What is a nerve block
A nerve block relieves pain by injecting a substance, such as local anesthetic, alcohol or phenol, into or around a nerve or into the spine, which interrupts or “turn off” how pain signals are sent to your brain. Doctors can also deaden a nerve with a probe that generates intense heat (radiofrequency denervation or ablation) or intense cold (cryoanalgesia). Imaging guidance may be used to place the needle in the most appropriate location for maximum benefit. A nerve block may allow a damaged nerve time to heal, provide temporary pain relief and help identify a more specific cause of pain.
Typically, the effects of a nerve block injection are temporary and offer little to no long-term relief. Each individual is different; however, nerve block injections are often delivered in a series and then discontinued, depending on the results they achieve. A patient may feel benefits after a round of injections, or none at all despite delivery of the medication to the correct spot. If the nerve blocks don’t help ease your pain, however, your doctor will most likely recommend a different treatment approach.
Nerve blocks are used to diagnose the causes of pain. Nerve blocks are also used to treat chronic pain when drugs or other treatments cause bad side effects or do not control pain. A test block is usually performed with local anesthetic. If you achieve good pain relief from the local anesthetic, your doctor may inject a nerve block, such as alcohol or phenol.
This procedure requires little to no special preparation. Tell your doctor if there’s a possibility you are pregnant. Wear loose, comfortable clothing and leave jewelry at home. You may be asked to wear a gown.
Nerve blocks may be used for several purposes, such as:
- To determine the source of pain.
- To treat painful conditions.
- To predict how pain will respond to long-term treatments.
- For short-term pain relief after some surgeries and other procedures.
- For anesthesia during some smaller procedures, such as finger surgery.
Nerve blocks often relieve pain. Nerve blocks work well for some types of cancer pain, such as pain from cancer in organs such as the pancreas 1.
A nerve block may cause temporary muscle paralysis or a loss of all feeling in the affected area or in the surrounding area.
Although peripheral nerve blocks are overall safe when performed correctly, there are rare but serious risks associated with them. Risks include block failure, bleeding, infection, damage to surrounding structures, permanent nerve injury, and intravascular uptake of local anesthetic resulting in systemic toxicity. Contraindications include an inability to cooperate with placement (sometimes seen in pediatric patients, combative patients, or those with severe dementia), pre-existent neurologic deficit, systemic or active local infection at the site of the block, body habitus or obesity obscuring optimal ultrasonographic visualization. Relative contraindications include the presence of bleeding disorder.
A peripheral nerve block can be used for most people, usually giving a safe and effective form of pain relief both during and after the operation.
How long does a nerve block last?
Nerve blocks numb the nerves touched by the drugs. This relieves pain by interrupting the pain signal sent by the nerves to your brain. Depending on the type of nerve block, your pain may be numbed for a short time or a long time.
Nerve blocks for chronic pain may work for 6 to 12 months. They may have to be repeated.
Peripheral nerve block
A peripheral nerve block is a type of regional anesthetic that involves injecting local anesthetics and other painkillers near the major nerves to your arm or leg. A nerve block works by temporarily numbing your nerves to give pain relief.
A nerve block can be used instead of a general anesthetic for the operation, and is also an effective form of pain relief afterwards.
A peripheral upper or lower limb nerve block can be used for most people, usually giving a safe and effective form of pain relief both during and after the operation.
The purpose of peripheral nerve blocks is to inhibit impulse transmission distally in a nerve terminal, thus terminating the pain signal perceived by the cerebral cortex (brain) 2. Nerve blocks can be used to treat acute pain (e.g., procedural anesthesia and perioperative analgesia), as well as for diagnosis and treatment of chronic pain. Impulse blockade can be brief (hours) or prolonged (months), depending on the medication used in the block and the technique (e.g., single shot block versus catheter). Nerve blocks are also useful in the emergency department for the following indications: Acute pain management of the extremities 3.
- Anesthesia of the extremity for procedures
- Alternative to procedural sedation
- Alternative to narcotics in certain patient populations (e.g., a head injury patient, patients with concomitant mental status change, patients given buprenorphine)
Peripheral nerve blocks offer many advantages to traditional anesthetic and analgesic techniques. Patients who would otherwise have excessive risks with general anesthesia can safely undergo surgery painlessly with regional anesthesia. Additionally, the side effects of perioperative opioid analgesia can be minimized or avoided entirely while still providing superior pain control. If the goal is prolonged blockade, peripheral nerve catheters can remain for several days to provide more extended analgesia than a single-shot block alone.
Many nerves can be blocked depending on the injury. These include the following upper or lower extremities:
- Brachial plexus roots at the interscalene location block the shoulder, upper arm, elbow, and forearm
- Brachial plexus trunks at the supraclavicular location block the upper arm, elbow, wrist, and hand
- Brachial plexus cords at the infraclavicular location block the upper arm, elbow, wrist, and hand
- Brachial plexus branches at the axillary location block the forearm, wrist, hand, and elbow including the musculocutaneous nerve
- Median nerve at the elbow blocks the hand and forearm
- The radial nerve at the elbow blocks the hand and forearm
- Ulnar nerve at the elbow blocks the hand and forearm
- The femoral nerve at the femoral crease blocks the anterior thigh, femur, knee, and skin anesthesia over the medial aspect of the leg below the knee
- The sciatic nerve at the subgluteal location or anterior approach below the femoral crease blocks the posterior aspect of the thigh, and anterior, lateral, and posterior lower leg, ankle, and foot
- The sciatic nerve at the popliteal location blocks the anterior, lateral, and posterior lower leg, ankle, and foot
- Ankle block of five separate nerves to the ankle and foot (saphenous nerve, deep peroneal nerve, superficial peroneal nerve, posterior tibial nerve, and sural nerve) blocks the entire foot
The technique for peripheral nerve blocks is based on the type of block. A quick summary of some of the more common blocks is listed below.
- Interscalene block: anesthetizes nerve roots from the cervical plexus (C3, C4, supraclavicular nerve), and upper and middle trunks of the brachial plexus (C5-C7). For positioning patient is placed in a supine position with head turned away from the side of the block. Sternal notch, the sternal and clavicular heads of the sternocleidomastoid muscle, and clavicle are identified and marked. If using ultrasound probe is placed in a transverse position with its long axis across the neck just above the clavicle. The carotid artery and internal jugular vein are visualized. Subclavian artery is identified by directing the beam towards the first rib. Nerves are then traced cephalad. At the C6 nerves of the brachial plexus are visualized in a vertical orientation within the interscalene groove. A needle is then placed in-plane or out-of-plane and directed toward the nerves. A needle tip is placed next to the nerve roots. A total of 12 cc to 30 cc of local anesthetic is injected
- Supraclavicular block: the patient is placed in the supine position with arms by the sides, and head turned away from the side of the block. The probe is placed in a transverse position just above the clavicle using ultrasound. The carotid artery and internal jugular vein are visualized. The needle is inserted in-plane (parallel to the probe), and a local anesthetic is injected to hydro dissect between the nerves until the tip reaches an area bordered by the first rib, subclavian artery, and brachial plexus. 20 cc to 30 cc of local anesthetic is injected. Before injection, however, aspiration should be performed to ensure there is no blood
- Infraclavicular block: the patient is placed in the supine position with the head turned away from the side of the block. The arm is abducted with the elbow flexed to identify the coracoid process. The axillary artery is identified, and the cords of the brachial plexus are visualized adjacent to the artery using ultrasound. The needle is placed adjacent to the axillary artery in the cranio-posterior quadrant, and 30-40 cc of local anesthetic is administered. Before injection, however, aspiration should be performed to ensure there is no blood
- Axillary block: block anesthetizes nerves of the brachial plexus at the level of the individual nerves and often requires multiple injections. The patient is positioned supine with the arm abducted 90 degrees and the elbow is flexed. The transducer is placed transversely in the axilla using ultrasound. The needle is introduced perpendicular to the skin and advanced until the tip is next to each nerve
- Intercostobrachial block: the patient is positioned supine with the arm abducted to expose the axillary fossa. The intercostobrachial nerve runs in the subcutaneous tissue of the medial upper arm. The needle is advanced subcutaneously across the medial aspect of the arm while injecting 5 cc to 10 cc of local anesthetic
- Radial nerve block: radial nerve emerges between the brachioradialis tendon and the radius just proximal to the styloid process. The needle is inserted subcutaneously just proximal to the styloid process of the radius, aiming medially and 3 cc to 5cc of local anesthetic is injected
- Median nerve block: median nerve is located between the tendons of the flexor palmaris longus and the flexor carpi radialis. The need is inserted between the two tendons until it penetrates the fascia and advanced until contact is made with bone. The needle should be redirected and local anesthetic injected in lateral and medial directions
- Ulnar nerve block: ulnar nerve runs between the ulnar artery and flexor carpi ulnaris tendon. The tendon is just superficial to the ulnar nerve. A needle is placed under the tendon close to its attachment just above the styloid process of the ulna and advanced 5 mm to 10 mm, and 3 cc to 5 cc of local anesthetic is injected at this location
- Lumbar plexus block: Patient is placed in the lateral decubitus position operative side up with the leg flexed at the hip and knee. Using the ultrasound probe, it is placed longitudinally adjacent to the spine at the second to third lumbar level. The needle is inserted at the cephalad edge using the in-plane technique. The length of the needle should be seen as it approaches the target structure which the posterior third of the psoas major muscle.
- Femoral nerve block: Patient is placed in a supine position. Using ultrasound the nerve is visualized which is lateral to the artery. An in-plane or out-of-plane approach can be used where the needle is inserted, and the tip is placed adjacent to the nerve, and 20 cc to 50 cc of local anesthetic is injected in 5 cc increments. Before injection, however, aspiration should be performed to ensure there is no blood.
- Fascia iliaca block: the patient is placed in a supine position where using ultrasound the probe is placed transversely to the leg at the junction of the middle and lateral thirds (between the ASIS and pubic tubercle) to identify the fascia lata, iliacus muscle, and fascia iliaca. The needle is introduced in-plane inferior to the inguinal ligament and guided beneath the fascia iliaca, and 30 cc of local anesthetic is injected in 5 cc increments. Before injection, however, aspiration should be performed to ensure there is no blood
- Obturator nerve block: the patient is placed in the supine position with the leg externally rotated. Using an ultrasound probe, it is placed in the inguinal crease, and the femoral vein is identified. The probe is then moved medially to visualize the pectineus and adductor longus muscles. The needle is inserted inplane or out of plane and is directed to the fascial plane between the adductor brevis and magnus, and 5 cc to 10 cc of local anesthetic is injected. Before injection, however, aspiration should be performed to ensure there is no blood
- Sciatic nerve block: can be approached anteriorly or posteriorly. For the posterior approach, the patient is placed in the lateral decubitus position with the hip flexed at 45 degrees and the knee at 90 degrees. In the anterior approach, the patient is positioned in the same manner. Using an ultrasound probe, it is held transverse to the course of the nerve. The nerve is found lateral to the ischial tuberosity and deep to the gluteus maximus muscle. The needle is inserted in-plane from the lateral aspect of the transducer and positioned with the tip of the needle adjacent to the nerve. Approximately 20 cc of local anesthetic is injected in 5 cc increments with gentle aspirations between injections. Before injection, however, aspiration should be performed to ensure there is no blood
- Popliteal nerve block: the patient can be placed in either prone, lateral decubitus, or supine. There are two approaches. For the posterior approach, the biceps femoris and semitendinosus/semimembranosus tendons are palpated. The ultrasound probe is placed transverse to the thigh and in the popliteal crease. The popliteal artery is used as the landmark, and the tibial nerve is found superficial and lateral to the popliteal artery. The nerve is then followed cephalad to the point where the common fibular nerve joins the tibial nerve from the lateral side to form the sciatic nerve. The sciatic nerve is blocked proximal to this to ensure that both the common fibular and tibial nerves are anesthetized
- Saphenous nerve block: the patient is positioned supine with the leg straight. Using the ultrasound probe, it is placed perpendicularly to the thigh at the midpoint between the anterior superior iliac spine and the distal end of the femur. The nerve is identified as it exits from the adductor canal adjacent to the femoral artery. As it is followed distally, it becomes more superficial traveling with an arterial branch just deep to the sartorius muscle. Using an in-plane approach ten cc of local anesthetic is injected deep to the sartorius muscle at the lateral border of the artery.
Nerve block procedure
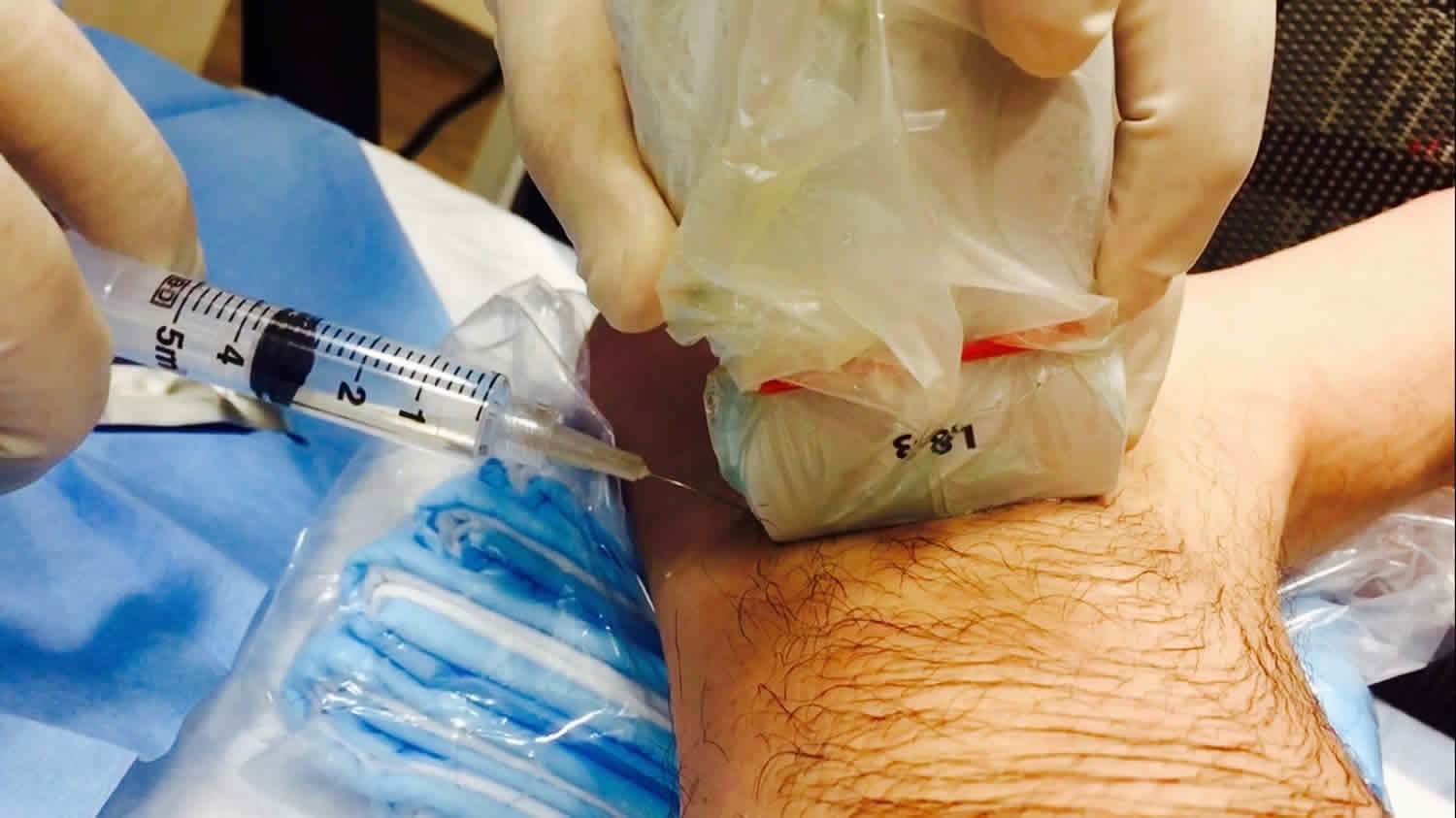
Your anesthetist will usually use an ultrasound scanner and nerve stimulator to help guide them where to inject the anesthetic.
Your anesthetist will insert the needle and when they are certain that it is in the right position they will inject anesthetic through it. Sometimes your anesthetist may insert a small tube through the needle before they remove it, leaving the tube in place so they can inject more anesthetic.
Nerve block for arm
- A nerve block for your arm can be used on its own while you are awake, with sedation, or with a general anesthetic.
- Depending on your operation, the injection may be given in the side of your neck, or near your collarbone or armpit, or in your elbow, forearm or wrist.
Nerve block for leg
- A nerve block for your leg can be used on its own while you are awake, with sedation, or with a spinal anesthetic or general anesthetic.
- Operations on lower limbs are usually performed under a general anesthetic or spinal anesthetic. A nerve block is usually used in addition to give pain relief afterwards. Depending on the operation, the injection may be given behind your thigh or knee, in your ankle or foot, or near your groin.
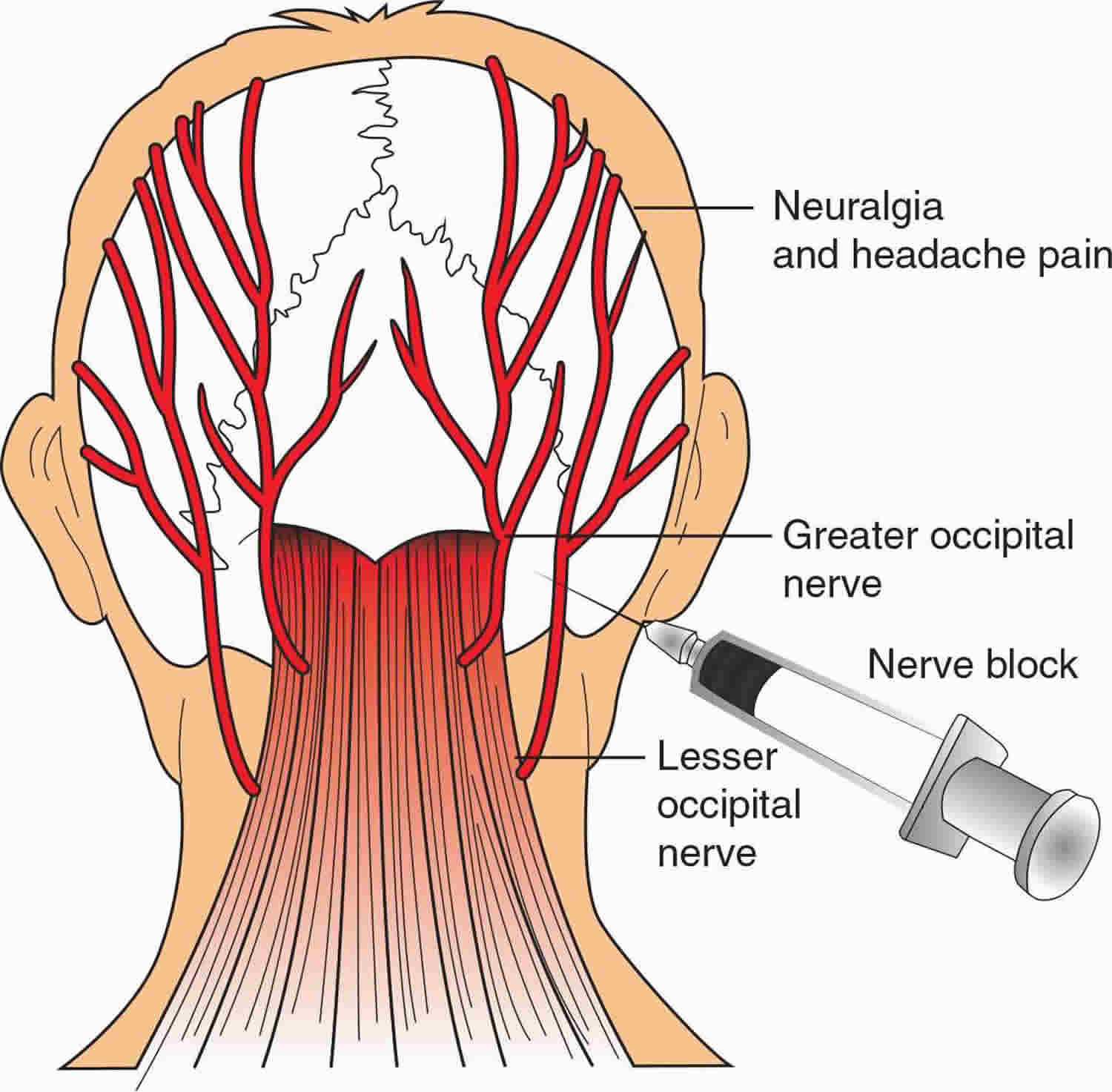
Occipital nerve block
Occipital nerve anatomy 4
- Greater occipital nerve: Arises from C2 dorsal ramus. It then passes medial to lower border of obliquus capitis inferior muscle and crosses the suboccipital triangle. It then runs rostral along the rectus capitis posterior major muscle; innervates and pierces the semispinalis capitis muscle; pierces tendon of the trapezius muscle; passes superior nuchal line of the occipital bone; and courses toward the apex of the scalp in proximity to the occipital artery, possibly up to the coronal suture.
- Lesser occipital nerve: Arises from C2 ventral ramus; loops inferior to the spinal accessory nerve; ascends along the posterior border of the sternocleidomastoid muscle; pierces deep cervical fascia and runs across the posterior edge of the sternocleidomastoid insertion and on into the superficial fascia of the scalp; splits into 3 branches: auricular, mastoid, and occipital.
- Third occipital nerve: Arises from the dorsal ramus of C3. This divides into lateral and medial branches; then the medial branch gives rise to superficial and deep branches, the superficial branch being the third occipital nerve, then curves around the dorsolateral surfaces of C2-C3 and travels along semispinalis capitis muscle. It turns dorsally at C2 spinous process, piercing semispinalis capitis, splenius capitis, and trapezius muscles and exits muscles and innervates small cutaneous area right below the nuchal line. Of importance, the third occipital nerve sends many branches to the greater occipital nerve and lesser occipital nerve which can make it difficult to separate symptoms due to the third occipital nerve alone 5.
Greater occipital nerve blocks are frequently used to treat migraine headaches and recent large retrospective cohort study have shown greater occipital nerve block seems to be an effective option for acute management of migraine headache, with promising reductions in pain scores 6. These results were consistent regardless of sex, age, prior treatments, single or multiple greater occipital nerve blocks, or specialty performing the procedure. Few side effects were reported in the period immediately following the procedure: 10 patients developed vasovagal symptoms that responded to conservative treatment measures, and 25 patients described “burning” at the injection site. No reports of lasting complications or side effects were found within the follow-up visit documentation.
Figure 1. Greater occipital nerve block
Intercostal nerve block
Intercostal nerve blocks are simple to perform and useful for pain management either as the primary intervention or as adjuncts. Intercostal nerve blocks are useful for pain in the chest wall and upper abdomen 7. Intercostal nerve blocks provide a reliable unilateral dermatomal band of analgesia for the vertebral level at which they are performed. Intercostal nerve blocks have been shown to reliably improve respiratory function in patients with chest wall pain making them useful for recovery after thoracic surgery. Intercostal nerve blocks are technically easier to perform than a paravertebral nerve block or epidural but risk increased vascular uptake of local anesthetic and systemic toxicity as well as pneumothorax. A potential disadvantage compared to paravertebral nerve block or thoracic epidural is the necessity for several blocks to be performed if more than one level or bilateral coverage is required. Intercostal nerve blocks do not provide complete surgical analgesia for thoracic surgery so they must be part of a multi-modal plan if they are to be used for intraoperative analgesia 8.
There are 12 intercostal nerves which supply the sensory innervation for much of the back, trunk, and upper abdomen, as well as, the muscular innervation for the intercostal muscles. Each intercostal nerve originates from spinal nerve roots at the same vertebral level as the rib they travel with. As each spinal nerve emerges from the spinal cord, it immediately divides into dorsal and ventral branches. The dorsal nerve branch supplies the motor and sensory innervation of the paravertebral musculature and overlying skin and subcutaneous tissue. The ventral branch continues anterolaterally and becomes the intercostal nerve. Immediately on exiting the intervertebral foramen the nerve lays between the parietal pleura and the innermost intercostal muscle. Within a few centimeters the nerve dives between the internal and innermost intercostal muscles where it remains until it terminates in the anterior chest wall or abdomen. Each intercostal nerve travels in a neurovascular bundle with an intercostal artery and vein with the nerve laying inferior to both blood vessels. This neurovascular bundle accounts for the high levels of local anesthetic uptake into the blood noted after intercostal nerve blocks. The bundle travels inferior to the accompanying rib in the costal groove. Near the midaxillary line, the intercostal nerve sends an offshoot called the lateral cutaneous branch which travels laterally through the internal and external intercostal muscles where it then divides into a dorsal and ventral branch. Together these innervate the skin and subcutaneous tissue of the lateral trunk and upper abdomen. Just before the individual intercostal nerves terminate, they send another branch called the anterior cutaneous branch which divides into a lateral and medial branch. These supply the skin and subcutaneous tissue of the anterior trunk and abdomen which includes the skin over both the sternum and rectus abdominis 9.
Intercostal nerve block indications
Intercostal nerve block indications include 10:
- Incisional pain from thoracic surgery
- Analgesia for thoracostomy
- Herpes zoster or post-herpetic neuralgia
- Rib fractures 11
- Breast surgery
- Upper abdominal surgery 12
- Differentiating between visceral and somatic pain
Intercostal nerve block contraindications
The only absolute contraindications are patient refusal for the procedure and active infection over the site of injection. Other relative contraindications are an allergy to local anesthetics, prior nerve injury or damage, inability of the patient to consent to procedure, anticoagulation or coagulopathy. Patients should be counseled on the expected results of the intercostal nerve block and pertinent potential complications. Special consideration should also be given if patients have prior nerve injury or neuromuscular disease which involves the area to be blocked.
Intercostal nerve block technique
Successful intercostal nerve block results in the deposition of local anesthetic in the intercostal sulcus outside of the parietal pleura. Correct placement will result in ipsilateral numbness of the individual intercostal levels that have been blocked. It is rare for the blockade to extend to superior or inferior levels unless a large amount of local anesthetic is injected or the needle placed too close to the midline resulting in spread to the paravertebral space. Usually, the block level is determined by the number of blocks performed and is limited to the dermatome of the intercostal nerves which have been targeted.
Anatomic Landmark
After cleansing the skin with an antiseptic, a skin wheal should be performed with 1 to 2 mL of local anesthetic. The fingers of the palpating hand should be used to pull the skin up so that the needle will contact the middle of the rib to be blocked. Generally, a 22-gauge 50-mm long needle is sufficient to perform the block. As the skin is fixed with the palpating hand, the needle is placed through the skin wheal at an approximately 20-degree angle cephalad until it makes contact with the rib, which should be made within 1cm. The palpating hand then allows the skin to return to its normal position as the needle is “walked-off” the inferior border of the rib. As the needle walks off the inferior edge, it should be advanced another 1 to 3 mm anteriorly where a subtle “pop” may be appreciated as the needle advances through the fascia of the internal intercostal muscle. After negative aspiration, 3 to 5 mL of local anesthetic can be injected 13.
Ultrasound Guided
Ultrasound guidance may decrease the chance of intravascular injection, pneumothorax and allows injection closer to the midline than anatomic landmarks. This increases the chance that injection is made before the division of the lateral branch which is necessary to achieve anesthesia of the entire intercostal dermatome.
The individual ribs to be blocked should be marked out as with the landmark technique. The ultrasound probe is then placed in a sagittal plane about 4 cm lateral to the spinous process. The ribs are visualized as a shadow while the pleura and lung are visualized anterior to the intercostal space. The needle can then be inserted in or out of a plane to the transducer and advanced until the tip is just below the inferior border of the rib. After negative aspiration, 3 to 5 mL of local anesthetic is injected, and the pleura should be visualized being pushed away 13.
Intercostal nerve block complications
Care should be taken to perform this block under sterile technique to avoid infection. History of coagulopathy or anticoagulation should be discussed to reduce the risk of bleeding. Performing this block awake can alert the provider to symptoms of pneumothorax or intraneural injection which may go unnoticed in a sedated or anesthetized patient. Pneumothorax is rare and usually requires monitored observation only although providers should be ready to perform needle decompression or insert a chest tube if necessary. Local anesthetic systemic toxicity is fortunately also a rare event. However, local anesthetic uptake from this region is high, and providers should be able to recognize local anesthetic systemic toxicity (LAST) and provide appropriate treatment. Use of dilute concentrations of local anesthetic and keeping total dose below the maximum allowable will decrease the risk of systemic toxicity. Several case reports of inadvertent spinal after intercostal nerve block have been described 14. This is thought to be secondary to local anesthetic spreading medially through the dura, or to the rare occurrence of injection into a dural sac which has been described protruding laterally from the vertebral foramen. Aspiration before injection to rule out intravascular, intrapleural or intrathecal injection should be performed to attempt to exclude these complications, but negative aspiration is not a guarantee. Patients should be monitored for 20 to 30 minutes after the block has been performed to exclude these complications.
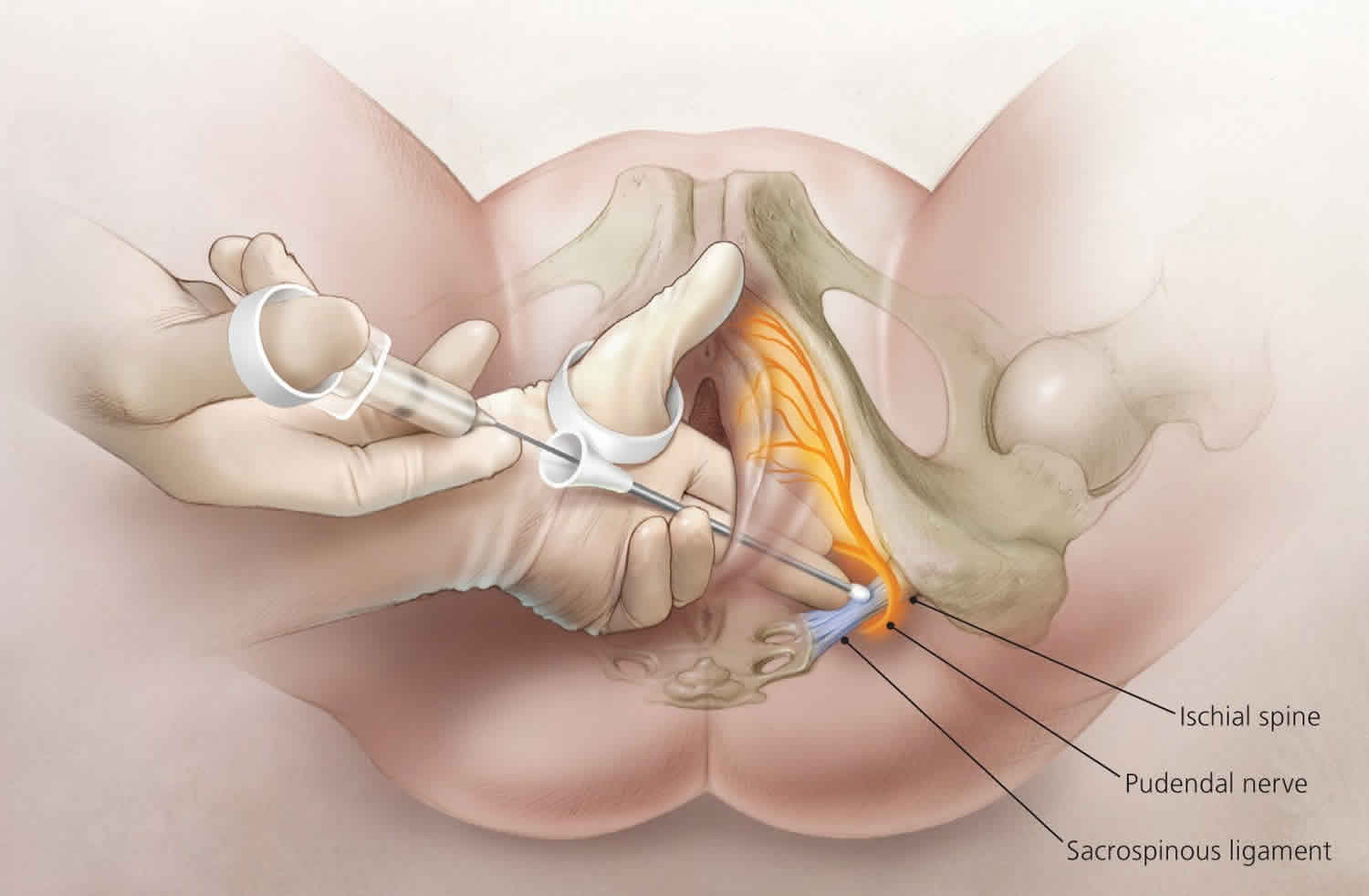
Pudendal nerve block
Pudendal nerve block is used to relieve pain associated with the second (pushing) stage of labour. Blocking the pudendal nerve with injection of local anesthetic is used for vaginal deliveries and for minor surgeries of the vagina and perineum. A pudendal nerve block can be given through the vaginal wall and into the pudendal nerve in the pelvis, numbing the area between the vagina and anus (perineum). Pudendal blocks do not relieve the pain of contractions.
A pudendal nerve block works quickly, is easily administered, and does not affect the baby. It is given shortly before delivery. But it cannot be used if the baby’s head is too far down in the birth canal (vagina).
The sensory and motor innervation of the perineum is derived from the pudendal nerve, which is composed of the anterior primary divisions of the second, third, and fourth sacral nerves. The pudendal nerve’s 3 branches include the following:
- Dorsal nerve of clitoris, which innervates the clitoris
- Perineal branch, which innervates the muscles of the perineum, the skin of the labia majora and labia minora, and the vestibule
- Inferior hemorrhoidal nerve, which innervates the external anal sphincter and the perianal skin
A pudendal nerve block targets the pudendal nerve trunk as it enters the lesser sciatic foramen, about 1 cm inferior and medial to the attachment of the sacrospinous ligament to the ischial spine. Here, the nerve is medial to the internal pudendal vessels. This nerve is accessed by 2 approaches, transvaginal and transcutaneous (or perineal). The former approach is more reliable and is used most often, except when an engaged head makes vaginal palpation more difficult. The anatomical basis for both approaches is to block the nerve proximal to its terminal branches.
Pudendal nerve block indications:
- Analgesia for the second stage of labor
- Repair of an episiotomy or perineal laceration
- Outlet instrument delivery (to assist with pelvic floor relaxation)
- Used in the past as an alternative to neuroaxial analgesia in assisted twin and breech deliveries
- Minor surgeries of the lower vagina and perineum
Even in the best hands, pudendal nerve block is less than 100% reliable. The patient must be checked bilaterally for loss of anal wink reflex before proceeding with the surgical procedure. If mild stimulus does not elicit a reflex response, a pinch confirms the effectiveness of bilateral anesthesia.
A smaller repeat dose can be used if an adequate block is not seen, but care must be taken to avoid toxic serum levels.
Appropriate monitoring of the patient and the fetus is mandatory, and intravenous access should be readily available. Provisions should be made for rapid resuscitation should toxicity or adverse reactions occur.
Keep in mind that the pudendal nerve block provides inadequate anesthesia for mid-forceps delivery, deliveries that require uterine manipulation, postpartum examination and repair of the upper vagina and cervix, and manual exploration of the uterine cavity 15.
- Under these circumstances, the addition of intravenous narcotics may provide appreciable, though not total, relief from pain.
- With such an approach, caution must be exercised to avoid dosages or combinations of narcotics and sedatives that might obtund the patient and cause possible airway obstruction or aspiration.
Pudendal nerve block key facts:
- Pudendal nerve block does not abolish sensation to the anterior part of the perineum, as the perineum is supplied by branches of the ilioinguinal and genitofemoral nerves.
- Failure to wait a sufficient time after injection is a common reason for block failure.
- Pudendal block does not abolish the pain of uterine contractions and cervical dilatation; this sensation is transmitted by the sympathetic fibers derived from the spinal levels of T10-L2.
- Pudendal nerve block does not help relax the uterus.
- The obstetrician should be alert to the total dose of local anesthetic given, especially in cases of repetitive pudendal nerve blocks or pudendal nerve block in association with perineal infiltration. When lidocaine without epinephrine is used, the dose recommended is 4.5 mg/kg. When lidocaine with epinephrine is used, the recommended dose is 7 mg/kg. The maximum dose of lidocaine used should not exceed 300 mg. When bupivacaine without epinephrine is used, the recommended dose is 2.5 mg/kg, with the maximum dose not to exceed 175 mg. When used with epinephrine, the maximum dose of bupivacaine that could be used is up to 225 mg.
- Be sure to use a needle with a guide (either the Iowa trumpet or the Kobak needle guide) to limit the depth of submucosal penetration and to prevent injury to the vagina and the fetus.
Figure 2. Pudendal nerve block
Pudendal nerve block contraindications
Contraindications to pudendal nerve block include:
- Patient refusal
- Patient’s inability to cooperate
- Patient sensitivity to local anesthetics
- Presence of infection in the ischiorectal space or the adjacent structures, including the vagina or perineum
- Coagulation disorders
Pudendal nerve block technique
- Lidocaine 1% is often used for pudendal nerve block. Agents that could be used instead include 2-chloroprocaine 2%, bupivacaine 0.25%, prilocaine 1%, or mepivacaine 1%.
- Pudendal nerve block is performed with the patient in the lithotomy position.
- Usually, no vaginal preparation is needed.
- Pudendal nerve block could be attempted under ultrasonographic, CT, or fluoroscopic guidance. Although imaging helps delineate the anatomic landmark for needle placement, it is rarely used by obstetricians and gynecologists.
- Palpate the ischial spine. This is usually done transvaginally but can also be done through the rectum.
- Be sure to use a needle with a guide (either the Iowa trumpet or the Kobak needle guide) to limit the depth of submucosal penetration and to prevent injury to the vagina and the fetus.
- To perform a left-sided block, palpate the ischial spine with the index finger of the left hand, hold the syringe in the right hand, and guide the needle between the index and middle finger of the left hand toward the ischial spine.
- The injection technique:
- Place the end of the guide beneath the tip of the ischial spine.
- Push the needle into the vaginal mucosa.
- Aspirate to ensure that the injection is not intravascular.
- Raise a mucosal wheal with 1 mL of local anesthetic.
- Advance the needle through the vaginal mucosa until it touches the sacrospinous ligament 1 cm medial and posterior to the ischial spine.
- Infiltrate the tissue with 3 mL of local anesthetic.
- Next, advance the needle further through the sacrospinous ligament for a distance of 1 cm until a loss of resistance is appreciated.
- The tip now lies in the area of the pudendal nerve. At this point, the pudendal vessels lie just lateral to the pudendal nerve, so care must be taken to avoid intravascular administration. Aspirate to confirm the needle placement is not intravascular prior to injecting lidocaine.
- Inject another 3 mL of local anesthetic solution into this region.
- Subsequently, withdraw the needle into the guide and move the tip of the guide to just above the ischial spine.
- At this new location, reinsert the needle though the mucosa and again inject 3 mL of local anesthetic.
- Many practitioners use a single 10-mL injection instead of the 3-injection technique described above. The single injection is done after the needle is introduced nearly 1 cm through the sacrospinous ligament medial and posterior to the ischial spine.
- To block the right side of the pelvis, repeat these steps using the right hand to hold the needle and needle guide (see image below).
Pudendal nerve block complications
Potential complications should be explained to the patient prior to getting informed consent. These complications are uncommon but may be serious. Direct intravascular injections or systemic absorption of an excessive dose of local anesthetic may result in systemic toxicities. Other risks include the following:
- Laceration of the vaginal mucosa is a potential complication.
- The second stage of labor may be prolonged 16 due to a loss of the bearing-down reflex, particularly when local anesthetics are combined with epinephrine (does not affect incidence of instrument delivery) 17.
- Systemic anesthetic complications, though rare and usually transient, may include palpitation, tinnitus, dysarthria, drowsiness, confusion, loss of consciousness, convulsions, hypotension, and bradycardia.
- Hematomas (vaginal, retroperitoneal, and ischiorectal) from injury to the pudendal artery can be a complication of pudendal block, particularly with defective coagulation 18. Hematomas are usually small, and surgical intervention is rarely needed.
- Infection (retro psoas and subgluteal abscess) has occasionally been reported, spreading superiorly along the psoas muscle or laterally along the obturator internus. Infrequent occurrence and diagnostic difficulties make these abscesses especially dangerous 19. Maintain a high suspicion for infection when severe pain in the back or hip, limitation of motion, and, especially, increasing fever follow pudendal anesthesia prior to vaginal delivery.
- Ischial region paresthesia on the first postpartum day, or sacral neuropathy, may occur 17.
- Needle-stick injury with associated risk of exposure to HIV and other bloodborne diseases may result, as the needle guide does not uniformly protect the physician and the procedure requires multiple blind needle punctures.
- Fetal complications are uncommon but may result from fetal trauma and or direct fetal injection of local anesthetic 20. Possible intoxication by local anesthetics should be considered when neonatal distress is seen at birth following the use of pudendal block. Typical features include hypotonia, papillary mydriasis fixed to light, apnea, and seizures. Complete recovery usually occurs.
Femoral nerve block
Femoral nerve block is an injection of local anesthetic medicine around the femoral nerve. Femoral nerve block usually goes into your groin area. Femoral nerve block is used to numb the leg and knee for surgery and to help with pain after surgery.
The femoral nerve runs from your spine all the way down your hip and leg. Femoral nerve sends movement and feeling signals to and from that part of your body.
Femoral nerve block is usually used along with medicine that makes you sleep during the surgery.
Figure 3. Femoral nerve block
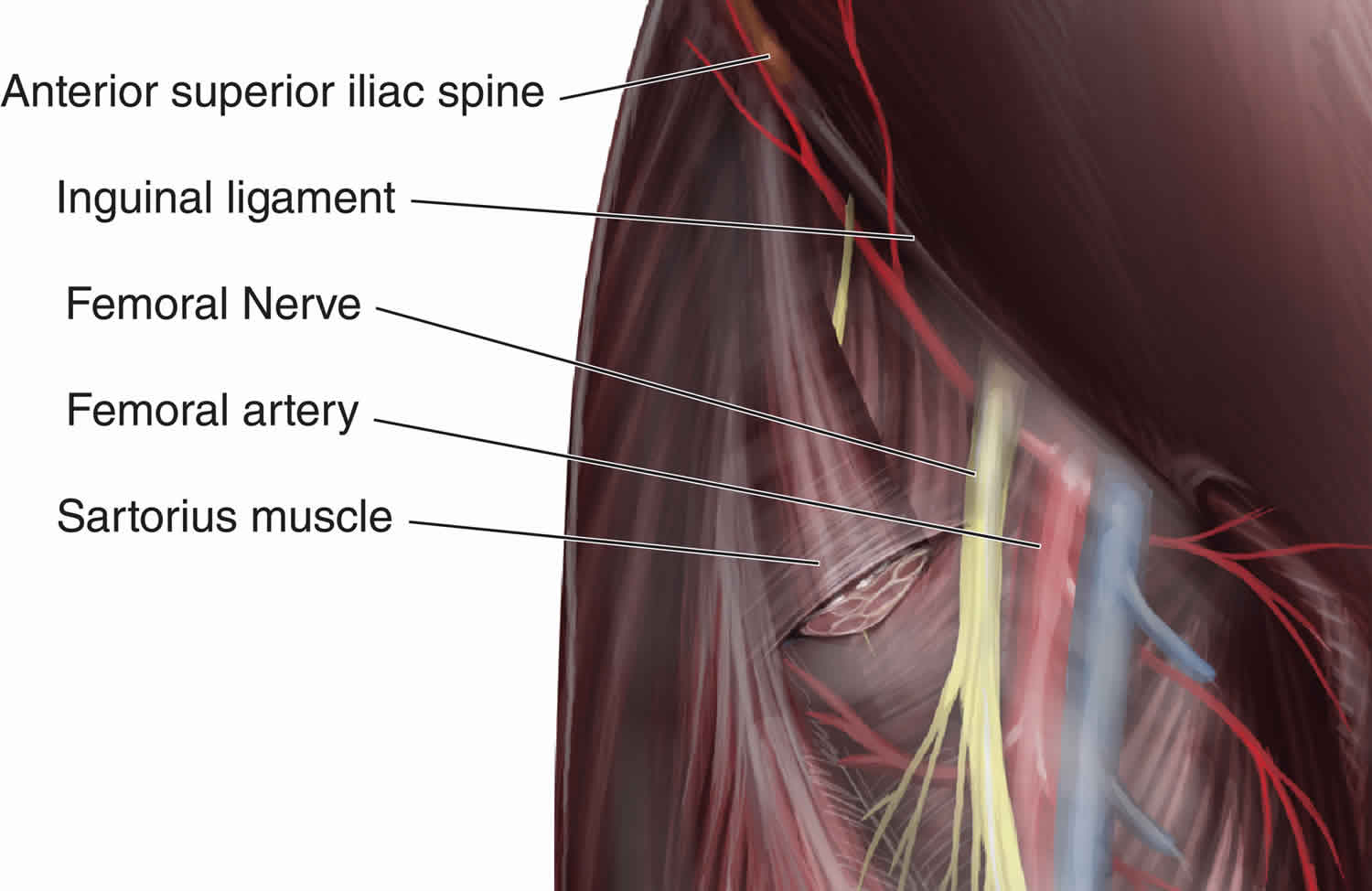
How is a femoral nerve block done?
The doctor may use ultrasound to help guide the femoral nerve block needle.
After finding the right spot, the doctor injects a numbing medicine into the skin near where you will get the nerve block. Then he or she puts the nerve block needle into the numbed area. You may feel some pressure. But you should not feel pain.
What can you expect after a femoral nerve block?
Femoral nerve block will leave your leg partly or totally numb for a while. Your doctor will tell you how long.
You will need someone to drive you home.
As the femoral nerve block wears off, you will start to feel some pain from the surgery. Be sure to take your pain medicines before the pain gets bad.
Problems from a nerve block are rare. There is a small risk of problems like seizures, heart problems, damage to nerves, infection, or bleeding. The benefits usually outweigh these risks.
Genicular nerve block
Genicular nerve block also called genicular radiofrequency ablation or genicular neurotomy 21 of the genicular nerves. Genicular radiofrequency ablation has recently emerged as a treatment option of chronic knee pain from osteoarthritis 22. Preliminary outcomes for genicular nerve radiofrequency ablation are promising 23.
Genicular nerve block procedure is performed in 2 phases:
- Diagnostic Genicular Nerve Block – This procedure consists of placing a small amount of a local anesthetic, like Lidocaine or Bupivacaine, on the genicular nerves to test the patient’s response and see if there is sufficient enough relief in the knee to justify performing a therapeutic neurotomy.
- Genicular Nerve Ablation – This is the therapeutic portion of the treatment whereby the physician will perform a radiofrequency ablation (RFA) of the genicular nerves, thus alleviating pain to the knee and restoring function.
Both portions of the procedure are performed as an outpatient under direct fluoroscopic guidance.
The literature to date supports ablation of the superior medial, superior lateral and inferior medial genicular nerves 23 and the inferior lateral branch is avoided due to its proximity to the common peroneal nerve and risk of motor neuron injury and foot drop 24. The need to ablate the intermediate genicular nerve, thought to provide afferent sensation to the patellofemoral compartment of the knee joint and capsule 24, has been debated, but has yet to be investigated.
Finally, it must be acknowledged that genicular nerve ablation using cooled radiofrequency ablation is an emerging procedure 21. No adverse events related to this procedure using thermal or cooled RFA have been reported in the published literature to date 22. However, post-procedural neuritis/deafferentation pain is a theoretical concern, as this is a known adverse event associated with radiofrequency ablation of the medial branch and sacral lateral branch nerves 25. Third degree skin burn has been reported with the use of cooled radiofrequency ablation to denervate a thoracic medial branch nerve in a patient with a very thin body habitus 26. While Charcot joint is unlikely given incomplete denervation of the knee when ablating only the superiomedial, superiolateral, and inferomeidal genicular nerves, no long-term investigation has been reported to confirm or refute this possibility.
Figure 4. Genicular nerve block
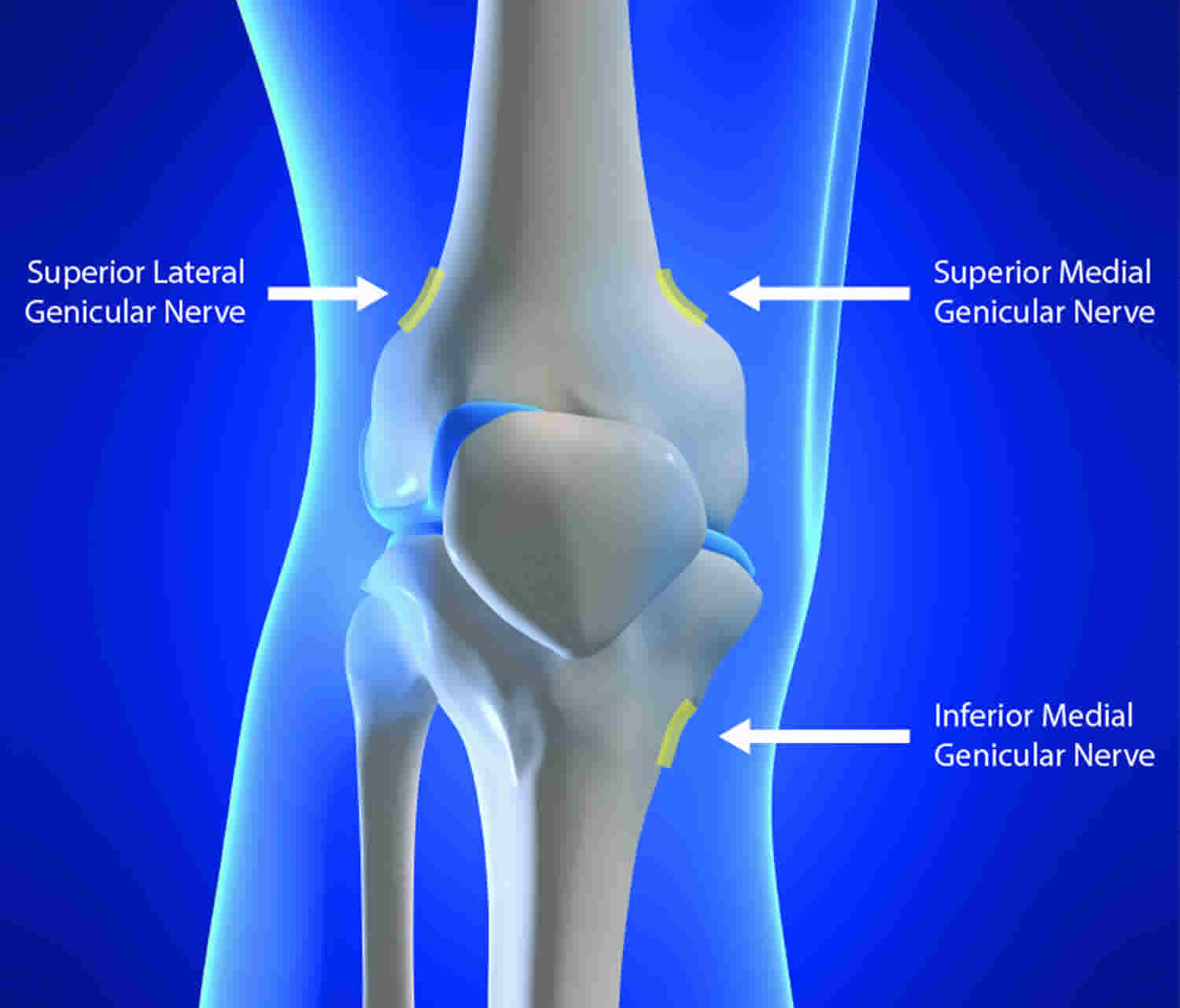
How many treatments will I need?
Before performing a genicular radiofrequency ablation or genicular neurotomy, your doctor will first schedule you for a diagnostic genicular nerve block to see if you are a candidate for the ablation procedure. The pain relieving effects of the genicular neurotomy can last up to a year or longer.
When will I feel better?
The effects of the diagnostic genicular nerve block block can be felt almost immediately, but will typically wear off in just a few hours – this is normal. This is just to let your doctor know if the actual ablation procedure will work for you. Relief from the genicular neurotomy proper typically takes effect in a few days.
How long will it last?
Early data from the clinical trial suggests the effects of genicular radiofrequency ablation or genicular neurotomy may last up to 24 months.
Is genicular neurotomy right for me?
If traditional treatments like physical therapy and injections with cortisone or hyaluronic acid have not provided you with relief, genicular neurotomy may be an option for you. The procedure involves minimal to no scarring, and can be performed as an alternative to surgery to relieve pain, and even for patients still experiencing pain after surgery.
Saphenous nerve block
Saphenous nerve block has wide use in both the emergency department and perioperative settings for procedural anesthesia and post-procedural pain management 27. Saphenous nerve block regional anesthesia procedure is often used to block pain from the medial leg and ankle and can be performed with ultrasound guidance.
The saphenous nerve block is indicated whenever the need exists for anesthesia of the lower leg or foot along its neural distribution. Saphenous nerve block is most commonly used in conjunction with a popliteal sciatic nerve block to provide complete anesthesia of the lower leg for various surgical and nonsurgical procedures 27. These include saphenous vein stripping or harvesting, wound repair or exploration, ankle fracture or dislocation reduction, abscess drainage, and foreign body removal.
Absolute contraindications to the saphenous nerve block include allergy to anesthetic solution or additives, infection at the injection site, and patient refusal. Relative contraindications include coagulopathy, systemic infection, and pre-existing neurologic deficit in the distribution of the block.
Figure 5. Saphenous nerve block
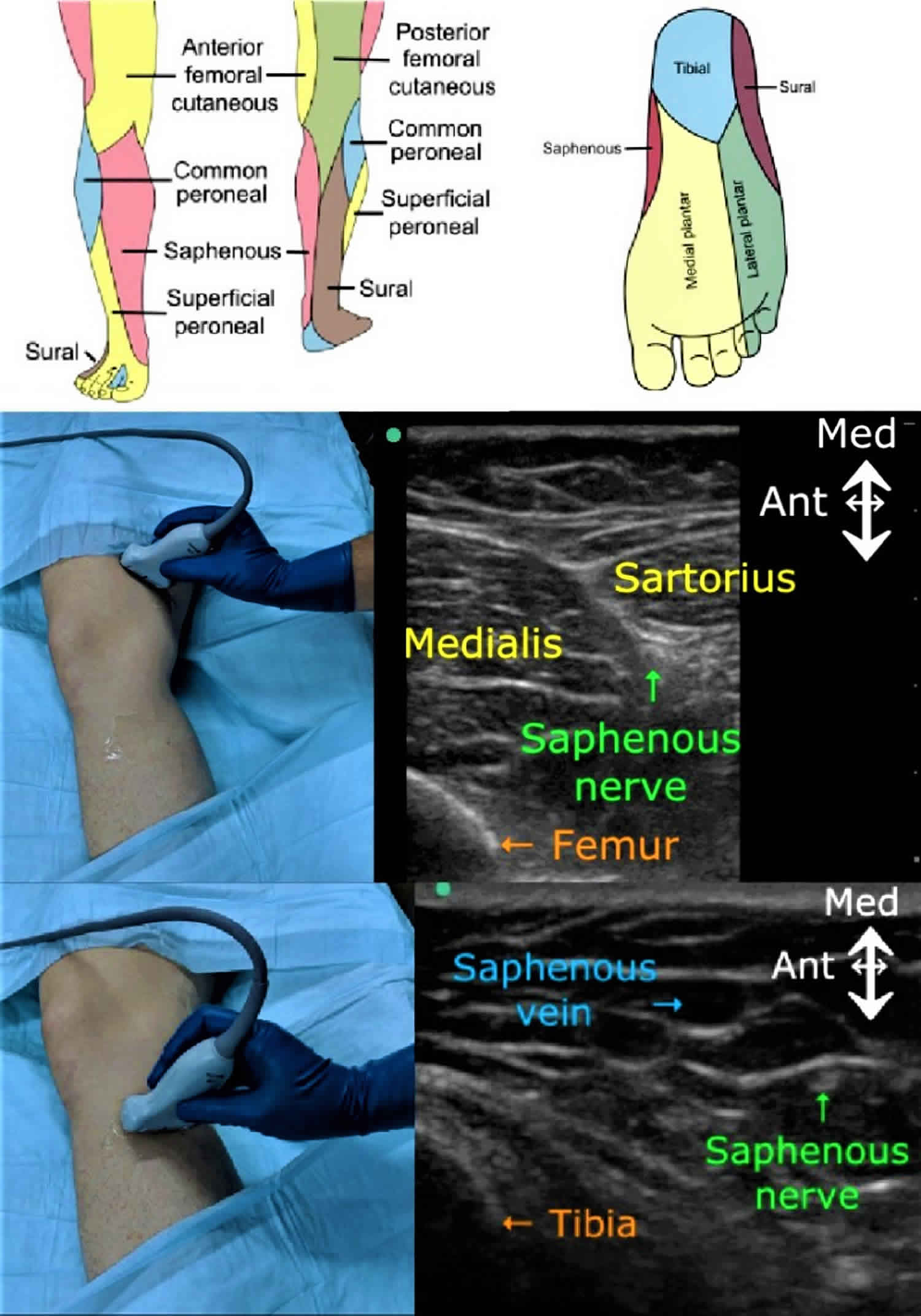
Saphenous nerve block technique
The saphenous nerve block can be performed at the mid-thigh in the adductor canal or just below the knee depending upon the desired area of anesthesia. Although these locations are identifiable anatomically, ultrasound visualization has become the standard of practice.
The adductor canal approach to saphenous nerve blockade provides anesthesia at the level of the mid-thigh. Patient placement is in the supine position with the leg abducted and externally rotated to allow access to the medial thigh. The patient is prepared in a standard sterile fashion. A linear ultrasound transducer is placed perpendicular to the long axis of the lower limb, approximately 5 to 7 cm proximal to the popliteal crease, and slid proximally until the hyperechoic appearance of the vastoadductor membrane fades, and the femoral artery is identified. The saphenous nerve is identified as a hyperechoic circle anterolateral to the femoral artery. After negative aspiration, an in-plane approach is used to inject 5 to 10 mL of local anesthetic deep to the sartorius muscle and lateral to the artery 28.
The saphenous nerve can be blocked below the knee for anesthesia of the lower leg and foot. The patient is positioned supine with the leg straight. After standard sterile preparation, a linear ultrasound transducer is placed at the level of the tibial tuberosity. A short-axis view of the saphenous vein and fascia lata is obtained, and local anesthetic is infiltrated between these two landmarks 29.
Saphenous nerve blockade may also be achieved more distally at the ankle, although the nerve is often not visible with ultrasound at this level. For this reason, a landmark based approach is more reliable but may require higher volumes of local anesthetic. After palpating the medial malleolus and great saphenous vein, local anesthetic is infiltrated approximately 2 cm anterior and posterior to the saphenous vein just superior to the medial malleolus. Ultrasound guidance is helpful if the saphenous vein cannot be visualized or palpated on exam. However, the saphenous nerve usually is not visible on ultrasound at this level 30.
Saphenous nerve block complications
Complications related to saphenous nerve block may include pain on injection, infection at injection site, bleeding, nerve injury, allergic reaction, and local anesthetic systemic toxicity. There is some controversy as to whether or not adductor canal blocks may result in quadriceps muscle weakness as a result of secondary blockade of the vastus medialis nerve.[10] However, several studies have reported that the adductor canal block results in little or no quadriceps muscle weakness, particularly when compared with the femoral nerve block.[7][11][12][13][14] Ultrasound visualization minimizes the likelihood of nerve injury, local toxicity, and vessel puncture.
Complications must be recognized and treated early to avoid long-term morbidity. Patients with suspected systemic toxicity should immediately receive intravenous lipid emulsion (Intralipid) therapy. The dose is 20% lipid emulsion as a 1.5 mL/kg bolus over 2 to 3 minutes, followed by a 0.25 mL/kg/min infusion. Consider consulting your poison control center for guidance.
Sciatic nerve block
The sciatic nerve originates from the sacral plexus (L4-S3) and the sciatic nerve is the workhorse of the lower extremity, supplying the vast majority of the motor and sensory function to the lower limb. It supplies motor function to the posterior thigh, and all muscles below the knee. Sensory function is provided to the posterior thigh, posterior knee joint, and everything below the knee except a narrow band on the medial lower leg. This area is supplied by the saphenous nerve, which is derived from the lumbar plexus.
The long course of the sciatic nerve, from the sciatic notch in the gluteal region to the popliteal fossa, allows for multiple possible sites for an anesthetic blockade. From proximal to distal, these sites are: sacral plexus, classic transgluteal approach, subgluteal approach, anterior approach and the popliteal approach. As with most other regional anesthetic techniques, ultrasound visualization has become the standard of practice. Positioning is an important consideration in sciatic nerve block, with sacral plexus and transgluteal approaches not available in the supine position. The only approach that routinely uses the supine position is the anterior sciatic approach, although both the popliteal and subgluteal approaches can be performed in the supine position also. Consideration must be given to factors such as tourniquet placement, site of surgery, availability of access and postoperative motor impairment when choosing a sciatic nerve block approach.
Sciatic nerve blockade is indicated whenever analgesia or anesthesia of the lower extremity is appropriate. This can range from surgical or nonsurgical procedures to acute or chronic pain relief therapies. Depending on the exact location of the lower extremity coverage required, a sciatic nerve block may need to be combined with blockade of nerves originating from the lumbar plexus to achieve the desired result.
Sciatic nerve block technique
The sacral plexus approach is achieved by drawing a line between the posterior superior iliac spine (PSIS) and the ischial tuberosity on the side to be anesthetized, with the patient in the prone or lateral position. The sacral plexus is normally located approximately 8 cm distal to the PSIS along this line, although individual variation exists from 6 cm to 12 cm. While sacral plexus block is uncommonly used in regular clinical practice, ultrasound approaches have been well described. Of note is that the sacral plexus is the only peripheral sacral nerve location which is proximal enough to provide anesthesia for surgery of the hip when combined with lumbar plexus blockade. Sensory articular branches to the hip arise from the superior gluteal nerve, which originates from the sacral plexus.
The transgluteal approach (aka Labat’s technique) was the originally described and long preferred approach to sciatic nerve block because of its relatively consistent anatomic location. With the patient in Sim’s position, the midpoint of a line from the greater trochanter of the hip to the posterior superior iliac spine is determined. A perpendicular to this first line is drawn from this midpoint. A second line is marked from the greater trochanter to the sacral hiatus. The spot where the perpendicular to the first line intersects the second line becomes the location of needle placement. While relatively consistent, the introduction of ultrasound into regional anesthetic practice has led to a shift away from the classic sciatic nerve block, in favor of subgluteal, anterior, and popliteal approaches.
The subgluteal approach to sciatic nerve blockade has now become the dominant approach to sciatic nerve block for procedures requiring complete knee or distal upper leg anesthesia (e.g., tourniquet placement). Visualizing along a line between the greater trochanter and ischial tuberosity utilizing ultrasound, the sciatic nerve is located in the subgluteal fascial plane above the quadratus femoris muscle. While this approach is usually performed in the lateral position, a supine variant with the hip flexed is also described.
The anterior sciatic approach occurs at the level of the lesser trochanter and has the advantage of being performed in the supine position. This is particularly useful when the patient cannot be positioned laterally. The thigh is externally rotated and the knee flexed. Ultrasound visualization is used to locate the lesser trochanter of the femur. The sciatic nerve is then located both medial and deep to this bony landmark. Anesthetic results are similar to the subgluteal approach.
The popliteal approach is the most distal location for sciatic nerve blockade. The sciatic nerve is anesthetized just proximal to its division into the tibial nerve and the more lateral common peroneal nerve, approximately 6 cm above the popliteal crease. Originally described as a landmark based blind technique, it has become a mainstay of knee and lower leg anesthesia and analgesia since the introduction of ultrasound visualization. The popliteal artery is located in the crease of the knee, as is the tibial nerve lying immediately posterior to it. The tibial nerve is continuously visualized as the probe is moved slowly in a proximal direction until the common peroneal nerve joins with it to form the sciatic nerve. Blockade utilizing the popliteal approach can be performed in the supine or lateral position. It is important to note that this approach will not relieve the pain from a tourniquet placed on the thigh, due to the distal block location.
It is worth noting that selective tibial or common peroneal nerve blocks may be performed in the popliteal region. A selective tibial nerve block is one well-utilized technique for relief of post total knee arthroplasty pain in the posterior knee or calf region. It also preserves the ability to dorsiflex the foot, since the common peroneal nerve is spared. Dorsiflexion is crucial for postoperative ambulation, as it prevents falls from a dragging foot getting caught on the floor as it moves forward.
Any of the above approaches to the sciatic nerve will provide satisfactory anesthesia of the distal lower leg and foot (with exception of the small strip of saphenous nerve sensory innervation previously mentioned). The choice of approach is determined by several factors with the site of the surgical procedure, presence and location of a tourniquet, accessibility of block location, and acceptability of postoperative motor weakness among the most important to consider.
Sciatic nerve block contraindications
Sciatic nerve blockade is absolutely contraindicated in two situations: active area of infection where needle puncture will occur, and the refusal of a competent patient to undergo the procedure. Other contraindications are relative and include alteration of normal coagulation mechanisms, systemic sepsis or isolated infection, and documented neurological disease or deficit. Before performing a regional anesthetic on these patients, careful consideration must be given to the expected benefit of the block, the potential of a complication occurring, and the expected degree of injury from such a complication.
Sciatic nerve block complications
Potential complications related to sciatic nerve blocks include infection at the site of injection, bleeding, nerve injury, and local anesthetic toxicity. Fortunately, all of these are rare, but simple precautions can minimize these occurrences if followed regularly. All nerve blocks should be performed under sterile technique to minimize the chance of infection at the injection site. Direct ultrasound visualization of the needle, nerve, and any nearby vascular structures minimizes the chance of nerve injury, local anesthetic toxicity, and accidental puncture of a blood vessel. Frequent negative aspiration during injection of local anesthetic, even when ultrasound visualization is utilized, is recommended.
Nerve block side effects
Potential side effects and complications are dependent upon the type of block performed. Nerve blocks can cause serious side effects, including paralysis, peripheral nerve injury (although not common the rate may be as high as 8% to 10%) which includes reduced sensation after nerve block, hematoma, local anesthetic systemic toxicity, allergic reaction, infection, and damage to the arteries that supply blood to the spinal cord. Other possible side effects include severely low blood pressure (hypotension), accidental injection of the local anesthetic, alcohol or phenol into an artery, puncture of the lung, damage to the kidneys, diarrhea, and weakness in the legs.
Nerve blocks are not recommended if you have a disease that affects blood clotting, take a medicine (called a blood thinner) that prevents blood clots, have a bowel obstruction, or have any type of uncontrolled infection.
Local anesthetics have a significant risk of systemic toxicity when administered intravascularly. Symptoms usually manifest in the central nervous system first (metallic taste, auditory changes, circumoral numbness, blurred vision, agitation, seizures), followed by cardiovascular effects (hypotension, decreased cardiac contractility, dysrhythmias, complete heart block, cardiovascular collapse). Bupivacaine is particularly cardiotoxic, and reports of cardiovascular collapse in the absence of antecedent neurologic symptoms exist. Neurolytic blocks with alcohol and phenol have utility in chronic pain, but usually as a last resort in cancer pain. They cause semi-permanent destruction of the nerve, which blocks impulse transmission and improves pain. Risks with neurolytic destruction of a nerve include the development of central or deafferentation pain syndromes, which are very difficult to treat 31.
Contraindications include an allergy to aminoesters (procaine, cocaine, tetracaine).
Amides-lidocaine/bupivacaine/mepivacaine/ropivacaine (usually preservative).
Arm nerve block side effects:
- change in your breathing
- failure of the nerve block
- allergic reaction
- bleeding
- nerve damage
- local anesthetic toxicity
- pneumothorax
- droopy eyelid on the side of the block
- developing a hoarse voice
Leg nerve block side effects:
- failure of the nerve block
- allergic reaction
- bleeding
- nerve damage
- local anesthetic toxicity
- National Comprehensive Cancer Network (2013). Adult cancer pain. NCCN Clinical Practice Guidelines in Oncology, version 1.2013.
- Wiederhold BD, Garmon EH, O’Rourke MC. Nerve Block Anesthesia. [Updated 2019 Jan 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431109
- Rao S, Rao S. Glossopharyngeal Nerve Block: The Premolar Approach. Craniomaxillofac Trauma Reconstr. 2018 Dec;11(4):331-332
- Djavaherian DM, Guthmiller KB. Occipital Neuralgia. [Updated 2019 Feb 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538281
- Cesmebasi A, Muhleman MA, Hulsberg P, Gielecki J, Matusz P, Tubbs RS, Loukas M. Occipital neuralgia: anatomic considerations. Clin Anat. 2015 Jan;28(1):101-8
- Greater Occipital Nerve Block for Acute Treatment of Migraine Headache. J Am Board Fam Med. 2018;31(2):211-218. https://www.medscape.com/viewarticle/893943
- Feng LJ. Painless abdominoplasty: the efficacy of combined intercostal and pararectus blocks in reducing postoperative pain and recovery time. Plast. Reconstr. Surg. 2010 Nov;126(5):1723-32.
- Shoeibi G, Babakhani B, Mohammadi SS. The efficacy of ilioinguinal-iliohypogastric and intercostal nerve co-blockade for postoperative pain relief in kidney recipients. Anesth. Analg. 2009 Jan;108(1):330-3.
- Saby A, Swaminathan K, Pangarkar S, Tribuzio B. Alleviating Thoracotomy Pain With Intercostal Liposomal Bupivacaine: A Case Report. PM R. 2016 Nov;8(11):1119-1122
- Baxter CS, Fitzgerald BM. Intercostal Nerve Block. [Updated 2019 Feb 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482273
- Hwang EG, Lee Y. Effectiveness of intercostal nerve block for management of pain in rib fracture patients. J Exerc Rehabil. 2014 Aug;10(4):241-4.
- Bhatia A, Gofeld M, Ganapathy S, Hanlon J, Johnson M. Comparison of anatomic landmarks and ultrasound guidance for intercostal nerve injections in cadavers. Reg Anesth Pain Med. 2013 Nov-Dec;38(6):503-7.
- Saby A, Swaminathan K, Pangarkar S, Tribuzio B. Alleviating Thoracotomy Pain With Intercostal Liposomal Bupivacaine: A Case Report. PM R. 2016 Nov;8(11):1119-1122.
- Chaudhri BB, Macfie A, Kirk AJ. Inadvertent total spinal anesthesia after intercostal nerve block placement during lung resection. Ann. Thorac. Surg. 2009 Jul;88(1):283-4.
- Hutchins CJ. Spinal analgesia for instrumental delivery. A comparison with pudendal nerve block. Anaesthesia. 1980 Apr. 35(4):376-7.
- Zador G, Lindmark G, Nilsson BA. Pudendal block in normal vaginal deliveries. Clinical efficacy, lidocaine concentrations in maternal and foetal blood, foetal and maternal acid-base values and influence on uterine activity. Acta Obstet Gynecol Scand Suppl. 1974. 51-64.
- Langhoff-Roos J, Lindmark G. Analgesia and maternal side effects of pudendal block at delivery. A comparison of three local anesthetics. Acta Obstet Gynecol Scand. 1985. 64(3):269-72.
- Kurzel RB, Au AH, Rooholamini SA. Retroperitoneal hematoma as a complication of pudendal block. Diagnosis made by computed tomography. West J Med. 1996 Jun. 164(6):523-5.
- Svancarek W, Chirino O, Schaefer G Jr, Blythe JG. Retropsoas and subgluteal abscesses following paracervical and pudendal anesthesia. JAMA. 1977 Feb 28. 237(9):892-4.
- Schnider SM, Levinson G, Ralston DH. Regional anesthesia for labor and delivery. Schnider SM, Levinson G, editors. Anesthesia for Obstetrics. 3rd Edition. Baltimore: Williams & Wilkins; 1993. 135-153.
- Reddy RD, McCormick ZL, Marshall B, Mattie R, Walega DR. Cooled Radiofrequency Ablation of Genicular Nerves for Knee Osteoarthritis Pain: A Protocol for Patient Selection and Case Series. Anesth Pain Med. 2016;6(6):e39696. Published 2016 Aug 24. doi:10.5812/aapm.39696 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5560582
- Shen WS, Xu XQ, Zhai NN, Zhou ZS, Shao J, Yu YH. Radiofrequency Thermocoagulation in Relieving Refractory Pain of Knee Osteoarthritis. Am J Ther. 2016 doi: 10.1097/MJT.0000000000000393
- Rojhani S, Qureshi Z, Chhatre A. Water-Cooled Radiofrequency Provides Pain Relief, Decreases Disability, and Improves Quality of Life in Chronic Knee Osteoarthritis. Am J Phys Med Rehabil. 2016 doi: 10.1097/PHM.0000000000000549
- Franco CD, Buvanendran A, Petersohn JD, Menzies RD, Menzies LP. Innervation of the Anterior Capsule of the Human Knee: Implications for Radiofrequency Ablation. Reg Anesth Pain Med. 2015;40(4):363–8. doi: 10.1097/AAP.0000000000000269
- Stolzenberg D, Gordin V, Vorobeychik Y. Incidence of neuropathic pain after cooled radiofrequency ablation of sacral lateral branch nerves. Pain Med. 2014;15(11):1857–60. doi: 10.1111/pme.12553.
- Walega D, Roussis C. Third-degree burn from cooled radiofrequency ablation of medial branch nerves for treatment of thoracic facet syndrome. Pain Pract. 2014;14(6):154–8. doi: 10.1111/papr.12222.
- Arnold C, Brady MF. Saphenous Nerve Block. [Updated 2019 Jan 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536967
- Marian AA, Ranganath Y, Bayman EO, Senasu J, Brennan TJ. A Comparison of 2 Ultrasound-Guided Approaches to the Saphenous Nerve Block: Adductor Canal Versus Distal Transsartorial: A Prospective, Randomized, Blinded, Noninferiority Trial. Reg Anesth Pain Med. 2015 Sep-Oct;40(5):623-30
- Gray AT, Collins AB. Ultrasound-guided saphenous nerve block. Reg Anesth Pain Med. 2003 Mar-Apr;28(2):148; author reply 148.
- Fredrickson MJ, White R, Danesh-Clough TK. Low-volume ultrasound-guided nerve block provides inferior postoperative analgesia compared to a higher-volume landmark technique. Reg Anesth Pain Med. 2011 Jul-Aug;36(4):393-8.
- Pollard R, Higham H, Quinlan J, Webster R, Lie J, Sivasubramaniam S. Nerve block site marking. Anaesthesia. 2019 Jan;74(1):123-124.