Morsicatio buccarum
Morsicatio buccarum also known as cheek-biting, habitual cheek biting, chronic cheek biting or chronic cheek chewing, is typically not a presenting complaint but an interesting diagnosis made as an aside during a complete oral examination 1. Morsus is the Latin word for “bite” and morsicatio buccarum refers to biting or chewing the buccal mucosa, morsicatio labiorum is a chewing or sucking of the lip tissue and morsicatio linguarum is chewing of the borders of the tongue 2. Clinically, morsicatio buccarum is a macerated grey-white patch and plaque of the mucosa caused by external stimuli (self-induced injury) such as habitual biting, chewing, or sucking of the lip 3. The shaggy, macerated cheeks seen (not removed by wiping) are asymptomatic or at most minimally uncomfortable. The lesions are usually bilateral, although sometimes they are limited to one location, depending on the parafunctional habits of the patient 4. There is variability in the location of biting with cheeks+lips > cheeks alone > lips alone and bilateral > unilateral. Most patients with this condition are unaware of their biting habit and will not aid in the diagnosis. Morsicatio buccarum, morsicatio labiorum and morsicatio linguarum is generally found among people who are stressed or psychologically impaired 5. Patients with this condition have a compulsive neurosis that causes habitual tongue or lip biting.
Reported cases of morsicatio buccarum, morsicatio labiorum or morsicatio linguarum are rare 6. Morsicatio buccarum and morsicatio labiorum is often confused with other dermatological disorders involving the oral mucosa such as lichen planus, pemphigus, benign mucosal pemphigoid, candidiasis, hairy leukoplakia, leukoedema, white sponge nevus, chemical burn or cancer, which can lead to a misdiagnosis. Some helpful clinical features that distinguish this from other whitish lesions are a rough, shaggy, often peeling surface 7. In addition, morsicatio is usually bilateral and located on movable, nonkeratinized mucosa that can be reached by the teeth 8. Although proliferative leukoplakia may be bilateral and sometimes even symmetric, they will often involve areas that cannot be reached by the teeth (such as the gingiva) 8. If the clinician is not absolutely certain that a white lesion is a morsicatio, a biopsy is always warranted 8.
Being careful to make a correct diagnosis can help one avoid providing inappropriate treatment 9. Most dentists are familiar with morsicatio buccarum et labiorum and seldom examine it via biopsy 10. However, it is rarely described in pathologic or dermatological textbooks, so dermatologists and pathologists are generally unfamiliar with this condition. The lesions regress once the biting of the cheek, lip or tongue stops. Morsicatio buccarum, morsicatio labiorum or morsicatio linguarum lesion is not considered to be potentially malignant 9.
Figure 1. Morsicatio buccarum
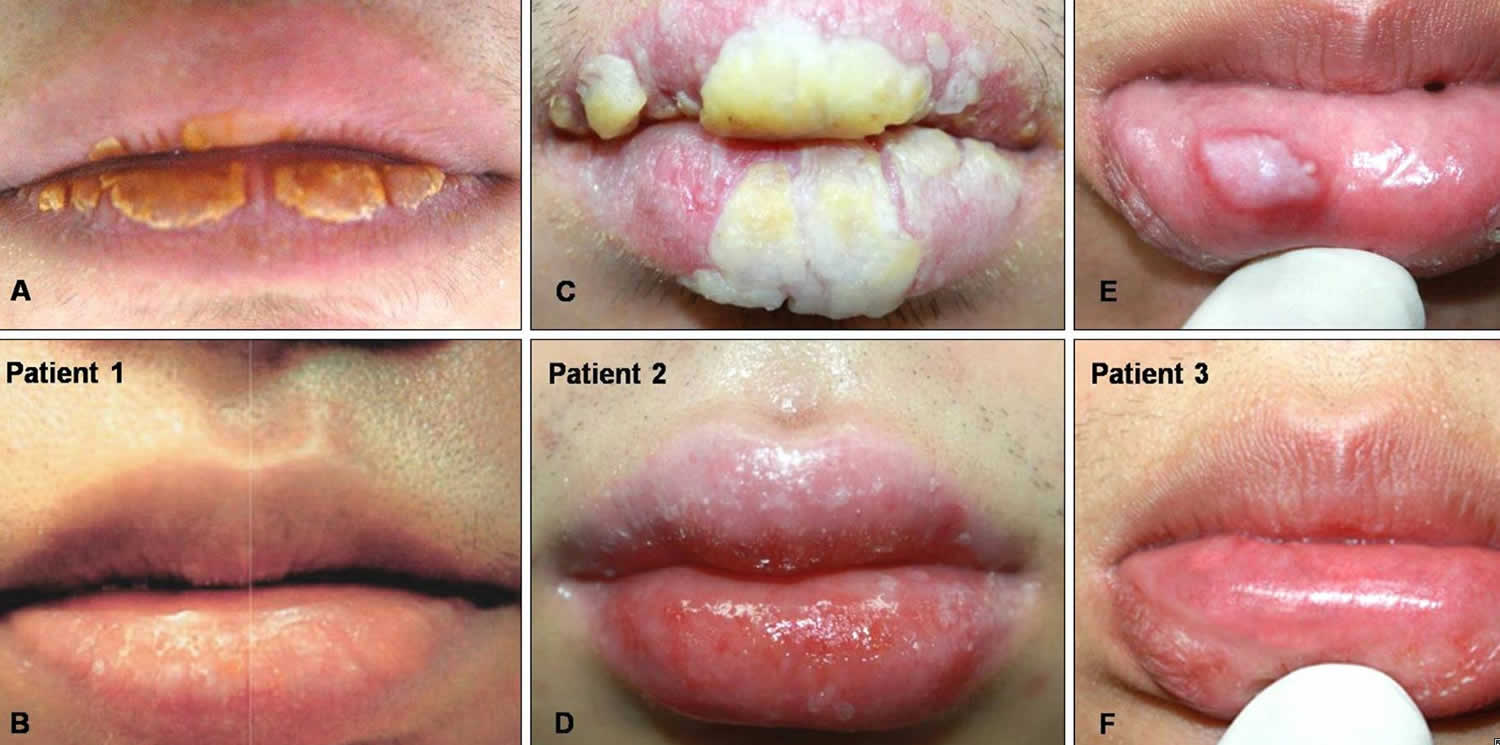
Figure 2. Morsicatio labiorum
Footnote: (A, C) Localized yellow hyperkeratotic plaques on the upper and lower lips in patients 1 & 2. (E) A well-demarcated, white, smooth plaque on the lower lip in patient 3. (B, D, F) The lesions had completely disappeared after the patients retained from their lesion causing habits.
[Source 7 ]Morsicatio buccarum causes
Morsicatio buccarum (cheek biting) and morsicatio labiorum (lip biting) is a form of self-inflicted injury that is caused by habitual cheek and lip chronic tissue irritation, such as biting or sucking 11. Patients actually hold pieces of mucosa between their teeth and tear them free from the surface, producing a distinctive clinical appearance termed morsicatio buccarum et labiorum 12.
Sometimes it may be confused with other dermatological disorders involving the oral mucosa, and can lead to misdiagnosis. Most people are aware of a cheek chewing habit, although it may be performed subconsciously 13. Sometimes poorly constructed prosthetic teeth may be the cause if the original bite is altered. Usually the teeth are placed too far facially (i.e. buccally and/or labially), outside the “neutral zone”, which is the term for the area where the dental arch is usually situated, where lateral forces between the tongue and cheek musculature are in balance. Glassblowing involves chronic suction and may produce similar irritation of the buccal mucosa 13. Identical, or more severe damage may be caused by self-mutilation in people with psychiatric disorders, learning disabilities or rare syndromes (e.g. Lesch–Nyhan syndrome and familial dysautonomia) 14.
Morsicatio buccarum signs and symptoms
Morsicatio buccarum, morsicatio labiorum or morsicatio linguarum is one of several self-inflicted or factitious injuries to the oral mucous membranes. Previous authors have thought that this results from a habitual biting or chewing of the oral mucosa 5. The lesions are located on the mucosa, usually bilaterally in the central part of the anterior buccal mucosa and along the level of the occlusal plane (the level at which the upper and lower teeth meet) 15. Sometimes the tongue or the labial mucosa (the inside lining of the lips) is affected by a similarly produced lesion, termed morsicatio linguarum and morsicatio labiorum respectively 13. There may be a coexistent linea alba, which corresponds to the occlusal plane 14 or crenated tongue. The lesions are white with thickening and shredding of mucosa commonly combined with intervening zones of erythema (redness) or ulceration 13. Clinical lesions result from torn-off ragged oral mucosa consisting of small superficial erosions alternating with white scaly areas 5. However, foci of erythema, erosion, or traumatic ulceration can occasionally be identified 15. It is thought that the surface irregularity of the oral mucosa may precede the onset of biting habits, and patients feel compelled to remove the lesion by manipulation 16. The scales are loose and can be removed easily.
Morsicatio buccarum diagnosis
A biopsy is essential to prevent misdiagnosis and incorrect treatment. Histopathologically, the hyperplastic epithelium shows acanthosis and hyperkeratosis with an irregular torn surface at which Gram-positive bacterial colonies and basophilic debris are present 6. A thin layer of necrotic keratinocytes can be seen immediately beneath the basophilic debris. In the stratum spinosum there are markedly swollen keratinocytes which display periodic acid-Schiff (PAS) stain-positive, diastase-digestible material consistent with glycogen. Mild chronic inflammatory infiltration can be seen in the stroma and occasionally reactive atypia are present if there is ulceration or inflammation 17. Because these findings are not that pathognomonic, biopsy specimens had previously been misinterpreted as nonspecific chronic inflammation of the oral mucosa 15.
Morsicatio buccarum treatment
The lesions are harmless, and no treatment is indicated beyond reassurance, unless the person requests it. The lesions regress once the biting of the cheek, lip or tongue stops. The most common and simple treatment is construction of a specially made acrylic prosthesis that covers the biting surfaces of the teeth and protects the cheek, tongue and labial mucosa (an occlusal splint). This is either employed in the short term as a habit breaking intention, or more permanently (e.g. wearing the prosthesis each night during sleep). Psychological intervention is also reported, but does not appear to be beneficial 13. A self-help technique, termed decoupling, has shown benefits in a single case study 18.
References- OBERMAYER ME. Cheekbiting (Morsicatio Buccarum). Arch Dermatol. 1964;90(2):185–190. doi:10.1001/archderm.1964.01600020053012
- Tomás Carmona I, Cameselle Tejeiro J, Diz Dios P, Seoane Lestón J, Castro Ferreiro M, Limeres Posse J. Morsicatio linguarum versus oral hairy leukoplakia. Dermatology. 2000;201(3):281-2. https://doi.org/10.1159/000018483
- Kang HS, Lee HE, Ro YS, Lee CW. Three cases of ‘morsicatio labiorum’. Ann Dermatol. 2012;24(4):455-458. doi:10.5021/ad.2012.24.4.455
- Obermayer ME. Cheekbiting (Morsicatio buccarum). Arch Dermatol1964; 90: 185-90.
- Morsicatio Labiorum/Linguarum. Three Cases Report and a Review of the Literature. The Korean Journal of Pathology 2009; 43: 174-6 DOI: 10.4132/KoreanJPathol.2009.43.2.174 https://www.jpatholtm.org/upload/pdf/kjp-43-2-174.pdf
- Carmona IT, Tejeiro JC, Dios PD, Leston JS, Ferreiro MC, Posse JL.Morsicatio linguarum versus oral hairy leukoplakia. Dermatology2000; 201: 281-2.
- Kang HS, Lee HE, Ro YS, Lee CW. Three cases of ‘morsicatio labiorum’. Ann Dermatol. 2012;24(4):455-458. doi:10.5021/ad.2012.24.4.455 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3505778
- Woo SB, Lin D. Morsicatio mucosae oris–a chronic oral frictional keratosis, not a leukoplakia. J Oral Maxillofac Surg. 2009;67:140–146.
- Banoczy J. Oral leukoplakia and other white lesions of the oral mucosarelated to dermatological disorders. J Cutan Pathol 1983; 10: 238-56.
- Glass LF, Maize JC. Morsicatio buccarum et labiorum (excessive cheekand lip biting). Am J Dermatopathol 1991; 13: 271-4.
- Damm DD, Fantasia JE. Bilateral white lesions of buccal mucosa: mor-sicatiobuccarum. Gen Dent 2006; 54: 442, 444.
- Glass LF, Maize JC. Morsicatio buccarum et labiorum (excessive cheek and lip biting). Am J Dermatopathol 1991; 13: 271-4.
- Bouquot, Jerry E.; Brad W. Neville; Douglas D. Damm; Carl M. Allen (2002). Oral & maxillofacial pathology (2. ed.). Philadelphia: W.B. Saunders. pp. 253–254. ISBN 0721690033
- Scully, Crispian (2008). Oral and maxillofacial medicine : the basis of diagnosis and treatment (2nd ed.). Edinburgh: Churchill Livingstone. pp. 223, 349. ISBN 9780443068188
- Allen AM, Camisa C. Oral disease. In: Callen JP, Horn TD, Mancini AJ, Salasche SJ, Schaffer JV, Schwarz T, et al., editors. Dermatology. 2nd ed. Spain: Mosby Elsevier; 2008. p. 1044.
- Glass LF, Maize JC. Morsicatio buccarum et labiorum (excessive cheek and lip biting) Am J Dermatopathol. 1991;13:271–274.
- Obermayer ME. Cheekbiting (morsicatio buccarum) Arch Dermatol. 1964;90:185–190.
- Escaping the mouth-trap: Recovery from long-term pathological lip/cheek biting (morsicatio buccarum, cavitadaxia) using decoupling. Journal of Obsessive-Compulsive and Related Disorders Volume 25, April 2020, 100530 https://doi.org/10.1016/j.jocrd.2020.100530