Milia en plaque
Milia en plaque is a rare variant of primary milia, characterized by numerous aggregated milia appearing on within an inflamed plaque up to several centimeters in diameter 1. Milia en plaque usually found on an eyelid, behind the ear, on a cheek or jaw. Milia en plaque has also been described as periorbital, on the nasal bridge, and truncal 1. Milia are small, benign superficial keratin-filled cysts that result from the obstruction of a hair follicle or eccrine sweat ducts, measuring 1 to 4 mm in diameter 2. Milia can be primary, appearing spontaneously, or secondary to trauma, skin disease, or medication 3. Milia en plaque affects children and adults, especially middle-aged women and 2 congenital cases 4, 5. Milia en plaque is sometimes associated with another skin disease including pseudoxanthoma elasticum, discoid lupus erythematosus 6, lichen planus, drugs such as cyclosporine, trauma and renal transplantation 1.
Milia en plaque was first described by Balzer and Fouquet in 1903 and denominated by Hubler et al. in 1978 1. Since then, less than 40 cases have been reported in literature till date 7. Earlier reports described milia en plaque as a retroauricular dermatosis; however, later more case reports emerged with different sites of involvement like peri-orbital 8, pre-auricular 9, earlobes 10, sub-mandibular area 11 and supraclavicular area 12.
Milia en plaque is classified as primary milia deriving from the infundibulum of the vellus hair follicle and usually develops spontaneously in healthy skin with no clear cause 13. Milia are classified as primary when their onset is spontaneous and secondary when they appear following trauma (such as burn, dermabrasion, ablative laser etc.), inflammatory skin diseases (particularly those involving the basement membrane zone, such as sub-epidermal bullous diseases), or the use of topical medication (topical corticosteroids, 5-fluorouracil) or systemic drugs (cyclosporine and benoxaprofen) 14. Primary milia en plaque is a rare clinical variant characterized by numerous tiny milia within an erythematous base that arise spontaneously on a healthy skin in a predisposed individual without any apparent causative factor 1. Evidences show that primary milia originate in the hair follicle infundibulum, whereas the secondary forms may develop in various adnexal structures like sweat ducts, sebaceous glands, and hair follicle 1.
Despite being an asymptomatic benign lesion, milia en plaque can be a major cosmetic concern to the patient.
Dermoscopy is helpful in diagnosing early, inconspicuous milia (Figure 3). Histologically, milia en plaque is characterized by keratin-filled epidermal cysts and a mononuclear cell infiltrate 15.
There is no standard treatment for milia en plaque, but there are reports of milia en plaque being successfully treated by various medical as well as surgical treatments. Medical treatments of milia en plaque include topical tretinoin 1, oral isotretinoin 16, etretinate 7, minocycline 10, photodynamic therapies 1, producing variable response. Surgical modalities like simple extraction 17, electrodessication 18, dermabrasion 19 and CO2 laser evaporation 20 had been tried with variable success. Spontaneous regression has also been reported 21.
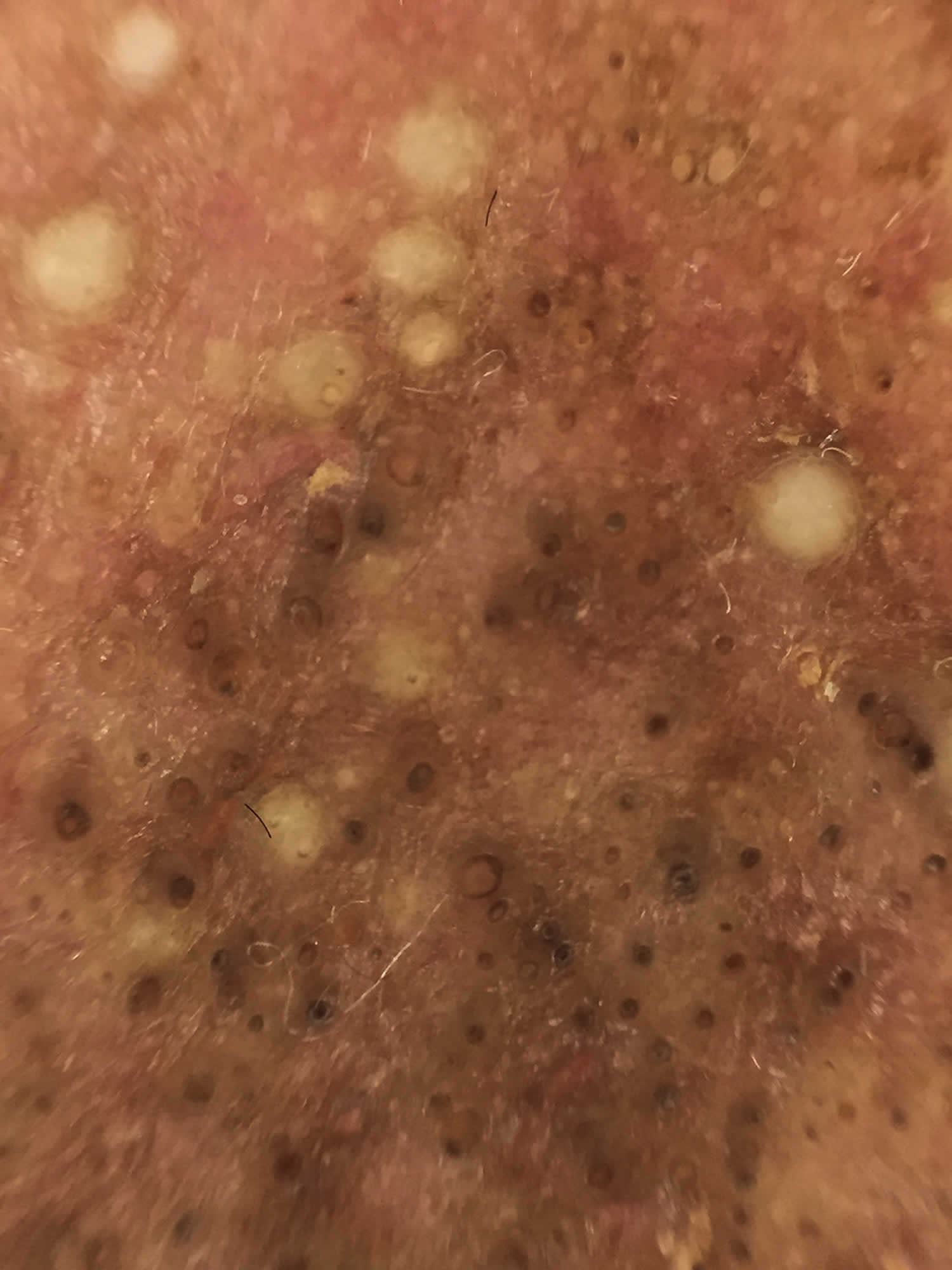
Figure 1. Milia en plaque (milia en plaque lupus)
Footnote: Multiple yellowish cysts on an erythematous plaque and scattered open comedones in a malar distribution.
[Source 22 ]Figure 2. Milia en plaque
Figure 3. Milia en plaque dermoscopy
Footnote: Dermoscopy found multiple milia cysts, follicular keratotic plugs, perifollicular whitish halos, pigmentation, and telangiectasia.
[Source 22 ]Milia en plaque causes
Milia en plaque mostly arises in healthy individuals and most cases are idiopathic (unknown), though it has been found to be associated with pseudoxanthoma elasticum 23, discoid lupus erythematosus 24, mycosis fungoides 25, lichen planus, systemic amyloidosis, trauma, and renal transplantation 26, 27, 28. Certain medications, specifically cyclosporine, may be involved in the development of milia en plaque 27. Additionally, a case of milia en plaque co-existing with cutis laxa was described in a patient who was taking penicillamine for more than 50 years 29.
The pathogenesis of milia en plaque remains elusive. Boehm and colleagues 30 proposed that damage to adnexal structures from underlying diseases results in the formation of milia. Milia en plaque after cryotherapy has been described, supporting the theory of trauma-induced milia 31. Kouba and colleagues 32 suggest that alteration in the infundibulum of a hair follicle, which causes impaired keratinization and outlet obstruction, plays a role in de novo milia en plaque. Ghosh and Sangal 5 postulate that intrauterine alteration in the infundibular portion and subsequent migration of the dysfunctional tissue contributes to the Blaschkoid pattern seen in congenital milia en plaque. Based on histopathological features, Terui and colleagues 33 suggest that milia en plaque may represent a hamartoma, similar to a tumor of follicular infundibulum and trichoadenoma.
Milia en plaque signs and symptoms
Milia en plaque is an uncommon benign skin condition that presents as multiple, tiny, white papules situated within an erythematous plaque. Milia en plaque is typically asymptomatic. Milia en plaque preferentially involves the head and neck area, including nose, forehead, cheeks, scalp, periauricular, periorbital, submandibular and supraclavicular regions (Figures 1 and 2) 34.
Lesions can be unilateral or bilateral 35. A linear milia en plaque following Blaschko lines has also been described 36.
Though most cases of milia en plaque have been described in adults, there were three case reports describing milia en plaque in children aged 6 years, 10 years, and 14 years 17, 18.
Milia en plaque diagnosis
Milia en plaque have a characteristic appearance. However, on occasion, a skin biopsy may be performed. Histopathologically, milia en plaque is characterized by keratin-filled epidermal cysts surrounded by a mononuclear cell infiltrate.
Milia en plaque should be distinguished from other types of cyst, comedones, xanthelasma and syringomas. Colloid milia are golden coloured bumps on cheeks and temples associated with excessive exposure to sunlight.
Milia en plaque should also be distinguished from milia-like cysts noted on dermoscopy in seborrhoeic keratoses, papillomatous moles and some basal cell carcinomas.
Milia en plaque treatment
Although milia en plaque is a benign condition, treatment is warranted if it causes a significant cosmetic disfigurement. Standard treatment for milia en plaque has not been established, but the condition can be treated with either medical or surgical modalities, including topical or oral retinoids, minocycline, photodynamic therapy, simple extraction, cryotherapy, ablative laser therapy, dermabrasion, electrodesiccation, or excision, with variable successes depending on the depth of the lesions 37, 38. Simple extraction and topical tretinoin are generally effective for superficial lesions. It should be noted, however, that recurrence is not uncommon 39. Rarely, spontaneous resolution may occur 21.
References- Stefanidou MP, Panayotides JG, Tosca AD. Milia en plaque: a case report and review of the literature. Dermatol Surg. 2002 Mar;28(3):291-5. doi: 10.1046/j.1524-4725.2002.01200.x
- Ghosh S, Sangal S. Congenital milia en plaque on scalp. Indian J Dermatol. 2015;60(1):105. doi:10.4103/0019-5154.147871 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4318039
- Berk D.R., Bayliss S.J. Milia: A review and classification. J Am Acad Dermatol [Internet]. 2008; 59: 1050-1063.
- Wang AR, Bercovitch L. Congenital milia en plaque. Pediatr Dermatol. 2016;33(4):e258-e259.
- Ghosh S, Sangal S. Congenital milia en plaque on scalp. Indian J Dermatol. 2015;60(1):105.
- Belhadjali H., Youssef M., Yahia S., Njim L., Zakhama A., Zili J. Milia en plaque and discoid lupus erythematosus. Clin Exp Dermatol. 2009; 34: 356-357.
- Ishiura N, Komine M, Kadono T, Kikuchi K, Tamaki K. A case of milia en plaque successfully treated with oral etretinate. Br J Dermatol. 2007 Dec;157(6):1287-9. doi: 10.1111/j.1365-2133.2007.08223.x
- Mendiratta V, Sarkar R, Sharma RC, Koranne RV. Milia en plaque- An unusual presentation. Indian J Dermatol. 1999;44:64–5.
- Losada-Campa A, De La Torre-Fraga C, Cruces-Prado M. Milia en plaque. Br J Dermatol. 1996 May;134(5):970-2.
- Keohane SG, Beveridge GW, Benton EC, Cox NH. Milia en plaque–a new site and novel treatment. Clin Exp Dermatol. 1996 Jan;21(1):58-60.
- García Sánchez MS, Gómez Centeno P, Rosen E, Sánchez-Aguilar D, Fernández-Redondo V, Toribio J. Milia en plaque in a bilateral submandibular distribution. Clin Exp Dermatol. 1998 Sep;23(5):227-9.
- Combemale P, Faisant M, Dupin M. ‘Milia en plaque’ in the supraclavicular area. Dermatology. 1995;191(3):262-3. doi: 10.1159/000246560
- Terui H, Hashimoto A, Yamasaki K, Aiba S. Milia En Plaque as a Distinct Follicular Hamartoma With Cystic Trichoepitheliomatous Features. Am J Dermatopathol. 2016;38(3):212-217. doi:10.1097/DAD.0000000000000445 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4760378
- Rose RF, Merchant W, Goulden V. Retroauricular milia en plaque: a rare presentation of lupus erythematosus. Clin Exp Dermatol. 2008 Nov;33(6):715-7. doi: 10.1111/j.1365-2230.2008.02863.x
- Terui H., Hashimoto A., Yamasaki K., Aiba S. Milia en plaque as a distinct follicular hamartoma with cystic trichoepitheliomatous features. Am J Dermatopathol. 2016; 38: 212-217.
- Leverkus M, Rose C, Bröcker EB, Goebeler M. Follicular cutaneous T-cell lymphoma: beneficial effect of isotretinoin for persisting cysts and comedones. Br J Dermatol. 2005 Jan;152(1):193-4. doi: 10.1111/j.1365-2133.2005.06360.x
- Bridges AG, Lucky AW, Haney G, Mutasim DF. Milia en plaque of the eyelids in childhood: case report and review of the literature. Pediatr Dermatol. 1998 Jul-Aug;15(4):282-4. doi: 10.1046/j.1525-1470.1998.1998015282.x
- Lee DW, Choi SW, Cho BK. Milia en plaque. J Am Acad Dermatol. 1994 Jul;31(1):107. doi: 10.1016/s0190-9622(09)80235-1
- van Lynden-van Nes AM, der Kinderen DJ. Milia en plaque successfully treated by dermabrasion. Dermatol Surg. 2005 Oct;31(10):1359-62, discussion 1362. doi: 10.1111/j.1524-4725.2005.31221
- Sandhu K, Gupta S, Handa S. CO2 laser therapy for Milia en plaque. J Dermatolog Treat. 2003 Dec;14(4):253-5. doi: 10.1080/09546630310016754
- Tsoïtis G, Papadimitriou C, Asvesti C, Lefaki J, Lambroudi M, Hatzibougias J, Babi A. Dermatoses rétro-auriculaires à type de grains de milium en plaque [Retroauricular dermatitis of the “milia en plaque” type]. Ann Dermatol Venereol. 1993;120(1):58-64. French.
- Bilateral malar milia en plaque as primary presentation of discoid lupus erythematosus. JAAD Case Reports 2017;3:106-9. https://doi.org/10.1016/j.jdcr.2017.01.010
- Cho SH, Cho BK, Kim CW. Milia en plaque associated with pseudoxanthoma elasticum. J Cutan Pathol. 1997 Jan;24(1):61-3. doi: 10.1111/j.1600-0560.1997.tb00788.x
- Boehm I, Schupp G, Bauer R. Milia en plaque arising in discoid lupus erythematosus. Br J Dermatol. 1997 Oct;137(4):649-51. doi: 10.1111/j.1365-2133.1997.tb03807.x
- Leverkus M, Rose C, Bröcker EB, Goebeler M. Follicular cutaneous T-cell lymphoma: beneficial effect of isotretinoin for persisting cysts and comedones. Br J Dermatol. 2005 Jan;152(1):193-4. doi: 10.1111/j.1365-2133.2005.06360.x.
- de Wet J, Jordaan HF, Visser WI. Bilateral malar milia en plaque as primary presentation of discoid lupus erythematosus. JAAD Case Rep. 2017;3(2):106-109.
- Carrington PR, Nelson-Adesokan P, Smoller BR. Plaque-like erythema with milia: a noninfectious dermal mucinosis mimicking cryptococcal cellulitis in a renal transplant recipient. J Am Acad Dermatol. 1998;39(2 Pt 2):334-337.
- Dogra S, Kaur I, Handa S. Milia en plaque in a renal transplant patient: a rare presentation. Int J Dermatol. 2002;41(12):897-898.
- Vajdi T, Lee WW, Paravar T. Penicillamine-associated cutis laxa and milia en plaque – case report and review of cutaneous changes associated with penicillamine. Dermatol Online J. 2016;22(5).
- Boehm I, Schupp G, Bauer R. Milia en plaque arising in discoid lupus erythematosus. Br J Dermatol. 1997;137(4):649-651.
- Beutler BD, Cohen PR. Cryotherapy-induced milia en plaque: case report and literature review. Dermatol Online J. 2014;21(2).
- Kouba DJ, Owens NM, Mimouni D, Klein W, Nousari CH. Milia en plaque: a novel manifestation of chronic cutaneous lupus erythematosus. Br J Dermatol. 2003;149(2):424-426.
- Terui H, Hashimoto A, Yamasaki K, Aiba S. Milia en plaque as a distinct follicular hamartoma with cystic trichoepitheliomatous features. Am J Dermatopathol. 2016;38(3):212-217.
- What Is This Skin Eruption? https://www.the-dermatologist.com/article/what-skin-eruption?page=1
- Berk DR, Bayliss SJ. Milia: a review and classification. J Am Acad Dermatol. 2008;59(6):1050-1063.
- Lee SH, Kim SC. Linear milia en plaque on the central face: an acquired skin rash following Blaschko’s lines? J Dermatol. 2012;39(11):936-937.
- Lee KY, Oh SW, Kim SC. A case of milia en plaque treated with modified rhomboid transposition flap. Korean J Dermatol. 2007;45:1227-1229.
- Ishiura N, Komine M, Kadono T, Kikuchi K, Tamaki K. A case of milia en plaque successfully treated with oral etretinate. Br J Dermatol. 2007;157(6):1287-1289.
- Fujita H, Iguchi M, Kenmochi Y, Fukunaga Y, Asahina A. Milia en plaque on the forehead. J Dermatol. 2008;35(1):39-41.