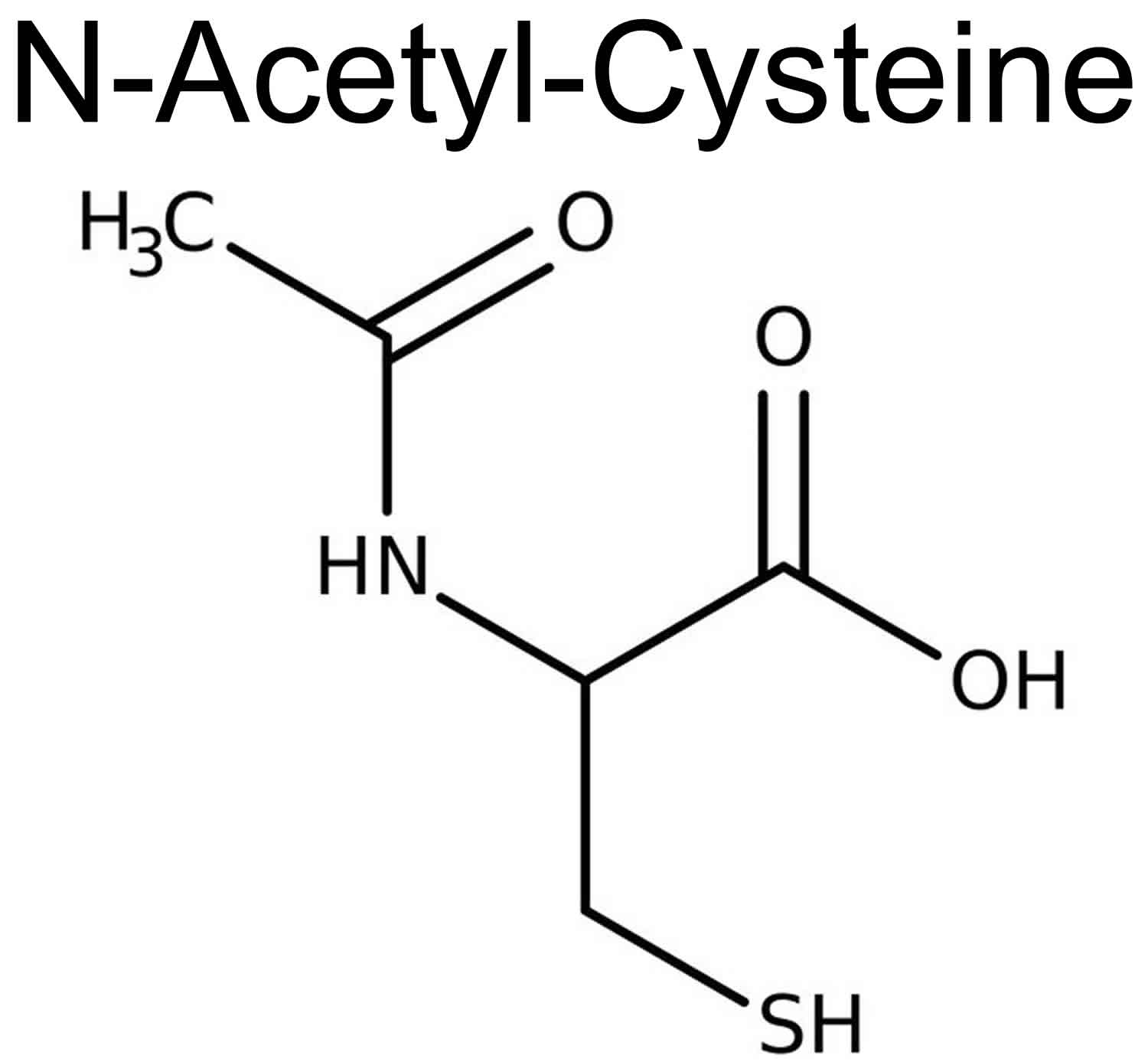
What is N-Acetyl-Cysteine
N-Acetyl-Cysteine (NAC) also known as N-acetylcysteine or acetylcysteine, is the acetylated precursor of both the amino acid L-cysteine and reduced glutathione (GSH), which is itself a component of an antioxidant. N-Acetyl-Cysteine repletes glutathione reserves by providing cysteine, which is an essential precursor in glutathione production. N-Acetyl-Cysteine by itself also binds to the toxic metabolites and scavenges free radicals. It also increases oxygen delivery to tissues, increases mitochondrial ATP production, and alters the microvascular tone to increase the blood flow and oxygen delivery to the liver and other vital organs 1. N-Acetyl-Cysteine has been shown to increase the levels of the brain’s primary antioxidant, glutathione, decrease pro‐inflammatory cytokines and enhance neurogenesis 2. Historically N-acetylcysteine has been used as a mucolytic agent to loosen thick mucus in chronic respiratory illnesses as well as an antidote for liver toxicity (hepatotoxicity) due to acetaminophen (paracetamol) overdose 1. More recently, animal and human studies of N-Acetyl-Cysteine have shown it to be a powerful antioxidant and a potential therapeutic agent in the treatment of cancer, heart disease, human immunodeficiency virus (HIV) infection, heavy metal toxicity, and other diseases characterized by free radical, oxidant damage 3. N-Acetyl-Cysteine may help protect against oxidative stress by maintaining or increasing antioxidant levels in the body. N-Acetyl-Cysteine has also been shown to be of some value in treating Sjogren’s syndrome 4, illness associated with cigarette smoking 5, influenza 6, hepatitis C 7 and myoclonus epilepsy 8. Some clinical trials testing formulations that included N-acetylcysteine have found modest improvements in cognitive function, but clinical trials testing it alone have shown less robust results. N-acetylcysteine supplements are generally regarded as safe when taken at recommended doses.
After oral administration, N-Acetyl-Cysteine undergoes deacetylation in the liver to form cysteine, which is used as substrate for glutathione (GSH) production 9. Unconverted cysteine enters the blood stream; however, reports on the ability of cysteine or the parent N-Acetyl-Cysteine compound, to cross the blood brain barrier (BBB) are contradictory 10. Regardless, detection of increased GSH levels in the brain were evident after administration of N-Acetyl-Cysteine to rats 11. More recently, patients with major depressive disorder supplemented with N-Acetyl-Cysteine were found to have increased levels of N-Acetyl-Cysteine metabolites (necessary for GSH production) in the anterior cingulate cortex detected by proton magnetic spectroscopy 12. These studies suggest that N-Acetyl-Cysteine does initiate effects in the brain. It has been postulated that cysteine may cross the blood brain barrier (BBB) via a sodium-dependent transport system where it is converted into cystine, the di-sulfide derivative of cysteine 13. High levels of cystine stimulate the exchange of intracellular glutamate for cystine through the cystine-glutamate antiporter, thereby elevating non-synaptic glutamate 14. This process activates the metabotropic glutamate receptors (mGluR2/3) on presynaptic neurons, responsible for inhibiting the synaptic release of glutamate and thereby restoring extracellular glutamate levels in the nucleus accumbens 15. Regulating this exchange system has been shown to improve impulse control and reduce addictive behavior both pre-clinically and clinically 16. Intracellular cystine can then be reduced back to cysteine and used for GSH production, the potent and most abundant endogenous antioxidant in the body 17.
A clearer understanding of the pharmacokinetics and pharmacodynamics of N-Acetyl-Cysteine has prompted clinical investigations of this nutraceutical as a glutamate-modulating therapeutic agent for psychiatric conditions, including addictive behavior (such as gambling, cocaine, nicotine and marijuana use) 18, bipolar disorder 19, schizophrenia 20 and autism 21. The ability of N-Acetyl-Cysteine to modulate factors associated with obsessive compulsive disorder (OCD) and obsessive compulsive related disorders, such as the regulation of extracellular glutamate and the reduction of oxidative stress (through direct radical scavenging and increasing GSH activity), indicates that N-Acetyl-Cysteine may be an effective treatment for obsessive compulsive disorder (OCD) and obsessive compulsive related disorders 22. Animal studies have provided some support of this hypothesis. In a mouse model of obsessive compulsive disorder (OCD) involving marble burying behavior, N-Acetyl-Cysteine dose-dependently decreased burying behavior independent of locomotor activity 23.
N-Acetyl-Cysteine benefits
N-Acetyl-Cysteine (NAC) has the US Food and Drug Administration (FDA) approval for the treatment of potentially liver toxic doses of acetaminophen (paracetamol) and it is almost 100% effective if given within 8 hours post-ingestion 24. N-Acetyl-Cysteine is also approved for use in conditions with abnormal, viscid or thickened mucous secretions such as pneumonia, bronchitis, tracheobronchitis, cystic fibrosis, tracheostomy patients, postoperative pulmonary complications, posttraumatic chest conditions and before diagnostic bronchoscopy to help with mucous plugging 1. Off-label N-acetylcysteine indications include acute liver failure, prevention of contrast-induced nephropathy and topical treatment of keratoconjunctivitis sicca.
In chronic obstructive pulmonary disease (COPD), cystic fibrosis, and other lung conditions, nebulized N-Acetyl-Cysteine has mucolytic, anti-inflammatory, and antioxidant properties 1. Studies are ongoing to understand its therapeutic efficacy, ideal dose ranges, and most effective mode of drug delivery for these indications.
N-Acetyl-Cysteine has also been investigated for use in xenobiotics with free radical or reactive metabolite toxicity. There is good evidence to show it is of benefits in acute exposures to cyclopeptide containing mushrooms and carbon tetrachloride 25. There are animal and human tissue studies showing its use in decreasing cisplatin-induced kidney toxicity 26, although clinical evidence is minimal. N-Acetyl-Cysteine may also have therapeutic application in chronic valproate liver toxicity and acute pennyroyal or clove oil ingestion-induced liver toxicity 27.
Other potential applications, but still in the experimental stage, include N-Acetyl-Cysteine being used as an anti-cancer agent as well as for psychiatric conditions like schizophrenia, bipolar disorder, depression, gastrointestinal conditions like hepatorenal syndrome, Helicobacter pylori infections, necrotizing enterocolitis, critical care patients like lung injury, cardiac injury, multiorgan dysfunction, sepsis and hematological conditions like sickle cell disease 1.
There are case reports of N-Acetyl-Cysteine helping with improving neurological status in patients comatose with carbon monoxide poisoning 28.
Acetaminophen overdose
Acetaminophen (paracetamol) poisoning is the most common medication poisoning reported to United States poison centers and accounts for more than 30,000 hospital admissions every year in the U.S. alone 29. N-Acetyl-Cysteine exerts its therapeutic effect in acetaminophen (paracetamol) overdose through several mechanisms. Acetaminophen (paracetamol) metabolism in therapeutic dosing primarily occurs through glucuronidation and sulfation (>90%), with less than 5% being oxidized by CYP450 isoform (predominately CYP2E1) to produce a toxic metabolite called N-acetyl-p-benzoquinone imine (NAPQI), which is the precursor to cellular injury 1. Glutathione (GSH) in the liver can normally detoxify these minuscule quantities of N-acetyl-p-benzoquinone imine (NAPQI) and prevent tissue damage. In acetaminophen (paracetamol) overdose, glucuronidation and sulfation pathways are saturated, and the CYP450 pathway takes more significance, producing more toxic metabolites that deplete the glutathione (GSH) reserves, leading to their accumulation and hence tissue injury by binding to cellular macromolecules 1.
N-Acetyl-Cysteine repletes glutathione reserves by providing cysteine, which is an essential precursor in glutathione production. N-Acetyl-Cysteine by itself also binds to the toxic metabolites and scavenges free radicals. It also increases oxygen delivery to tissues, increases mitochondrial ATP production, and alters the microvascular tone to increase the blood flow and oxygen delivery to the liver and other vital organs.
The decision to give N-Acetyl-Cysteine (NAC) in acetaminophen (paracetamol) overdose depends on the likelihood of hepatotoxicity in the patient. Assessment is by obtaining a thorough history, physical examination, and serum acetaminophen (paracetamol) and transaminase concentrations.
A detailed history including the quantity of acetaminophen (paracetamol) consumed is necessary. It is important to know whether consumption took place all at once or overtime. History of any other coingestants like anticholinergic medications or opioids that could cause a delayed absorption of acetaminophen (paracetamol) is also necessary, as is the presence of risk factors including malnutrition, alcoholism, or cirrhosis as these have associations with decreased glutathione reserves. Determination should also be made whether the acetaminophen (paracetamol) formulation taken is a regular or an extended-release preparation as the latter can cause a delayed peak serum concentration. Determination should also be made about the concurrent use of drugs that can induce CYP2E1 (for example, isoniazid and chronic alcohol consumption), which increases the risk of hepatotoxicity.
The Rumack-Mathew Nomogram is a useful tool to assess the risk of hepatotoxicity and hence the need for starting N-Acetyl-Cysteine in an acute single ingestion of acetaminophen (paracetamol) 30.
- If the time of ingestion of acetaminophen (paracetamol) is less than 4 hours, 4-hour levels of serum acetaminophen (paracetamol) are obtained and plotted on the nomogram. If it is above the treatment line, starting N-Acetyl-Cysteine should be the course of action. If it is below, the risk of hepatotoxicity is virtually nonexistent.
- If the time of ingestion is between 4 and 24 hours and the time required to obtain serum acetaminophen (paracetamol) levels is less than 8 hours, one may wait for the acetaminophen (paracetamol) levels before deciding to start N-Acetyl-Cysteine. If the acetaminophen (paracetamol) levels reports are not obtainable until more than 8 hours have passed, N-Acetyl-Cysteine can be started empirically and stopped if the levels are below the treatment line.
- If the acetaminophen (paracetamol) dose ingested is unclear or if it’s been more than 24 hours since ingestion, give the first dose of N-Acetyl-Cysteine and send acetaminophen (paracetamol) levels and transaminases levels. If acetaminophen (paracetamol) levels are more than 10 mg/L OR transaminases are elevated, N-Acetyl-Cysteine can be continued.
- In chronic ingestion, N-Acetyl-Cysteine therapy should be initiated if acetaminophen (paracetamol) levels are more than 20 mg/L or transaminases are elevated. In pregnant women, there are no reports of fetal risk with starting N-Acetyl-Cysteine. Dosing for these patients can initiate according to similar protocols as in the general population.
N-Acetyl-Cysteine may be given either orally or intravenously with minimal differences in its effectiveness 31. The commonest regimes used are 21-hour IV protocol and 72-hour oral dosing protocol. N-Acetyl-Cysteine should be started in patients at risk of hepatotoxicity and continued if hepatotoxicity develops. It may be stopped following the completion of the protocol or upon resolution of hepatotoxicity, whichever occurs last. Both oral and IV routes of administration are equally efficacious in preventing and treating acetaminophen (paracetamol) overdose toxicity. The IV route has preference over the oral route in established hepatic failure and in patients who cannot tolerate oral N-Acetyl-Cysteine due to intractable vomiting or nausea 32.
N-Acetyl-Cysteine is available as a 20% concentration in 30 ml vials that requires dilution before being given IV. Oral N-Acetyl-Cysteine is available in 10% and 20% vials of 10 ml each, which also requires dilution before administration.
The dosing schedule for the 21-hour IV protocol is as follows:
- Loading dose: 150mg/kg up to a maximum of 15 gm in 200 ml Dextrose 5% Water over 60 minutes.
- Second (maintenance) dose: 50mg/kg up to a maximum of 5 gm in 500 ml Dextrose 5% Water over 4 hours (12.5 mg/kg/hour).
- Third dose: 100mg/kg up to a maximum of 10 gm in 1000 ml Dextrose 5% Water over 16 hours (6.25 mg/kg/hour).
The dosing schedule for the 72-hour Oral N-Acetyl-Cysteine protocol is as follows:
- 140 mg/kg loading dose orally.
- After 4 hours of the loading dose, 70 mg/kg should be given every 4 hours for an additional 17 doses, which is a total dose of 1330 mg/kg. The solution should be diluted to 5% and preferably mixed with a soft drink or juice to enhance palatability.
- Any vomited doses should be readministered.
N-Acetyl-Cysteine should be continued until acetaminophen (paracetamol) levels are undetectable, prothrombin time (PT) or International Normalized Ratio (INR) is near normal, encephalopathy has resolved, and transaminases are normal or are down trending and AST < 1000 U/L. In the 21-hour IV protocol, the acetaminophen (paracetamol) levels and transaminases level testing should occur at 20 hours. The oral protocol requires checking at 24 hours. If acetaminophen (paracetamol) is undetectable and transaminase levels are normal, N-Acetyl-Cysteine can be discontinued at the end of the regime. If there is a detectable acetaminophen (paracetamol) level or AST is still elevated, restarting N-Acetyl-Cysteine at 6.25 mg/kg per hour (for IV protocol) or 70 mg/kg every four hours (for oral protocol) is the proper course. This can be continued until the patient returns to normal mental status and INR is below 2.0 or if the patient obtains a liver transplant 1.
Dementia
No randomized controlled trials have examined whether N-Acetyl-Cysteine alone can prevent cognitive decline or dementia, though some evidence exists for combination therapies. No studies have examined prevention of cognitive decline or dementia in humans with N-acetylcysteine alone. In a clinical trial of thirty-four individuals with mild cognitive impairment, daily consumption of a nutraceutical formulation containing 600 mg of N-Acetyl-Cysteine (along with folate, alpha-tocopherol, vitamin B12, S-adenosyl methionine, and acetyl-L-carnitine) for 6 months was associated with improvement in dementia rating scale and executive function 33. However, no direct comparisons were made between the nutraceutical treatment group and the placebo group, making the results inconclusive. Another clinical trial using the same nutraceutical formulation for three months did find that it was associated with improved verbal learning compared to the placebo group 34. And both the placebo and nutraceutical groups improved further during a three-month extension during which everyone received the formulation.
A clinical trial in Alzheimer’s patients found that a nutraceutical formulation containing N-acetylcysteine resulted in significant improvements in some cognitive functions compared to the placebo group 35. However, a clinical trial testing it alone showed less robust effects. The patients receiving N-Acetyl-Cysteine performed better than the placebo group on a letter fluency task but not on other cognitive tests 36.
Moreover, studies conducted in patients with schizophrenia 37 or bipolar disorder 38 testing the effects of N-Acetyl-Cysteine alone found only limited evidence for cognitive protection.
Respiratory illness
Several animal and human studies have explored N-Acetyl-Cysteine’s effectiveness as a therapeutic agent forv arious types of respiratory illness. While results varied, N-Acetyl-Cysteine administration resulted in decreased expectoration difficulty, cough severity 39 and diaphragm fatigue 40. A small study was conducted with 18 patients diagnosed with fibrosing alveolitis; a condition characterized by severe oxidative stress and decreased glutathione levels. N-Acetyl-Cysteine was administered at a dose of 600 mg three times daily for 12 weeks and improvement in both pulmonary function and glutathione levels was noted 41. In contrast, studies ofpatients with chronic bronchitis, severe airway obstruction, and cystic fibrosis showed a slight, although not statistically significant, decrease in the exacerbation rate 42.
HIV infection
Human immunodeficiency virus (HIV)-positive individuals usually exhibit low glutathione (GSH) and cysteine levels, prompting studies on N-Acetyl-Cysteine’s effectiveness as a therapeutic tool for these patients. Research suggests that N-Acetyl-Cysteine is capable of enhancing T cell immunity by stimulating T cell colony formation 43 and blocking NF kappa B expression 44. In a double-blind, placebo-controlled trial Akerlund et al 45 found N-Acetyl-Cysteine to positively impact both plasma cysteine levels and CD4+ lymphocyte cell counts. More studies are needed but it appears that if given to HIV-positive patients early in the course of disease, N-Acetyl-Cysteine may help to prevent progression to AIDS.
Cancer and chemoprevention
Research has shown N-Acetyl-Cysteine to have potential both as a chemopreventative agent and a treatment in certain types of cancer, including lung, skin, head and neck, mammary, and liver cancer 46. In vitro (test tube) studies have demonstrated N-Acetyl-Cysteine to be directly anti-mutagenic and anti-carcinogenic as well as inhibiting the mutagenicity of certain compounds in vivo (animal study) 47. Research also indicates N-Acetyl-Cysteine administration in both cell cultures and animal studies selectively protects normal cells, but not malignant ones, from chemotherapy and radiation toxicity 48. Other in vitro studies noted N-Acetyl-Cysteine’s effectiveness at inhibiting cell growth and proliferation in human melanoma 49, prostate 50 and astrocytoma 51 cell lines.
Heart disease
Several small clinical studies have demonstrated that N-Acetyl-Cysteine may be an effective therapeutic agent in the management of heart disease. Wiklund et al 52 demonstrated N-Acetyl-Cysteine’s ability to reduce plasma homocysteine levels by 45 percent, while Gavish and Breslow 53 demonstrated N-Acetyl-Cysteine (2-4 grams daily foreight weeks) was able to reduce lipoprotein(a) by 70 percent. Due to its ability to significantly increase tissue glutathione (GSH), N-Acetyl-Cysteine may also be useful in treating the ischemia and reperfusion seen in acute myocardial infarction, and the resultant depletion in cellular sulfhydryl groups 54. In addition, N-Acetyl-Cysteine appears to potentiate nitroglycerin’s coronary dilating and anti-platelet properties and therefore may be a useful combination therapy in-patients with unstable angina pectoris and myocardial infarction 55.
What is N-Acetyl-Cysteine good for?
N-Acetyl-Cysteine (NAC) has the US Food and Drug Administration (FDA) approval for the treatment of potentially liver toxic doses of acetaminophen (paracetamol) and it is almost 100% effective if given within 8 hours post-ingestion 24. N-Acetyl-Cysteine is also approved for use in conditions with abnormal, viscid or thickened mucous secretions such as pneumonia, bronchitis, tracheobronchitis, cystic fibrosis, tracheostomy patients, postoperative pulmonary complications, posttraumatic chest conditions and before diagnostic bronchoscopy to help with mucous plugging 1. Off-label N-acetylcysteine indications include acute liver failure, prevention of contrast-induced nephropathy and topical treatment of keratoconjunctivitis sicca.
N-Acetyl-Cysteine dosage
N-Acetyl-Cysteine is available as a dietary supplement typically containing 600 mg per capsule. A nutraceutical formulation that showed some cognitive benefits in people with mild cognitive impairment or Alzheimer’s disease contained 600 mg of N-Acetyl-Cysteine, along with other compounds (i.e., folate, alpha-tocopherol, S-adenosyl methionine, acetyl-L-carnitine) 33, 34.
The typical oral dose for N-Acetyl-Cysteine as a mucolytic agent and for most other clinical indications is 600-1500 mg N-Acetyl-Cysteine daily in three divided doses. In patients with cancer or heart disease the therapeutic dosage is higher, usually in the range of two to four grams daily 3. For acetaminophen (paracetamol) poisoning, N-Acetyl-Cysteine isusually administered orally with a loading dose of 140 mg/kg and 17 subsequent doses of 70 mg/kg every four hours. In acetaminophen (paracetamol) poisoning, it is important to begin administering N-Acetyl-Cysteine within 8-10 hours of overdose to ensure effectiveness 56.
Oral administration of N-Acetyl-Cysteine and charcoal at the same time is not recommended, as charcoal may cause a reduction in the absorption of N-Acetyl-Cysteine 57. In addition, as with any single antioxidant nutrient, N-Acetyl-Cysteineat therapeutic doses (even as low as 1.2 grams daily), has the potential to have pro-oxidant activity and is not recommended at these doses in the absence of significant oxidative stress 3.
N-Acetyl-Cysteine side effects
N-Acetyl-Cysteine supplements are generally regarded as safe for most adults when taken at standard doses. The nutraceutical formulation used in older people and those with mild cognitive impairment was well-tolerated and no serious side effects were reported for any of the 300+ participants 33, 35, 36. The most common side-effects associated with high oral N-Acetyl-Cysteine doses are nausea, vomiting, diarrhea, flatulence, gastroesophageal reflux and other gastrointestinal disturbances. Therefore oral N-Acetyl-Cysteine administration is contraindicated in persons with active peptic ulcer. N-acetylcysteine should not be administered with nitroglycerin, as the combination can cause severe hypotension 58 and headache 59. N-acetylcysteine interacts with inhaled insulin (Afrezza, Exubera) and may affect the absorption of insulin into the blood stream.
Infrequently, anaphylactic reactions due to histamine release occur and can consist of rash, pruritis, angioedema, bronchospasm, tachycardia and changes in blood pressure 56. Intravenous administration of N-Acetyl-Cysteine can cause rate related anaphylactoid reactions in up to 18% of patients, which is not an issue with the oral route 60. Most of the anaphylactoid reactions are mild (6%) or moderate (10%) generally in the form of rash or angioedema with severe reactions like bronchospasm and hypotension rare at 1% 61. Interestingly, anaphylactoid reactions occur more commonly with lower acetaminophen (paracetamol) levels than with higher acetaminophen (paracetamol) levels 62. One possible explanation is that acetaminophen (paracetamol) decreases the histamine release from mast cells and mononuclear cells, proportionate to the dose ingested. Bronchospasm more commonly occurs in patients with pre-existing reactive airway diseases, like asthma. Bronchodilating agents are effective in treating these patients.
When an anaphylactoid reaction occurs, N-Acetyl-Cysteine should be stopped immediately, and the patient treated with anti-histamine medication (e.g., diphenhydramine) and IV fluid for hypotension. Vasopressors are not typically necessary. N-Acetyl-Cysteine therapy may restart at a slower rate after the resolution of the reaction. If there is a persistent reaction, oral N-Acetyl-Cysteine should is the alternative approach.
IV N-Acetyl-Cysteine can cause a spurious increase in International Normalized Ratio (INR) which normalizes once infusion stops 63. It can also cause a false-positive result for urine ketones 64.
Oral N-Acetyl-Cysteine may cause vomiting in up to 33% 65. In patients with preexistent gastrointestinal ulcers or varices, there can be concerns about inducing gastrointestinal bleed with oral N-Acetyl-Cysteine.
Contraindications
In patients with a tendency to develop fluid overload (e.g., cardiomyopathy or congestive heart failure), the quantity of diluent fluid used in IV N-Acetyl-Cysteine needs to be appropriately titrated to prevent fluid overload. A pharmacist can perform this titration during the preparation of the N-Acetyl-Cysteine IV infusion.
During IV N-Acetyl-Cysteine administration, patients need to be monitored for manifestations of anaphylactoid reaction as described earlier.
Toxicity
N-Acetyl-Cysteine is “Ames test” negative but animal studies on embryotoxicity are equivocal. In addition, studies in pregnant women are inadequate so N-Acetyl-Cysteine administration during pregnancy should be with caution and only if clearly indicated 66.
Given its complicated regime, N-Acetyl-Cysteine has a high potential for iatrogenic (caused by medical examination or treatment) errors, including overdose 67. A 23-year-old female developed hemolysis, thrombocytopenia, metabolic acidosis and acute renal failure after N-Acetyl-Cysteine overdose. She erroneously received 100 gm instead of 10 gm of N-Acetyl-Cysteine. She then required daily hemodialysis but eventually died after developing hemolytic uremic syndrome 68. Another case report describes a 20-year-old female, who developed hemolysis and elevated serum bilirubin. She improved with supportive measures, and her liver function tests and anemia improved within a few days 69. Massive accidental N-Acetyl-Cysteine administration in the order of 100 mg/kg/hr had resulted in cerebral edema, seizures, uncal herniation, and permanent brain injury in another patient with acetaminophen (paracetamol) overdose 70.
References- Ershad M, Naji A, Vearrier D. N Acetylcysteine. [Updated 2020 Jun 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537183
- Dean O, Giorlando F, Berk M. N‐acetylcysteine in psychiatry: Current therapeutic evidence and potential mechanisms of action. J. Psychiatry Neurosci. 2011; 36: 78–86.
- N-acetylcysteine. Alternative Medicine Review Volume 5, Number 5, 2000. https://altmedrev.com/wp-content/uploads/2019/02/v5-5-467.pdf
- Walters MT, Rubin CE, Keightley SJ, Ward CD. A double-blind, cross-over, study of oral N-acetylcysteine in Sjogren’s syndrome. Scand J Rheumatol Suppl 1986;61:253-258.
- Rogers DF, Jeffery PK. Inhibition by oral N-acetylcysteine of cigarette smoke-induced “bronchitis” in the rat. ExpLung Res 1986;10:267-283.
- De Flora S, Grassi C, Carati L. Attenuation of influenza-like symptomatology and improvement of cell-mediated immunity with long-term N-acetylcysteine treatment. Eur Respir J 1997;10:1535-1541.
- Beloqui O, Prieto J, Suarez M, et al. N-acetylcysteine enhances th response to interferon-alpha in chronic hepatitisC: a pilot study. J Interferon Res 1993;13:279-282.
- Hurd RW, Wilder BJ, Helveston WR, Uthman BM. Treatment of four siblings with progressive myoclonus epilepsy of the Unverricht-Lundborg type with N-acetylcysteine. Neurology 1996;47:1264-1268.
- Atkuri KR, Mantovani JJ, Herzenberg LA, Herzenberg LA. N-Acetylcysteine–a safe antidote for cysteine/glutathione deficiency. Curr Opin Pharmacol. 2007;7:355–359. doi: 10.1016/j.coph.2007.04.005
- Erickson MA, Hansen K, Banks WA. Inflammation-induced dysfunction of the low-density lipoprotein receptor-related protein-1 at the blood-brain barrier: protection by the antioxidant N-acetylcysteine. Brain Behav Immun. 2012;26:1085–1094. doi: 10.1016/j.bbi.2012.07.003
- Dean OM, van den Buuse M, Berk M, Copolov DL, Mavros C, Bush AI. N-acetyl cysteine restores brain glutathione loss in combined 2-cyclohexene-1-one and d-amphetamine-treated rats: relevance to schizophrenia and bipolar disorder. Neurosci Lett. 2011;499:149–153. doi: 10.1016/j.neulet.2011.05.027
- Das P, Tanious M, Fritz K, Dodd S, Dean OM, Berk M, et al. Metabolite profiles in the anterior cingulate cortex of depressed patients differentiate those taking N-acetyl-cysteine versus placebo. Aust N Z J Psychiatry. 2013;47:347–354. doi: 10.1177/0004867412474074
- Smith QR. Transport of glutamate and other amino acids at the blood-brain barrier. J Nutr. 2000 Apr;130(4S Suppl):1016S-22S. doi: 10.1093/jn/130.4.1016S
- Kalivas PW. The glutamate homeostasis hypothesis of addiction. Nat Rev Neurosci. 2009;10:561–572. doi: 10.1038/nrn2515
- Moran MM, McFarland K, Melendez RI, Kalivas PW, Seamans JK. Cystine/glutamate exchange regulates metabotropic glutamate receptor presynaptic inhibition of excitatory transmission and vulnerability to cocaine seeking. J Neurosci. 2005;25:6389–6393. doi: 10.1523/JNEUROSCI.1007-05.2005
- Kupchik YM, Moussawi K, Tang XC, Wang X, Kalivas BC, Kolokithas R, et al. The effect of N-acetylcysteine in the nucleus accumbens on neurotransmission and relapse to cocaine. Biol Psychiatry. 2012;71:978–986. doi: 10.1016/j.biopsych.2011.10.024
- Lushchak VI. Glutathione homeostasis and functions: potential targets for medical interventions. J Amino Acids. 2012;2012:736837. doi: 10.1155/2012/736837
- Gray KM, Watson NL, Carpenter MJ, Larowe SD. N-acetylcysteine (NAC) in young marijuana users: an open-label pilot study. Am J Addict. 2010;19:187–189. doi: 10.1111/j.1521-0391.2009.00027.x
- Berk M, Dean O, Cotton SM, Gama CS, Kapczinski F, Fernandes BS, et al. The efficacy of N-acetylcysteine as an adjunctive treatment in bipolar depression: an open label trial. J Affect Disord. 2011;135:389–394. doi: 10.1016/j.jad.2011.06.005
- Bulut M, Savas HA, Altindag A, Virit O, Dalkilic A. Beneficial effects of N-acetylcysteine in treatment resistant schizophrenia. World J Biol Psychiatry. 2009;10:626–628. doi: 10.1080/15622970903144004
- Hardan AY, Fung LK, Libove RA, Obukhanych TV, Nair S, Herzenberg LA, et al. A randomized controlled pilot trial of oral N-acetylcysteine in children with autism. Biol Psychiatry. 2012;71:956–961. doi: 10.1016/j.biopsych.2012.01.014
- Berk M, Malhi GS, Gray LJ, Dean OM. The promise of N-acetylcysteine in neuropsychiatry. Trends Pharmacol Sci. 2013;34:167–177. doi: 10.1016/j.tips.2013.01.001
- Egashira N, Shirakawa A, Abe M, Niki T, Mishima K, Iwasaki K, et al. N-acetyl-L-cysteine inhibits marble- burying behavior in mice. J Pharmacol Sci. 2012;119:97–101. doi: 10.1254/jphs.11228SC
- Prescott, L. F., Illingworth, R. N., Critchley, J. A., Stewart, M. J., Adam, R. D., & Proudfoot, A. T. (1979). Intravenous N-acetylcystine: the treatment of choice for paracetamol poisoning. British medical journal, 2(6198), 1097–1100. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1597048/pdf/brmedj00098-0009.pdf
- Flanagan RJ, Meredith TJ. Use of N-acetylcysteine in clinical toxicology. Am J Med. 1991 Sep 30;91(3C):131S-139S. doi: 10.1016/0002-9343(91)90296-a
- Nisar S, Feinfeld DA. N-acetylcysteine as salvage therapy in cisplatin nephrotoxicity. Ren Fail. 2002 Jul;24(4):529-33. doi: 10.1081/jdi-120006780
- Said SA, El-Agamy DS. Prevention of sodium valproate-induced hepatotoxicity by curcumin, rosiglitazone and N-acetylcysteine in rats. Arzneimittelforschung. 2010;60(11):647-53. doi: 10.1055/s-0031-1296342
- Howard RJ, Blake DR, Pall H, Williams A, Green ID. Allopurinol/N-acetylcysteine for carbon monoxide poisoning. Lancet. 1987 Sep 12;2(8559):628-9. doi: 10.1016/s0140-6736(87)93018-2
- Manthripragada AD, Zhou EH, Budnitz DS, Lovegrove MC, Willy ME. Characterization of acetaminophen overdose-related emergency department visits and hospitalizations in the United States. Pharmacoepidemiol Drug Saf. 2011 Aug;20(8):819-26. doi: 10.1002/pds.2090
- Hodgman MJ, Garrard AR. A review of acetaminophen poisoning. Crit Care Clin. 2012 Oct;28(4):499-516. doi: 10.1016/j.ccc.2012.07.006
- Green JL, Heard KJ, Reynolds KM, Albert D. Oral and Intravenous Acetylcysteine for Treatment of Acetaminophen Toxicity: A Systematic Review and Meta-analysis. West J Emerg Med. 2013 May;14(3):218-26. doi: 10.5811/westjem.2012.4.6885
- Keays R, Harrison PM, Wendon JA, Forbes A, Gove C, Alexander GJ, Williams R. Intravenous acetylcysteine in paracetamol induced fulminant hepatic failure: a prospective controlled trial. BMJ. 1991 Oct 26;303(6809):1026-9. doi: 10.1136/bmj.303.6809.1026
- Remington R, Lortie JJ, Hoffmann H, Page R, Morrell C, Shea TB. A Nutritional Formulation for Cognitive Performance in Mild Cognitive Impairment: A Placebo-Controlled Trial with an Open-Label Extension. J Alzheimers Dis. 2015;48(3):591-5. https://content.iospress.com/articles/journal-of-alzheimers-disease/jad150057
- Chan, A., Remington, R., Kotyla, E. et al. A vitamin/nutriceutical formulation improves memory and cognitive performance in community-dwelling adults without dementia. J Nutr Health Aging 14, 224–230 (2010). https://doi.org/10.1007/s12603-010-0054-5
- Remington R, Bechtel C, Larsen D, Samar A, Doshanjh L, Fishman P, Luo Y, Smyers K, Page R, Morrell C, Shea TB. A Phase II Randomized Clinical Trial of a Nutritional Formulation for Cognition and Mood in Alzheimer’s Disease. J Alzheimers Dis. 2015;45(2):395-405. https://content.iospress.com/articles/journal-of-alzheimers-disease/jad142499
- Adair JC, Knoefel JE, Morgan N. Controlled trial of N-acetylcysteine for patients with probable Alzheimer’s disease. Neurology. 2001 Oct 23;57(8):1515-7. doi: 10.1212/wnl.57.8.1515
- Magalhães PV, Dean O, Andreazza AC, Berk M, Kapczinski F. Antioxidant treatments for schizophrenia. Cochrane Database Syst Rev. 2016 Feb 5;2:CD008919. doi: 10.1002/14651858.CD008919.pub2
- Dean OM, Bush AI, Copolov DL, Kohlmann K, Jeavons S, Schapkaitz I, Anderson-Hunt M, Berk M. Effects of N-acetyl cysteine on cognitive function in bipolar disorder. Psychiatry Clin Neurosci. 2012 Oct;66(6):514-7. doi: 10.1111/j.1440-1819.2012.02392.x
- Jackson IM, Barnes J, Cooksey P. Efficacy and tolerability of oral acetylcysteine (Fabrol) in chronic bronchitis: a double-blind placebo controlled study. J Int Med Res 1984;12:198-206.
- Hida W. Shindo C, Satoh J, et al. N-acetylcysteine inhibits loss of diaphragm function in streptozotocin-treated rats. Am J Respir Crit Care Med 1996;153:1875-1879.
- Behr J, Maier K, Degenkolb B, et al. Antioxidative and clinical effects of high-dose N-acetylcysteine in fibrosing alveolitis. Adjunctive therapy to maintenance immunosuppression. Am J Respir Crit Care Med 1997;156:1897-1901.
- British Thoracic Society Research Committee. Oral N-acetylcysteine and exacerbation rates in patients with chronic bronchitis and severe airways obstructions. Thorax 1985;40:832-835.
- Wu J, Levy M, Black PH. 2-Mercaptoethanol and n-acetylcysteine enhance T cell colony formation in AIDS and ARC. Clin Exp Immunol 1989;77:7-10.
- Breithaupt TB, Vazquez A, Baez I, Eylar EH. The suppression of T cell function and NF (kappa) B expression byserine protease inhibitors is blocked by N-acetylcysteine. Cell Immunol 1996;173:1323-1329.
- Akerlund B, Jarstrand C, Lindeke B, et al. Effect of N-acetylcysteine (NAC) treatment on HIV-1 infection: a double-blind placebo-controlled trial. Eur J Clin Pharmacol 1996;50:457-461.
- De Flora S, Cesarone CF, Izzotti A, et al. N-acetylcysteine as antimutagen and anticarcinogen. Toxicol Lett 1992;53:Abstract W4/L2.
- De Flora S, Rossi GA, De Flora A. Metabolic, desmutagenic and anticarcinogenic effects of N-acetylcysteine. Respiration 1986;50:S43-S49.
- De Flora S, D’ Agostini F, Masiello L, et al. Synergism between N-acetylcysteine and doxorubicin in the prevention of tumorigenicity and metastasis in murine models. Int J Cancer 1996;67:842-848.
- Redondo P, Badres E, Solano T, et al. Vascular endothelial growth factor (VEGF) and melanoma. N-acetylcysteinedownregulates VEGF production in vitro. Cytokine 2000;12:374-378.
- Chiao JW, Chung F, Krzeminski J, et al. Modulation of growth of human prostate cancer cells by the N-acetylcysteine conjugate of phenethyl isothiocyanate. Int J Oncol 2000;16:1215-1219.
- Arora-Kuruganti P, Lucchesi PA, Wurster RD. Proliferation of cultured human astrocytoma cells in response to anoxidant and antioxidant. J Neurooncol 1999;44:213-221.
- Wiklund O, Fager G, Andersson A, et al. N-acetylcysteine treatment lowers plasma homocysteine but not serum lipoprotein(a) levels. Atherosclerosis1996;119:99-106.
- Gavish D, Breslow JL. Lipoprotein(a) reduction by N-acetylcysteine. Lancet 1991;337:203-204.
- Ceconi C, Curello S, Cargnoni A, et al. The role of glutathione status in the protection against ischaemic and reperfusion damage: effects of N-acetyl cysteine. J Mol Cell Cardiol 1988;20:5-13.
- Chirkov YY, Horowitz JD. N-Acetylcysteine potentiates nitroglycerin-induced reversal of platelet aggregation. J Cardiovasc Pharmacol 1996;28:375-380.
- Zimet I. Acetylcysteine: A drug that is much more than a mucokinetic. Biomed & Pharmacother 1988;42:513-520.
- Klein-Schwartz W, Oderda GM. Adsorption of oral antidotes for acetaminophen poisoning (methionine and N-acetylcysteine) by activated charcoal. Clin Toxicol 1981;18:283-290.
- Horowitz JD, Henry CA, Syrjanen ML, Louis WJ, Fish RD, Antman EM, Smith TW. Nitroglycerine/N-acetylcysteine in the management of unstable angina pectoris. Eur Heart J. 1988 Jan;9 Suppl A:95-100. doi: 10.1093/eurheartj/9.suppl_a.95
- Ardissino D, Merlini PA, Savonitto S, Demicheli G, Zanini P, Bertocchi F, Falcone C, Ghio S, Marinoni G, Montemartini C, Mussini A. Effect of transdermal nitroglycerin or N-acetylcysteine, or both, in the long-term treatment of unstable angina pectoris. J Am Coll Cardiol. 1997 Apr;29(5):941-7. doi: 10.1016/s0735-1097(97)00005-3
- Kerr F, Dawson A, Whyte IM, Buckley N, Murray L, Graudins A, Chan B, Trudinger B. The Australasian Clinical Toxicology Investigators Collaboration randomized trial of different loading infusion rates of N-acetylcysteine. Ann Emerg Med. 2005 Apr;45(4):402-8. doi: 10.1016/j.annemergmed.2004.08.040
- Tenenbein M. Hypersensitivity-like reactions to N-acetylcysteine. Vet Hum Toxicol 1984;26:S3-S5.
- Waring WS, Stephen AF, Robinson OD, Dow MA, Pettie JM. Lower incidence of anaphylactoid reactions to N-acetylcysteine in patients with high acetaminophen concentrations after overdose. Clin Toxicol (Phila). 2008 Jul;46(6):496-500. doi: 10.1080/15563650701864760
- Jepsen S, Hansen AB. The influence of N-acetylcysteine on the measurement of prothrombin time and activated partial thromboplastin time in healthy subjects. Scand J Clin Lab Invest. 1994 Nov;54(7):543-7. doi: 10.3109/00365519409088566
- Poon R, Hinberg I, Peterson RG. N-acetylcysteine causes false-positive ketone results with urinary dipsticks. Clin Chem. 1990 May;36(5):818-9.
- Yip L, Dart RC. A 20-hour treatment for acute acetaminophen overdose. N Engl J Med. 2003 Jun 12;348(24):2471-2. doi: 10.1056/NEJM200306123482422
- Threlkeld DS, ed. Drug Facts and Comparisons. St Louis, Missouri: Facts and Comparisons;1997:1090-1094.
- Hayes BD, Klein-Schwartz W, Doyon S. Frequency of medication errors with intravenous acetylcysteine for acetaminophen overdose. Ann Pharmacother. 2008 Jun;42(6):766-70. doi: 10.1345/aph.1K685
- Mahmoudi GA, Astaraki P, Mohtashami AZ, Ahadi M. N-acetylcysteine overdose after acetaminophen poisoning. Int Med Case Rep J. 2015 Feb 27;8:65-9. doi: 10.2147/IMCRJ.S74563
- Srinivasan V, Corwin D, Verceles AC. An accidental overdose of N-acetylcysteine during treatment for acetaminophen toxicity. Clin Toxicol (Phila). 2015 Jun;53(5):500. doi: 10.3109/15563650.2015.1033629
- Heard K, Schaeffer TH. Massive acetylcysteine overdose associated with cerebral edema and seizures. Clin Toxicol (Phila). 2011 Jun;49(5):423-5. doi: 10.3109/15563650.2011.583664