Navicular fracture also called tarsal navicular fracture, most commonly the result of either traumatic injury or undue stress, with the latter having a higher incidence in younger individuals and athletes 1. Even though midfoot fractures are relatively uncommon injuries, navicular stress fractures represent up to one-third of all stress fractures 2. Navicular fractures are at high risk of nonunion and osteonecrosis owing to the navicular bone’s tenuous blood supply as well as the inherent complexity of the joint 3. Navicular fractures often require surgical intervention, though they can be treated conservatively in some cases 1.
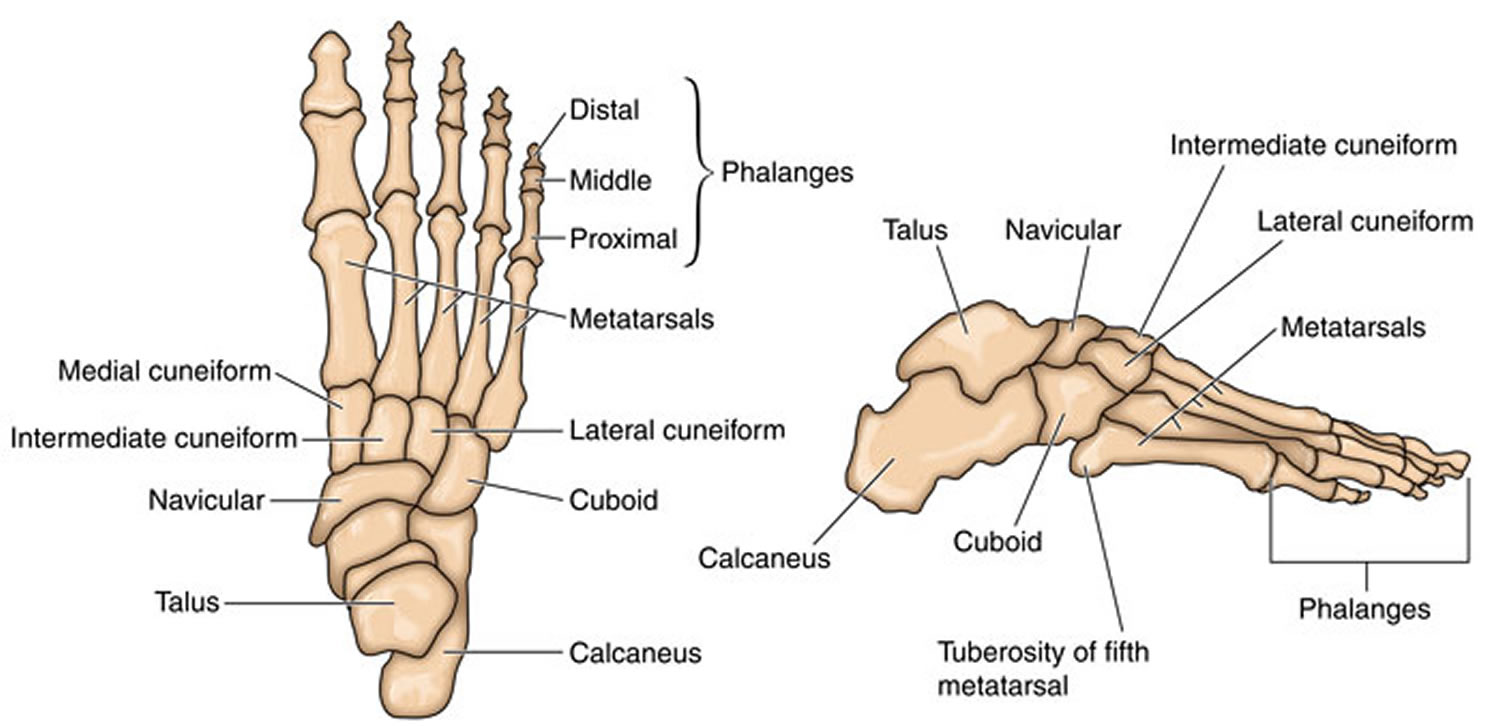
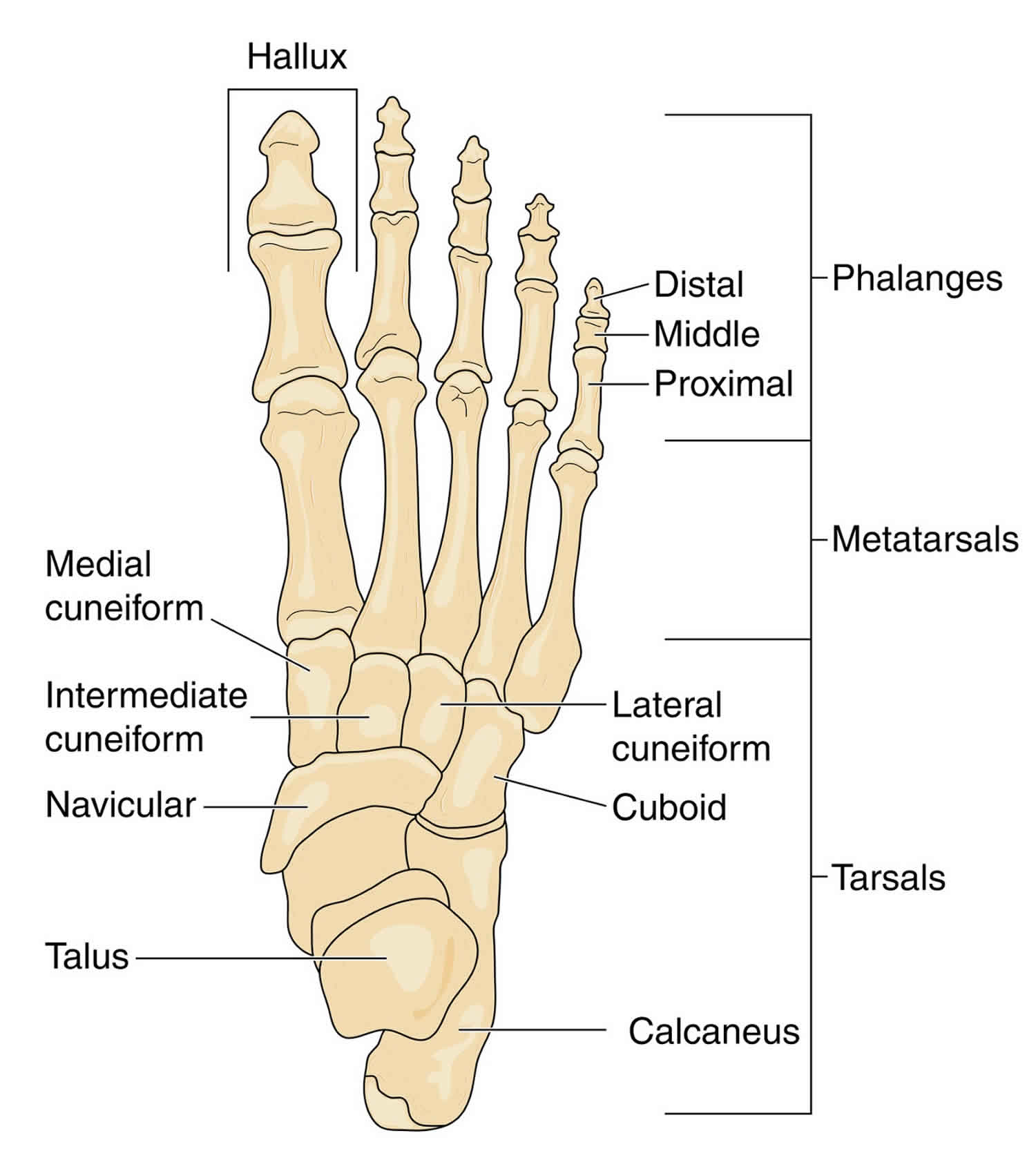
The navicular is a wedge-shaped bone articulating with the talus, calcaneus, the three cuneiform bones, and the cuboid 4. The bone’s major oblique axis lies dorsoplantar and lateromedial, with its base situated dorsolaterally, and its apex plantar medial 4. The navicular is part of 2 important structures that are essential for normal gait: (1) the medial longitudinal arch and (2) the transverse tarsal joint (also called the midtarsal or Chopart joint).
Posteriorly, the navicular has a biconcave surface which articulates with the head of the talus 4. Anteriorly, the navicular has plantar concavity, with there being three articular surfaces 4. The largest of these surfaces is found medially with a convex surface, articulating with the medial cuneiform 5. The navicular tuberosity, found medially, is the insertion site for the posterior tibial tendon. Considering the large number of articulations found on the various surfaces of the navicular, a large portion of the bone is covered in articular cartilage.
The medial longitudinal arch is composed of the navicular, calcaneus, talus, 3 cuneiforms, and 3 medial metatarsals. This arch provides support for normal gait, in particular from mid stance until push-off.
The transverse tarsal joint is essential for normal gait and is composed of the talonavicular joint and the calcaneocuboid joint. At heel strike, this joint is flexible and plays an important role in absorbing ground impact and accommodating the foot to the ground. At push-off, the transverse tarsal joint is locked and is helpful in forward propulsion.
The dorsal aspect of the navicular receives vascular supply by the medial tarsal branches of the dorsalis pedis artery, along with branches of the lateral tarsal artery 6. Supplying the medial plantar aspect of the navicular is a branch of the tibialis posterior artery 6. Some literature suggests a zone of avascularity from the central third to the distal cortex of the navicular, which may contribute to the avascular necrosis sometimes associated with these fractures 6.
Navicular bone is an essential component of the Chopart joint, which itself consists of the talonavicular and calcaneocuboid joints 7. Both of these joints are crucial for inversion and eversion of the foot.
Midfoot fractures only represent a small portion of all foot injuries, though stress fractures comprise approximately one-third of all stress fractures of the foot 8. Navicular stress fractures may account for up to 35% of stress fractures in athletes. Because navicular stress fractures are not easily observed on plain radiographs, the reported incidence rates vary widely. The overall incidence may appear to be increasing due to advances in imaging 9.
Among track-and-field athletes, up to 21% may experience a stress fracture in the course of a year 10. In these athletes, up to 15% of stress fractures are of the navicular 11. Other studies have demonstrated similar findings. [28, 29, 30, 31] The highest incidence of stress fractures is in jumping and sprinting events.
Among military recruits, the incidence is approaching that of athletes, as the training of military recruits closely mirrors the training of athletes 12.
In the case of traumatic navicular injuries, the vast majority result from motor vehicle accidents, followed by falls and blunt injuries 13. Stress fractures are most common in young individuals with high functional demand such as competitive athletes 8.
There are 4 types of navicular fractures 14:
- Navicular avulsion fracture,
- Navicular tuberosity fracture,
- Navicular body fracture
- Navicular stress fracture.
Avulsion fracture, the most common fracture of the navicular, is often associated with ligamentous injuries and results from twisting forces on the mid foot. These fractures are commonly treated conservatively, except for avulsion of the posterior tibial tendon insertion (tuberosity fracture), which may be repaired operatively, especially if a proximal dislocation of 1 cm or more is present. An avulsion of the posterior tibial tendon insertion must be differentiated from an accessory navicular.
Fractures of the navicular body are commonly associated with other injuries of the midtarsal joint. Sangeorzan et al 15 in 1989 categorized navicular body fractures into 3 types. The Sangeorzen classification system classifies tarsal navicular body fractures according to the direction of the fracture line, degree of disruption of surrounding joints, and the direction of foot displacement 16.
- Type 1 is a coronal fracture with no dislocation or no angulation of the forefoot.
- Type 2 is a dorsolateral to plantar-medial fracture fracture with medial displacement of the major fragment and forefoot.
- Type 3 is a comminuted fracture in the sagittal plane of the bone with lateral forefoot displacement and carries the worst prognosis.
All navicular body fractures with 1 mm or more of displacement require open reduction and internal fixation.
Navicular stress fractures are usually sports-related injuries.
In 1855, Brehaulpt first described stress fractures in military recruits who were subjected to long marches. As more civilians took up physically demanding sports, the incidence of stress fractures has increased in the general population. Towne et al first described stress fracture of the tarsal navicular in 1970 17.
In athletes, navicular stress fractures are of particular concern because they are underdiagnosed and can lead to significant disability if the diagnosis is delayed 18. In a study by Torg et al 19 in 1982, the average time between the fracture and diagnosis was estimated to be 7 months. Given the significant improvement in outcome with early diagnosis and proper treatment, navicular stress fractures should be considered in any athlete with midfoot pain. In a 2006 study by Saxena and Fullem 20, navicular stress fractures took up to 4 months to heal posttreatment.
Fracture-dislocation of the navicular may occur in athletes 21. This uncommon injury generally requires reduction and examination for stability via fluoroscopy, with the patient under general anesthesia. If the postreduction examination findings confirm stability of the navicular, treatment with a non–weight-bearing cast may be sufficient; otherwise, internal fixation is required.
While the biomechanics behind stress fractures of the tarsal navicular are somewhat poorly understood, those of traumatic injuries are more comprehensively elucidated. It is known, however, that stress fractures are a chronic overuse injury associated with microfractures of the bone 8. Traumatic injuries can cause a variety of navicular fracture patterns, including avulsion fractures, tuberosity fractures, and body fractures.
Avulsion fractures of the navicular may occur dorsally, medially, or in a plantar direction, depending on the force applied to the midfoot. In the case of foot dorsal avulsion, fractures result from extreme plantar flexion causing undue stress on the deltoid and dorsal capsules 3. Excessive pull from the posterior tibialis tendon can result in medial and tuberosity fractures, and plantar avulsion fractures are secondary to ligamentous injury 3.
Navicular body fractures can be caused either by a direct or an indirect force. There are several other theories on the forces causing navicular body fractures, though all are due to axial forces on a foot in plantar flexion 8.
Some risk factors for navicular stress fracture include the following:
- Female sex
- Menstrual irregularities 22
- Unequal leg length
- Any medical condition or behavior that may result in relative osteopenia, including smoking, hypothyroidism, steroid use, and rheumatoid arthritis
- Sudden, significant weight loss
Some factors that have been implicated as causes of navicular stress fractures include the following:
- Starting athletic activity at a high level without a gradual increase in activity over time
- Starting a second sport and assuming that the body is conditioned to participate at that sport immediately and at a high level. The navicular is at particular risk when runners participate in sports that require jumping and do not take the time for proper conditioning in their new sport.
- Ill-fitting and/or old, worn equipment
- Change in running or field surfaces
- Relative osteopenia
- Biomechanical abnormality.
There is some evidence that Calcium and Vitamin D supplements decrease the incidence of stress fractures, particularly in females. Smoking, low physical activity and poor nutritional status are also known risk factors for stress fractures.
Patients of navicular avulsion fractures typically present with a significant degree of pain in the midfoot area, particularly during push-off of the fractured segment. Patients who have endured a navicular body fracture are typically unable to bear any weight on the affected extremity and present with a profound degree of swelling on the dorsal and medial aspects of the foot, all of which is due to the mechanism of the injury and disruption of the medial column of the foot 23. Owing to the risk of compartment syndrome, a thorough neurovascular assessment should take place, with an evaluation of any open wounds. Additionally, navicular body injuries are often associated with additional injuries on the ipsilateral foot, with a recent study showing fifteen patients out of twenty-four having further injuries 24.
On the other hand, patients who have endured a navicular stress fracture typically have a milder clinical presentation, with an extended history of vague midfoot discomfort. Examination of these patients typically reveals a well-localized source of their pain over the dorsal aspect of the midsection of the navicular 23.
Navicular stress fractures must be considered in any athlete with midfoot pain. Typically, the pain is of insidious onset and may have been present for months. In addition, the pain often worsens with activity and improves with rest. Pain may be present at the dorsum of the foot, or it may radiate along the medial longitudinal arch. Slight swelling may or may not be present.
Historically, persons participating in the following sports and activities have a relatively high risk of navicular fracture:
- Track and field – Particularly sports involving jumping and sprinting 11
- Ballet and other dancing activities 25
- Equestrian sports
- Basketball
- Soccer 26
- American football
- Australian-rules football
- Rugby
- Gymnastics 27
- Military training 28
Physical examination
Possible findings from the physical examination in an individual who has a navicular fracture include the following:
- Tenderness at the “N spot,” which is defined as the proximal dorsal portion of the navicular (see the image below). This is the most important physical finding.
- Tenderness at the midmedial arch over the navicular
- Pain with passive eversion
- Pain with active inversion
- Pain that is often reproduced if the patient hops while in the equinus position
- Possible mild dorsal midfoot swelling
Figure 1. Navicular fracture N spot
As with most periarticular regions, there are several potential complications and risks associated with fractures of the navicular. These complications include osteonecrosis, malunion, nonunion, persistent stiffness, and pain. Patients suffering a nonunion may have deformity which can be mitigated through the use of an orthosis or surgical revision, depending on the severity of the deformity. Osteonecrosis, however, can result in profound deformity and is typically treated with the primary goal of restoring length and alignment, which is often through the fusion of the talonavicular or naviculocuneiform joints 3.
In a patient with a suspected tarsal navicular fracture, the initial radiographic evaluation is the three-view radiograph of the foot; this includes a non-weight bearing anteroposterior, lateral, and oblique X-ray. However, patients with suspected ligamentous injury or minor injuries may require a weight-bearing radiograph. An external oblique radiograph of the foot is useful in the evaluation of a suspected tuberosity fracture 23. In evaluating radiographs, the clinician should be aware of the potential for the appearance of an accessory navicular, which is identifiable with a radiograph of the contralateral foot.
The use of computed tomography (CT) can be helpful in high-energy injuries, as it can more precisely delineate complex fracture patterns, the geometry of the talonavicular joint, and can assist in preoperative planning. Additionally, CT can be used to create three-dimensional reconstructions of the navicular.
Tarsal navicular fractures can be managed either nonsurgically or surgically, depending on the individual fracture characteristics, such as the size, the degree of displacement, the location, comminution, as well as the condition and integrity of the soft tissues of foot, the presence of additional injuries on the ipsilateral foot, comorbidities and overall functional status 23.
In the case of navicular stress fractures, immobilization, and protected weight bearing for a period of six to eight weeks are indicated. However, patients with high functional demand, such as athletes may opt for surgical intervention instead 8. In the event of surgical intervention, these fractures may undergo repair with open reduction and internal fixation 8.
The management of traumatic navicular fractures can also be surgical or nonsurgical. Small avulsion fractures, tuberosity fractures, and nondisplaced body fractures can be managed nonoperatively, with the use of a weight-bearing short leg cast and ultimately a walking boot 23.
Displaced navicular body fractures typically require operative intervention, with the use of open reduction and internal fixation. The goals of operative intervention are anatomic fracture reduction, restoration of the length of the medial column, and creation of a rigid osseous construct which would allow for early range of motion 23.
Rehabilitation program
After the affected foot has been placed in a non–weight-bearing cast for 6 weeks, the cast is removed and tenderness at the N spot is assessed. If tenderness persists, then an additional 2 weeks of non–weight-bearing cast immobilization is recommended. However, if tenderness is not present at the N spot, then weight-bearing activity may begin. This activity is limited to a gradual return to normal activity under the care of a sports physician or physical therapist. The therapy may include muscle strengthening, range-of-motion exercises, and soft-tissue massage.
A stepwise regimen for the course of activity is as follows:
- The patient participates in his or her normal activities of daily life (ADLs), which may include swimming, for 2 weeks (Weeks 1 and 2).
- If the athlete remains free of pain after 2 weeks, a gradual return to jogging may be prescribed.
- After 2 weeks of a gradually progressive jogging regimen (Weeks 3 and 4), the patient is again assessed for pain.
- If the patient remains free from pain after 2 weeks after gradually progressing in the jogging regimen, then the athlete may gradually return to full activity over the final 2 weeks of the rehabilitation program (Weeks 5 and 6).
Therapeutic Ultrasound may have a role in determining return to play decisions as pain with therapeutic ultrasound has corelated with MRI finding in navicular stress injuries 29.
Medical issues and complications
Delayed union and nonunion produce persistent pain at the navicular 30. Plain radiographs and/or a CT scan may show the persistent fracture. In such cases, referral to a surgeon is required for open reduction and fixation. In addition, fracture of the tarsal navicular may be complicated by avascular necrosis.
Surgical treatment
Most physicians do not recommend immediate open surgical procedures when treating uncomplicated navicular stress fractures. In a comparison study by Potter et al 31, surgery had similar long-term return-to-activity rates relative to conservative therapy. In another study, bone healing took up to 4 months, for both operative and nonoperative treatment 20.
Fractures that are complicated by dislocation are assessed for stability following reduction. If the navicular is stable, then treatment may continue as outlined for uncomplicated navicular fractures. If the navicular is unstable, then internal fixation is required.
A complete fracture with wide separation may benefit from early surgical intervention. In addition, if the patient is not expected to tolerate the rehabilitation program, surgical correction may be considered.
Return to sport, particularly in elite athletes, may be quicker with surgical vs non-surgical treatment 32.
A retrospective analysis by Coulibaly et al that compared operative and non-operative treatment of navicular fractures reported that the operative treatment group had considerably more complications of secondary osteoarthritis 33.
Other treatment
Although no trials support the use of bone growth stimulators for navicular stress fractures, they may be a helpful adjunct 34. In particular, bone growth stimulators that use pulsed electromagnetic fields (PEMFs) have been shown to have similar success rates when compared with open repair in tibial fracture nonunions 35. Whether these results are applicable to acute fractures and fractures of the navicular remains to be determined.
Platelet-rich plasma may help bone healing. Whole blood taken from the patient is processed to be used at the injury site. Although evidence suggests that platelet-rich plasma is safe and can promote bone formation, no clear evidence of benefit in fracture healing has been reported 36. No controlled trials of platelet-rich plasma use in healing of navicular fractures are underway 37.
Patients who have suffered a navicular stress fracture typically have a favorable prognosis if treated promptly and appropriately. A recent study demonstrated that 57 out of their 62-patient cohort had been able to return to activity at their preinjury level, implying an optimal clinical outcome 38. In another case study of 10 patients who had suffered comminuted tarsal navicular fractures, the union was achievable in all surgically treated patients, with none requiring an arthrodesis at a mean follow up of 20 months 39.
References- Gheewala R, Arain A, Rosenbaum AJ. Tarsal Navicular Fractures. [Updated 2019 Jun 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542221
- Khan KM, Brukner PD, Kearney C, Fuller PJ, Bradshaw CJ, Kiss ZS. Tarsal navicular stress fracture in athletes. Sports Med. 1994 Jan;17(1):65-76.
- Ramadorai MU, Beuchel MW, Sangeorzan BJ. Fractures and Dislocations of the Tarsal Navicular. J Am Acad Orthop Surg. 2016 Jun;24(6):379-89.
- Golano P, Fariñas O, Sáenz I. The anatomy of the navicular and periarticular structures. Foot Ankle Clin. 2004 Mar;9(1):1-23.
- Gross CE, Nunley JA. Navicular Stress Fractures. Foot Ankle Int. 2015 Sep;36(9):1117-22.
- McKeon KE, McCormick JJ, Johnson JE, Klein SE. Intraosseous and extraosseous arterial anatomy of the adult navicular. Foot Ankle Int. 2012 Oct;33(10):857-61.
- Benirschke SK, Meinberg EG, Anderson SA, Jones CB, Cole PA. Fractures and dislocations of the midfoot: Lisfranc and Chopart injuries. Instr Course Lect. 2013;62:79-91.
- Shakked RJ, Walters EE, O’Malley MJ. Tarsal navicular stress fractures. Curr Rev Musculoskelet Med. 2017 Mar;10(1):122-130.
- Wall J, Feller JF. Imaging of stress fractures in runners. Clin Sports Med. 2006 Oct. 25(4):781-802.
- Bennell KL, Malcolm SA, Thomas SA, et al. Risk factors for stress fractures in track and field athletes. A twelve-month prospective study. Am J Sports Med. 1996 Nov-Dec. 24(6):810-8.
- Bennell KL, Malcolm SA, Thomas SA, Wark JD, Brukner PD. The incidence and distribution of stress fractures in competitive track and field athletes. A twelve-month prospective study. Am J Sports Med. 1996 Mar-Apr. 24(2):211-7.
- Rome K, Handoll HH, Ashford R. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 2005. 2:CD000450.
- Richter M, Wippermann B, Krettek C, Schratt HE, Hufner T, Therman H. Fractures and fracture dislocations of the midfoot: occurrence, causes and long-term results. Foot Ankle Int. 2001 May;22(5):392-8.
- Thordarson DB. Fractures of the midfoot and forefoot. Myerson MS, Leonard ME, eds. Foot and Ankle Disorders. 2nd ed. Orlando, Fla: Harcourt; 2000. 1265-85.
- Sangeorzan BJ, Benirschke SK, Mosca V, Mayo KA, Hansen ST Jr. Displaced intra-articular fractures of the tarsal navicular. J Bone Joint Surg Am. 1989 Dec. 71(10):1504-10.
- Sangeorzan BJ, Benirschke SK, Mosca V, Mayo KA, Hansen ST. Displaced intra-articular fractures of the tarsal navicular. J Bone Joint Surg Am. 1989 Dec;71(10):1504-10.
- Towne LC, Blazina ME, Cozen LN. Fatigue fracture of the tarsal navicular. J Bone Joint Surg Am. 1970 Mar. 52(2):376-8.
- Simons SM. Foot injuries of the recreational athlete. Phys Sportsmed. 1999 Jan. 27(1):57-70.
- Torg JS, Pavlov H, Cooley LH, Bryant MH, Arnoczky SP, Bergfeld J, et al. Stress fractures of the tarsal navicular. A retrospective review of twenty-one cases. J Bone Joint Surg Am. 1982 Jun. 64(5):700-12.
- Saxena A, Fullem B. Navicular stress fractures: a prospective study on athletes. Foot Ankle Int. 2006 Nov. 27(11):917-21.
- Samoladas E, Fotiades H, Christoforides J, Pournaras J. Talonavicular dislocation and nondisplaced fracture of the navicular. Arch Orthop Trauma Surg. 2005 Feb. 125(1):59-61.
- Bennell KL, Malcolm SA, Wark JD, Brukner PD. Skeletal effects of menstrual disturbances in athletes. Scand J Med Sci Sports. 1997 Oct. 7(5):261-73.
- Rosenbaum AJ, Uhl RL, DiPreta JA. Acute fractures of the tarsal navicular. Orthopedics. 2014 Aug;37(8):541-6.
- Evans J, Beingessner DM, Agel J, Benirschke SK. Minifragment plate fixation of high-energy navicular body fractures. Foot Ankle Int. 2011 May;32(5):S485-92.
- Macintyre J, Joy E. Foot and ankle injuries in dance. Clin Sports Med. 2000 Apr. 19(2):351-68.
- Knapp T, Mandelbaum B, Garrett W Jr. Why are stress injuries so common in the soccer player?. Clin Sports Med. 1998 Oct. 17(4):835-53.
- Zetaruk MN. The young gymnast. Clin Sports Med. 2000 Oct. 19(4):757-80.
- Armstrong DW 3rd, Rue JP, Wilckens JH, Frassica FJ. Stress fracture injury in young military men and women. Bone. 2004 Sep. 35(3):806-16.
- Malliaropoulos N, Alaseirlis D, Konstantinidis G, Papalada A, Tsifountoudis I, Petras K, et al. Therapeutic Ultrasound in Navicular Stress Injuries in Elite Track and Field Athletes. Clin J Sport Med. 2017 May. 27 (3):278-282.
- Mann JA, Pedowitz DI. Evaluation and treatment of navicular stress fractures, including nonunions, revision surgery, and persistent pain after treatment. Foot Ankle Clin. 2009 Jun. 14(2):187-204.
- Potter NJ, Brukner PD, Makdissi M, et al. Navicular stress fractures: outcomes of surgical and conservative management. Br J Sports Med. 2006 Aug. 40(8):692-5; discussion 695.
- Shakked RJ, Walters EE, O’Malley MJ. Tarsal navicular stress fractures. Curr Rev Musculoskelet Med. 2017 Jan 21.
- Coulibaly MO, Jones CB, Sietsema DL, Schildhauer TA. Results and complications of operative and non-operative navicular fracture treatment. Injury. 2015 Aug. 46 (8):1669-77.
- Cohen M, Roman A, Lovins JE. Totally implanted direct current stimulator as treatment for a nonunion in the foot. J Foot Ankle Surg. 1993 Jul-Aug. 32(4):375-81.
- Raasch WG, Hergan DJ. Treatment of stress fractures: the fundamentals. Clin Sports Med. 2006 Jan. 25(1):29-36, vii.
- Guzel Y, Karalezli N, Bilge O, Kacira BK, Esen H, Karadag H, et al. The biomechanical and histological effects of platelet-rich plasma on fracture healing. Knee Surg Sports Traumatol Arthrosc. 2013 Oct 30.
- Vannini F, Di Matteo B, Filardo G, Kon E, Marcacci M, Giannini S. Platelet-rich plasma for foot and ankle pathologies: a systematic review. Foot Ankle Surg. 2014 Mar. 20(1):2-9.
- Saxena A, Behan SA, Valerio DL, Frosch DL. Navicular Stress Fracture Outcomes in Athletes: Analysis of 62 Injuries. J Foot Ankle Surg. 2017 Sep – Oct;56(5):943-948.
- Cronier P, Frin JM, Steiger V, Bigorre N, Talha A. Internal fixation of complex fractures of the tarsal navicular with locking plates. A report of 10 cases. Orthop Traumatol Surg Res. 2013 Jun;99(4 Suppl):S241-9.