Metatarsal stress fracture
Metatarsal stress fractures also known as march fractures, are a form of overuse injury, meaning they occur when the foot are pushed beyond their limits by repetitive activities or stress 1. The metatarsals are long bones in the feet which end at the base of the toes. Metatarsal stress fracture or march fractures most commonly involve the second and third metatarsal bones. The most common location of metatarsal stress fractures is the second metatarsal neck as it is less flexible and prone to torsional forces given its strong ligamentous attachment to the 1 and 2 cuneiforms. In addition, the second metatarsal is the longest of the metatarsals, subjected to the most force 2.
Metatarsal stress fractures are not limited to high-level athletes or military recruits. Metatarsal stress fracture is seen in runners of all levels, as well as ballet dancers and gymnasts and patients with rheumatoid arthritis (RA), metabolic bone disease, and neuropathic conditions 3. Metatarsal stress fractures are also seen with increasing frequency in patients who engage in aerobics activities, particularly high-impact aerobics 4.
The incidence of stress fractures in the general population is unknown, as virtually all literature on the subject is derived from a military population or advanced-level athletes. Stress fractures are estimated to constitute up to 16% of all injuries that are related to athletic participation; running is the cause in most of these cases. Most stress fractures (95%) involve the lower extremities, particularly the metatarsals.
A study by Waterman et al reported the incidence rate for lower extremity stress fractures in the US military (not adjusted for sex, race, age, rank, and service branch), including of the metatarsals, to be 5.69 per 1000 person-years, although tibial/fibular fractures were the most common. The highest fracture risk was found in service members under age 20 years or age 40 years or above, with the risk also higher in white service members than in black service members 5.
A combination of historical features and physical evaluation with imaging can help make the diagnosis. Metatarsal stress fractures are typically managed conservatively but can be complicated by nonunion. In such instances, surgical fixation may be warranted.
Metatarsal anatomy
The second and third metatarsals are relatively fixed in position within the foot; the first, fourth, and fifth metatarsals are relatively mobile. More stress is placed on the second and third metatarsals during ambulation; thus, these bones are at increased risk for stress fractures.
The fifth metatarsal, which is approximately 1.5 cm from the proximal pole of the bone, bears greater stress in those who oversupinate when they walk or run. The fifth metatarsal also has a diminished blood supply and, thus, a decreased ability to heal 6.
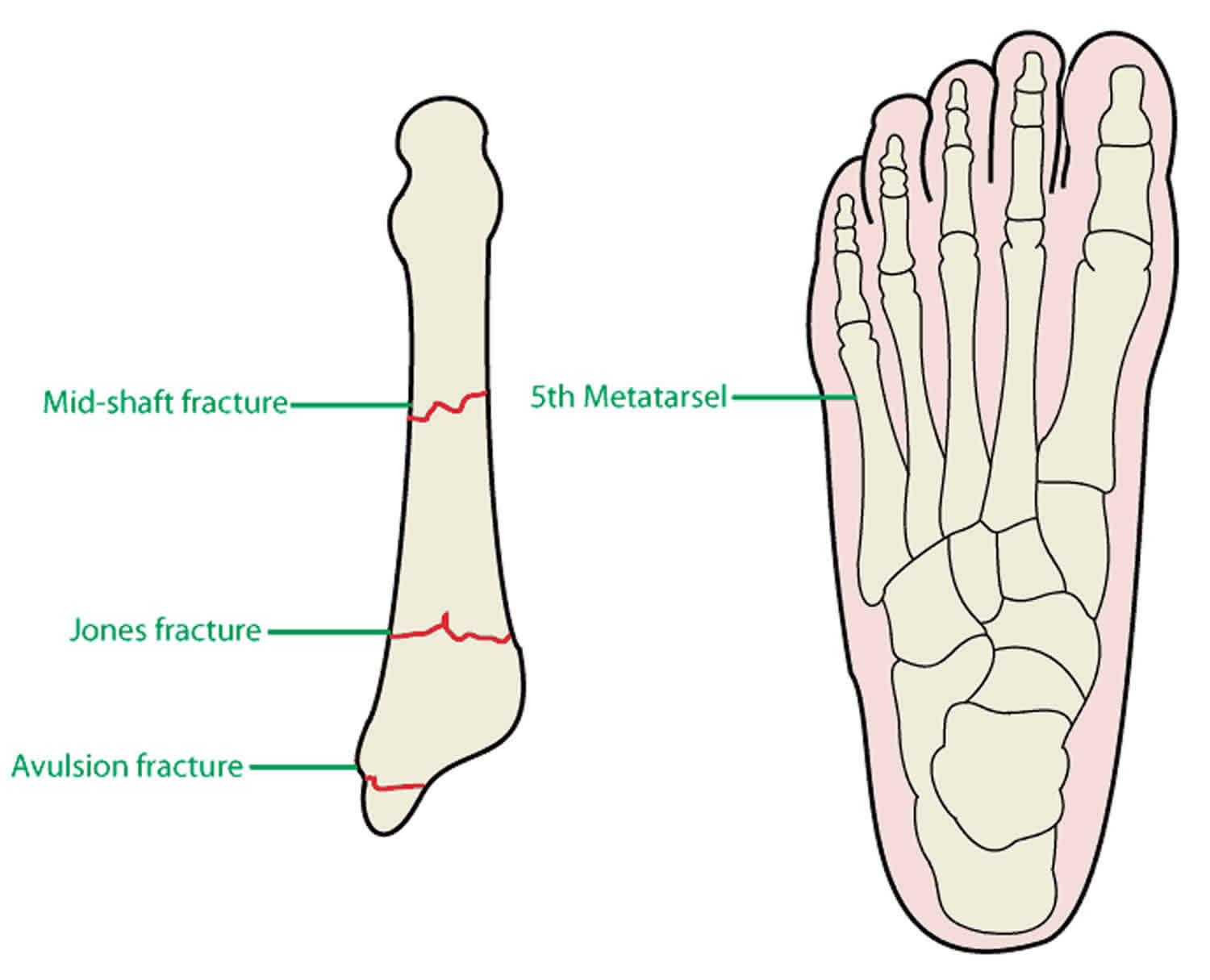
Stress fractures of the proximal fifth metatarsal must be distinguished from proximal avulsion fractures (“pseudo-Jones” fractures) and Jones fractures. The proximal avulsion fracture is usually associated with a lateral ankle strain and occurs at the insertion of the peroneus brevis tendon. The true Jones fracture is an acute fracture of the proximal diametaphyseal junction.
Metatarsal stress fracture causes
Metatarsal stress fracture or march fractures most commonly involve the second and third metatarsal bones are caused by an overuse injury. The repetitive impact to the metatarsals with weight-bearing exercises cause microfractures, which consolidate to stress fractures 7. Metatarsal stress fractures occur secondary to bone fatigue or bone insufficiency. Bone fatigue occurs when normal bone is unable to resist excessive mechanical demands. Bone insufficiency occurs when normal strain occurs on abnormal bone. Intrinsic risk factors as nutritional deficiencies as vitamin D or calcium increase the risk of these fractures. In addition, extrinsic risk factors as the training type or shoe type can also contribute to an increased risk of metatarsal stress fractures 8.
Metatarsal stress fractures occur commonly with sports and sudden increases in physical activity over 6 to 8 weeks. Metatarsal stress fractures are common in college athletes and the military, accounting for 25% of all stress fractures 7. Overall data suggest that females have a higher incidence of march fractures than men. In addition, those with prior stress fractures are more likely to develop another. Sixty percent of patients with a stress fracture will have had a previous one 9.
Metatarsal stress fracture causes include:
- Increased intensity, duration, or frequency of exercise
- New footwear
- Insufficient rest periods
- Continuing to train despite pain
- Osteopenia/osteoporosis
- Rheumatoid arthritis
- Neuropathic foot
- Female athletic triad
Fujitaka et al 10 studied a cohort of 273 collegiate male soccer players which included 16 who developed a fifth metatarsal stress fracture. Analysis of various history, physical, and equipment variables suggested that stress fracture may be a result of a weak toe-grip that leads to an increase in the load applied onto the lateral side of the foot.
Queen et al 11 investigated whether foot type (flat or normal) resulted in loading differences during four sport-specific tasks (cross-cut, side-cut, shuttle run, and landing from a simulated lay-up). Of 22 healthy individuals, 12 had normal feet and 10 had flat feet, and each completed 5 trials per condition. In-shoe pressure data were collected at 50 Hz, and analyses of the entire foot and 8 regions of the foot were carried out on contact area, maximum force, and the force time integral. The investigators’ findings included the following statistically significant findings 11:
Flat feet
- During the cross-cut task, there was an increase in medial midfoot contact area.
- During the side-cut task, an increase in contact area, force time integral, and maximum force in both the medial and lateral midfoot were demonstrated.
- During the shuttle run task, an increase in force time integral in the lateral midfoot and increases in maximum force in both the medial and lateral midfoot were present
- During the landing task, an increase in maximum force in the medial midfoot was present. However, flat feet showed a decrease in middle forefoot maximum force.
Queen et al 11 concluded that individuals with a normal foot may have a lower risk for medial and lateral midfoot injuries such as metatarsal stress fractures. Thus, foot type should be assessed when determining an individual’s risk for metatarsal stress fractures.
A case-control study that included 51 NFL players reported increased risk for fifth metatarsal fractures in players with long, narrow, and straight fifth metatarsals with an adducted forefoot 12.
Metatarsal stress fracture classification
Kaeding and Miller’s 5-Tier Grading System 13
Grade of Stress Fracture and Radiographic Finding
- Grade 1: Asymptomatic radiographic findings
- Grade 2: Pain with no fracture on imaging
- Grade 3: Nondisplaced fracture on imaging
- Grade 4: Displaced fracture on imaging
- Grade 5: Sclerotic nonunion on imaging
Metatarsal stress fracture prevention
Increases in sports-training demands, whether in intensity or duration, should be performed in a slow cyclical manner, and rest periods need to be built into training regimens. Use of orthotics has not been proven to decrease the incidence of metatarsal stress fractures.
Athletes who develop pain during exercise need to decrease their training level to one that is painless, and then they can slowly resume a training regimen.
Physicians, coaches, trainers, and parents need to be aware of metatarsal stress fractures and the symptoms. Prompt treatment can reduce morbidity and time lost from the offending sport or activity.
Metatarsal stress fracture symptoms
Patients usually report having increased the intensity or duration of their exercise regimen.
Initially, dull pain only occurs with exercise, then the condition progresses to pain at rest. Pain may improve transiently with rest but increases again with activity. Pain often is described as dull and aching. Pain starts diffusely, then localizes to the site of the fracture.
Stress fractures can be historically distinguished from a true Jones fracture, because patients with a stress mechanism as the etiology report a long history of prodromal symptoms of pain over the proximal fifth metatarsal.
Menstrual irregularities should be explored in female patients due to a high association between female athletics, amenorrhea, and osteoporosis — otherwise known as the female athletic triad 14.
Physical examination
Physical examination consists of palpation of the pain site, eliciting boney tenderness. If the fracture is in the proximity of a joint, the joint motion will aggravate the pain. Patients may have a limping gait with weight bearing.
- Inspect the affected foot for swelling, bruising, or warmth.
- Inspect both feet for a side-by-side comparison.
- Palpate the affected foot to find the point of maximal tenderness. Specifically seek to determine if the point of maximal tenderness is related to bony or soft-tissue problems.
- Inspect the patient’s athletic shoes for signs of excessive supination or excessive wear under the metatarsal heads.
Metatarsal stress fracture complications
Nonunion is a complication of march fractures with symptoms of chronic pain, swelling, or instability. In such cases, surgery with intramedullary nailing may be warranted. Post-operatively, healing can be arduous, sometimes taking months to years 2. Nonunion rates of 35-50% in fifth-metatarsal stress fractures are reported in the literature. For other metatarsal stress fractures, the nonunion rate is low.
Metatarsal stress fracture diagnosis
Metatarsal stress fractures or march fractures are diagnosed based on historical clues, physical examination, and confirmed with diagnostic imaging. Plain radiographs are the initial imaging modality of choice. However, plain radiographs have a high rate of false negative for metatarsal stress fractures early on and may not demonstrate fractures until 2 to 4 weeks after the onset of pain 15. While a clear fracture through the metatarsal may be seen on a radiograph, subtle periosteal reactions and blurring of the cortex may be the only clues of a stress fracture. More mature fractures may demonstrate callus formation or cortical lucency 8.
Occult, suspected fractures not visible on plain radiographs can be imaged using three-phase bone scans with technetium-99 or magnetic resonance imaging (MRI). Both advanced imaging modalities have been proven to be sensitive to these fractures up to 24 hours after onset of pain. While bone scans are considered sensitive, but not specific, MRI is both sensitive and specific for metatarsal stress fractures 8.
Lastly, thorough testing of the patient’s intrinsic risk factors may be needed. For example, measuring serum 25(OH), vitamin D concentration can be considered in those suspected of nutritional deficiencies 2.
Due to a known association between rheumatoid arthritis and stress fractures, the clinician may consider a workup for rheumatoid arthritis, with an erythrocyte sedimentation rate (ESR) and rheumatoid panel. This workup is not routine in most patients, but it is a consideration when the clinical picture is unclear or indicates the possibility of rheumatoid arthritis.
Metatarsal stress fracture treatment
In most cases, analgesia and rest are all that is needed for metatarsal stress fracture healing. Acetaminophen and ice are implemented for pain and swelling. The effect of nonsteroidal anti-inflammatory drugs (NSAIDs) on fracture healing remains contested 8.
Immobilization is often unnecessary, and a stiff-soled orthopedic boot or walking boot may be used for 4 to 8 weeks. Weight-bearing is allowed as long as the patient is pain-free. Thus, exercise may resume with lower impact exercises as swimming, cycling, or deep water running. The exception to this treatment is areas higher risk for nonunion, consisting of the base of the fifth metatarsal and neck of the second metatarsal. Special consideration should be given to pain elicited at these areas for advanced imaging if radiographs are negative. In addition, if a fracture at these sites is present, non-weight bearing status can be achieved with crutches and casting. Additionally, a referral to an orthopedic surgeon should be placed in cases of nonunion that may need surgical fixation 2.
Modifiable risk factors should be treated. Nutritional deficiencies as low levels of vitamin D, calcium, or calories should be addressed by ensuring adequate intake and supplementation as needed. Environmental changes should be considered. Shock-absorbing insoles for shoes or boots can distribute force during weight-bearing exercises. The type of training activity, surface, and intensity can be adjusted 2.
As a march fracture heals, a graded return to activity should be employed. When the patient is fully weight-bearing and pain-free with low-intensity exercise, the patient gradually increases their exercise intensity by 10% every week to avoid further stress fractures 2.
Prevention of march fractures includes stretching with gradual increments in exercise intensity and duration to avoid abrupt changes in stress. In addition, correcting predisposing biomechanical conditions as gait training and arch supports can be beneficial.
Rehabilitation
During the recovery phase, the patient may progress to weight bearing as tolerated, initially in a wooden-soled shoe, and then in a comfortable shoe.
Aqua-running, swimming, or bicycling may be continued to maintain physical fitness.
The patient may be allowed to gradually return to his or her sport with a slow build-up in intensity and duration, with regular rest intervals. No more than a 10% increase in intensity or duration should be allowed from week to week. Any pain recurrence should prompt a rest period, followed by resuming the activity at a lower level.
Return to play
After recovery from metatarsal stress fractures, patients may return to play when they can participate without pain.
The intensity and duration of activities need to be increased slowly, and the patient must adhere to regular rest periods.
Surgical intervention
Stress fractures of the second or third metatarsals rarely require surgical intervention. Most of these fractures heal uneventfully, and nonunion is rare. However, stress fractures of the fifth-metatarsal base are more problematic. Displacement of these fractures tends to increase with continued weight bearing. The treatment options are 2-fold as follows:
- Less-active patients should be non-weight bearing in a short-leg cast for 6-8 weeks or until there is radiographic evidence of healing. If an established nonunion develops, screw fixation and/or bone grafting may be required 16.
- For active patients, early intramedullary screw fixation, with or without bone grafting, is often recommended 17.
Other treatment options
Albisetti et al 18 reported their experience with diagnosing and treating stress fractures at the base of the second and third metatarsals in young ballet dancers from 2005-2007. Of 150 trainee ballet dancers, 19 had stress fractures of the metatarsal bone bases. All of the dancers were recommended to rest, but external shockwave therapy (ESWT) was also used in 18 and electromagnetic fields (EMF) and low-intensity ultrasonography was used in 1, with good results in each case 18.
Albisetti 18 advised the best approach to metatarsal stress fractures is early diagnosis with clinical examination and radiologic studies such as x-ray and MRI. The investigators also noted external shockwave therapy led to good results, with a relatively short time of rest from the patients’ activities and a return to dancing without pain. However, further study is warranted given the small study size and that all but one of the young dancers received external shockwave therapy.
Smith et al 19 identify the prevalence of vitamin D deficiency in patients with a low energy fracture of the foot or ankle. The study concluded that hypovitaminosis D was common among patients with a foot or ankle injury. Patients with a low energy fracture of the foot or ankle were at particular risk for low vitamin D, especially if they smoked, were obese, or had other medical risk factors. The authors 19 conclude that since supplementation with vitamin D (± calcium) has been shown to reduce the risk of fragility fractures and improve fracture healing, monitoring of 25-OH vitamin D and supplementation should be considered in patients with fractures.
Metatarsal stress fracture prognosis
Stress fractures in the first 4 metatarsals routinely heal without complication.
Stress fractures at the base of the fifth metatarsal have a nonunion rate of 35-50%.
References- Koo AY, Tolson DR. March (Metatarsal Stress) Fracture. [Updated 2019 May 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532289
- Pegrum J, Dixit V, Padhiar N, Nugent I. The pathophysiology, diagnosis, and management of foot stress fractures. Phys Sportsmed. 2014 Nov;42(4):87-99.
- Finestone A, Milgrom C, Wolf O, Petrov K, Evans R, Moran D. Epidemiology of metatarsal stress fractures versus tibial and femoral stress fractures during elite training. Foot Ankle Int. 2011 Jan. 32(1):16-20.
- Metatarsal stress fractures. https://emedicine.medscape.com/article/85746-overview
- Waterman BR, Gun B, Bader JO, Orr JD, Belmont PJ Jr. Epidemiology of Lower Extremity Stress Fractures in the United States Military. Mil Med. 2016 Oct. 181 (10):1308-13.
- Polzer H, Polzer S, Mutschler W, Prall WC. Acute fractures to the proximal fifth metatarsal bone: development of classification and treatment recommendations based on the current evidence. Injury. 2012 Oct. 43(10):1626-32.
- Sanderlin BW, Raspa RF. Common stress fractures. Am Fam Physician. 2003 Oct 15;68(8):1527-32.
- Jacobs JM, Cameron KL, Bojescul JA. Lower extremity stress fractures in the military. Clin Sports Med. 2014 Oct;33(4):591-613.
- Patel DS, Roth M, Kapil N. Stress fractures: diagnosis, treatment, and prevention. Am Fam Physician. 2011 Jan 01;83(1):39-46.
- Fujitaka K, Taniguchi A, Isomoto S, Kumai T, Otuki S, Okubo M, et al. Pathogenesis of Fifth Metatarsal Fractures in College Soccer Players. Orthop J Sports Med. 2015 Sep. 3 (9):2325967115603654.
- Queen RM, Mall NA, Nunley JA, Chuckpaiwong B. Differences in plantar loading between flat and normal feet during different athletic tasks. Gait Posture. 2009 Jun. 29(4):582-6.
- Karnovsky SC, Rosenbaum AJ, DeSandis B, Johnson C, Murphy CI, Warren RF, et al. Radiographic Analysis of National Football League Players’ Fifth Metatarsal Morphology Relationship to Proximal Fifth Metatarsal Fracture Risk. Foot Ankle Int. 2018 Nov 7. 1071100718809357.
- Miller TL, Jamieson M, Everson S, Siegel C. Expected Time to Return to Athletic Participation After Stress Fracture in Division I Collegiate Athletes. Sports Health. 2018 Jul/Aug;10(4):340-344.
- Brukner P, Bennell K. Stress fractures in female athletes. Diagnosis, management and rehabilitation. Sports Med. 1997 Dec. 24(6):419-29.
- Patel DR. Stress fractures: diagnosis and management in the primary care setting. Pediatr. Clin. North Am. 2010 Jun;57(3):819-27.
- Weinfeld SB, Haddad SL, Myerson MS. Metatarsal stress fractures. Clin Sports Med. 1997 Apr. 16(2):319-38.
- Tsukada S, Ikeda H, Seki Y, Shimaya M, Hoshino A, Niga S. Intramedullary screw fixation with bone autografting to treat proximal fifth metatarsal metaphyseal-diaphyseal fracture in athletes: a case series. Sports Med Arthrosc Rehabil Ther Technol. 2012 Jul 20. 4(1):25.
- Albisetti W, Perugia D, De Bartolomeo O, et al. Stress fractures of the base of the metatarsal bones in young trainee ballet dancers. Int Orthop. 2009 May 5. epub ahead of print.
- Smith JT, Halim K, Palms DA, Okike K, Bluman EM, Chiodo CP. Prevalence of vitamin D deficiency in patients with foot and ankle injuries. Foot Ankle Int. 2014 Jan. 35(1):8-13.