What is nephrosclerosis
Nephrosclerosis is a progressive kidney disease that results from sclerosis (hardening) of the small blood vessels in the kidneys. Nephrosclerosis is most commonly associated with hypertension (hypertensive nephrosclerosis) or diabetes and can lead to kidney failure. Hypertensive nephrosclerosis is defined as chronic kidney disease caused by non-malignant hypertension. Hypertensive nephrosclerosis is the second most common cause of end-stage renal disease (ESRD), but its pathophysiology is poorly understood. Hypertensive nephrosclerosis should be seen as a process with two principal modes of glomerular sclerosis, ischemic and hypertrophic, with consequent focal segmental glomerulosclerosis, contributing variably to renal failure according to race and level of hypertension.
In a 2015 review, Meyrier 1 cites clinical and experimental evidence that nephrosclerosis, especially in blacks, can be explained by a genetic renovasculopathy that precedes the rise in blood pressure. He argues that the use of the term nephrosclerosis to classify a patient with renal insufficiency leads to the possibility of an overlooked nephropathy complicated by hypertension and to the mistaken belief that drastic blood pressure control may retard progression to end-stage renal disease (ESRD).
Unlike morbidity and mortality of stroke and coronary disease, incident cases of end-stage renal disease (ESRD) attributed to hypertension continue to increase. Some authors suggest that many of these cases are more likely related to other factors, including small-vessel injury related to aging, diabetes, or obesity-related kidney injury.
A couple of important points have been made in different studies. First, in an unselected sample of community-based participants in the Framingham Heart Study, the combination of hypertension and a mild reduction in the glomerular filtration rate (GFR) was found to be an important risk factor for the development of new-onset kidney disease. Other factors noted were diabetes, obesity, smoking, and a low high-density lipoprotein cholesterol level. Second, systolic blood pressure is a strong, independent predictor of a decline in kidney function in older persons with isolated systolic hypertension. This is a significant finding because most cases of uncontrolled hypertension in the United States are due to systolic hypertension in older adults.
Most patients reaching end-stage renal disease (ESRD) from any cause are hypertensive, with nephrosclerosis being the classic finding in end-stage kidneys. Regardless of the etiology, once hypertension develops, a cycle of renal injury, nephrosclerosis, worsening of hypertension, and further renal injury is established. As a result, in a patient presenting with end-stage renal disease (ESRD), determining whether nephrosclerosis is the cause or the consequence of chronic renal injury may be difficult.
Hypertensive nephrosclerosis
Hypertensive nephrosclerosis is the presumed underlying disease in 10-30% of patients with end-stage renal disease worldwide 2, 3. Hypertensive nephrosclerosis typically presents without proteinuria or any abnormalities in the urine sediment. The mechanisms of injury in hypertensive nephrosclerosis are heterogeneous. In areas with preserved arteriolar myogenic responses (i.e., autoregulation), there is ischemic glomerular tuft collapse and interstitial fibrosis. In other areas with impaired autoregulation, the lesions reflect glomerular hypertension leading to podocyte loss and glomerulosclerosis. Apolipoprotein-L1 gene mutations are associated with increased susceptibility to hypertensive nephrosclerosis. The management of hypertensive nephrosclerosis should focus on blood pressure control (target<140/90 mm Hg) using a blocker of the renin-angiotensin system as base therapy.
According to the 2011 US Renal Data System, the annual mortality rate for patients on hemodialysis in the United States is 23.3%. Hypertensive nephrosclerosis accounts for more than one third of patients on hemodialysis.
The term hypertensive nephrosclerosis has traditionally been used to describe a clinical syndrome characterized by long-term essential hypertension, hypertensive retinopathy, left ventricular hypertrophy, minimal proteinuria, and progressive renal insufficiency 4. Most cases are diagnosed based solely on clinical findings. In fact, most of the literature dedicated to hypertensive nephrosclerosis is based on the assumption that progressive renal failure in a patient with long-standing hypertension, moderate proteinuria, and no evidence suggesting an alternative diagnosis characterizes hypertensive nephrosclerosis.
The lack of firm criteria on which to base a histologic diagnosis and the lack of a clear demonstration that hypertension initiates the development of renal failure likely indicate that the true prevalence of hypertensive nephrosclerosis has been overestimated 4. The paradoxical results of increasing incidence of renal failure despite wider antihypertensive drug therapy and reduction in hypertensive target events, such as stroke and cardiovascular disease, raises questions about the causal role of hypertension in hypertensive nephrosclerosis 4.
As reported by Zuccalà and Zucchelli 5, part of the confusion in the classification of hypertensive nephrosclerosis stems from the use of the word nephrosclerosis. Coined almost a century ago by Theodor Fahr, nephrosclerosis literally means “hardening of the kidney.” In the United States and Europe, the terms hypertensive nephrosclerosis, benign nephrosclerosis, and nephroangiosclerosis are commonly used to describe the same clinical condition. These terms refer more to the renal pathologic changes attributed to the effects of hypertension than to the clinical disorder in question 6. Unfortunately, the pathologic changes are not specific to hypertensive renal injury; they are also observed in kidney biopsy specimens of patients who are normotensive, particularly those of advanced age or with diabetes.
The diagnosis of hypertensive nephrosclerosis increases with advancing age. The peak age for the development of end-stage renal disease (ESRD) in white patients is 65 years and older, while the peak age is 45-65 years in black people. In most cases, the diagnosis of hypertensive nephrosclerosis in older patients is made clinically because of the reluctance to perform a renal biopsy in this elderly population 7. Even when a renal biopsy specimen is available, distinguishing vascular lesions due to aging from those due to hypertension may be difficult. In this respect, atheromatous renal vascular disease has been increasingly recognized as a common finding in patients older than 50 years.
Hypertensive nephrosclerosis causes
No specific causes for hypertensive nephrosclerosis are known.
A gene that predisposes to hypertensive renal injury has been identified in rats. To date, however, no specific hypertensive end-stage renal disease (ESRD)-associated gene has been identified in humans. It must be noted that the APOL1 gene variant can increase the risk of renal disease progression in African American hypertensive patients, but the mechanism by which it causes progression of renal disease is unknown and it is unclear whether the gene variant causes hypertension other than by causing renal disease first.
Correct identification of hypertensive nephrosclerosis susceptibility genes requires accurate hypertensive nephrosclerosis phenotyping. The major impediment to establishing a reliable hypertensive nephrosclerosis phenotype is the absence of strong clinical criteria to distinguish hypertensive nephrosclerosis from other renal diseases. Genetic approaches to hypertensive nephrosclerosis require careful scrutiny of clinical diagnoses before assigning phenotypes to study subjects.
Hypertensive nephrosclerosis pathophysiology
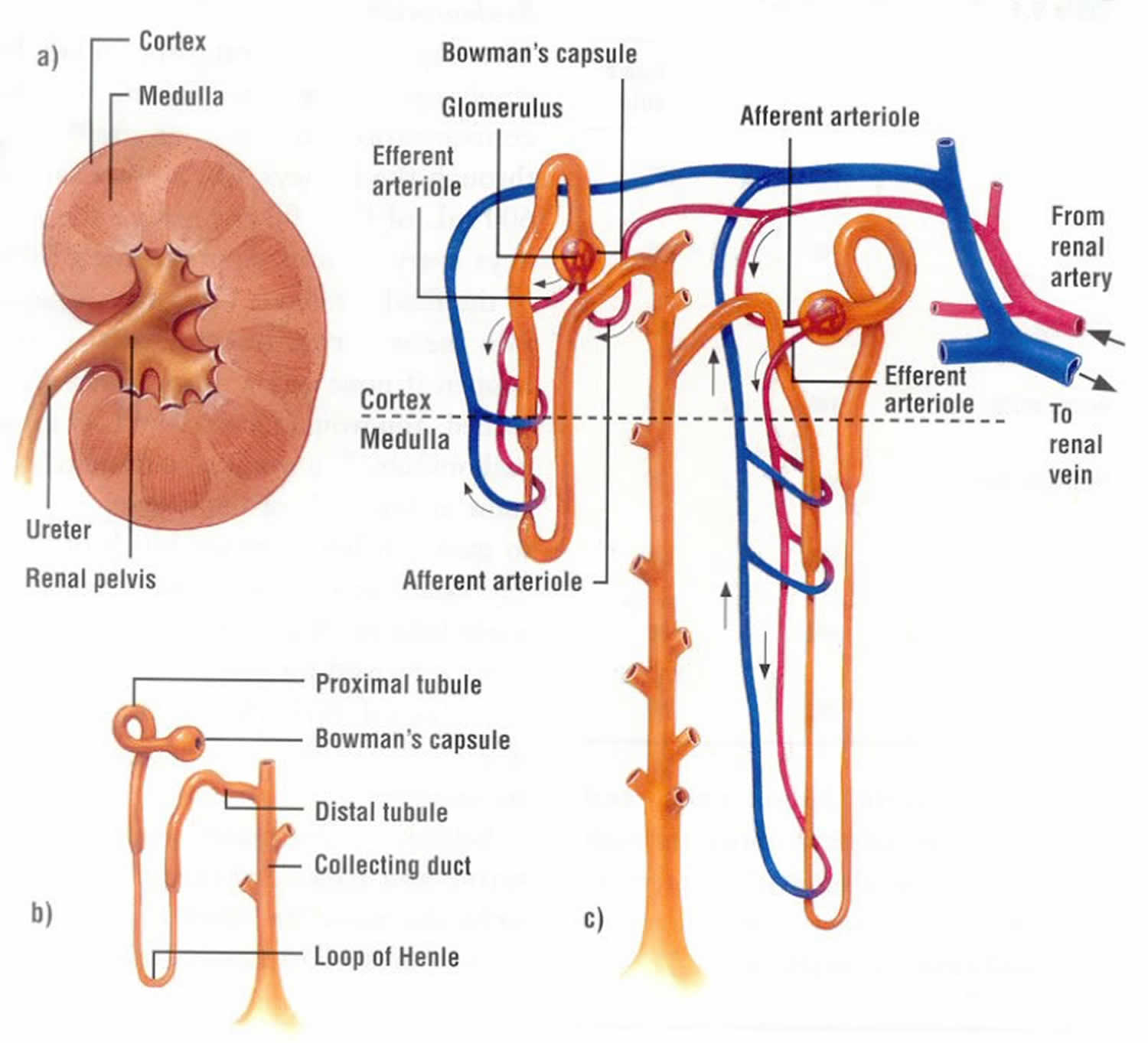
Two pathophysiologic mechanisms have been proposed for the development of hypertensive nephrosclerosis. One mechanism suggests that glomerular ischemia causes hypertensive nephrosclerosis. This occurs as a consequence of chronic hypertension resulting in narrowing of preglomerular arteries and arterioles, with a consequent reduction in glomerular blood flow.
Alternatively, glomerulosclerosis may occur because of glomerular hypertension and glomerular hyperfiltration. According to this theory, hypertension causes some glomeruli to become sclerotic. As an attempt to compensate for the loss of renal function, the remaining nephrons undergo vasodilation of the preglomerular arterioles and experience an increase in renal blood flow and glomerular filtration. The result is glomerular hypertension, glomerular hyperfiltration, and progressive glomerular sclerosis. These mechanisms are not mutually exclusive, and they may operate simultaneously in the kidney.
Furthermore, Tracy and Ishii 8 postulate that nephrosclerosis may not be a single disease entity in the sense of responding to a single etiology, such as hypertension or aging. Rather, nephrosclerosis appears to be multifactorial. It may be, in part, a consequence of fibroplasias in microscopic arteries causing ischemic damage to some nephrons; however, it also may be the end product of a mixture of converging separate pathologic conditions, ie, “second hits,” of which only some are known.
Genetically mediated animal models of hypertension, including the Dahl rat and the spontaneous hypertensive rat, have been used to investigate the role of hypertension in the development of nephrosclerosis. Fundamental differences exist among the strains and between rat and human hypertension. The spontaneous hypertensive rat most closely resembles human essential hypertension. The spontaneous hypertensive rat becomes hypertensive without exposure to salt. Micropuncture studies in hypertensive rats demonstrate an increased preglomerular vasoconstriction that is effective in preventing the development of intraglomerular hypertension. In fact, the spontaneous hypertensive rat develops little renal damage, unless uninephrectomized. In these animals, rigorous blood pressure control does not prevent the development of proteinuria and the pathologic changes of hypertensive nephrosclerosis. The Dahl salt-sensitive rat develops proteinuria before hypertension and before a high-sodium diet is administered.
In patients with primary hypertension, hemodynamic studies frequently show a reduction in renal blood flow. The increased preglomerular vasoconstriction of the afferent arteriole and interlobular artery is thought, at least initially, to exert a protective effect in the glomerulus. With time, sclerosis of the preglomerular vessels causes further reduction in renal blood flow. The GFR is maintained because of increased intraglomerular pressure secondary to efferent arteriolar vasoconstriction and systemic hypertension. Eventually, glomerular ischemia and tubular ischemia develop. Considered together, these data suggest that hypertension precedes and accelerates arteriolar changes in the renal vessels.
Wang et al investigated whether podocyte injury is an important factor in the pathogenesis of hypertensive nephrosclerosis. In a study involving 41 patients with biopsy-proven hypertensive nephrosclerosis, 10 cadaveric kidney donors, and 9 healthy subjects, the authors found that compared with controls, intrarenal messenger ribonucleic acid (mRNA) expression was lower, and urinary mRNA expression was higher, for the podocyte-associated molecules nephrin, podocin, and synaptopodin in patients with hypertensive nephrosclerosis. Moreover, patients with nephrosclerosis had a significantly lower density of glomerular podocytes than did kidney donors (545 +/- 237 vs 773 +/- 296 per glomeruli, respectively) 9.
Genetics
A genetic link for hypertension and related renal failure is supported by studies demonstrating familial clustering of hypertensive nephrosclerosis in black people and, to some extent, in white people.
In the Multiple Risk Factor Intervention Trial (MRFIT), no changes in the reciprocal creatinine slope were observed in white people, but a significant loss in kidney function was observed in black people despite similar levels of blood pressure (BP) control. Similarly, secondary analyses from the Modification of Diet in Renal Diseases (MDRD) study demonstrated that at equivalent mean arterial pressures greater than 98 mm Hg, black patients had a reduction in their GFR at a rate of approximately 1 mL/min/y more than white patients. These observations have led to investigations into genetic factors predisposing to renal damage.
In 2008, 2 separate groups showed strong association between genomic variants within MYH9 (non–muscle myosin heavy chain 9) on 22q and nondiabetic ESRD in African Americans 10. The 2 other disease entities associated with MYH9 included HIV nephropathy and focal segmental glomerulosclerosis (FSGS) in African Americans.
In 2010, 2 other groups showed an even stronger association between the APOL1 gene and risk of end-stage renal disease (ESRD) in African Americans 11. APOL1, which encodes apolipoprotein L1, is also on 22q and is separated from the MYH9 gene by only 14’000 nucleotides. Two variants of APOL1 that have been associated with increased risk of nephropathy include nonsynonymous coding variants termed G1 (glycine-342 to methionine-384) and in-frame 6bp deletion termed G2. The ApoL1 protein protects against Trypanosoma infection. However, the wild-type ApoL1 protein can be neutralized by Trypanosoma brucei rhodesiense. These 2 gene variants restore immunity to Trypanosoma brucei rhodesiense. As a result, genomic evolution has led to positive selection for APOL1 risk variant.
More recent studies have further shown that nondiabetic carriers of 2 APOL1 variants have a 3-times higher rate of proteinuria and reduced renal function and carriers of 1 or 2 variants are significantly younger at the time of initiation of dialysis.
The African American Study of Kidney disease (AASK) trial evaluated the role of intensive versus standard BP control on progression of kidney disease in 1094 black patients with chronic kidney disease (GFR 20-65 mL/min/SA) 12. The study was done in a trial phase followed by a cohort phase. Overall, no difference was noted in the rate of disease progression in the 2 groups. In the subanalysis, in which patients were stratified based on the degree of proteinuria, patients who had initial urinary protein-to-creatinine ratios of less than 0.22 did not benefit from the intensive BP control, whereas those with urinary protein-to-creatinine ratio of greater than 0.22 benefited from the intensive therapy at the end of the cohort phase. APOL1 and MYH9 nephropathy risk variants have been associated with kidney disease in the African American Study of Kidney disease participants 13.
This genetic predisposition may be the reason why tighter control of blood pressure (BP) in this black population does not slow the progression of kidney disease. Some authors argue that hypertension in this setting is secondary to underlying renal injury 14.
In different populations studied regarding polymorphism in the angiotensin-converting enzyme (ACE) gene, the DD genotype is associated with a higher prevalence of progressive renal disease. This genotype is more common in the black population than the white population. Black people with hypertension also have increased angiotensinogen mutations compared with white people with hypertension. Homozygous D polymorphism is associated with an enhanced pressor response to angiotensin I. In patients with immunoglobulin A nephropathy, homozygous D polymorphism appears to influence the rate of progression of renal diseases and the response to ACE inhibitors; thus, ACE polymorphism could be a modulator for the renal response to injury and the response to treatment in persons with hypertensive nephrosclerosis. Whether these data are also applicable to the black population remains to be determined.
Noting that hypertension-associated ESRD displays familial aggregation in the black population, Fung et al investigated possible links between genetic variations and GFR declines. In a study of 554 black patients, the investigators found evidence that such declines can be predicted by variations in the adrenergic beta-1 (ADRB1) receptor at the Ser49Gly position. The authors also found that GFR decline was significantly smaller in patients who were Gly(49)/Gly(49) (minor allele) homozygotes than in those who were Ser(49) carriers 15.
Hypertensive nephrosclerosis symptoms
Patients may present with hypertension, its complications (eg, heart failure, stroke), and/or symptoms of uremia. In most patients, hypertension is present for many years (usually >10 years), with evidence of periods of accelerated or poorly controlled blood pressure (BP).
Features suggesting the diagnosis of hypertensive nephrosclerosis are as follows:
- Black race
- Hypertensive retinal changes
- Left ventricular hypertrophy
- Long-standing or very severe hypertension
- Proteinuria less than 0.5 g/d
- Hypertension diagnosed prior to the onset of proteinuria
- Hypertension preceding renal dysfunction
- No evidence of another renal disease
- Biopsy findings compatible with the diagnosis
Upon physical examination, evidence of hypertension-related target organ damage includes hypertensive changes in the retinal vessels and signs of left ventricular hypertrophy.
Hemorrhages or exudates are characteristic of accelerated hypertension, and papilledema is a feature of malignant hypertension.
Hypertensive nephrosclerosis diagnosis
Based on Joint National Commission recommendations 16, evaluation of a hypertensive patient has the following three objectives:
- Identifying other cardiovascular risk factors
- Revealing identifiable causes of high blood pressure (BP,)
- Evaluating for evidence of end-organ damage.
A definitive diagnosis of hypertensive nephrosclerosis cannot be made without a renal biopsy, especially in the white patient population. In the absence of a renal biopsy, the diagnosis of hypertensive nephrosclerosis is one of exclusion.
Laboratory evaluation includes the following studies:
- Hematocrit
- Creatinine (or the estimated glomerular filtration rate [eGFR])
- Serum potassium
- Serum calcium
- Lipid panel
- Blood glucose
- Urinalysis
- Urinary albumin-to-creatinine ratio
In a large series of patients, most had urine protein excretion of lower than 1 g/d; however, in some patients with biopsy-proven hypertensive nephrosclerosis, a 24-hour urinary protein excretion greater than 1 g/d has been described. When secondary changes of focal segmental glomerulosclerosis related to hyperfiltration develop, proteinuria can increase to the nephrotic range.
Innes et al 17 reviewed 185 cases of patients with renal biopsy specimens that were classified solely as hypertensive nephrosclerosis. In 40% of these patients, urinary protein excretion was greater than 1.5 g/d, with 22% excreting more than 3 g/d and 18% having serum albumin values less than 3 g/dL. Similar findings were reported by Harvey et al 18. Freedman et al 19 questioned these findings because many biopsy specimens showed segmental and diffuse glomerulosclerosis. Harvey et al 18 attributed these lesions to the effect of hypertension, but Freedman et al believed that these patients had idiopathic focal segmental glomerulosclerosis, not hypertensive nephrosclerosis.
The contrasting conclusions of Harvey et al 18 and Freedman et al 19 highlight the problems of distinguishing hypertensive nephrosclerosis from primary glomerular disease purely on clinical grounds. Nevertheless, in black people who are hypertensive, do not have diabetes, and have mild-to-moderate renal failure and proteinuria less than 2 g/day, renal biopsy specimens are likely to show morphological lesions consistent with the clinical diagnosis of hypertensive nephrosclerosis. On the other hand, the diagnosis of hypertensive nephrosclerosis in a young white patient is unusual, and these findings suggest an alternative diagnosis.
Measurement of uric acid may also be valuable for providing prognostic information. A review of data from 45 patients diagnosed with arterial/arteriolar nephrosclerosis concluded that a baseline serum uric acid level of 8.0 mg/dL or higher was significantly associated with a ≥50% decline in eGFR or end-stage renal disease (ESRD) 20.
Imaging Studies
An echocardiogram may be required to assess left ventricular size.
Renal imaging with either an ultrasound or an intravenous pyelogram reveals that kidney size is usually symmetric and may be normal or modestly reduced.
The renal calices and pelves are normal.
Renal asymmetry or irregularities in the contour raise the possibility that hypertension could be secondary to renal artery stenosis or reflux nephropathy.
Other Tests
An electrocardiogram (ECG) typically shows left ventricular hypertrophy; however, this condition may not be evident on the ECG tracings. The sensitivity of ECG in helping to detect left ventricular hypertrophy may be as low as 22%. However, ECG is recommended as part of the initial evaluation of hypertensive patients.
Hypertensive nephrosclerosis treatment
Lifestyle changes such as eating healthy foods, increasing physical activity and maintaining a healthy weight — can help keep your blood pressure low. You may need to continue to take blood pressure medication as well, and any underlying medical condition you have may affect your doctor’s choice of medication.
Possible drug choices include:
- Thiazide diuretics. Diuretics, sometimes called water pills, are medications that act on your kidneys to help your body eliminate sodium and water, reducing blood volume. Thiazide diuretics are often the first — but not the only — choice in high blood pressure medications. These medications are often generic and tend to be less expensive than other high blood pressure medications. If you’re not taking a diuretic and your blood pressure remains high, talk to your doctor about adding one or replacing a drug you currently take with a diuretic. Possible side effects include weakness, leg cramps and a higher risk of sexual dysfunction.
- Beta blockers. These medications reduce the workload on your heart and open your blood vessels, causing your heart to beat slower and with less force. When prescribed alone, beta blockers don’t work as well in black people — but they’re effective when combined with a thiazide diuretic. Possible side effects include fatigue, sleep problems, a slowed heart rate, and cold hands and feet. In addition, beta blockers generally aren’t prescribed for people with asthma, as they can increase muscle spasms in the lungs.
- Angiotensin-converting enzyme (ACE) inhibitors. These medications help relax blood vessels by blocking the formation of a natural chemical that narrows blood vessels. ACE inhibitors may be especially important in treating high blood pressure in people with coronary artery disease, heart failure or kidney failure. Like beta blockers, ACE inhibitors don’t work as well in black people when prescribed alone, but they’re effective when combined with a thiazide diuretic. Possible side effects include dizziness and coughing, and these medications aren’t recommended during pregnancy.
- Angiotensin II receptor blockers. These medications help relax blood vessels by blocking the action — not the formation — of a natural chemical that narrows blood vessels. Like ACE inhibitors, angiotensin II receptor blockers often are useful for people with coronary artery disease, heart failure or kidney failure. These medications have fewer potential side effects than do ACE inhibitors, but are also not used during pregnancy.
- Calcium channel blockers. These medications help relax the muscles of your blood vessels or slow your heart rate. Calcium channel blockers may work better for some people than ACE inhibitors or beta blockers alone. Possible side effects include water retention, dizziness and constipation. Grapefruit juice interacts with some calcium channel blockers, increasing blood levels of the medication and putting you at higher risk of side effects. Ask your doctor or pharmacist if your medication is affected by grapefruit juice.
- Direct renin inhibitors. Newer treatments for hypertension include direct renin inhibitors, such as aliskiren (Tekturna™). Aliskiren relaxes and widens the arteries by preventing the action of renin. Renin is the initial enzyme in a cascade of steps in the production of chemicals (angiotensin, aldosterone, others) important in cardiovascular health and disease. The Food and Drug Administration strongly cautions against using aliskiren in combination with ACE inhibitors or angiotensin II receptor blockers in people with diabetes or moderate to severe kidney problems. Common side effects of aliskiren include dizziness and diarrhea.
Treatment can sometimes be complicated. You may need more than one medication combined with lifestyle changes to control your high blood pressure. And your doctor will want to see you more frequently until your blood pressure is stabilized, possibly as frequently as once a month. Your doctor may also recommend that you keep track of your blood pressure at home.
Lifestyle and home remedies
Although lowering hypertension can be difficult, making the same lifestyle changes you would make if you had primary high blood pressure can help.
These include:
- Eat healthy foods. Try the Dietary Approaches to Stop Hypertension (DASH) diet, which emphasizes fruits, vegetables, whole grains and low-fat dairy foods. Get plenty of potassium, which is found in fruits and vegetables such as potatoes, spinach, bananas and apricots, to help prevent and control high blood pressure. Eat less saturated fat and total fat.
- Decrease the salt in your diet. A lower sodium level — 1,500 milligrams (mg) a day — is appropriate for people 51 years of age and older and for people of any age who are black or who have hypertension, diabetes or chronic kidney disease. Otherwise healthy people can aim for 2,300 mg a day or less. While you can reduce the amount of salt you eat by putting down the saltshaker, you should also pay attention to the amount of salt that’s in the processed foods you eat, such as canned soups or frozen dinners.
- Maintain a healthy weight. If you’re overweight, losing even 10 pounds (4.5 kilograms) can lower your blood pressure.
- Increase physical activity. Regular physical activity can help lower your blood pressure and keep your weight under control. Strive for at least 30 minutes of physical activity a day.
- Limit alcohol. Even if you’re healthy, alcohol can raise your blood pressure. If you choose to drink alcohol, do so in moderation — up to one drink a day for women and two drinks a day for men aged 65 or younger. For men and women 65 years old or older, stick to one drink a day.
- Don’t smoke. Tobacco injures blood vessel walls and speeds up the process of hardening of the arteries. If you smoke, ask your doctor to help you quit.
- Manage stress. Reduce stress as much as possible. Practice healthy coping techniques, such as muscle relaxation and deep breathing. Getting plenty of sleep can help, too.
- Meyrier A. Nephrosclerosis: a term in quest of a disease. Nephron. 2015. 129 (4):276-82.
- Jha V., Garcia-Garcia G., Iseki K. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:260–272.
- United States Renal Data System, 2014 Annual Data Report: Epidemiology of Kidney Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2014
- Nephrosclerosis. https://emedicine.medscape.com/article/244342-overview
- Zuccalà A, Zucchelli P. Is nephroangiosclerosis a hypertension-induced nephropathy?. Contrib Nephrol. 1996. 119:110-4.
- Rule AD, Amer H, Cornell LD, Taler SJ, Cosio FG, Kremers WK, et al. The association between age and nephrosclerosis on renal biopsy among healthy adults. Ann Intern Med. 2010 May 4. 152(9):561-7.
- Moutzouris DA, Herlitz L, Appel GB, et al. Renal biopsy in the very elderly. Clin J Am Soc Nephrol. 2009 Jun. 4(6):1073-82.
- Tracy RE, Ishii T. What is ‘nephrosclerosis’? lessons from the US, Japan, and Mexico. Nephrol Dial Transplant. 2000 Sep. 15(9):1357-66.
- Wang G, Kwan BC, Lai FM, et al. Intrarenal expression of miRNAs in patients with hypertensive nephrosclerosis. Am J Hypertens. 2010 Jan. 23(1):78-84.
- Kao WH, Klag MJ, Meoni LA, Reich D, Berthier-Schaad Y, Li M, et al. MYH9 is associated with nondiabetic end-stage renal disease in African Americans. Nat Genet. 2008 Oct. 40(10):1185-92
- Freedman BI, Sedor JR. Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med. 2010 Dec 23. 363(26):2565; author reply 2565-6.
- Kopp JB, Smith MW, Nelson GW, Johnson RC, Freedman BI, Bowden DW, et al. MYH9 is a major-effect risk gene for focal segmental glomerulosclerosis. Nat Genet. 2008 Oct. 40(10):1175-84.
- Appel LJ, Wright JT Jr, Greene T, Agodoa LY, Astor BC, Bakris GL, et al. Intensive blood-pressure control in hypertensive chronic kidney disease. N Engl J Med. 2010 Sep 2. 363(10):918-29.
- Freedman BI, Murea M. Target organ damage in African American hypertension: role of APOL1. Curr Hypertens Rep. 2012 Feb. 14(1):21-8.
- Fung MM, Chen Y, Lipkowitz MS, et al. Adrenergic beta-1 receptor genetic variation predicts longitudinal rate of GFR decline in hypertensive nephrosclerosis. Nephrol Dial Transplant. 2009 Dec. 24(12):3677-86.
- Wheatley K, Ives N, Gray R, Kalra PA, Moss JG, Baigent C, et al. Revascularization versus medical therapy for renal-artery stenosis. N Engl J Med. 2009 Nov 12. 361(20):1953-62.
- Innes A, Johnston PA, Morgan AG, et al. Clinical features of benign hypertensive nephrosclerosis at time of renal biopsy. Q J Med. 1993 Apr. 86(4):271-5.
- Harvey JM, Howie AJ, Lee SJ, et al. Renal biopsy findings in hypertensive patients with proteinuria. Lancet. 1992 Dec 12. 340(8833):1435-6.
- Freedman BI, Iskander SS, Buckalew VM Jr, et al. Renal biopsy findings in presumed hypertensive nephrosclerosis. Am J Nephrol. 1994. 14(2):90-4.
- Momoki K, Kataoka H, Moriyama T, Mochizuki T, Nitta K. Hyperuricemia as a Predictive Marker for Progression of Nephrosclerosis: Clinical Assessment of Prognostic Factors in Biopsy-Proven Arterial/Arteriolar Nephrosclerosis. J Atheroscler Thromb. 2017 Jun 1. 24 (6):630-642.