Osteopenia
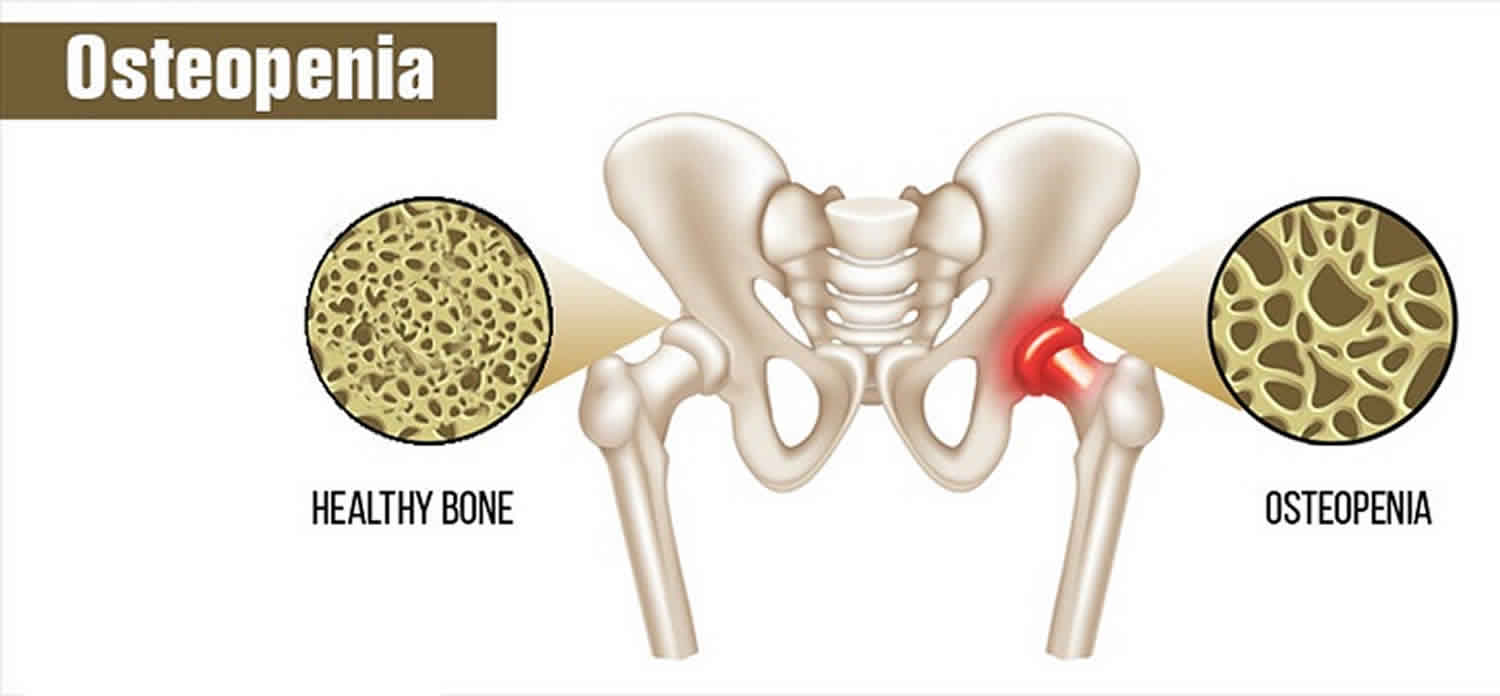
Osteopenia means weak bones or decrease in bone mineral density below normal reference values, but not low enough to meet the diagnostic criteria to be considered osteoporosis 1. Like their names suggest, osteopenia and osteoporosis are related conditions. Both are varying degrees of bone loss, as measured by dual-energy x-ray absorptiometry (DXA) bone scans, a marker for how strong a bone is and the risk that it might break. The T-score is measured in standard deviations and reflects the difference between the patient’s measured bone mineral density and the mean value of bone mineral density in healthy, young, matched controls (30-year-old women). By definition, a normal bone mineral density measurement is within one standard deviation of the young adult mean. As defined by the World Health Organization (WHO), a bone density scan test T-score ranging from -1 to -2.5 is classified as osteopenia and T-score lower than -2.5 would be labeled osteoporosis 2.
This means a bone density scan shows you have lower bone density than the average for your age, but not low enough to be classed as osteoporosis. The lower the T-score, the more porous your bone. If you think of bone mineral density as a slope, normal would be at the top and osteoporosis at the bottom. The stage before osteoporosis is called osteopenia. Osteopenia, which affects about half of Americans over age 50, would fall somewhere in between. Osteopenia happens when the inside of your bones become brittle from a loss of calcium. Osteopenia is very common as you age. Total bone mass peaks around age 35 3. People who have osteopenia are at a higher risk of having osteoporosis.
Osteopenia does not always lead to osteoporosis. It depends on many factors.
If you have osteopenia, there are steps you can take to keep your bones healthy and reduce your risk of developing osteoporosis.
Your doctor also will suggest ways to get more calcium and vitamin D in your diet. Nonfat and low-fat dairy products, such as yogurt, cheese, and milk, are good sources of calcium. Other sources of calcium include dried beans, salmon, spinach, and broccoli. Some foods, such as orange juice, breads, and dry cereals, may be fortified with calcium, vitamin D, or both. Your doctor may suggest a vitamin D or calcium supplement as well.
Your doctor may also prescribe one of the bone-strengthening treatments that are given to people with osteoporosis, depending on how weak your bones are and your risk of breaking a bone.
Currently, 34 million Americans are afflicted with osteopenia 2. The incidence is expected to exponentially increase as our population becomes older with each ensuing decade. Between 2010 and 2030, the United States population over 65 years of age is expected to increase from 13% to over 20%. By 2020, projections estimate that over 47 million Americans will be afflicted with osteopenia 4.
Overall, females have a four-fold higher overall prevalence of osteopenia compared to males. However, males are more likely to demonstrate secondary causes of decreased bone mass. While secondary osteopenia and osteoporosis can develop at any age, the incidence of osteopenia in select subgroups demonstrates predictable patterns and trends. In the United States, 54% of postmenopausal women are osteopenic, and an additional 30% are already considered osteoporotic. By age 80, this relative trend predictably shifts in favor of osteoporosis as 27% of women are osteopenic, and 70% are osteoporotic.
Worldwide, Asia has reported the lowest average t-scores by region. Australia reported an incidence rate of osteopenia in 42% of men and 51% of women. In 2005, India reported a 52% overall incidence in its population. Perhaps more important than the population-based absolute bone mineral density values reported is the associated burden of disease, which has been demonstrated in the reported fragility fractures by region worldwide. The greatest number of fragility fractures occur in Europe, followed by the Western Pacific region, Southeast Asia, and the Americas.
Fragility fractures significantly compromise a patient’s quality of life and financially devastate the healthcare system. Roughly 2 million fragility fractures occur each year in the United States alone, and by 2025 this number is expected to increase to over 3 million. Worldwide, 9 million fragility fractures occur each year. The overall impact of fragility fractures on the healthcare system is staggering. In 2005, direct costs of care associated with fragility fractures alone tallied $19 billion, and the direct and indirect costs of care are expected to surpass $25 billion by 2025. In addition, fragility fractures significantly decrease the quality of life, and hip fractures alone are associated with a one-year mortality rate of greater than 20% 5.
Should I get a bone mineral density test?
Experts disagree about who should get their bone mineral density measured because it’s not clear that the benefits justify the cost. Consider this: 750 tests of women between the ages of 50 and 59 would need to be done to prevent just one hip or spine fracture over a five-year period. From a societal point of view, is that worth it?
Currently, the National Osteoporosis Foundation recommends testing for:
- women 65 and older
- postmenopausal women younger than 65 who have one or more risk factors, which include being thin
- postmenopausal women who have had a fracture
If you aren’t in one of these categories yet, don’t wait until you are to start doing some weight-bearing exercise. Some “uplifting” activity now might prevent frail bones later.
For men, testing is done more on a case-by-case basis.
Osteopenia causes
During your life, your bones constantly change. New bone grows while old bone breaks down and your body absorbs it. When you are young, you grow new bone faster than your body breaks down old bone. This contributes to a high bone mass. Once your body starts to break down old bone faster than it creates new bone, your bone mass begins to decrease. Loss of bone mass weakens your bones and can cause them to break. The beginning of this decline is known as osteopenia. For some people, it can lead to osteoporosis, which is more alarming.
Peak bone mass is normally achieved by the third decade of life. Failure to achieve peak bone mass as a young adult results in early-onset conditions of decreased bone mass (osteopenia or osteoporosis) and increased risk of fragility fractures even in adolescence and young adulthood. After age 30, there is a gradual and natural bone mass reduction that takes place over the ensuing decades into later life 6.
While it is estimated that heritable factors dictate up to 80% of your ability to achieve and maintain optimal bone mineralization levels, modifiable factors attributed to the rate of natural bone mass reduction into adulthood include weight-bearing exercises, nutrition status (adequate calcium and vitamin D daily intake), body mass, and hormonal factors 2.
The natural bone loss that occurs gradually during adulthood is considered to be the cause of primary forms of osteopenia and osteoporosis. Secondary causes serve to accelerate this process and include lifestyle factors such as alcohol use disorder, smoking, sedentary lifestyle, thin body habitus (BMI under 18.5 kg/m²). White and Asian races are also established risk factors.
Overall disease states and certain medications are considered secondary causes as well. Medical conditions include hyperparathyroidism, anorexia, malabsorption syndromes, hyperthyroidism, chronic renal failure, hypogonadism, amenorrhea/oligomenorrhea, early onset menopause, and chronic conditions resulting in calcium and/or vitamin D deficiencies. Medications implicated in the disease process include excess glucocorticoids/long-term steroid use, valproic acid, proton pump inhibitors, antiepileptics, and chemotherapy agents 2.
Women are more likely to have osteopenia than men. This is due to several factors. Women have a lower bone mass overall and absorb less calcium than men do. They also tend to live longer. In women, the rate of bone loss speeds up after menopause as estrogen levels fall. Since the ovaries make estrogen, faster bone loss will occur if both ovaries are removed by surgery.
Natural factors that increase your risk of osteopenia include:
- Bone mass decreases over time.
- Osteopenia is more common in Caucasians and Asians.
- It is more common in women than men.
- Family history of osteopenia or osteoporosis.
- Early menopause for women (before age 45).
- Surgery to remove ovaries.
- Hyperthyroidism.
Long-term use of certain medicines also can increase your risk. Examples include corticosteroids and anticonvulsants. Talk to your doctor about all the ways you can prevent unwanted bone loss.
Osteopenia prevention
Your genes are responsible for determining your height and the strength of your skeleton, but lifestyle factors such as diet and exercise influence how healthy your bones are.
Regular exercise
Regular exercise is essential. Adults aged 19 to 64 should do at least 2 hours and 30 minutes of moderate-intensity aerobic activity, such as cycling or fast walking, every week.
Weight-bearing exercise and resistance exercise are particularly important for improving bone density and helping to prevent osteopenia.
As well as aerobic exercise, adults aged 19 to 64 should also do muscle-strengthening activities on 2 or more days a week by working all the major muscle groups, including the legs, hips, back, abdomen, chest, arms and shoulders.
If you’ve been diagnosed with osteopenia, it’s a good idea to talk to your doctor or health specialist before starting a new exercise program to make sure it’s right for you.
Weight-bearing exercises
Weight-bearing exercises are exercises where your feet and legs support your weight.
High-impact weight-bearing exercises, such as running, skipping, dancing, aerobics, and even jumping up and down on the spot, are all useful ways to strengthen your muscles, ligaments and joints.
When exercising, wear footwear that provides your ankles and feet with adequate support, such as trainers or walking boots.
People over the age of 60 can also benefit from regular weight-bearing exercise. This can include brisk walking, keep-fit classes or a game of tennis. Swimming and cycling aren’t weight-bearing exercises, however.
Resistance exercises
Resistance exercises use muscle strength, where the action of the tendons pulling on the bones boosts bone strength. Examples include press-ups, weightlifting or using weight equipment at a gym.
If you’ve recently joined a gym or have not been for a while, your gym will probably offer you an induction. This involves being shown how to use the equipment and having exercise techniques recommended to you.
Always ask an instructor for help if you’re not sure how to use a piece of gym equipment or how to do a particular exercise.
Stop smoking and drink less
Other lifestyle factors that can help prevent osteopenia include:
- quitting smoking – smoking is associated with an increased risk of osteopenia
- limiting your alcohol intake, it’s also important to avoid binge drinking
Osteopenia diet
Eating a healthy, balanced diet is recommended for everyone. It can help prevent many serious health conditions, including heart disease, diabetes and many forms of cancer, as well as osteopenia.
For healthy muscles and bones, you need calcium, vitamin D and protein:
- calcium makes your bones (and teeth) strong and rigid
- vitamin D helps your bodies to absorb calcium
- protein is important for muscle strength
Calcium is important for maintaining strong bones. Adults need 700mg a day, which you should be able to get from your daily diet. Calcium-rich foods include:
- leafy green vegetables
- dried fruit
- tofu
- yogurt
Vitamin D is important for strong muscles, healthy bones and teeth because it helps your body absorb calcium. All adults should consume 10 micrograms of vitamin D a day. Good dietary sources are:
- oily fish – such as salmon, sardines, herring and mackerel
- red meat
- liver
- egg yolks
- fortified foods such as most fat spreads and some breakfast cereals
- dietary supplements
However, it can be difficult to get enough vitamin D from foods alone. So, consider taking a daily supplement containing 10 micrograms of vitamin D.
From late March/April to the end of September, sunlight triggers the production of vitamin D on your skin, which helps your body absorb calcium. This process helps strengthen teeth and bones, which in turn helps prevent conditions such as osteopenia.
People who are not often exposed to the sun should take a daily vitamin D supplement.
These include people who:
- are not often outdoors, such as those ware are frail or housebound
- are in an institution, such as a care home
- usually wear clothes that cover up most their skin when outdoors
People with dark skin, such as those of African, African-Caribbean and south Asian origin, might not get enough vitamin D from sunlight, so they should consider taking a supplement throughout the year.
Osteopenia symptoms
Most people who have osteopenia do not have symptoms. Loss of bone mass is not painful. Broken bones or fractures can occur, but these problems tend to happen once you have osteoporosis.
Osteopenia diagnosis
In order to diagnose osteopenia, your doctor will do a bone density test. Bone density measures bone mass and bone strength. One type of test is a dual-energy X-ray absorptiometry (DEXA or DXA). It measures bone density in your hips, spine, and wrist. The result can tell if you have osteopenia or osteoporosis, or if your bones are normal. The lower your score, the higher your risk of bone breakage. A T-score between -1 and -2.5 is labeled osteopenia. A T-score lower than -2.5 is labeled osteoporosis.
According to the U.S. Preventive Services Task Force, all women over 65 years old should have a bone density test 7.. Women under 65 years old should be tested as well if they are at high risk.
Women with normal DEXA scans do not need follow-up DEXA scans, as studies have shown that most women with normal scores did not progress to osteoporosis. Some experts may advocate for follow-up scans upon treatment implementation, but this modality remains controversial as the literature suggests subsequent DEXA scans have rarely resulted in interventions or treatment adjustments 4.
Standard laboratory workup includes checking calcium, phosphorus, albumin, alkaline phosphatase, liver function tests, creatinine (serum and urine), 25 hydroxyvitamin D, TSH and free T4, and intact PTH levels. Males should have a free testosterone level checked to rule out hypogonadism.
The routine use of checking bone turnover markers (BTM) is debated. The utility of obtaining markers of bone resorption can be considered if this is being considered the possible underlying cause of secondary osteoporosis. Although reports question the reproducibility of such values, available tests include checking serum or urinary cross-links of type I collagen (deoxypyridinoline), N-telopeptide of type I collagen (NTx), or C-telopeptide of type I collagen (CTx).
The WHO created a fracture risk assessment tool (FRAX score) to predict the 10-year risk of sustaining a hip or other major osteoporotic fracture. These other major fragility fractures include fractures of the spine, wrist, forearm, or humerus. The assessment includes 12 questions weighted by the relative risk associated with a future fragility fracture event. Assessment includes age, sex, personal history of fracture, low BMI, oral steroid use, secondary osteoporosis, parental history of hip fracture, smoking status, and alcohol intake. In addition, optional BMD measurement values can be included from a prior DXA scan (if available) to provide a more comprehensive score report 8.
The utility of the FRAX score is emphasized, especially in the osteopenic patient. Although fracture risk increases with decreases in bone mineral density, the concept that the vast majority of these fragility fractures occur in osteopenic (as opposed to osteoporotic) patients poses a conflicting treatment paradigm. Thus, clinicians rely on the FRAX score to stratify in which osteopenic patients exceed the risk threshold to warrant more aggressive pharmacologic treatments.
Patients younger than 50 at increased fragility fracture risk are recommended to obtain a DEXA scan if one has not been already obtained for another reason. A study from 2013 analyzed the worldwide uptake of FRAX calculation over one year from 2012 to 2013. Nearly 2.5 million calculations from 173 countries were reported, with the USA, UK, Canada, Spain, Japan, France, Belgium, Italy, Switzerland, and Turkey representing over 80% of all calculations.
Osteopenia treatment
Treatment for osteopenia starts with changes to your lifestyle. Osteopenia can be treated either with exercise and nutrition or with medications. But some doctors are increasingly wary about over-medicating people who have osteopenia. Your doctor will want you to increase your physical activity. Weight-bearing exercise can help strengthen your bones. It also can build muscle and improve your balance, which help prevent against broken bones. Examples of weight-bearing exercise include walking, jogging, and climbing steps.
The fracture risk is low to begin with and research has shown that medication may not reduce it that much. Scientists also don’t know if the medications might have some long-term effects. So if your T-score is under -2, you need to be sure you are doing regular weight-bearing exercise, and you are getting enough vitamin D and dietary calcium. If you’re closer to -2.5, your doctor may consider adding medication to keep your bones strong.
Bisphosphonates are the most commonly prescribed medication class for treatment. Adverse side effects are well documented in the literature as prolonged use has been linked to two major clinical side effects: osteonecrosis of the jaw and the atypical subtrochanteric femur fracture.
Common agents include:
- Alendronate may reduce the rate of hip, spine, and wrist fractures by 50%
- Risedronate may reduce vertebral and nonvertebral fractures by 40% over three years
- IV zoledronic acid reduces the rate of spine fractures by 70% and hip fractures by 40% over three years
Osteonecrosis of the jaw is rare and is associated with intravenous forms and not oral forms of the medication. Treatment entails immediately stopping the offending agent. Atypical femur fractures also are rare but have significant associated morbidity, and clinicians are cautioned against the chronic, uninterrupted bisphosphonate use beyond 3 to 5 years or in situations when patients report mild thigh discomfort while undergoing treatment 9.
Other medication classes
- Conjugated estrogen-progestin hormone replacement (HRT)
- Estrogen-only replacement (ERT)
- Salmon calcitonin
- Selective estrogen receptor modulators (Raloxifene) – Raloxifene is an agonist to estrogen receptors on bone and reduces osteoclast resorption
- Anabolic – Teriparatide is a recombinant form of parathyroid hormone (PTH) that stimulates osteoblasts to produce more bone. Teriparatide is now FDA approved for osteoporosis treatment in males and females
- RANKL inhibitors (Denosumab) – Denosumab is a monoclonal Ig2 that targets RANKL and inhibits its ability to bind to RANK and results in the inhibition of osteoclast activation
Treatment and follow-up considerations 10
Treatment duration varies depending on the class of medication utilized. Agents such as teriparatide and hormonal-based therapy require immediate follow-up treatment with another agent upon stopping the medication; otherwise, bone mass is rapidly lost. Clinicians also must remain cautious against the prolonged use of uninterrupted bisphosphonate therapy beyond a 3- to 5-year period. Patients should also be made aware of these potentially morbid adverse events, and they should be counseled to seek immediate care if they are experiencing any symptoms of thigh discomfort.
Any patient on bisphosphonates for any given period and presenting with mild thigh discomfort should have the following treatment workup:
- Educate on the risks of and immediately stop all weight-bearing activity.
- Obtain full-length femur and hip radiographs. Thigh pain may be indicative of an impending pathologic, atypical femur fracture. Attention should be directed to the subtrochanteric and diaphyseal regions of the femur, particularly the lateral cortex, which often demonstrates evidence of periosteal reaction.
- Immediately discontinue bisphosphonate use.
- Refer to an orthopedic surgeon for prophylactic surgical fixation.
- Varacallo MA, Fox EJ. Osteoporosis and its complications. Med. Clin. North Am. 2014 Jul;98(4):817-31, xii-xiii.
- Varacallo M, Pizzutillo P. Osteopenia. [Updated 2019 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499878
- Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, O’Karma M, Wallace TC, Zemel BS. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int. 2016 Apr;27(4):1281-1386.
- Varacallo MA, Fox EJ, Paul EM, Hassenbein SE, Warlow PM. Patients’ response toward an automated orthopedic osteoporosis intervention program. Geriatr Orthop Surg Rehabil. 2013 Sep;4(3):89-98.
- Donnally III CJ, DiPompeo CM, Varacallo M. Vertebral Compression Fractures. [Updated 2019 Oct 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448171
- El Sayed SA, Nezwek TA, Varacallo M. Physiology, Bone. [Updated 2019 Jul 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441968
- Karaguzel G, Holick MF. Diagnosis and treatment of osteopenia. Rev Endocr Metab Disord. 2010 Dec;11(4):237-51.
- Kanis JA, Johansson H, Oden A, Cooper C, McCloskey EV., Epidemiology and Quality of Life Working Group of IOF. Worldwide uptake of FRAX. Arch Osteoporos. 2014;9:166.
- Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, Felsenberg D, Gagel RF, Gilsanz V, Guise T, Koka S, McCauley LK, McGowan J, McKee MD, Mohla S, Pendrys DG, Raisz LG, Ruggiero SL, Shafer DM, Shum L, Silverman SL, Van Poznak CH, Watts N, Woo SB, Shane E., American Society for Bone and Mineral Research. Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J. Bone Miner. Res. 2007 Oct;22(10):1479-91.
- Lenart BA, Lorich DG, Lane JM. Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. N. Engl. J. Med. 2008 Mar 20;358(12):1304-6.