Metastatic adenocarcinoma
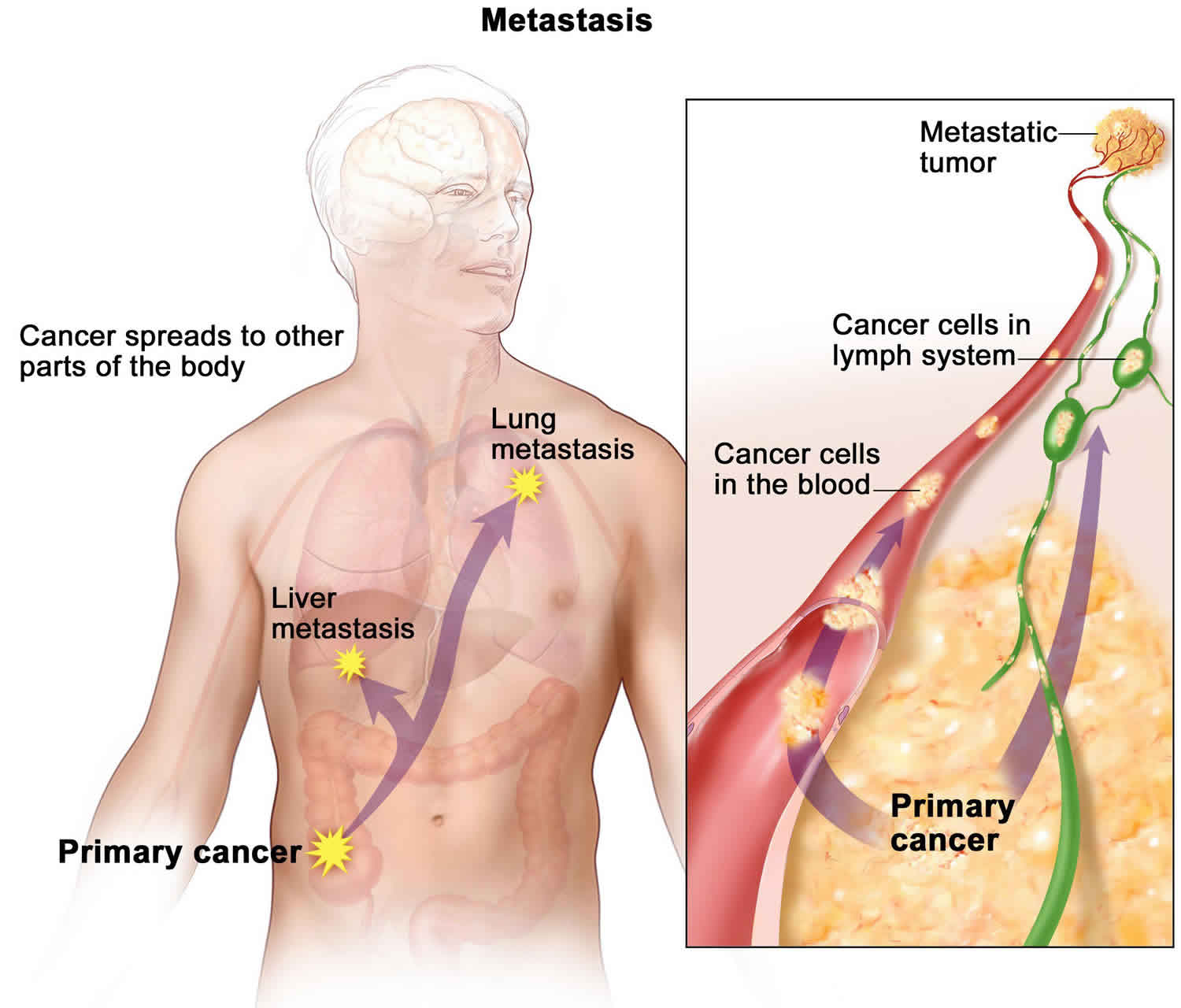
Metastatic adenocarcinoma means malignant cancer of glandular origin, or resembling glandular secretory properties has spread to a different body part from where it started. When this happens, doctors say the cancer has “metastasized.” Your doctor may also call it “metastatic cancer,” “advanced cancer,” or “stage 4 cancer.” But these terms can have different meanings. For example, a cancer that is large but has not spread to another body part can also be called advanced cancer or locally advanced cancer. Ask your doctor to explain where the cancer has spread. Metastases most commonly develop when cancer cells break away from the main tumor and enter the bloodstream or lymphatic system. These systems carry fluids around the body. Common sites are lymph nodes, lungs, liver, and bones. May invade pancreas, breast, small intestine, and prostate. Signs and symptoms include abdominal pain, bone pain, cachexia, diarrhea, dyspnea, hepatomegaly, icterus, regional lymphadenopathy, and vomiting.
Glandular (secretory) cells are found in tissue that lines certain internal organs and makes and releases substances in the body, such as mucus, digestive juices, or other fluids. Most cancers of the breast, pancreas, lung, prostate, and colon are adenocarcinomas. When metastatic, it can behave in a site-specific way depending on where the cancer has spread. Metastatic adenocarcinoma may manifest in the brain, liver, lung, lymph nodes, bone, and even bone marrow.
Treatment depends on the extent and location of the metastases. Treatment of specific organ systems should follow treatment guidelines for that organ system, as in the case of prostate or breast cancer. Treatments can include chemotherapy, radiation therapy, and resection.
What is metastatic cancer?
The main reason that cancer is so serious is its ability to spread in the body. Cancer cells can spread locally by moving into nearby normal tissue. Cancer can also spread regionally, to nearby lymph nodes, tissues, or organs. And it can spread to distant parts of the body. When this happens, it is called metastatic cancer. For many types of cancer, it is also called stage IV (four) cancer. The process by which cancer cells spread to other parts of the body is called metastasis.
When observed under a microscope and tested in other ways, metastatic cancer cells have features like that of the primary cancer and not like the cells in the place where the cancer is found. This is how doctors can tell that it is cancer that has spread from another part of the body.
Metastatic cancer has the same name as the primary cancer. For example, breast cancer that spreads to the lung is called metastatic breast cancer, not lung cancer. It is treated as stage IV breast cancer, not as lung cancer.
Sometimes when people are diagnosed with metastatic cancer, doctors cannot tell where it started. This type of cancer is called cancer of unknown primary origin.
When a new primary cancer occurs in a person with a history of cancer, it is known as a second primary cancer. Second primary cancers are rare. Most of the time, when someone who has had cancer has cancer again, it means the first primary cancer has returned.
Is metastatic adenocarcinoma the same type of cancer as before?
Yes, a cancer that has spread to another area is given the same name as the original cancer. For example, a breast cancer that spreads to the liver is called metastatic breast cancer, not liver cancer. This is because the cancer started in the breast and the treatment used is for breast cancer.
How do metastatic adenocarcinoma develop?
Metastases (plural form of metastasis) most commonly develop when cancer cells break away from the main tumor and enter the bloodstream or lymphatic system. These systems carry fluids around the body. This means that the cancer cells can travel far from the original tumor and form new tumors when they settle and grow in a different part of the body.
Metastases can also sometimes develop when cancer cells from the main tumor, typically in the belly, or abdominal cavity, break off and grow in nearby areas, such as in the liver, lungs, or bones.
Any type of cancer can spread. Whether this happens depends on several factors, including:
- The type of cancer. Some cancers are more likely to spread than others.
- How fast the cancer is growing
- Other factors about the behavior of the cancer that your doctor may find.
Cancer cells spread through the body in a series of steps. These steps include:
- Growing into, or invading, nearby normal tissue
- Moving through the walls of nearby lymph nodes or blood vessels
- Traveling through the lymphatic system and bloodstream to other parts of the body
- Stopping in small blood vessels at a distant location, invading the blood vessel walls, and moving into the surrounding tissue
- Growing in this tissue until a tiny tumor forms
- Causing new blood vessels to grow, which creates a blood supply that allows the tumor to continue growing
Most of the time, spreading cancer cells die at some point in this process. But, as long as conditions are favorable for the cancer cells at every step, some of them are able to form new tumors in other parts of the body. Metastatic cancer cells can also remain inactive at a distant site for many years before they begin to grow again, if at all.
Where in the body can metastatic adenocarcinoma spread to?
Cancer can spread to almost every part of the body. Some types of cancer tend to spread to certain parts of the body. For example:
- Breast cancer tends to spread to the bones, liver, lungs, chest wall, and brain
- Lung cancer tends to spread to the brain, bones, liver, and adrenal glands
- Prostate cancer tends to spread to the bones
- Kidney cancer tends to spread to the adrenal glands, bones, brain, liver and lungs
- Stomach cancer tends to spread to the liver, lungs and the peritoneum
- Colon and rectal cancers tend to spread to the liver and lungs
- Pancreas cancer tends to spread to the liver, lungs and the peritoneum
- Thyroid cancer tends to spread to the bones, liver and the lungs
- Endometrial cancer tends to spread to the bones, liver, lungs, peritoneum and the vagina
Less frequently, cancer can spread to the skin, muscle, or other organs in the body. Cancer cells can also spread to the lining around the lungs called the pleural cavity. It can also spread to the space around the belly called the peritoneal cavity. When these cancer cells cause fluid to build up in these areas, it is called malignant pleural effusion and malignant ascites.
What are symptoms of metastatic cancer?
Metastatic cancer does not always cause symptoms. When symptoms do occur, their nature and frequency will depend on the size and location of the metastatic tumors. Some common signs of metastatic cancer include:
- Pain and fractures, when cancer has spread to the bone
- Headache, seizures, or dizziness, when cancer has spread to the brain
- Shortness of breath, when cancer has spread to the lung
- Jaundice or swelling in the belly, when cancer has spread to the liver
How do doctors diagnose metastatic cancer?
If you already had cancer treatment for non-metastatic cancer, you probably have a follow-up care plan. You will see your doctor for regular checkups. Specific tests may be done to look for metastases.
Alternatively, some people already have metastases when they are first diagnosed with cancer. In this situation, the metastases are usually found during the initial tests to stage the cancer.
Cancer may cause symptoms such as pain or shortness of breath. Sometimes these symptoms will lead your doctor to do necessary tests to find the metastases.
How do doctors treat metastatic cancer?
Treatment depends on:
- The original cancer and where it started
- How much the cancer has spread and where it is located
- Your age and health
- Your personal treatment choices
Researchers are learning more about how metastases may differ from the original tumor at the molecular and genetic level. This is why treatment for metastasis is often different from the treatment used for the original tumor.
Treatment may include chemotherapy or hormone therapy. Surgery and radiation therapy may also be options for some types of cancer. Doctors might try one type of treatment and then switch to another when the first treatment no longer works. Or you might have a combination of treatments.
Types of metastatic cancer treatment
The main types of treatment for metastasis include:
- Treatment that affects your entire body. Doctors call this systemic therapy. It includes chemotherapy and other medications, such as targeted therapy, hormone therapy, and immunotherapy.
- Treatment for the area with cancer. Doctors call this local therapy. It includes surgery, radiation therapy, and some other treatments.
- When you choose a treatment, talk with doctors who have experience treating metastatic cancer. Doctors can have different opinions on the best treatment plan.
Does treatment cure metastatic cancer?
In some situations, metastatic cancer can be cured, but most commonly, treatment does not cure the cancer. But doctors can treat it to slow its growth and reduce symptoms. It is possible to live for many months or years with certain types of cancer, even after the development of metastatic disease.
How well any treatment works depends on:
- The type of cancer
- How far the cancer has spread and where it is located
- How much cancer there is
- If the cancer is growing quickly or slowly
- The specific treatment
- How the cancer responds to treatment
It is important to ask your doctor about the goals of treatment. These goals may change during your care, depending on whether the cancer responds to the treatment. It is also important to know that pain, nausea, and other side effects can be managed with the help of your health care team. This is called palliative care and should be a part of any treatment plan.
Research shows that palliative care can improve the quality of your life and help you feel more satisfied with the treatment you receive. Learn more about palliative care, or supportive care.
Goals of treatment
For many people with cancer, the goal of treatment is to try to cure the cancer. This means getting rid of the cancer and never having it come back. With metastatic cancer, curing the cancer may not be a realistic goal. However, it might still be a hope or dream. It is reasonable to ask your doctor if curing the cancer is the goal.
If curing the cancer is not the goal of treatment, the goal is to help a person live as well as possible for as long as possible. Getting more specific, this goal can be broken into 4 parts:
- To have the fewest possible side effects from the cancer
- To have the fewest possible side effects from the cancer treatment
- For the person with cancer to have the best quality of life
- For the person with cancer to live as long as possible with the cancer
Each person values these items differently. It is important to tell your health care team what is important to you.
Getting treatment for metastatic cancer can help you live longer and feel better. But getting treatment is always your decision.
Treatment in clinical trials
Clinical trials offer treatments that are not yet available to the public. A clinical trial might be the main treatment for metastases, or just one of the options. Only 3% to 5% of adults with cancer take part in clinical trials. The clinical trial treatment may or may not help. But even if it does not, it gives researchers information that could help future patients.
Living with metastatic cancer
Living with metastatic cancer is challenging. The challenges are different for everyone, but they can include:
- Feeling upset that the cancer came back. You might feel hopeless, angry, sad, or like no one understands what you are going through, even family.
- Worrying that treatment will not help and the cancer will get worse.
- Dealing with tests, doctor’s appointments, and decisions.
- Talking with family and friends about the cancer.
- Needing help with daily activities if you feel exhausted or have side effects from treatment.
- Finding emotional and spiritual support.
- Coping with the cost of more treatment. Even if you have insurance, it might not cover everything.
To understand your situation, you may want to get a second opinion. Many people find that it helps to get an opinion from another oncologist, and many doctors encourage it.
Your doctor can help you cope with cancer symptoms and treatment side effects. For example, if you have pain, your treatment might include surgery to remove a tumor in a painful area. Your doctor might also prescribe pain medication or anti-nausea medication.
Coping with emotions and lifestyle challenges is an important part of living with metastatic cancer. Ways of coping include:
- Learning about the metastasis. You might want to know everything possible, or just basic information.
- Talking with another health care professional such as a psychologist, psychiatrist, counselor, or oncology social worker about your situation.
- Managing stress. From planning ahead to trying meditation and yoga, there are many options to help lower your stress level.
- Finding meaning. Talking with a hospital chaplain, a counselor, or your religious leader can help.
Talking about fears and concerns is important, even when treatment is working well. Tell your health care team about emotional symptoms. People may live for years with metastatic cancer. Your doctor can help you have the best quality of life possible during this time. Hospitals and medical centers have many resources for you and your family.
Support for your caregivers
Your loved ones might also need help coping. Having a family member or friend with metastatic cancer is challenging, especially for people who help care for you. They can try the ways of coping above. Or your health care team can suggest other tips. For example, there are in-person and online support groups for family members of people with cancer.
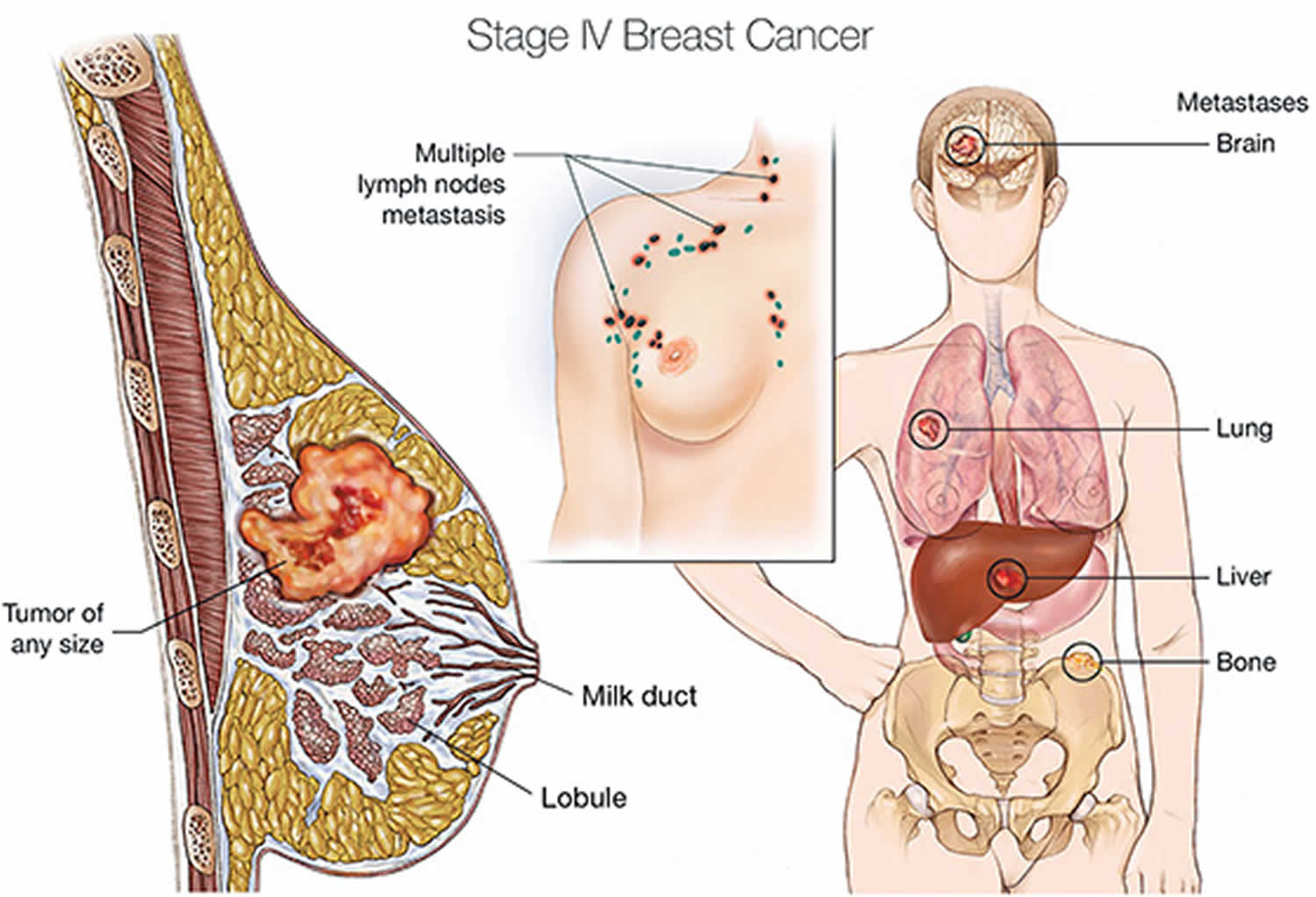
Metastatic breast cancer
Breast cancer starts in the ducts or lobules of the breast. Metastatic breast cancer means that breast cancer has spread to other parts of the body. It is also called stage IV (4) breast cancer. When breast cancer spreads, it most commonly spreads to the bones, lungs, liver, and brain.
Metastatic breast cancer can be a new cancer. Or it can be the return of a prior breast cancer. If you have breast cancer for the first time and it has already spread, it is called de novo metastatic breast cancer.
Even though the cancer may be in a different part of the body, it is still breast cancer. This is true even if your breasts were removed. This means that breast cancer treatments, not treatments for other cancers, will work best.
Figure 1. Metastatic breast cancer
Treatment options for metastatic breast cancer (cancer that has spread to distant parts of the body) may include the following:
Hormone therapy
In postmenopausal women who have just been diagnosed with metastatic breast cancer that is hormone receptor positive or if the hormone receptor status is not known, treatment may include:
- Tamoxifen therapy.
- Aromatase inhibitor therapy (anastrozole, letrozole, or exemestane). Sometimes cyclin-dependent kinase inhibitor therapy (palbociclib, ribociclib, abemaciclib, or alpelisib) is also given.
In premenopausal women who have just been diagnosed with metastatic breast cancer that is hormone receptor positive, treatment may include:
- Tamoxifen, an LHRH agonist, or both.
- Cyclin-dependent kinase inhibitor therapy (ribociclib).
In women whose tumors are hormone receptor positive or hormone receptor unknown, with spread to the bone or soft tissue only, and who have been treated with tamoxifen, treatment may include:
- Aromatase inhibitor therapy.
- Other hormone therapy such as megestrol acetate, estrogen or androgen therapy, or anti-estrogen therapy such as fulvestrant.
Targeted therapy
In women with metastatic breast cancer that is hormone receptor positive and has not responded to other treatments, options may include targeted therapy such as:
- Trastuzumab, lapatinib, pertuzumab, or mTOR inhibitors.
- Antibody-drug conjugate therapy with ado-trastuzumab emtansine.
- Cyclin-dependent kinase inhibitor therapy (palbociclib, ribociclib, or abemaciclib) which may be combined with hormone therapy.
In women with metastatic breast cancer that is HER2/neu positive, treatment may include:
- Targeted therapy such as trastuzumab, pertuzumab, ado-trastuzumab emtansine, or lapatinib.
In women with metastatic breast cancer that is HER2 negative, with mutations in the BRCA1 or BRCA2 genes, and who have been treated with chemotherapy, treatment may include:
- Targeted therapy with a PARP inhibitor (olaparib or talazoparib).
Chemotherapy
In women with metastatic breast cancer that is hormone receptor negative, has not responded to hormone therapy, has spread to other organs or has caused symptoms, treatment may include:
- Chemotherapy with one or more drugs.
Chemotherapy and immunotherapy
In women with metastatic breast cancer that is hormone receptor negative and HER2 negative, treatment may include:
- Chemotherapy and immunotherapy (atezolizumab).
Surgery
- Total mastectomy for women with open or painful breast lesions. Radiation therapy may be given after surgery.
- Surgery to remove cancer that has spread to the brain or spine. Radiation therapy may be given after surgery.
- Surgery to remove cancer that has spread to the lung.
- Surgery to repair or help support weak or broken bones. Radiation therapy may be given after surgery.
- Surgery to remove fluid that has collected around the lungs or heart.
Radiation therapy
- Radiation therapy to the bones, brain, spinal cord, breast, or chest wall to relieve symptoms and improve quality of life.
- Strontium-89 (a radionuclide) to relieve pain from cancer that has spread to bones throughout the body.
Other treatment options
Other treatment options for metastatic breast cancer include:
- Drug therapy with bisphosphonates or denosumab to reduce bone disease and pain when cancer has spread to the bone. (See the PDQ summary on Cancer Pain for more information about bisphosphonates.)
- A clinical trial of high-dose chemotherapy with stem cell transplant.
- A clinical trial of an antibody-drug conjugate (sacituzumab).
- Clinical trials testing new anticancer drugs, new drug combinations, and new ways of giving treatment.