Ototoxicity
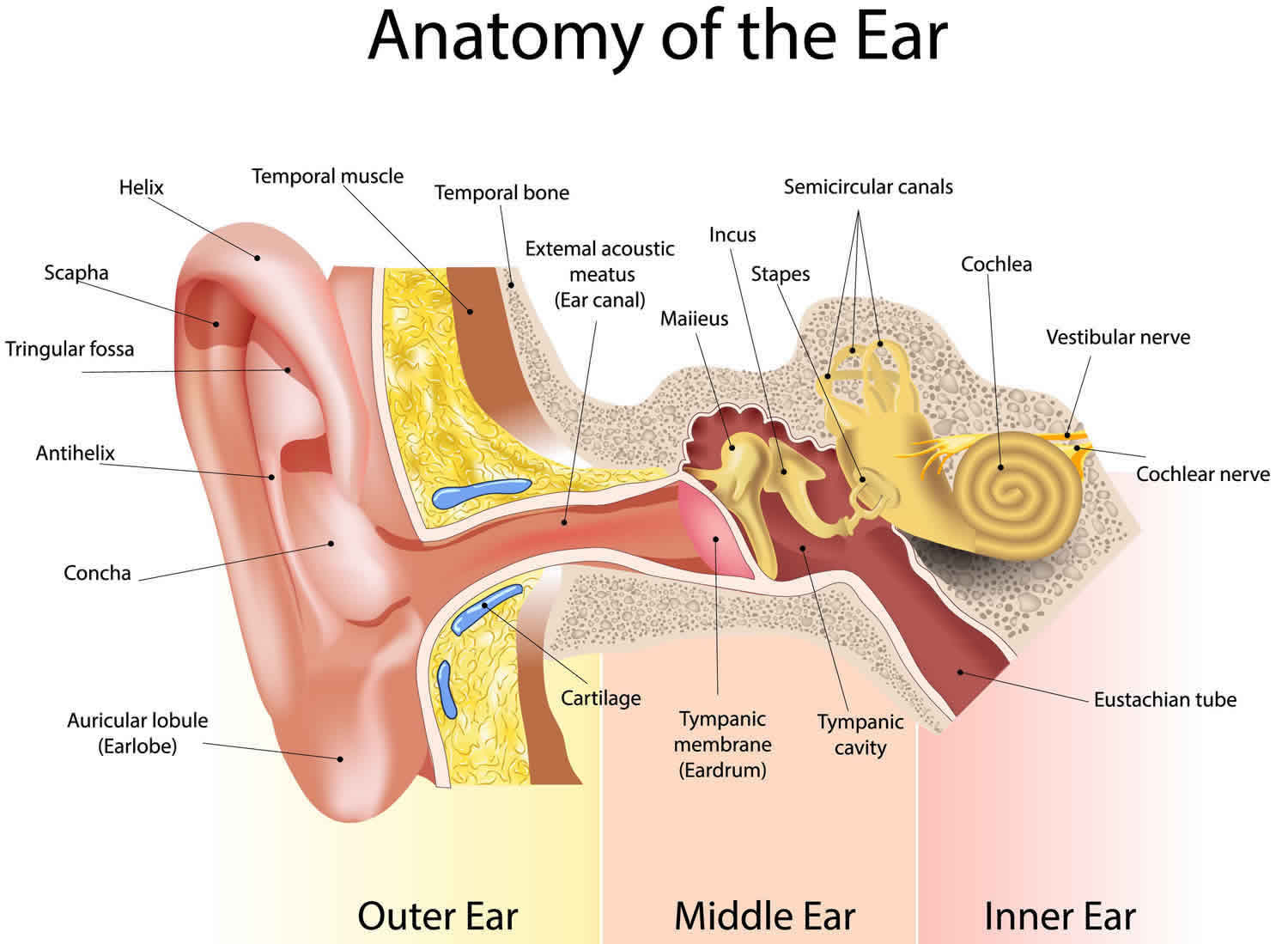
Ototoxicity is a medical term for ear poisoning (oto = ear, toxicity = poisoning), which results from exposure to drugs or chemicals that damage the inner ear or the vestibulo-cochlear nerve (the nerve sending balance and receiving/sending sounds from the inner ear to the brain). Because the inner ear is involved in both hearing and balance, ototoxicity can result in disturbances of either or both of these senses. The parts of the brain that receive hearing and balance information from the inner ear can also be affected by poison, but this is not technically considered ototoxicity. Poisoning of the brain is classified as neurotoxicity.
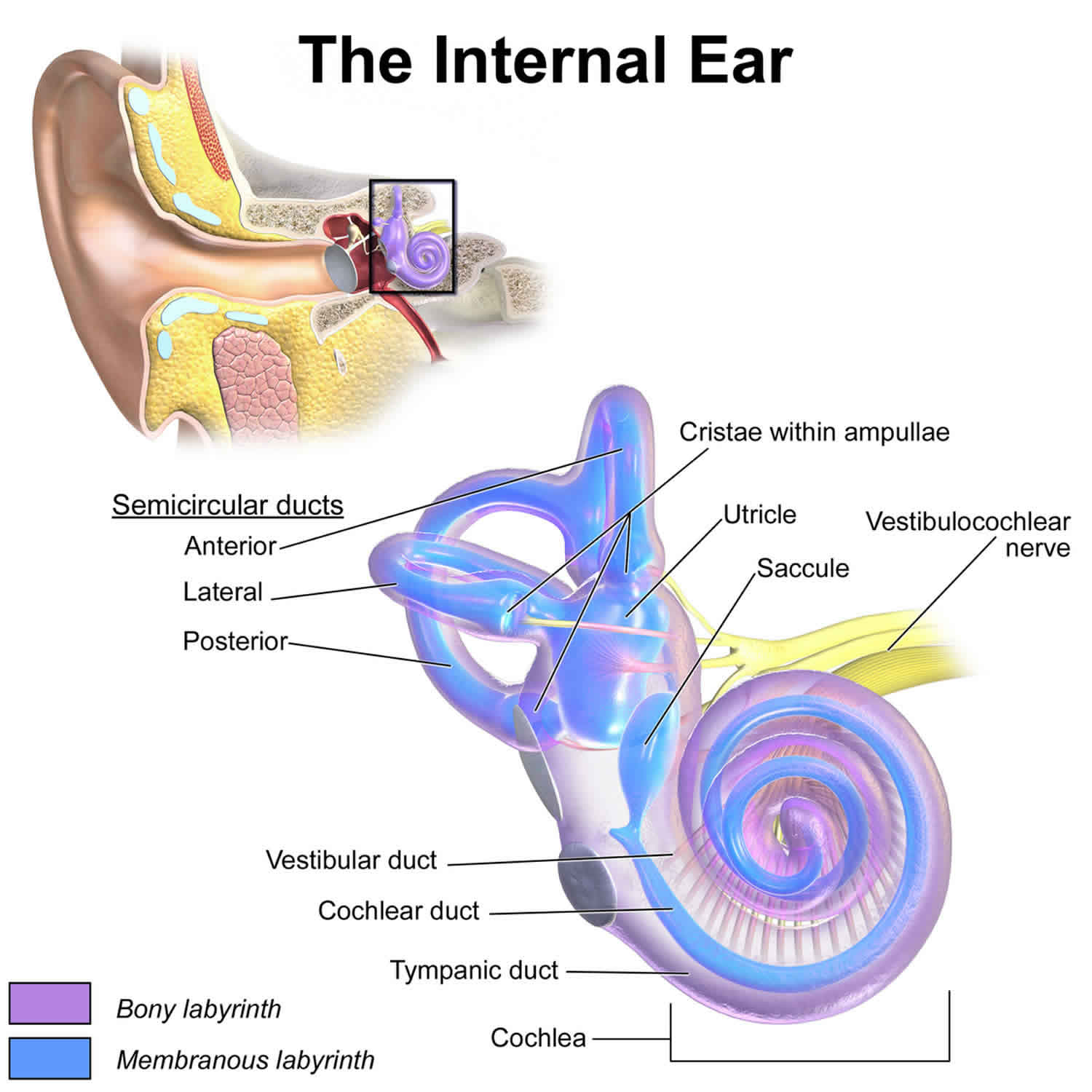
Two areas can be damaged or destroyed through ototoxicity: the hair cells within the inner ear, and the vestibulo-cochlear nerve that links the inner ear to the brain. When damage occurs, any degree and combination of hearing loss and balance disruption are possible depending upon the part(s) affected and on what type of drug a person is taking, how much, and for how long. Some people may have no problems or very minimal hearing loss and “ringing in the ears” (tinnitus). But other people might have major problems with balance and/or profound hearing loss (sensorineural deafness).
Hair cells are located in both the cochlea and the vestibular areas of the inner ear. They are composed of a cell body with a hair-like attachment. When these “hairs” are normally bent with sound vibrations or movement, they send electrical signals to the brain about hearing or balance function. In ototoxicity, these hairs can be damaged to the point that they no longer stand up, thus reducing the auditory and/or balance signals sent to the brain.
The occurrence and degree of ototoxicity (inner ear poisoning) depends upon the drug involved as well as other factors such as heredity. Ototoxicity can be temporary or permanent. The effect of certain drugs is often temporary, while other drugs typically produce permanent changes to the ear. Some drugs can cause either temporary or permanent problems. It is important to note here that the broad majority of people who experience ototoxicity have a temporary or reversible form that does not result in a major or long-term disruption in their lives.
With cochleotoxicity, hearing loss or the start or worsening of tinnitus (ringing in the ears) can occur through damage to the cochlea (the hearing apparatus) or the cochlear branch of the vestibulo-cochlear nerve. Vestibular ototoxicity or vestibulotoxicity are terms used to describe ototoxicity that affects the balance organs or the vestibular branch of the vestibulo-cochlear nerve.
When ototoxicity is caught early, doctors can work to prevent problems from becoming worse and get patients the rehabilitation they need to deal with any damage that’s been done.
It is important to note that no drug is known to cause Ménière’s disease, benign paroxysmal positional vertigo, or any other vestibular disorder causing fluctuating function.
Figure 1. Ear anatomy
Figure 3. The Cochlea (cross section view)
Note: a) Cross section of the cochlea. (b) The spiral organ and the tectorial membrane.
Figure 4. Inner ear maculae respond to changes in head position
Note: (a) Macula of the utricle with the head in an upright position. (b) Macula of the utricle with the head bent forward.
Figure 5. Dynamic inner ear balance organs (crista ampullaris) within the Semicricular ducts
Drugs that cause ototoxicity
Scientific studies are required to confirm whether a drug is ototoxic. Unfortunately, such research often involves years of study. When assessing the safety of a drug prior to releasing it on the market, the U.S. Food and Drug Administration (FDA) does not require testing of inner ear function or examination of the inner ear structures. This is one reason it is almost impossible to say with confidence how many and which drugs cause ototoxicity and how many or which people are affected by it.
Problems with a particular drug are usually only discovered after enough people have suffered the consequences and when physicians or other health care professionals can see a probable connection between the symptoms or problems and a drug. This was the case with aspirin and quinine centuries ago, with the antibiotic streptomycin in the 1940s, and more recently with some anti-cancer drugs. Since then, scientific studies have shown that these drugs cause ototoxicity in animals and people. Other, newer drugs have been implicated as ototoxic as well, but solid scientific proof is often lacking.
Many chemicals have ototoxic potential, including over-the-counter drugs, prescription medications, and environmental chemicals. The information below includes substances thought to cause ototoxicity. The discussion is incomplete because of the limited research thus far. If you are taking drugs on the advice of your physician, DO NOT STOP TAKING THEM just because you see them listed here. Speak with your doctor about your concerns to determine the best choice in your own unique situation.
Aspirin and quinine
Aspirin (acetylsalicylic acid) and quinine are well known to cause temporary ototoxicity resulting in tinnitus. They may also reduce hearing, particularly when given at high doses. Quinine products can also temporarily reduce balance ability. Once aspirin or quinine is stopped, the ototoxicity generally disappears. Some quinine products include:
- chloroquine
- quinidine
- quinine (including Q-vel)
- tonic water
Loop diuretics
Loop diuretics are a specific family of “water pills” that is known to occasionally cause temporary ototoxicity. These drugs cause ringing in the ears or decreased hearing that reverses when the drug is stopped.
An increased probability of ototoxicity is thought to occur with loop diuretics when they are administered during the same time period that an aminoglycoside antibiotic (see next section) is given. The loop diuretics include:
- bumetanide (Bumex)
- ethacrynic acid (Edecrin)
- furosemide (Lasix)
- torsemide (Demadex)
Hydrochlorothiazide and Maxide (triamterene and hydrochlorothiazide) diuretics commonly prescribed to people with Ménière’s disease or other forms of endolymphatic hydrops—are not loop diuretics.
Aminoglycoside antibiotics
All members of the aminoglycoside antibiotic family are well known for their potential to cause permanent ototoxicity if they enter the inner ear. Some of these drugs are more likely to cause hearing loss; others are more likely to cause vestibular loss. Others can cause either problem.
Members of the aminoglycoside family include:
- amikacin
- netilmicin
- dihydrostreptomycin
- ribostamycin
- gentamicin
- streptomycin
- kanamycin
- tobramycin
- neomycin
A higher risk for aminoglycoside-antibiotic induced ototoxicity occurs when a person receives concurrent ototoxic drugs (such as a loop diuretic or another antibiotic—vancomycin), has insufficient kidney function or is receiving a drug that causes insufficient kidney function, or has a genetic vulnerability.
The risk of ototoxicity also increases with an increasing amount of the drug that enters the blood stream, the longer the drug is in the body, and the duration of time the drug is taken.
Aminoglycoside antibiotics can enter the inner ear through the blood system or via diffusion from the middle ear into the inner ear. They enter the blood stream in largest amounts when given intravenously (by IV) and in the least amounts by pill. Inhaled drugs also enter the blood stream; an example of this is the use of inhaled tobramycin for long-term treatment of cystic fibrosis.
Ear drops containing aminoglycosides can be problematic if they find their way into the middle ear in large enough quantities, such ear drops can diffuse into the inner ear and cause damage. Physicians do not agree about how often and under what circumstances this occurs. Many papers in medical journals address this argument.
Anti-neoplastics (anti-cancer drugs)
Anti-cancer drugs work by killing cancer cells. Unfortunately some can also damage or kill cells elsewhere in the body, including the ears. Cisplatin is well known to cause massive and permanent hearing loss. Carboplatin is also known to be ototoxic.
Environmental chemicals
Environmental chemicals have long been implicated in ototoxicity. Little research has been done to substantiate their precise effect on ears, but most are associated with hearing disturbances that may be permanent. In addition, mercury has also been linked to permanent balance problems. These include:
- butyl nitrite
- mercury
- carbon disulfide
- styrene
- carbon monoxide
- tin
- hexane
- toluene
- lead
- trichloroethylene
- manganese
- xylene
Ototoxicity prevention
Limit using drugs to those that are absolutely needed and follow the instructions carefully for those medications that are prescribed for you. If possible, avoid taking multiple types of ototoxic drugs (aspirin, quinine, loop diuretics, and aminoglycosides). When using airborne chemicals that are potentially ototoxic, good ventilation should be used. Open the windows, turn on a fan, and refrain from using the chemical for any longer than necessary. Stay well hydrated.
Ototoxicity signs and symptoms
The symptoms of ototoxicity can come on suddenly after a course of medicine or show up gradually over time.
Cochleotoxicity symptoms [hearing loss or the start or worsening of tinnitus (ringing in the ears) can occur through damage to the cochlea (the hearing apparatus) or the cochlear branch of the vestibulo-cochlear nerve] range from mild tinnitus to total hearing loss, depending upon each person and the form and level of exposure to the ototoxin. They can include one-sided or two-sided hearing loss and constant or fluctuating tinnitus. Some people may notice obvious hearing problems, usually in both ears (called bilateral hearing loss). They may have trouble hearing certain things, from high-pitched sounds to talking if there’s background noise. Or they may have tinnitus, which can cause annoying ringing in the ears as well as other strange sounds like hissing, buzzing, humming, and roaring. Sometimes, though, there’s only limited damage, and people might not even notice a problem. Or they might just have a hard time hearing high-frequency sounds while everything else sounds perfectly clear.
Signs of hearing problems include:
- limited, poor, or no speech
- being frequently inattentive
- having problems at work, in school or difficulty learning
- constantly turning up the volume on the TV or stereo
- not responding to conversation-level speech or noises as expected (in babies and pre-verbal children, this would mean not startling or turning their heads when they hear a loud sound)
- becoming tired more quickly or more often after hours of careful listening (such as after work or school)
Vestibulotoxicity symptoms [vestibular ototoxicity describe ototoxicity that affects the balance organs or the vestibular branch of the vestibulo-cochlear nerve] range from mild imbalance to total incapacitation. Symptoms of a vestibular or balance function loss depend upon the degree of damage, if the damage occurred rapidly or slowly, if it’s one-sided or two-sided, and how long ago the damage occurred. A slow one-sided loss might not produce any symptoms, while a rapid loss could produce enough vertigo, vomiting, and nystagmus (eye jerking), to keep a person in bed for days. Most of the time, the symptoms slowly pass, allowing a person to return to normal activities.
A two-sided loss in vestibulotoxicity typically causes headache, a feeling of ear fullness, imbalance to the point of being unable to walk, and a bouncing and blurring of vision (oscillopsia) rather than intense vertigo, vomiting, and nystagmus. It also tends to produce inability to tolerate head movement, a wide-based gait (walking with the legs farther apart than usual), difficulty walking in the dark, unsteadiness or the sensation of unsteadiness, lightheadedness, and significant fatigue. If the damage is severe, symptoms such as oscillopsia and problems with walking in the dark or with the eyes closed will not diminish with time.
Ototoxicity diagnosis
Ototoxicity diagnosis is based upon the patient’s history, symptoms, and test results. There is no specific test for ototoxicity; this makes a positive history for ototoxin exposure crucial to the diagnosis. Some of the tests that may be used to determine how much hearing or balance function have been lost involve the vestibular autorotation test, vestibulo-ocular reflex testing equipment (VORTEQ), electronystagmography (ENG), computerized dynamic posturography, rotary chair, head-shaking, electrocochleography, auditory brainstem response (ABR), otoacoustic emissions, pure tone audiometry, speech discrimination, and most other tests often used to identify and quantify inner ear problems.
Ototoxicity treatment
Research continues on ways to prevent or reverse ototoxicity, but so far there are no treatments that can reverse the damage. Currently available treatments focus on reducing the effects of the damage and rehabilitating function. Specifically, individuals with serious damage to the inner ear and with hearing loss may be helped with amplification device and hearing aids; those with profound bilateral (two-sided) hearing loss have been shown to benefit from cochlear implants. In fact, many early recipients of cochlear implants were victims of ototoxicity. An amplification device called an FM system can help reduce background noise. FM systems, sometimes called “auditory trainers,” may be provided to improve hearing in group or noisy environments and also can be fitted for personal or home use. Other assistive listening or alerting devices may help older people. Hearing aids come in various forms that fit inside or behind the ear and make sounds louder. They are adjusted by an audiologist so that the sound coming in is amplified enough to allow the person to hear it clearly. Sometimes, the hearing loss is so severe that the most powerful hearing aids can’t amplify the sound enough. In those cases, a cochlear implant may be recommended. Cochlear implants are surgically implanted devices that bypass the damaged inner ear and send signals directly to the auditory nerve. A small microphone behind the ear picks up sound waves and sends them to a receiver that has been placed under the scalp. This receiver then transmits impulses directly to the auditory nerve. These signals are perceived as sound and allow the person to hear.
When a loss of balance function has occurred, balance therapy also called vestibular rehabilitation can help the brain become accustomed to the altered balance signals coming from the inner ear. This may include training exercises that help strengthen balance skills and coordination. Exercises may involve bending down, standing or walking with eyes open and then with eyes closed, or having a therapist reposition the patient’s head at different angles to move fluid or debris out of certain parts of the ear. Balance therapy can also assist an individual in developing other ways to maintain balance such as emphasizing the use of vision and proprioception—the sensation felt by the soles of the feet, the ankles, knees, and hips— and structuring a program of general physical conditioning and exercises designed to strengthen and tone muscles.
The major long-term goals include continuing with conditioning activities to improve balance function, protecting the other systems involved with maintaining balance, and preventing further ototoxic damage.
Protection of other components of balance—vision and proprioception—is essential. Good vision is crucial in the face of a severe vestibular loss. Yearly ophthalmological examinations that include a glaucoma check should become routine. Use of ultraviolet (UV) eye protection in the sun and eye protection in the wind (such as goggles or sunglasses) should be considered.
Protecting proprioception involves taking precautions such as avoiding walking barefooted on any surface that could injure or damage the soles (such as on a macadam road surface), not wearing clothing that restricts circulation to the legs and feet (such as a tight girdle), and taking off excess body weight that can cause knee and hip difficulties.
Avoidance of ototoxic substances is also very important because individuals who have suffered from ototoxicity have a higher likelihood of experiencing it again, if exposed. A medic alert tag might be helpful for warning health care professionals about the need to avoid prescribing ototoxic medications unless needed to save your life. Such tags might also serve to flag an existing reduction in balance and/or hearing function.