture callous prevents frustration and problems obtaining occlusion/anatomic bony reduction, ultimately yielding a better outcome.
During plate placement, holding reduction, or more importantly occlusion, while drilling and placing screws, is of utmost importance. If the plan includes postoperative maintenance of intermaxillary fixation (IMF)/maxillomandibular fixation (MMF), then the arch bars should be placed prior to attempting open reduction and internal fixation (ORIF) and the IMF/MMF can hold occlusion while plating. However, one of the benefits of plate fixation is to absolve the need for intermaxillary fixation (IMF)/maxillomandibular fixation (MMF), as spending valuable operating room time placing arch bars only to remove them after plating can be tedious and time consuming. In these cases, where postoperative IMF/MMF is not indicated, it may be possible to use manual occlusal reduction, temporary 4- or 6-point intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) with screws, bone reduction forceps, or, most commonly, a combination of these. These techniques not only save time but also allow for rapid removal and checking of occlusion after placement of each screw to ensure sequential and incremental increases in alignment and stability. A potential pitfall can arise if the manual reduction or 4-point fixation is too close to the midline/focused on the inferior border of the parasymphyseal region, as this vector tends to open up the inferior border of the posterior body or mandibular angle fractures. This can be avoided with bilateral manual pressure distributed across the body and symphysis or properly spaced (between canine and bicuspid) 4-point intermaxillary fixation (IMF)/maxillomandibular fixation (MMF). However, placing the patient in intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) with arch bars and wires will always be the best way to guarantee occlusional integrity during fracture plating.
Screw choice will also require some thought. Screws can vary based on their amount of cortical bone purchase, and are termed monocortical and bicortical screws. Monocortical screws only travel through one of the bony cortices because of their decreased length. Subsequently, the screws are helpful in areas with important underlying structures, such as tooth roots, or the inferior alveolar neurovascular bundle; however, the limited bony purchase results in only functionally stable fixation, and thus must be placed along areas of less dynamic tension, such as Champy’s lines.
Screws can also vary based on their diameter. In general, as the screw’s diameter increases, so does the stability against the forces on the mandible. Subsequently, smaller screws (2.0 mm) are effective for simple fractures, and screws of larger diameters (2.3 mm) are better suited for comminuted or multiple fractures. The Stryker mandibular plating system has 2.0-, 2.3-, and 2.7-mm screws that can be used in any one of their plates (miniplates, recon plates, etc.). However, in general, the heavier the plate used, the thicker the screw should be.
When placing screws, it is important to work from the screw holes nearest the fracture outward to avoid splaying the fracture site, as can happen when working in the opposite direction. Using a threaded drill guide is important when using locking plates, as it ensures that you are within the angulation tolerances of the threading on the plate, and occlusion will not be altered when tightening that screw. If you freehand a hole that is angulated more than the plate can tolerate, the screw can be forced into conforming within the tolerances of the plate hole, and subsequently after the occlusion.
Screws can be also be applied without the use of plates. Lag screws are specialized screws that can stabilize simple fractures, and are placed at a 90-degree angle to the fracture in a plane that is parallel to the long axis of the bone. To prevent rotational and other forces from disrupting the rigid fixation of the fracture site, at least two screws are needed for stabilization. The proper use of lag screws, and the many other fixation methods mentioned previously, depends on the fracture site and type.
Fracture Management Based on Location
Symphysis/parasymphysis
Fractures in this region can generally be managed in three ways. First, symphyseal and parasymphyseal fractures, even if displaced, do not need to be treated with internal fixation. Because this is a tooth-bearing region, maxillomandibular fixation (MMF) with arch bars can be used to reestablish and fixate the occlusion. Internal fixation can be used, however, and two methods for treatment exist, with both using an intraoral approach. One method is to place lag screws across the defect. The other is to fixate the fractured segments using a plate placed monocortically at the superior border or tension band (to prevent damage to underlying tooth roots), and a second plate at the inferior border, placed bicortically. In general, there is more room to work in this central region of the mandible as the tooth roots are vertically short, and the mental nerve can be mobilized and retracted to allow for appropriate visualization and fixation.
When fixating the region, it helps to temporarily fix the inferior border with bone clamps and then plate the superior border. The temporary fixation can then be released and the inferior border plated. The two points of fixation are necessary to prevent rotational forces from causing the superior border from splaying and disrupting the continuity of the alveolar arch. Arch bars or dental splints can also serve as the tension band for the region; however, it is important to use an arch bar that is strong enough to last for the period of fracture healing. After reduction and fixation, it is important to examine both the lingual and buccal aspects of the mandible, as inappropriate plate bending (with nonlocking plates) can cause gapping on the lingual aspect of the mandible, resulting in a cross-bite and an increase in mandibular width. Additionally, if multiple areas require fixation, it is important to check the occlusion after every plate is applied.
Body of mandible fracture
Fractures in the mandibular body are generally managed with a greater degree of caution because of the neighboring structures in the region. Like fractures in the symphyseal and parasymphyseal regions, these fractures within the tooth-bearing segments of the mandible can be treated with closed reduction and fixation. When internal fixation needs to be performed, these fractures are generally repaired using an intraoral approach. An extraoral approach may be required, however, for isolated fractures that are located along the posterior and inferior aspects of the mandibular body, as an intraoral incision does not provide enough visualization to rule out gapping after fracture reduction.
Treatment generally involves plating a monocortical miniplate along the superior border or tension band and a bicortical miniplate along the inferior border. During the repair, several key anatomic features must be respected. The inferior alveolar nerve and artery must be identified, as well the smaller distance between the tooth roots and inferior mandibular border, because of the greater space taken up by the tooth buds.
Angle of mandible fracture
Angular fracture management is nuanced because of the inferior alveolar nerve and artery, and the variable presence of the third molar or wisdom tooth. Although removal criteria for impacted third molars are generally agreed upon (including infected, grossly mobile, or inhibiting fracture reduction), certain situations that do not meet these criteria need to be managed on a case-by-case basis. If a third molar is to be removed in mandibular angle fractures, these should generally be removed only after fracture reduction and fixation; however, in cases where the tooth is preventing fracture reduction, removal may be necessary prior to fixation.
The ideal surgical management involves using either an intraoral approach with or without transbuccal trochar instrumentation (for screw placement along the posterior and inferior aspects of the angle) or an extraoral approach (for comminuted and complex fractures). When combining an intraoral approach with a transbuccal trochar, placement of the trochar is essential. Frequently, a single access point will work for most but not every screw hole. Using the same incision to affix the entire plate will often work, as one can reposition the trochar by altering its course through the buccinator and buccal mucosa; however, struggling with a trochar that is severely angulated and that is placing extreme traction against the soft tissues simply increases surgeon frustration. This may also in fact do more damage to the soft tissue versus another tunnel, and makes subsequent successful screw placement difficult or impossible.
Fixation then requires either placing a miniplate along the oblique ridge of the mandible (Champy technique) with or without a miniplate along the inferior border, placing a strut plate (two miniplates buttressed with perpendicular strut bars) along the lateral aspect, or placing a recon plate in cases of significant comminution or poor bone stock. Preference toward stabilization with a strut plate versus plating the oblique ridge should occur in situations of individuals that are able to generate significant bite forces, as stabilization along the oblique ridge does not provide fixation that is as rigid.
Ramus of mandible fractures
Mandibular ramus fractures can be managed with either rigid fixation or functionally stable fixation. In cases of nondisplaced fractures, some individuals have advocated for treatment using intermaxillary fixation (IMF)/maxillomandibular fixation (MMF), albeit for a longer period of time (6 to 8 weeks); however, in our experience, we have found this to be an inadequate form of fixation as the stabilization affects the portions of the mandible involving the alveolar arches and fails to fully stabilize the posterior portions of the mandible against the intrinsic forces of the pterygomasseteric sling. Subsequently, consideration should be given toward open reduction and internal fixation (ORIF), increasingly so as fractures descend along the ramus. Exposure of this region can involve either a preauricular or a submandibular approach (based on fracture location); however, both may be necessary in significantly comminuted fractures.
Coronoid of mandible fracture
Coronoid fractures are generally stabilized by the insertion of the temporalis muscle. Subsequently, if the fracture is isolated, and the patient can open and close his or her mouth without difficulty, then conservative treatment is the best option. In the rare situation where a patient is unable to go through a range of motion or is limited by pain, open reduction and internal fixation (ORIF) is the best method for management.
Condyle of mandible fracture
The management of condylar fractures varies based on the specific location of the injury. Management options have historically been either an open approach, open with endoscopic approach, or closed approach, and investigators have made arguments for each modality 53. Generally speaking, though, the optimal management differs based on the location of the fracture. Condylar fractures involving the capsule of the temporomandibular joint are significant because of the associated risk of temporomandibular joint ankylosis, and it is generally understood that a conservative approach of intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) for 7 to 10 days with an early return to function is the best treatment option 54. This is probably due to a combination of the devascularization necessary to plate this distal segment and the difficulty associated with gaining stability of a small distal segment through open reduction and internal fixation (ORIF).
Subcondylar fractures are an area of greater contention. Both closed and open reduction and internal fixation (ORIF) methods of treatment have been described, and although several studies have demonstrated superior results and fewer complications with open reduction and internal fixation (ORIF), many other aspects must be considered. The open approach requires a significantly greater degree of expertise and carries a significant risk of facial nerve traction injury because of a required extraoral approach. Though the injury is usually temporary, the uncertain period of time spent waiting for resolution can be stressful for both the physician and patient. Because of these concerns, we now use an algorithm for the management of these fractures, which takes into account the stability of the maxilla, the status of the occlusion, and the laterality of the injury.
Maxillary stability is the most important issue when formulating a management plan. If the maxilla is stable, then management differs based on whether the fracture is unilateral (with or without malocclusion) or bilateral. In cases of unilateral subcondylar fractures with a normal/stable occlusion, the patient can be safely managed with observation. In cases of unilateral subcondylar/neck fractures with malocclusion, patients can be treated with intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) for 7 to 10 days, followed by temporomandibular joint rehabilitation with a soft diet and elastics. If the fracture is bilateral, at least one side needs to be fixated using an open approach. Subsequently, the contralateral side can be managed with an open approach or be treated in a similar manner to a unilateral fracture with management based on the status of the occlusion. In cases of unilateral or bilateral subcondylar/neck fractures where the maxilla is unstable, the management will be similar; however, the first step in management will be to stabilize the maxilla with plating techniques.
It is important to recognize that treatment of subcondylar fractures via a closed approach does not equal “closed reduction” as the majority of subcondylar fractures remain displaced after placement in intermaxillary fixation (IMF)/maxillomandibular fixation (MMF). However, with the patient maintained in occlusion by IMF/MMF and then likely elastics, the bone can begin callous formation, and subsequently the soft tissue envelope and musculature is trained to maintain a good occlusal relationship in the closed position.
Open reduction and internal fixation (ORIF) of these fractures generally involves either a retromandibular and/or preauricular approach, but despite the combination of these incisions, visualization can still be difficult. Mobilization and adequate reduction of the fracture segments can be facilitated by placing bone clamps on the inferior fracture segment via the submandibular incision and by placing a small lag screw superficially through the superior segment outside of the temporomandibular joint capsule via the preauricular incision. The lag screw helps to manipulate the bone to achieve adequate reduction. Additionally, because of the issues with getting adequate visualization and access, there is usually only enough room to place one plate, and two screws on either side of the fracture.
Common Combinations
Mandibular fractures are rarely isolated and are commonly present at two or more fracture sites. Studies have shown that, because of the mandible’s biomechanics, roughly half of all mandibular injuries involve more than one fracture, occurring in a coup-contrecoup fashion 55. Multiple fractures are significant as they have been associated with the highest risk for postsurgical sequelae, such as persistent pain, malocclusion, and facial contour deformity 56. One common example of this type of fracture injury is the combined body/symphyseal and contralateral subcondylar injury, often seen with direct blows. In these cases, management uses principles similar to isolated mandibular fractures; however, larger stabilizing forces are required for at least one of the fracture sites because of biomechanical changes, and greater consideration should be given to recon plate placement.
Complex fractures
Complex injuries, such as comminuted fractures, blast injuries, or multiple fractures, deserve special consideration. Visualization of the fracture site becomes increasingly important, and whereas intraoral approaches are beneficial for improving aesthetic outcomes, extraoral approaches provide greater visualization and allow for the placement of larger plates in cases of extended areas with fracture involvement. Recon plates also play a larger role in management, and can be used in conjunction with miniplates for mandibular stabilization. Miniplates can also be used to stabilize the smaller bone fragments both to each other and to the larger bone fragments, while the recon plate serves as the major structural buttress of the mandible. With multiple fractures, the occlusion should be ideally checked after every plate has been placed because of the possibility of plate application creating torsional forces on the fracture segments causing malocclusion. Additionally, bone grafting plays a more significant role in these situations and should be used for significant defects of the mandible. In general, free bone grafts will survive if stabilization and soft tissue coverage is adequate36; however, in cases of large, irradiated, or anterior defects, vascularized bone grafts are preferred 57.
External fixation is used for fractures with severe comminution, infections, nonunions, or significant bone or soft tissue defects and is used when the dentition is not sufficiently intact for stable intermaxillary fixation (IMF)/maxillomandibular fixation (MMF). This method of fixation eliminates the need for significant soft tissue disruption, which may devascularize the bone fragments, and does not require the placement of an internal device.
When external fixation is used for significant comminution, one should be prepared for a high risk of complications. One study found that greater than one third of mandibular fractures treated with external fixation had complications, which was double the rate for closed treatment and more than triple the rate versus open reduction and internal fixation (ORIF) 58. Additionally, the rate of malocclusion after the treatment of comminuted fractures with external fixation approaches 11.7%, almost triple the rate of complications seen with open reduction. This increased incidence of complications most likely is not a statement of the problematic nature of external fixation but reflects that although external fixation is appropriate for significant comminution, the significant comminution itself is associated with a significant risk of postoperative complications regardless of the fixation method used 58.
Notably, when used for gunshot or shotgun blasts, external fixation can allow for remarkable healing and bridging of large bony defects. Therefore, external fixation can be used as a temporary damage control measure, to be followed by open reduction and internal fixation (ORIF) at a later date, if needed for stability or occlusion modification.
Pediatric fractures
Pediatric facial trauma accounts for less than 15% or less of all maxillofacial injuries; however, amongst this age group, the mandible was the most commonly fractured facial bone, occurring in 20 to 50% of all facial fractures 59. These patients are managed differently from adult patients for several reasons. First, the pediatric population tends to fracture less significantly, with most fractures being unicortical in nature (greenstick) and minimally displaced. This is thought to be secondary to increased elasticity of the thin cortical bone and the significant adipose tissue cushioning the bones. Additionally, options for immobilization may be limited in this population. The pediatric mandible can be a dynamic anatomic structure with missing and partially erupted teeth at times, as well as tooth surfaces that are not retentive for intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) wiring conversly, plate fixation of the mandible has the potential to disrupt tooth growth, as the mandible is filled with tooth buds during the dentitional transition period. Lastly, children have a thicker periosteal envelope with an increased capacity for bony remodeling. Subsequently, as a result of these factors, the majority of the fractures seen in the pediatric population are managed in a nonoperative or closed manner.
Other differences exist that make pediatric mandibular fractures a distinct breed of injury. Because these cases are largely caused by motor vehicle collisions, a database survey of more than 600 U.S. trauma centers also revealed that these cases also differ in their overall morbidity and mortality compared with those of adult patients 60. About 32% of facial fractures in this age group were admitted to the intensive care unit, with a mean intensive care unit length of stay of 2.9 days and an associated 4% mortality rate. Additionally, the risk of having an associated facial soft tissue injury, brain injury, skull base fracture, or cervical fracture is also substantial.
One of the most common fractures seen in the pediatric population is the condylar fracture 61, which is significant because of its potential to disrupt growth of the mandible and its potential for ankylosis. Diagnosis can be difficult in the pediatric population because of age-related limitations in assessment, but certain presentations, such as bruising or a cut on the chin, should raise one’s suspicion level. Although in the majority of these cases observation plays a prominent role in management, select cases will require fixation.
Closed methods of fixation can be difficult in pediatric patients in whom the permanent tooth roots have developed sufficiently 62, as the deciduous dentition is not able to support the hardware. Transitioning dentition is also troublesome for this end. Subsequently, circummandibular wiring, lingual splints, 4-point fixation with intermaxillary fixation (IMF) screws, open reduction and internal fixation (ORIF), and other forms of fixation are used as alternatives to achieve functional stability. Lingual splints achieve some degree of stability, without any internal hardware, but ultimately require multiple operations to be used appropriately. Open reduction and internal fixation (ORIF) is not commonly performed until late mixed dentition, but may be indicated in the early or mixed dentition in severely dislocated and comminuted fractures, and in patients that are not able to handle intermaxillary fixation (IMF)/maxillomandibular fixation (MMF). Resorbable plates should be considered in young patients with deciduous teeth and mixed dentition, especially in the setting of displaced fractures. If titanium plates are used in the growing mandible (age < 18 years), they should be removed.
Postoperative care
Postoperative management of mandibular fractures generally involves several key steps. At the outset, all patients who have undergone open reduction and internal fixation (ORIF) should be placed on a non-chew diet postoperatively. This will serve to reduce bite forces on the healing mandible and control fracture motion. Patients who are placed in intermaxillary fixation (IMF)/maxillomandibular fixation (MMF) for long periods need to be counseled regarding the significant risk for nutritional issues. Patients need to be instructed to watch their weight and be given calorie supplementation as necessary. Patients also need to be instructed on oral hygiene, and the use of Peridex (3M, St. Paul, MN) oral rinse solution is invaluable for this end. Postoperative imaging should be performed to assess for callus formation and fracture healing, fracture segment alignment, and the status of the occlusion. This can be done with either a Panorex (can be performed in the clinic) or via CT scan (offers better visualization).
Complications
Complications after the management of mandibular fractures are not uncommon, with the most common forms being infectious and malunion/nonunion. Studies have demonstrated that factors such as patient age, sex, location, cause of fracture, associated facial injuries, time to repair, and length of hospitalization were unrelated to the development of complications.5 However, several other factors play significant roles. Smoking and substance abuse play a critical role in outcomes as studies have shown that complication rates increase significantly for these groups when using open reduction and internal fixation (ORIF) 63, with the majority of these (60–72%) being infectious in nature.
Antibiotics play an important role in the management of the postoperative infections; however, the underlying cause in many of the cases is inadequate fixation, and if there is any concern, reoperation and either intermaxillary fixation (IMF)/maxillomandibular fixation (MMF), external fixation, or recon plates should be applied for rigid fixation. Infections that occur within 2 weeks (early infections) tend to be a soft tissue problem that can be treated with drainage, as long as the hardware in place is stable. If there is loose hardware present, however, it must be replaced. Infections occurring after 2 weeks (late infections) are more likely to be caused by inadequate fixation or dental pathology. These require removal of hardware and larger fixation (bigger plates). The role of perioperative and postoperative antibiotics for preventing this complication is currently unclear, as there exist data to support both the benefits and the lack of benefits of their use 64; however, given the degree of equipoise, the standard of care with antibiotics should be undertaken until more definitive evidence is available.
Another feared complication of mandibular fracture treatment is malunions/nonunions. Risk factors have been identified, as studies have shown that having complex fractures nearly doubles the risk of having a mandibular nonunion 65. Other factors affecting the risk of nonunion include poor fixation, osteomyelitis, and patient risk factors, among others. The most important complication to identify and treat, however, is malocclusion. This is generally managed by first evaluating the status of the fixation with either a Panorex or CT scan and subsequently re-plating or placing the patient in intermaxillary fixation (IMF)/maxillomandibular fixation (MMF).
References- Breeland G, Patel BC. Anatomy, Head and Neck, Mandible. [Updated 2018 Oct 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532292
- Ladani P, Sailer HF, Sabnis R. Tessier 30 symphyseal mandibular cleft: early simultaneous soft and hard tissue correction – a case report. J Craniomaxillofac Surg. 2013 Dec;41(8):735-9.
- Wadhwani P, Mathur RM, Kohli M, Sahu R. Mandibular canal variant: a case report. J. Oral Pathol. Med. 2008 Feb;37(2):122-4.
- Saka B, Wree A, Henkel KO, Anders L, Gundlach KK. Blood supply of the mandibular cortex: an experimental study in Göttingen minipigs with special reference to the condyle. J Craniomaxillofac Surg. 2002 Feb;30(1):41-5.
- Lee MH, Kim HJ, Kim DK, Yu SK. Histologic features and fascicular arrangement of the inferior alveolar nerve. Arch. Oral Biol. 2015 Dec;60(12):1736-41.
- Sharma NK, Singh AK, Pandey A, Verma V, Singh S. Temporomandibular joint dislocation. Natl J Maxillofac Surg. 2015;6(1):16-20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4668726/
- Landes CA, Lipphardt R. Prospective evaluation of a pragmatic treatment rationale: Open reduction and internal fixation of displaced and dislocated condyle and condylar head fractures and closed reduction of non-displaced, non-dislocated fractures. Part I: Condyle and sub condylar fractures. Int J Oral Maxillofac Surg. 2005;34:859–70.
- Harstall R, Gratz KW, Zwahlen RA. Mandibular condyle dislocation into the middle cranial fossa: A case report and review of literature. J Trauma. 2005;59:1495–503.
- Vasconcelos BC, Porto GG, Neto JP, Vasconcelos CF. Treatment of chronic mandibular dislocations by eminectomy: Follow-up of 10 cases and literature review. Med Oral Patol Oral Cir Bucal. 2009;14:e593–6.
- Medra AM, Mahrous AM. Glenotemporal osteotomy and bone grafting in the management of chronic recurrent dislocation and hypermobility of the temporomandibular joint. Br J Oral Maxillofac Surg. 2008;46:119–22.
- Bhandari S, Swain M, Dewoolkar LV. Temporomandibular joint dislocation after laryngeal mask airway insertion. The Internet J of Anaesth. 2008;16:1–4.
- Shakya S, Ongole R, Sumanth KN, Denny CE. Chronic bilateral dislocation of temporomandibular joint. Kathmandu Univ Med J (KUMJ) 2010;8:251–6.
- Gupta M, Iyer N, Das D, Nagaraj J. Analysis of different treatment protocols for fractures of condylar process of mandible. J. Oral Maxillofac. Surg. 2012 Jan;70(1):83-91.
- Akinbami BO. Evaluation of the mechanism and principles of management of temporomandibular joint dislocation. Systematic review of literature and a proposed new classification of temporomandibular joint dislocation. Head Face Med. 2011;7:10
- StakesbyLewis JE. A simple technique for reduction of long-standing dislocation of the mandible. Br J Oral Surg. 1981;19:52–6.
- Howe GL. 3rd ed. Wright: Bristol; 1985. Minor Oral Surgery; pp. 393–5.
- Awang MN. A new approach to the reduction of acute dislocation of the temporomandibular joint: A report of three cases. Br J Oral Maxillofac Surg. 1987;25:244–9.
- Vasconcelos BC, Porto GG. Treatment of chronic mandibular dislocations: A comparison between eminectomy and mini plates. J Oral Maxillofac Surg. 2009;67:2599–604.
- Caminiti MF, Weinberg S. Chronic mandibular dislocation: The role of non-surgical and surgical treatment. J Can Dent Assoc. 1998;64:484–91.
- Brachmann F. Eigenblutinjektionen beirezidivierenden, nichtfixierten Kiefergelenkluxationen. Zahnarztl. 1964;15:97.
- Gulses A, Bayar GR, Aydintug YS, Sencimen M, Erdogan E, Agaoglu R. Histological evaluation of the changes in temporomandibular joint capsule and retrodiscal ligament following autologous blood injection. J Craniomaxillofac Surg. 2013;41:316–20.
- Machon V, Abramowicz S, Paska J, Dolwick MF. Autologous blood injection for the treatment of chronic recurrent temporomandibular joint dislocation. J Oral Maxillofac Surg. 2009;67:114–9.
- Hooiveld MJ, Roosendaal G, Jacobs KM, Vianen ME, van den Berg HM, Bijlsma JW, et al. Initiation of degenerative joint damage by experimental bleeding combined with loading of the joint: A possible mechanism of hemophilic arthropathy. Arthritis Rheum. 2004;50:2024–31
- Alons K, Naphausen MT, Von den Hoff JW, van der Kraan PM, Maltha JC, Veltien AA, et al. Induction of haemarthrosis in the TMJ of rats: Validation by M Rimaging (MRI) and histology. J Craniomaxillofac Surg. 2008;37:140–4
- Triantafillidou K, Venetis G, Markos A. Short-term results of autologous blood injection for treatment of habitual TMJ luxation. J Craniofac Surg. 2012;23:689–92.
- Truong DD, Jost WH. Botulinum toxin: Clinical use. Parkinsonism Relat Disord. 2006;12:331–55.
- Ziegler CM, Haag C, Mühling J. Treatment of recurrent temporomandibular joint dislocation with intramuscular botulinum toxin injection. Clin Oral Investig. 2003;7:52–5.
- Martínez-Pérez D, García Ruiz-Espiga P. Recurrent temporomandibular joint dislocation treated with botulinum toxin: Report of 3 cases. J Oral Maxillofac Surg. 2004;62:244–6.
- Brin MF. Botulinum toxin therapy: Basic science and overview of other therapeutic applications. In: Blitzer A, Binder WJ, Carruthers A, editors. Management of Facial Lines and Wrinkles. Philadelphia: Lippincott Williams and Wilkins; 2000. pp. 279–302.
- Freund B, Schwartz M, Symington JM. Botulinum toxin: New treatment for temporomandibular disorders. Br J Oral and Maxillofac Surg. 2000;38:466–71.
- Hall HD, Navarro EZ, Gibbs SJ. Prospective study of modified condylotomy for treatment of non reducing disk displacement. Oral surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:147–58.
- Sindet-Pedersen S. Intraoral myotomy of lateral pterygoid muscle for treatment of recurrent dislocation of the mandibular condyle. J Oral Maxillofac Surg. 1988;46:445–9.
- Laskin DM. Myotomy for the management of recurrent and protracted mandibular dislocations. Trans Int Conf Oral Surg. 1973;4:264–8.
- Adekeye EO, Shamia RI, Cove P. Inverted L-shaped ramus osteotomy for prolonged bilateral dislocation of the temporomandibular joint. Oral Surg Oral Med Oral Pathol. 1976;41:568–77.
- Debnath SC, Kotrashetti SM, Halli R, Baliga S. Bilateral vertical-oblique osteotomy of ramus (external approach) for treatment of a long-standing dislocation of the temporomandibular joint: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e79–82.
- Myrhaug H. A new method of operation for habitual dislocation of the mandible; review of former methods of treatment. Acta Odontol Scand. 1951;9:247–60.
- Kuttenberger JJ, Hardt N. Long-term results following miniplate eminoplasty for treatment of recurrent dislocation and habitual luxation of temporomandibular joint. Int J Oral Maxillofac Surg. 2003;32:474–9.
- Karabouta I. Increasing the articular eminence by the use of blocks of porous coralline hydroxyapatite for treatment of recurrent TMJ dislocation. J Craniomaxillofac Surg. 1990;18:107–13.
- Erdmann D, Follmar K E, Debruijn M, et al. A retrospective analysis of facial fracture etiologies. Ann Plast Surg. 2008;60:398–403.
- Haug R H, Foss J. Maxillofacial injuries in the pediatric patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:126–134.
- The relationship between facial fractures and death from neurologic injury. Plaisier BR, Punjabi AP, Super DM, Haug RH. J Oral Maxillofac Surg. 2000 Jul; 58(7):708-12; discussion 712-3.
- Beirne J C, Butler P E, Brady F A. Cervical spine injuries in patients with facial fractures: a 1-year prospective study. Int J Oral Maxillofac Surg. 1995;24(1 Pt 1):26–29
- Haug R H, Prather J, Indresano A T. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926–932.
- An experimental model for improving fat graft viability and purity. Piasecki JH, Gutowski KA, Lahvis GP, Moreno KI. Plast Reconstr Surg. 2007 Apr 15; 119(5):1571-83.
- Koshy JC, Feldman EM, Chike-Obi CJ, Bullocks JM. Pearls of mandibular trauma management. Semin Plast Surg. 2010;24(4):357-74. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3324216/
- Andreasen J O, Storgård Jensen S, Kofod T, Schwartz O, Hillerup S. Open or closed repositioning of mandibular fractures: is there a difference in healing outcome? A systematic review. Dent Traumatol. 2008;24:17–21.
- Marciani R D, Haley J V, Kohn M W. Patient compliance—a factor in facial trauma repair. Oral Surg Oral Med Oral Pathol. 1990;70:428–430.
- Cohen S R, Leonard D K, Markowitz B L, Manson P N. Acrylic splints for dental alignment in complex facial injuries. Ann Plast Surg. 1993;31:406–412.
- Champy M, Loddé J P, Schmitt R, Jaeger J H, Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg. 1978;6:14–21.
- Haug R H, Street C C, Goltz M. Does plate adaptation affect stability? A biomechanical comparison of locking and nonlocking plates. J Oral Maxillofac Surg. 2002;60:1319–1326.
- Ellis E, III, Graham J. Use of a 2.0-mm locking plate/screw system for mandibular fracture surgery. J Oral Maxillofac Surg. 2002;60:642–645. discussion 645–646.
- Collins C P, Pirinjian-Leonard G, Tolas A, Alcalde R. A prospective randomized clinical trial comparing 2.0-mm locking plates to 2.0-mm standard plates in treatment of mandible fractures. J Oral Maxillofac Surg. 2004;62:1392–1395
- Eckelt U, Schneider M, Erasmus F, et al. Open versus closed treatment of fractures of the mandibular condylar process-a prospective randomized multi-centre study. J Craniomaxillofac Surg. 2006;34:306–314.
- Lee J W, Lee Y C, Kuo Y L. Reappraisal of the surgical strategy in treatment of mandibular condylar fractures. Plast Reconstr Surg. 2010;125:609–619.
- Ellis E, III, Moos K F, el-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985;59:120–129.
- Carinci F, Arduin L, Pagliaro F, Zollino I, Brunelli G, Cenzi R. Scoring mandibular fractures: a tool for staging diagnosis, planning treatment, and predicting prognosis. J Trauma. 2009;66:215–219.
- Foster R D, Anthony J P, Sharma A, Pogrel M A. Vascularized bone flaps versus nonvascularized bone grafts for mandibular reconstruction: an outcome analysis of primary bony union and endosseous implant success. Head Neck. 1999;21:66–71
- Ellis E, III, Muniz O, Anand K. Treatment considerations for comminuted mandibular fractures. J Oral Maxillofac Surg. 2003;61:861–870.
- Imahara S D, Hopper R A, Wang J, Rivara F P, Klein M B. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg. 2008;207:710–716
- Eskitascioglu T, Ozyazgan I, Coruh A, Gunay G K, Yuksel E. Retrospective analysis of two hundred thirty-five pediatric mandibular fracture cases. Ann Plast Surg. 2009;63:522–530
- Ferreira P C, Amarante J M, Silva P N, et al. Retrospective study of 1251 maxillofacial fractures in children and adolescents. Plast Reconstr Surg. 2005;115:1500–1508.
- Smartt J M, Jr, Low D W, Bartlett S P. The pediatric mandible: II. Management of traumatic injury or fracture. Plast Reconstr Surg. 2005;116:28e–41e
- Serena-Gómez E, Passeri L A. Complications of mandible fractures related to substance abuse. J Oral Maxillofac Surg. 2008;66:2028–2034.
- Abubaker A O, Rollert M K. Postoperative antibiotic prophylaxis in mandibular fractures: a preliminary randomized, double-blind, and placebo-controlled clinical study. J Oral Maxillofac Surg. 2001;59:1415–1419
- Mathog R H, Toma V, Clayman L, Wolf S. Nonunion of the mandible: an analysis of contributing factors. J Oral Maxillofac Surg. 2000;58:746–752. discussion 752–753.