Hidradenoma papilliferum
Hidradenoma papilliferum also called papillary hidradenoma, is benign tumor arising from apocrine sweat glands or anogenital mammary glands (see Figures 2 and 3) 1. Papillary hidradenoma has been reported primarily to affect Caucasian females, typically during the third to fifth decades of life 2. Hidradenoma papilliferum has not been reported prior to puberty 3. The lesions are usually solitary, well-demarcated dermal or subcutaneous papules or nodules covered with normal skin, and are generally less than 10 mm in diameter 4. Handa et al. 5 reported a case of a large ulcerated perianal hidradenoma papilliferum up to 4 cm in diameter in a young female. Hidradenoma papilliferum tumor is frequently asymptomatic, though may be associated with a itching, burning sensation or pain and bleeding or discharge, especially if there is ulceration of the lesion 6. Hidradenoma papilliferum usually occurs in a vulval, perineal or perianal location. When these tumors are not located in the anogenital area, they are termed ectopic hidradenoma papilliferum 7. Hidradenoma papilliferum can also occur in male or extragenital areas, this is considered as an ectopic variety 2. Ectopic hidradenoma papilliferum, which involves the skin away from anogenital region, is exceedingly rare, and unexpectedly, affects males as well as females 8.
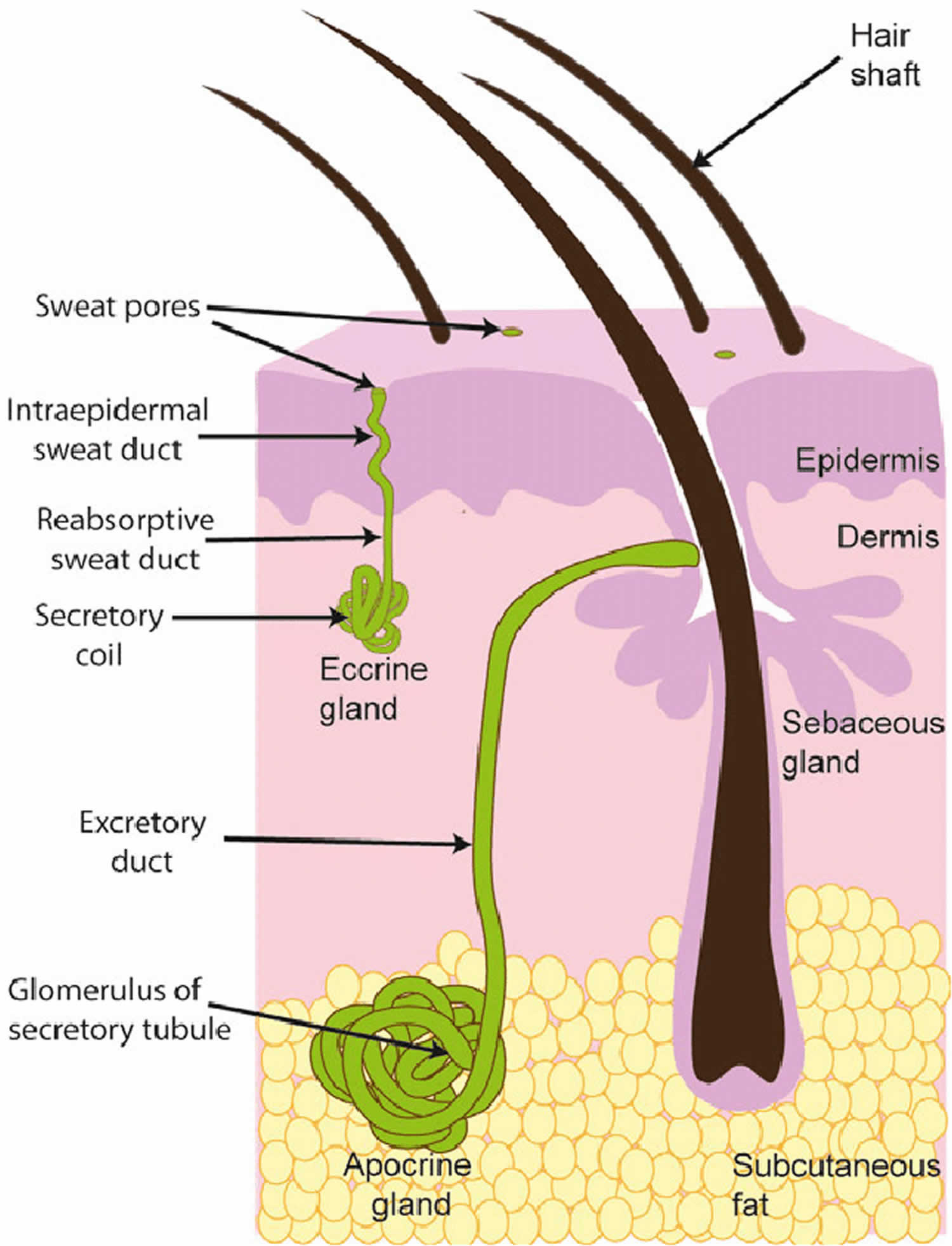
Your skin has two types of sweat glands: eccrine and apocrine. Eccrine glands occur over most of your body and open directly onto the surface of your skin. Apocrine glands are usually associated with hair follicles or open into the hair follicle, leading to the surface of the skin. Apocrine sweat glands continuously secrete a fatty sweat into the gland tubule. Emotional stress causes the tubule wall to contract, expelling the fatty secretion to the skin, where local bacteria break it down into odorous fatty acids. Apocrine glands develop in areas abundant in hair follicles, such as on your scalp, armpits and genital regions; the glands are inactive until they are stimulated by hormonal changes in puberty.
Hidradenoma is a benign adnexal neoplasm originating from the apocrine sweat gland 9. Hidradenoma is histologically sub-divided into four categories:
- Tubular,
- Cystic,
- Papillary (hidradenoma papilliferum), and
- Syringocystadenoma papilliferum-like (occurs mostly on the skin of the head and neck and rarely involves the eyelid).
Hidradenoma papilliferum is a benign tumor that requires differentiation from many other diseases such as thrombosed external hemorrhoids, anal abscess, viral warts, and epidermoid carcinoma. Less often, hidradenoma papilliferum may be confused with sebaceous cysts, lipomas, or neurofibromas. In cases of associated pigmentation, hidradenoma papilliferum may also be confused with anal endometriosis, angioma, or melanoma of the anogenital area 10.
Regardless of the site, the treatment of choice is local excision 6. Recurrence of anogenital and ectopic hidradenoma papilliferum is unusual and is typically attributed to incomplete excision of the primary tumor. Malignant transformation is rare. The malignant counterpart is very aggressive, with high rates of recurrence. These have many synonyms, including malignant hidradenoma, hidradenocarcinoma, malignant acrospiroma, acrospirocarcinoma, and clear cell eccrine carcinoma 8.
Figure 1. Sweat glands (apocrine and eccrine sweat glands)
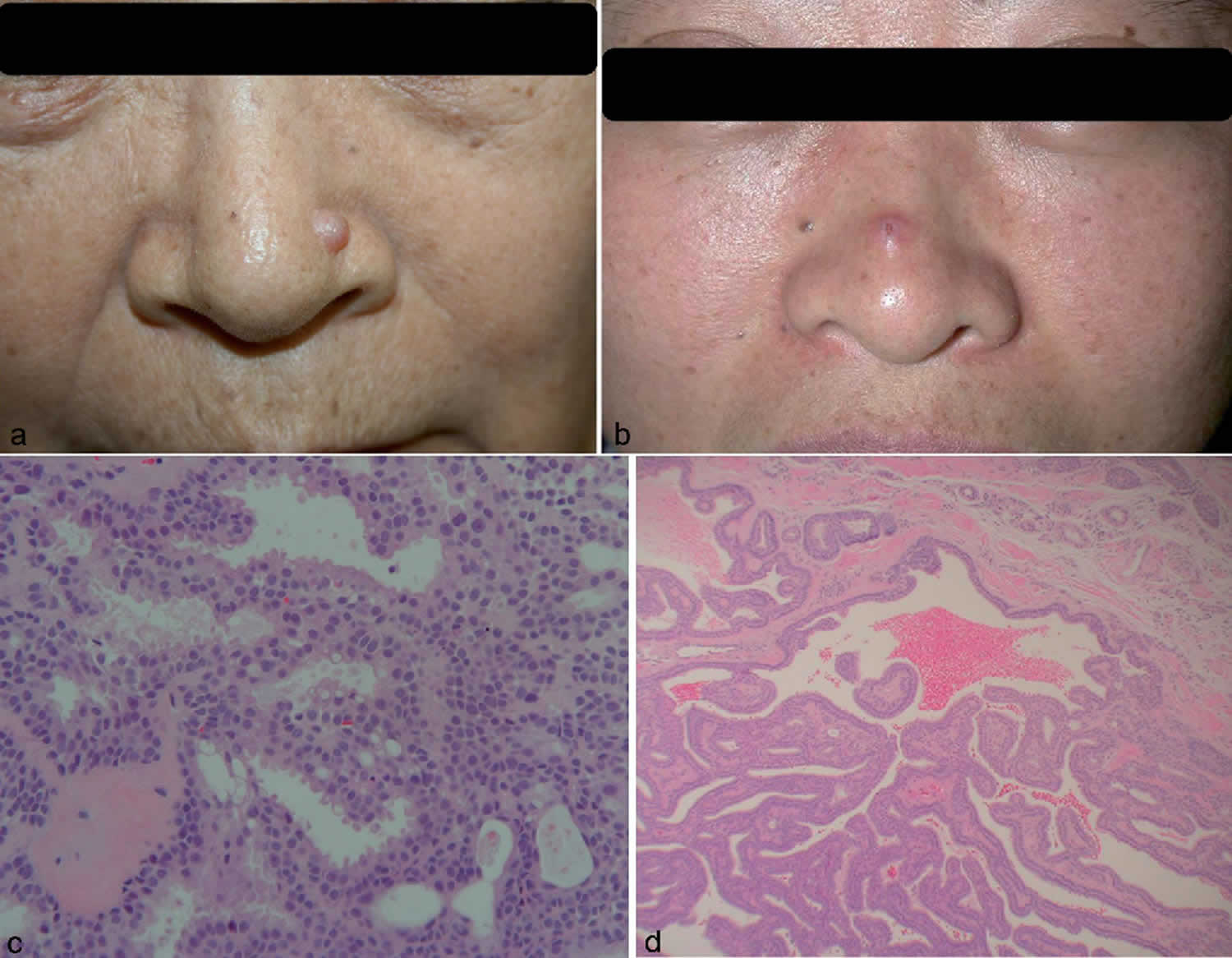
Figure 2. Papillary hidradenoma
Footnote: (a) A 7 × 7 mm sized, soft, dome-shaped mass with normal skin colour on the left lateral side of nose (case 1). (b) A 10 × 10 mm sized, slightly erythematous, dome-shaped nodule with central ulceration (case 2). (c) The lumen of the papillary glandular structure was lined with two layers of columnar and cuboidal cell with active decapitation (case 1, haematoxylin and eosin (HE) × 200). (d) Complex anastomosing papillary glandular structure (case 2, HE × 40).
[Source 11 ]Figure 3. Hidradenoma papilliferum
Footnote: (A) Shows the bluish mass involving the anterior superior-medial aspect of the left orbit (arrow). (B and C) Histopathological slides show papillary glandular pattern with always apparent myoepithelial layer (Haematoxylin and eosin stain, ×40 and ×200, respectively).
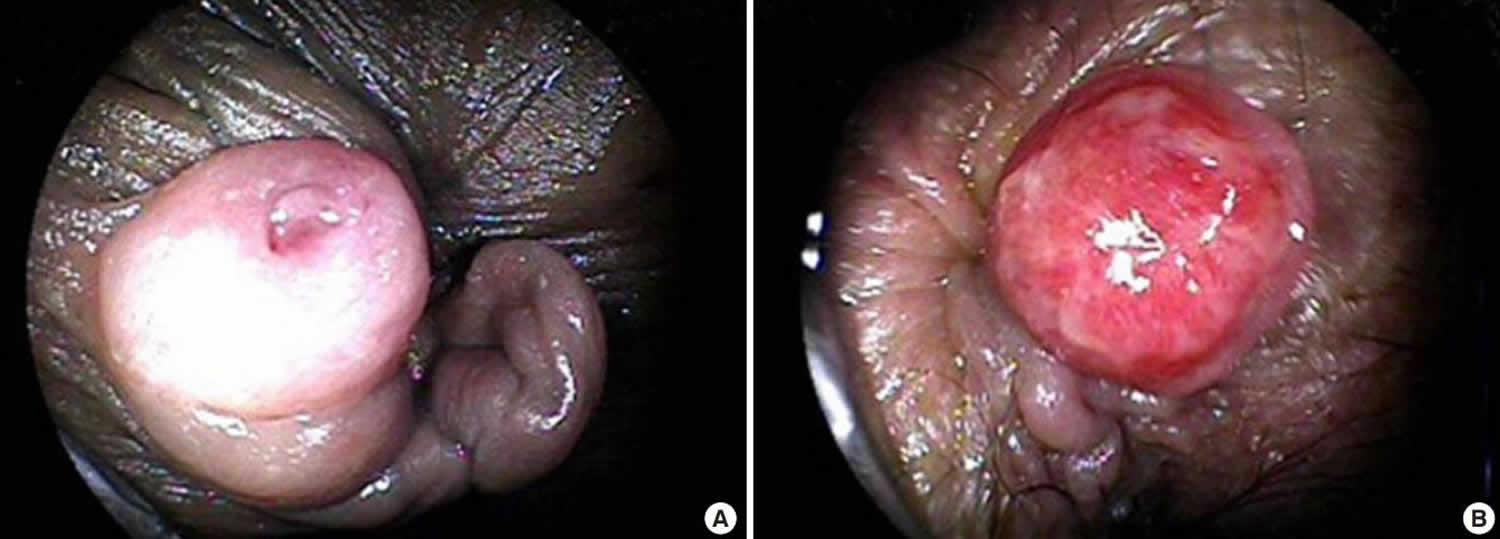
[Source 12 ]Figure 4. Hidradenoma papilliferum of the anus
[Source 1 ]Hidradenoma papilliferum causes
The cause of hidradenoma papilliferum is unclear. Hidradenoma papilliferum occurs almost exclusively in the female anogenital area; however, there have been a few isolated reports of perianal hidradenoma papilliferum in male patients 10. Hidradenoma papilliferum tumors were previously believed to originate from apocrine sweat glands; however, some authors believe that rudimentary glandular structures, eccrine sweat glands or ectopic vulvar breast tissue could also be a possible source of the tumor 8. In support of this possibility, mammary-like glands have been documented in several nonanogenital areas such as the ears, face, chest, and scalp 13 and hidradenoma papilliferum tumors do rarely occur in nonanogenital areas, where they are referred to as ectopic hidradenoma papilliferum. The most common site of ectopic hidradenoma papilliferum is the head and neck 13 and in contrast to hidradenoma papilliferum, the incidence of ectopic hidradenoma papilliferum is nearly equal between men and women 13.
The specific predilection of hidradenoma papilliferum to the vulva and perianal area could be explained by the abundant apocrine sweat glands, especially the mammary-like glands, which are thought to be the origin of hidradenoma papilliferum 12. This is because of its similarity to intraductal papilloma of the breast. Moreover, expression of the estrogen receptor in anogenital hidradenoma papilliferum explains the lack of reported cases before puberty and sex predilection 12.
Hidradenoma papilliferum symptoms
Hidradenoma papilliferum occurs almost exclusively in middle-aged women 14 and presents as a solitary, circumscribed nodule usually less than 1 cm in diameter that may resemble hemorrhoids 15. Hidradenoma papilliferum tumor is frequently asymptomatic, though may be associated with a itching, burning sensation or pain and bleeding or discharge, especially if there is ulceration of the lesion 6.
Hidradenoma papilliferum diagnosis
Hidradenoma papilliferum diagnosis requires surgical excision and histology. Hidradenoma papilliferum is a well-circumscribed dermal nodule, usually without connection to the overlying epidermis. Microscopically, the lesions are cystic papillary tumors and are composed of proliferation of papillary fronds made of loose fibrous connective tissue lined with a double-layered epithelium. The inner layer is comprised of cuboidal myoepithelial cells and the outer is tall columnar apocrine cells with a pale eosinophilic cytoplasm, which may demonstrate decapitation secretion. Larger fronds may have a fibrous core. Fibrous tissue surrounding the tumor may be compressed to form a pseudocapsule.
Hidradenoma papilliferum treatment
Surgical excision is the treatment of choice regardless of location and size. Surgical excision of the lesion is curative and recurrence is only reported where there is incomplete excision of the primary tumor 6.
Hidradenoma papilliferum prognosis
The overall prognosis for both anogenital and ectopic hidradenoma papilliferum is good. Malignant transformation of hidradenoma papilliferum is rare, but there are a few documented cases 16.
References- Seo GJ, Seo JH, Cho KJ, Cho HS. Hidradenoma Papilliferum of the Anus: A Report of 2 Cases and Review of the Literature. Ann Coloproctol. 2019;35(6):361-363. doi:10.3393/ac.2018.08.03 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6968723
- Kaufmann, R.H., Faro, S., Brown, D., 2005. Benign Diseases of the Vulva and Vagina. Cystic Tumors, fifth ed., vol. 9. Elsevier, Inc., Philadelphia, pp. 219–221.
- Stenchever, M.A., Droegemuller, W., Herbst, L., Mishell, D., 2001. Comperhensive Gynecology. Benign Gynecologic Lesions, fourth ed., vol. 18. Mosby, Inc., Missouri, pp. 484–485.
- William DJ, Tomothy GB, Dirk ME. Andrews’ diseases of the skin, Clincal dermatology, 10th edn. Philadelphia: Saunders, 2006: p. 667–668.
- Handa Y, Yamanaka N, Inagaki H, Tomita Y. Large ulcerated perianal hidradenoma papilliferum in a young 22-year-old female. Dermatol Surg. 2003 Jul;29(7):790-2. doi: 10.1046/j.1524-4725.2003.29201.x
- Kim YJ, Lee JW, Choi SJ, et al. Ectopic hidradenoma papilliferum of the breast: ultrasound finding. J Breast Cancer. 2011;14(2):153-155. doi:10.4048/jbc.2011.14.2.153 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3148539
- Vang R, Cohen PR. Ectopic hidradenoma papilliferum: a case report and literature review. J Am Acad Dermatol 1999; 41: 115–118.
- V.D. Durairaj, H.M. Bartlett, S. Said. Malignant hidradenoma of the medial canthus with orbital and intracranial extension. Ophthalmic Plast. Reconstr. Surg., 22 (3) (2006), pp. 229-232.
- Yanoff, M., Fine, B.S., 2002. Ocular Pathology Skin and Lacrimal Drainage System, fifth ed., vol. 6. Mosby, Inc., Missouri, pp. 204–205.
- Huddleston MK, Jenkins CP, Nelson EC. Hidradenoma Papilliferum: A Case Report of an Uncommon Perianal Lesion. Am Surg. 2016 Feb;82(2):E43-4.
- Lee, E., Shin, M., Haw, C., & Lee, M. (2010). Two cases of hidradenoma papilliferum of the nose. Acta dermato-venereologica, 90 3, 322-3.
- Periocular hidradenoma papilliferum. Saudi Journal of Ophthalmology Volume 23, Issues 3–4, October 2009, Pages 211-213. https://doi.org/10.1016/j.sjopt.2009.10.005
- Vang R, Cohen PR. Ectopic hidradenoma papilliferum: a case report and review of the literature. J Am Acad Dermatol. 1999 Jul;41(1):115-8. doi: 10.1016/s0190-9622(99)70418-4
- Daniel F, Mahmoudi A, de Parades V, Fléjou JF, Atienza P. An uncommon perianal nodule: hidradenoma papilliferum. Gastroenterol Clin Biol. 2007 Feb;31(2):166-8. doi: 10.1016/s0399-8320(07)89349-3
- MEEKER JH, NEUBECKER RD, HELWIG EB. Hidradenoma papilliferum. Am J Clin Pathol. 1962 Feb;37:182-95. doi: 10.1093/ajcp/37.2.182
- Vazmitel M, Spagnolo DV, Nemcova J, Michal M, Kazakov DV. Hidradenoma papilliferum with a ductal carcinoma in situ component: case report and review of the literature. Am J Dermatopathol. 2008 Aug;30(4):392-4. doi: 10.1097/DAD.0b013e31817c6a7d