Metacarpal fracture
Metacarpal fracture is usually the injury described as ‘a broken hand’, is a fracture in one of the five bones that are located in the palm of your hand that connect your wrist to your thumb and fingers. Metacarpal fractures are common. Fractures of the metacarpal bones account for 10% of all fractures and 40% of all hand fractures 1. The lifetime incidence of a metacarpal fracture is 2.5%. Some metacarpal fractures can be managed nonoperatively with immobilization like wearing a splint or a cast. For certain intra-articular fractures, displaced and angulated fractures, unstable fracture patterns, combined or open injuries, as well as irreducible and unstable dislocations, surgical intervention may be required for restoration of function and appearance. Most metacarpal fractures occur in the active and working population, particularly adolescents and young adults.
Fractures of the metacarpal bone either involve the proximal base, the shaft, neck, or the distal head. The neck and shaft are more commonly injured in contradiction to the first metacarpal where the base is most often involved.
Fractures of the metacarpal head are by definition intra-articular, and are rarer than fractures involving the distal parts of the bone. The second metacarpal is the most common to be injured, and the cause is often as a result of a direct blow or crush injury. Fractures in this region are often comminuted, causing additional difficulty with their management. These injuries generally require open reduction and fixation although it is reported that metacarpal head fractures can be treated conservatively, with good long-term outcome if there is less than 25% joint involvement 2.
The neck of metacarpal is the most common site of fracture and is greatest in the 4th and 5th metacarpals. The shaft of the metacarpal is also referred to as the body. The shaft can be fractured in 3 ways, oblique, transverse or spiral, and comminuted with the least protected fifth metacarpal at highest risk of injury 2. Rotational deformity is greater in injuries to the shaft.
Both neck and shaft fractures are characteristically related to axial loading or direct trauma. Both typically angulate with a dorsal apex. This angulation is often accepted due to the carpometacarpal joint range of movement that can compensate for angles up to 10-15 degrees in the index and middle finger, and 20 degrees in the ring. The more proximal the fracture generally the greater the angulation, and the more noticeable any hand deformity such as clawing becomes. It has been reported that volar angles up to 70 degrees have been tolerated with conservative management and no long-term functional deficit 3.
The Boxer’s fracture is a fracture involving the fifth metacarpal neck (see Figure 5). There is no stabilization along its ulnar aspect (the other digits have a neighboring bone) and therefore fractures result in the metacarpal head being freed from any proximal attachments. This allows the head to rest in a greater volar angle and if left long term causes reduced metacarpal flexion due to collateral ligament shortening. Angulation of the head below 30-40 degrees is often acceptable in the fifth metacarpal, again thanks to carpometacarpal joint movements 4 and again angles up to 70 degrees have been successfully managed conservatively 5.
Fractures at the metacarpal base are the most stable of the metacarpal fractures due to both dorsal and palmar carpometacarpal, and the interosseous, ligaments. This stability is greatest in the second and third digits as there is some greater mobility allowed in the ulnar sided fourth and fifth digits 6.
They are generally classed as intra or extra-articular. Insertion of the flexor and extensor carpi muscles into the metacarpal bases (radialis into the second and third metacarpal, and ulnaris into the fourth and fifth) can potentially aggravate any deformities 7. Intra-articular base of metacarpal fractures are uncommon but there may have a tendency of being both under-reported and diagnosed thanks to the stability of the surrounding structures 8.
Management of fractures to the metacarpal bones of the hand is decided on both the clinical examination and radiological findings. The reasons behind this are that the hands long-term function is often dependant on the fractures angulation and rotation.
The key parts of the clinical examination is to assess the degree of rotational deformity, and whether there is any soft tissue compromise, including evidence of compound fractures with or without the involvement of a ‘fight bite.’ This term relates to the high incident of hand fractures secondary to punches and that a number of these involve a punch to an individual’s mouth and thus an accidental ‘bite’ to the skin. Inability to extend at the metacarpophalangeal joint also correlates to increased need of operative fixation.
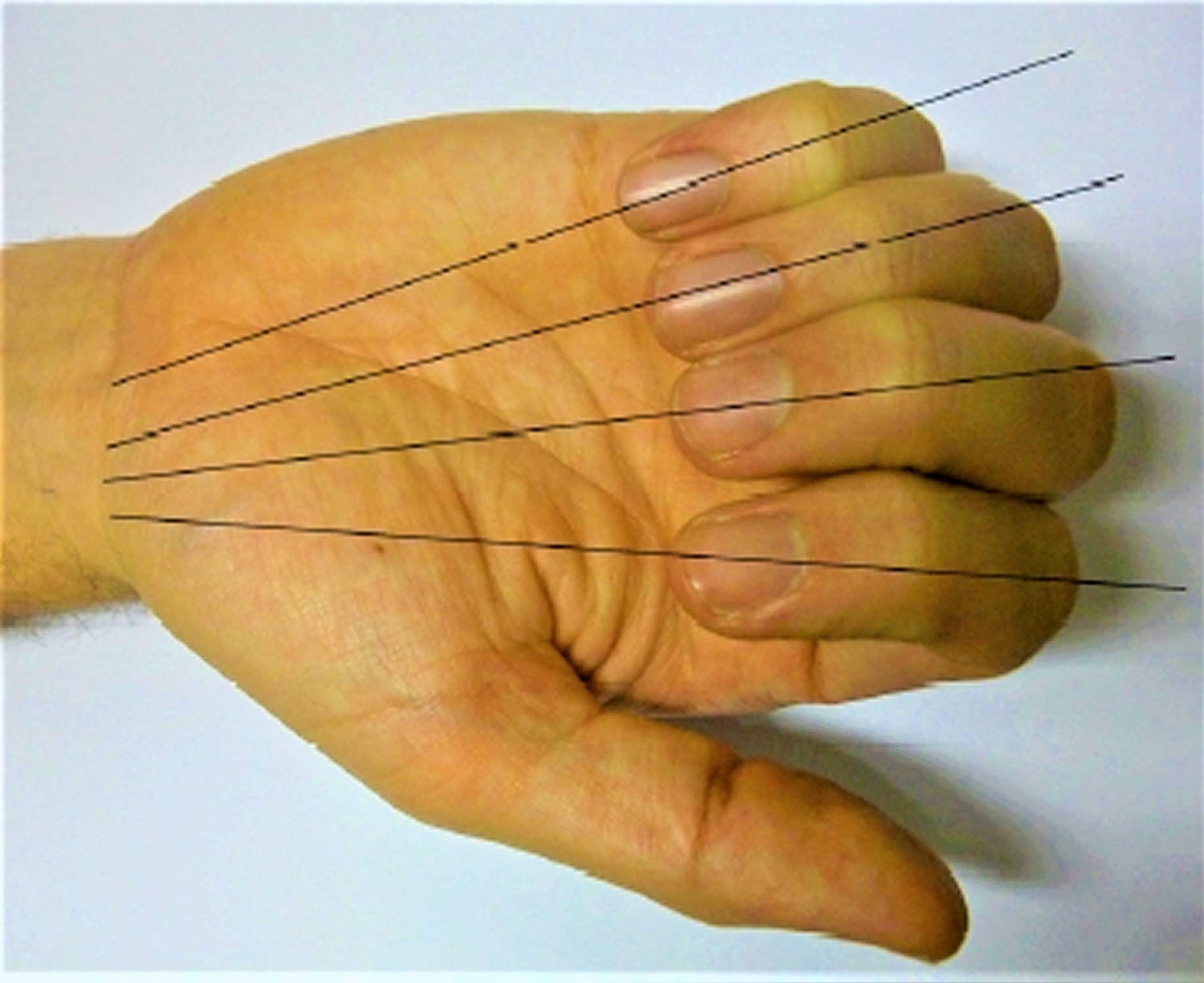
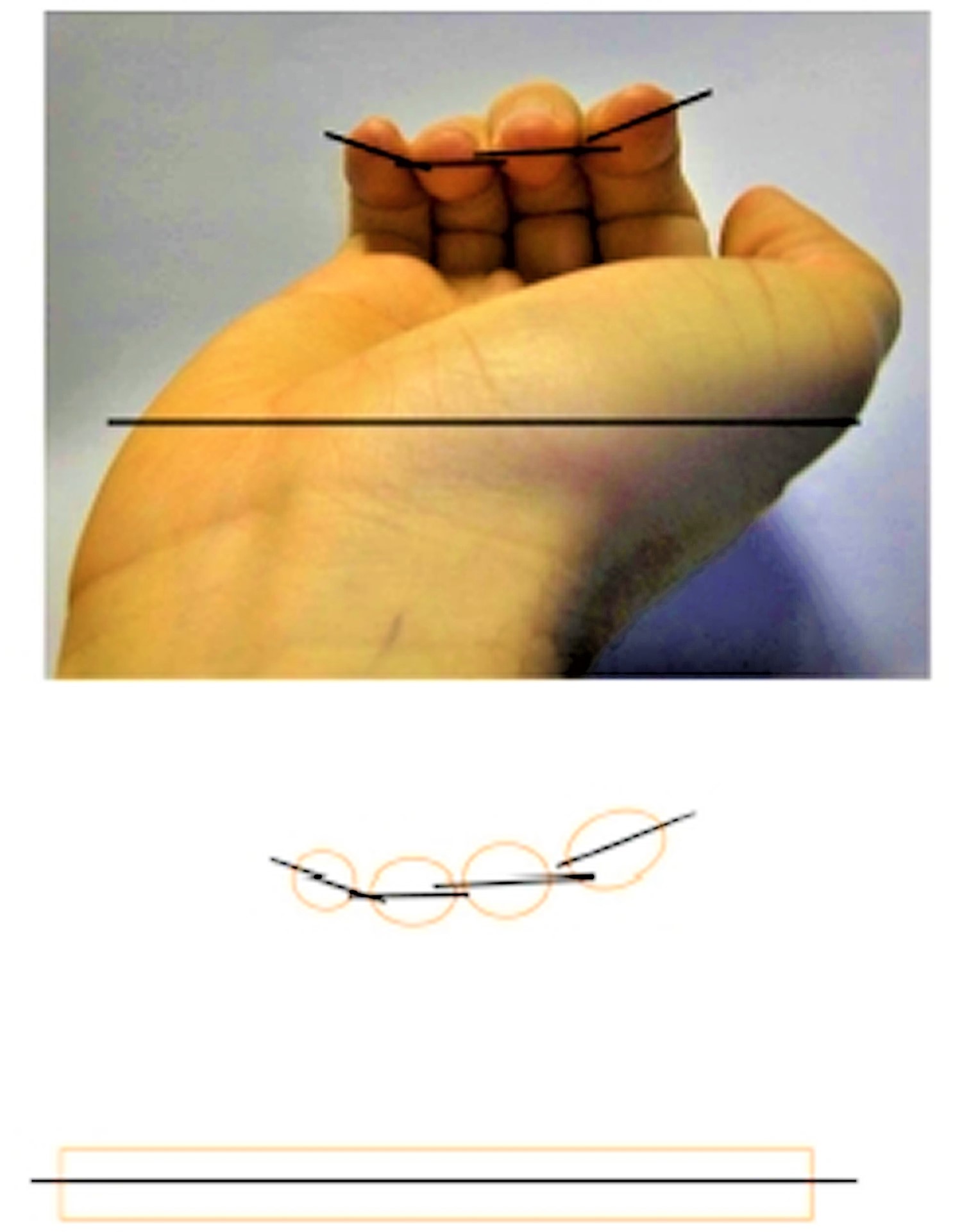
Rotation of the digit impacts greatly on functional grip, and can be a source of chronic pain 9. lt is best assessed by asking the patient to make a fist. The digits of all 4 fingers should point towards the scaphoid tubercle, without overlapping with the metacarpophalangeal joint and proximal interphalangeal joint flexed (Figure 2). Likewise the nail should appear parallel to the hand and neighbouring digits when looking end-on (Figure 3). The digits should then tuck in as the distal interphalangeal joint is flexed, although pain often restricts a degree of the flexion of all these joints. Comparison should be made to the other hand, but there is now a feeling that both digit overlap and nail alignment vary greatly within the population, making the clinical examination all the more difficul 10.
The radiological findings correlate to the angulation of the fracture, as well as metacarpal shortening. Metacarpal shortening appears to consequently affect interosseous function with a 10mm loss of length corresponding to up to 55% muscle power loss 11.
Radiological views of the individual metacarpals are not possible. Posteroanterior and oblique views are mandatory. Ulnar digit injury lateral views should be optimally taken with 30-degrees pronation, and the radial digits with 30 degrees supination. However, angulation of the metacarpal bones is often best seen with a true lateral view. The Brewerton view can be useful if collateral ligament avulsion injury is suggested, and is taken with the metacarpophalangeal joint flexed at 65 degrees and the radiological view angled at a 15-degree angle ulnar to radial 7.
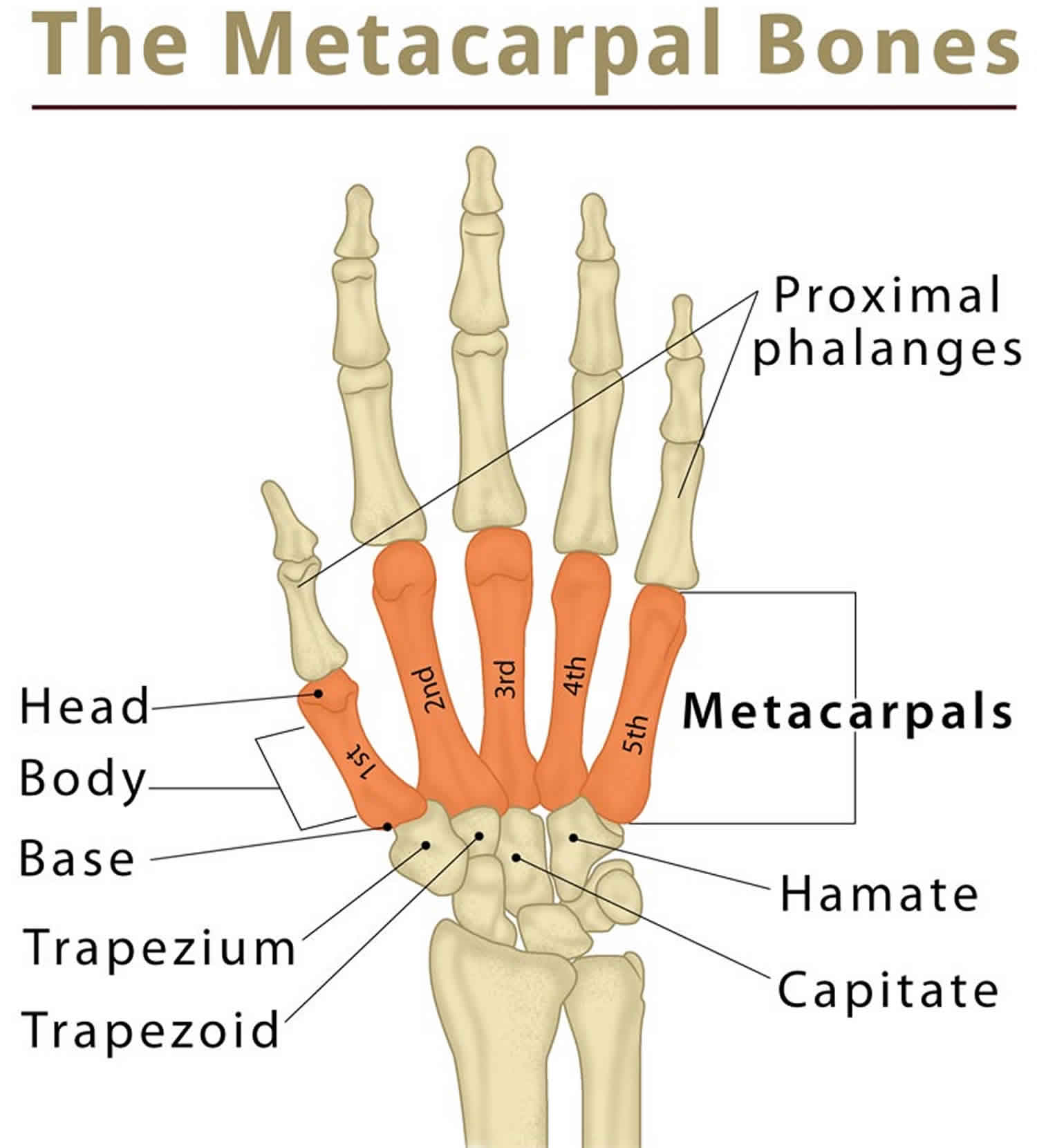
Metacarpal anatomy
Patterns of metacarpal injuries result from the unique anatomy of the hand. Metacarpals are long tubular bones with an intrinsic longitudinal arch and a collective transverse arch. Bones are concave on the palmar surface and are joined proximally and distally by ligamentous attachments.
The second and third metacarpals are fixed rigidly at their bases, whereas the fourth and fifth carpometacarpal joints are capable of at least 15° and 25° of motion, respectively. The thumb carpometacarpal saddle joint is highly mobile, and its unique motion and injury patterns are addressed more fully elsewhere. Briefly, a Bennett fracture is a fracture of the base of the thumb resulting from forced abduction of the first metacarpal. It is defined as an intra-articular two-part fracture of the base of the first metacarpal bone. Rolando fracture is a three-part or comminuted intra-articular fracture-dislocation of the base of the thumb (proximal first metacarpal). Rolando fracture can be thought of as a comminuted Bennett fracture.
The carpometacarpal joints of the second and third metacarpals are very stable, and there is very little relative motion at these joints. The sawtooth articular arrangement combined and the strong dorsal and palmar carpometacarpal ligaments and metacarpal ligaments form very strong and relatively immobile joint capsules.
These joints are further stabilized by extensor carpi radialis longus and brevis tendon insertions on the bases of the second and third metacarpals, respectively. The insertion of the flexor carpi radialis at the base of the second metacarpal contributes as well. The articulation with the hamate and the fourth and fifth metatarsal bases allows for much freer movement, but the carpometacarpal and metacarpal ligaments are still very strong.
The insertion of the extensor carpi ulnaris on the dorsal aspect of the ulnar fifth metacarpal base often provides a deforming force in fractures of the fifth metacarpal. Articular fractures of the base of the fifth metacarpal often occur between the metacarpal ligament insertions and the insertion of the extensor carpi ulnaris, resulting in proximal and dorsal migration of the fractured metacarpal due to the unopposed tendon action often called “reverse Bennett fracture” due to its similarity to the injury in the thumb. A reverse Bennett fracture-dislocation is a fracture-dislocation of the base of the 5th metacarpal bone. It is pathologically and radiographically analogous to the Bennett fracture of the thumb. A reverse Bennett fracture-dislocation is quite unstable due to unopposed extensor carpi ulnaris pull on the fracture fragment, which causes migration and subluxation of the fragment.
The metacarpophalangeal joints are multiaxial condyloid joints capable of flexion, extension, and some lateral motion and circumduction. The cam-shape of the metacarpal heads leads to relaxation of the collateral ligaments in extension, permitting adduction and abduction of the finger. With about 70° of metacarpophalangeal joint flexion, the collateral ligaments become taut, stabilizing the finger for power pinch and grip.
Increased tension in the collateral ligaments with metacarpophalangeal flexion can be helpful in stabilizing the metacarpal head during reduction of a metacarpal neck fracture. metacarpophalangeal joints are routinely immobilized in at least 70° of flexion to maintain maximum stretch of these ligaments, thus lessening postimmobilization stiffness.
The volar plate is a cartilaginous structure on the palmar aspect of each metacarpophalangeal joint, which limits extension of the joint. The volar plate is thicker at its insertions on the proximal phalanges and weaker at the proximal metacarpal origin. Volar plates are interconnected through deep transverse intermetacarpal ligaments, which provide additional volar stability.
Figure 1. Metacarpal fracture
Figure 2. Direction of the fingers when flexing to make a fist pointing towards the area of the scaphoid tubercle. These lines are disrupted when the finger is rotated with the the rotated finger lying under neighbouring digits.
[Source 7 ]Figure 3. Examination of rotation of the fractured digit. The fingers should be held with the metacarpophalangeal joint, proximal and distal interphalangeal joint flexed and the angle of the nail should correspond to the plane of the palm. Some rotation may be normal for the patient (as in index and little finger in example).
[Source 7 ]Figure 4. Fifth metacarpal fracture base (reverse Bennett fracture)
Figure 5. Fifth metacarpal fracture neck (boxer’s fracture)
Metacarpal fracture symptoms
Injuries to metacarpal base
Many fractures and fracture dislocations of the metacarpal base are caused by substantial axial loads and frequently are associated with other injuries. Diagnosis usually is directed by the history and clinical examination. Tenderness, swelling, and loss of motion are common, as with any fracture or dislocation. Additionally, dorsal carpometacarpal joint dislocations may be associated with marked swelling and sometimes a palpable stepoff. Stress of the fifth metacarpal reveals instability in cases of intra-articular fractures of that metacarpal base.
Metacarpal shaft and neck fractures
Problems associated with metacarpal shaft fractures relate to shortening, rotation, and dorsal apex angulation. Of these, malrotation is the most critical. Minor rotational deformities can cause the fingers to overlap when the hand is made into a fist.
Rotational abnormalities are best judged clinically by comparing the injured and uninjured digits through a full range of motion (ROM). With flexion, each digit should point toward the scaphoid tuberosity. The plane of the nail should be similar between the injured digit and the contralateral corresponding finger when evaluated in an intrinsic plus position.
Like shaft fractures, metacarpal neck fractures usually are easily diagnosed by localized tenderness and swelling with loss of dorsal knuckle contour. The ring and small metacarpals are most commonly fractured.
Injuries to metacarpal head
Pain, swelling, and loss of motion are the key clinical signs of injury to the metacarpophalangeal joint. Crepitus may be present with motion in intra-articular injuries.
Metacarpal fracture diagnosis
Plain radiography is the primary means of evaluating hand injuries beyond the history and physical examination. Any significant injury to the hand should be assessed with posteroanterior (PA), lateral, and oblique views. A 30° pronated lateral view for second and third metacarpal fractures and a 30° supinated lateral view for fourth and fifth metacarpal fractures are helpful 12.
Metacarpal head fractures
Evaluation of these injuries may require additional imaging studies. Specifically, tomograms or CT scans may be necessary to visualize the fracture and degree of articular displacement.
The Brewerton view (metacarpophalangeal joint flexed 65° with the dorsum of the proximal phalanx flat against the radiograph cassette and the beam angled 15° ulnar to radial) profiles the collateral recesses and is helpful for collateral ligament avulsion fractures.
Metacarpophalangeal dislocations
Most commonly, lateral radiographs reveal the dorsal displacement of the proximal phalanx. In more severe and complex dislocations, there may also coexist a metacarpal head fracture.
Carpometacarpal injuries
Carpometacarpal fractures and dislocations are frequently difficult to visualize or fully characterize with standard radiographic projections. Additional oblique views, fluoroscopy, or computed tomography (CT) may be necessary. Additionally, traction radiographs can sometimes best demonstrate the bony and ligamentous injuries and their severity. This is accomplished by distracting the involved digits and obtaining multiple radiographic views.
Carpometacarpal dislocation results in subtle loss of joint space as viewed on the anteroposterior (AP) projection. Often, this is seen as a broken sawtooth sign at the carpometacarpal joint. This sign may be accompanied by displacement noted on lateral or oblique views.
Assessing closely for other additional injuries is important. Because significant force is required to disrupt the strong carpometacarpal ligaments, fracture-dislocation of one carpometacarpal joint is often accompanied by an injury to one or more of its neighbors.
Metacarpal fracture treatment
Most metacarpal injuries are managed by sedation or local anesthesia, followed by closed reduction and immobilization or sometimes controlled mobilization utilizing a forearm-based splint and held in place with a loose compressive wrap 13. The goals of nonoperative management are to obtain alignment and stability and to begin motion of the fingers and wrist as soon as possible. Generally acceptable reduction of metacarpal fractures includes articular congruity of less than 2 mm and angulation and rotation that do not interfere with function or cause significant cosmetic deformity.
Immobilization of most metacarpal fractures follows a few simple guidelines, including the following:
- Fracture splints should be forearm-based and should allow for motion of the interphalangeal joints
- Splints should extend over the dorsal and palmar aspect of the entire metacarpal being treated
- Generally, the wrist should be placed in 20-30° of extension; the metacarpophalangeal (MCP) joints should be immobilized in 70-90° of flexion, with the dorsal aspect of the splint extending to the interphalangeal joints; and the volar aspect should end at the distal palmar crease
- Buddy taping the fingers of the involved metacarpal can aid in maintaining rotational control
- After a short period of immobilization, patients may be encouraged to use the fingers on the affected hand to maintain motion
Indications for surgical treatment include the following:
- Failure to achieve or maintain acceptable reduction using closed techniques
- Open fractures
- Multiple hand fractures
- Complex injuries
- Displaced intra-articular fractures
- Fractures with severe soft-tissue loss requiring a stable skeleton
No absolute contraindications exist for treatment of metacarpal injuries. Almost all injuries are amenable to either immobilization or closed or open reduction, with or without fixation.
Bioresorbable implants are being used more frequently for fixation of fractures. Biomechanical testing of polyglycolic acid and poly–L-lactic acid plates compare favorably in rigidity to titanium but are inferior in torsional testing. Self-reinforced polyglycolic acid rods used in place of K-wires for intramedullary fixation have an initial bending stiffness of only 60% of stainless-steel wires. When subjected to saline bath, polyglycolic acid rods lose stability within 4 weeks.
New techniques and equipment may make these implants more cost-effective, and their use precludes the need for implant removal at a second operation. Further development of low-profile implants may allow more rigid fixation for certain problem fractures, thereby minimizing postoperative stiffness and perhaps diminishing the need for metal removal.
Metacarpal base fractures and dislocation
Impaction fractures of the metacarpal bases that are not significantly displaced can be treated with splinting, followed by early mobilization.
Fractures of the metacarpal base require reduction if there is greater than 2 mm of articular surface displacement or if there is significant angular deformity or dislocation of the carpometacarpal joint. Anesthesia for the reduction is usually accomplished by conscious sedation or regional block; local hematoma block is usually inadequate.
The reduction is accomplished using a combination of traction and direct digital pressure, usually by the physician’s thumb. The wrist should be splinted in 20-30° of extension after reduction in order to decrease the deforming pull of the wrist extensors, and the metacarpophalangeal joints should be flexed.
Immobilization of reduced metacarpal base fractures or nondisplaced fractures should be continued for a minimum of 3-4 weeks. Active motion of the finger IP joints should be encouraged throughout the immobilization period.
Carpometacarpal dislocations and fracture-dislocations, especially when multiple, are unstable injuries. In the past, these fractures were managed by closed reduction and external immobilization, which frequently lead to grip weakness and residual pain. The current literature supports closed reduction, if joint congruity can be obtained, but with the addition of internal fixation.
Displaced fracture-dislocations of the fourth and fifth metacarpals, which are accompanied by fracture of the dorsal hamate, require open reduction and internal fixation (ORIF). Reverse Bennett fractures frequently need Kirschner-wire (K-wire) stabilization to counteract the deforming forces. If little articular incongruity is present, this may be a closed procedure.
Metacarpal shaft fractures
Most closed metacarpal shaft fractures are best treated nonoperatively. Because of the adjacent intact metacarpals and the strong intermetacarpal ligaments, isolated third and fourth metacarpal fractures are particularly stable.
The amount of acceptable angulation varies depending on the location of the metacarpal fracture and the specific metacarpal involved. Less angulation can be accepted in metacarpal fractures closer to the carpometacarpal joints, as the amount of deformity appears accentuated. Greater angular deformity can be accepted in the fourth and fifth metacarpals, because the greater mobility of the carpometacarpal joints compensates for this deformity.
Metacarpal shaft fractures tend to angulate apex dorsal with the head displaced palmarly due to the deforming pull of the interossei muscles. Only small amounts of angulation (≤10°) are acceptable in the second and third metacarpals. The fourth and fifth finger metacarpals are much more mobile, and 20° for the fourth metacarpal and 30° for the fifth metacarpal, can be accepted. The more proximal the fracture, the more pronounced the deformity and the less angulation that can be accepted. Any malrotation is an indication for surgical intervention. Shortening from 3-4 mm is well tolerated.
In addition to fractures that cannot be reduced and stabilized closed, fractures such as open fractures, multiple fractures, and malreduced subacute fractures are best addressed surgically.
Reduction of displaced metacarpal shaft fractures is best accomplished by using a technique developed by Jhass 14. The fracture is anesthetized with the hematoma block. The affected finger metacarpophalangeal joint and the proximal interphalangeal joints are flexed to 90°, and the fracture is reduced by applying upward pressure on the middle phalanx and downward pressure over the dorsal apex of the fracture. Flexing of the metacarpophalangeal joint tightens the collateral ligaments and provides a rigid lever for reduction. The finger then can be used to control or correct the rotation.
After reduction, the fracture is held via splinting or can be pinned to maintain reduction. Do not use the Jahss splinting technique (ie, the finger is kept in flexion with upward force applied across the proximal interphalangeal joint), because the risk of skin necrosis and flexor contracture is prohibitive. Immobilization should be limited to less than 4 weeks, as stiffness and tendon adhesion limit range of motion and lead to an unfavorable result.
Metacarpal neck fractures
Minimally angulated or displaced metacarpal fractures can be managed with simple immobilization for 3-4 weeks. The degree of acceptable angulation is controversial.
Most surgeons agree that no more than 10-15° of angulation in the second and third metacarpals should be accepted without reduction. The lateral digits are more mobile at the carpometacarpal joint and function well with greater amounts of angulation of the metacarpal shaft or neck. Though some studies have shown little disability associated with fifth metacarpal neck fractures angulated as much as 70°, most surgeons advocate reduction of those fractures with more than 45° of angulation. This level of angulation is especially true for boxer’s fractures of the fifth metacarpal neck. Despite overall good functional results, this degree of angulation alters dorsal knuckle contour and may result in a tender palmar mass with heavy gripping. Though quite unusual, fracture rotation is an indication for surgical intervention.
As in other fractures of the hand, no rotational deformity is acceptable, as the resultant finger overlap with grip leads to weakness and disability. Reduction of metacarpal neck fractures is accomplished by the same method as metacarpal shaft fractures. Closed reduction and immobilization with splints or casts has been shown to maintain approximately 50% of the initial deformity correction.
Metacarpal head fractures
Except for some collateral ligament avulsion fractures, metacarpal head fractures are intra-articular and, if displaced, should be treated with open reduction and internal fixation (ORIF), the goal being anatomic reduction and early mobilization.
Nondisplaced fractures can be managed with splinting for 3 weeks, followed by gentle motion. Fractures in which the articular surface is displaced greater than 1-2 mm should be managed operatively. Splinting of metacarpal head fractures should incorporate the metacarpophalangeal joint. This can be accomplished with the ulnar gutter splint for fourth and fifth metacarpal fractures.
Metacarpophalangeal dislocations
Dorsal metacarpophalangeal dislocations are classified as simple or complex. Both are the result of hyperextension injuries with avulsion of the palmar plate. The distinction between the two types is the difficulty of reduction.
Simple dislocations are easy to diagnose because the metacarpophalangeal joint rests in 60-90° of hyperextension. In this injury, the volar plate is distracted and not interposed between the bone ends.
Reduction of simple metacarpophalangeal dislocations is carried out easily with local or regional anesthesia in the emergency department. The wrist and IP joints are flexed—and the finger is very gently distracted—and a volarly directed force from the dorsum brings the joint into at least 50° of flexion. One must avoid hyperextension (accentuation of the deformity) during reduction so as to not interpose the volar plate. Immediate motion can then be started in a dorsal block splint that prohibits extension beyond 30°.
Metacarpophalangeal dislocations that are not readily reducible are characterized as complex. The reduction is prevented by either interposed soft tissue or “buttonholing” of the metacarpal head. On presentation, the metacarpophalangeal joint is only slightly hyperextended with the distal joints mildly flexed. The involved digit deviates toward the adjacent central digit. A prominence is present in the palm with dimpling of the skin in the area of the proximal volar crease. Dorsally, a depression is palpable proximal to the base of the proximal phalanx. The patient cannot actively flex the digit. These dislocations require operative reduction.
Fifth metacarpal fracture
Specific names are given to the fifth metacarpal fractures:
- Fracture dislocation of the base of the 5th metacarpal also called reverse Bennett fracture dislocation. A reverse Bennett fracture-dislocation is a fracture-dislocation of the base of the 5th metacarpal bone. It is pathologically and radiographically analogous to the Bennett fracture of the thumb. It is quite unstable due to unopposed extensor carpi ulnaris pull on the fracture fragment, which causes migration and subluxation of the fragment.
- Fracture of 5th metacarpal neck also called Boxer fracture. Boxer fractures are minimally comminuted (fracture producing multiple bone fragments), transverse fractures of the 5th metacarpal and are the most common type of metacarpal fracture. They typically occur (as the name suggests) when punching and are a common sight in all emergency departments on Friday nights. Boxer fractures are an impaction injury (axial loading of the 5th metacarpal) almost always result as a consequence of a direct blow with a clenched fist against a solid surface. Typical solid surfaces are human faces or walls. It is, therefore, no surprise that young adult males are by far the most commonly affected group (~95%) 15.
Fractures through the base of the fifth metacarpal require special consideration. Fifth metacarpal fractures are often intra-articular, with the fracture line between the insertion of the strong intermetacarpal ligaments and the insertion of the extensor carpi ulnaris tendon. The pull of the extensor carpi ulnaris becomes a deforming force, causing the fractured metacarpal to displace proximally and dorsally. This is similar to the Bennett fracture of the thumb (“reverse Bennett fracture”).
Management of fifth metacarpal fractures usually requires open reduction and internal fixation (ORIF) or closed reduction and percutaneous pinning to counteract the strong force of the extensor carpi ulnaris. Minimally or nondisplaced fractures should be splinted in the same manner described for other carpometacarpal injuries.
References- Ashkenaze DM, Ruby LK. Metacarpal fractures and dislocations. Orthop Clin North Am. 1992;23:19.
- Green DP, Pederson WC, Hotchkiss RN, Wolfe SW. Greens operative hand surgery. 5th. Churchill Livingstone, London, UK: Elsevier Health Sciences; 2005.
- Ford DJ, Ali MS, Steel WM. Fractures of the fifth metacarpal neck: is reduction or immobilisation necessary? J Hand Surg. 1989;14B:165–7.
- Birndorf MS, Daley R, Greenwald DP. Metacarpal fracture angulation decreases flexor mechanical efficiency in human hands. Plast Reconstr Surg. 1997;9(4):1079–83.
- Statius Muller MG, Poolman RW, van Hoogstraten MJ, Steller EP. Immediate mobilization gives good results in boxer’s fractures with volar angulation up to 70 degrees: a prospective randomized trial comparing immediate mobilization with cast immobilization. Arch Orthop Trauma Surg. 2003;123(10):534–7.
- El-Shennawy M, Nakamura K, Patterson RM, Viegas SF. Three-dimensional kinematic analysis of the second through fifth carpometacarpal joints. J Hand Surg. 2002;26A:1030–5.
- Haughton D, Jordan D, Malahias M, Hindocha S, Khan W. Principles of hand fracture management. Open Orthop J. 2012;6:43–53. doi:10.2174/1874325001206010043 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3296112
- Crichlow TP, Hoskinson J. Avulsion fracture of the index metacarpal base: three case reports. J Hand Surg. 1988;3A:212–4.
- Bulcher U, Gupta A, Ruf S. Corrective osteotomy for post-traumatic malunion of the phalanges in the hand. J Hand Surg Br . 1996;1:33–42.
- Lahey PJ, Patel A, Kang KK, Patel MR, Choueka J. Assessing rotational deformity of the little finger. Orthopaedics. 2011;34(7):287.
- Meunier MJ, Hentzen E, Ryan M, Shin AY, Lieber RL. Predicted effects of metacarpal shortening on interosseous muscle function. The Journal of Hand Surgery. 2004;29(4):689–93.
- Westbrook AP, Davis TR. An evaluation of a clinical method to assess malunion of little finger metacarpal fractures. J Hand Surg Eur Vol. 2007 Dec. 32(6):641-6.
- Giddins GE. The non-operative management of hand fractures. J Hand Surg Eur Vol. 2015 Jan. 40 (1):33-41.
- Jhass S. Fractures of the metacarpals – a new method of reduction and immobilization. J Bone Joint Surg. 1938. 20 (1):178-186.
- Porter ML, Hodgkinson JP, Hirst P et-al. The boxers’ fracture: a prospective study of functional recovery. Arch Emerg Med. 1988;5 (4): 212-5.