Patella fracture
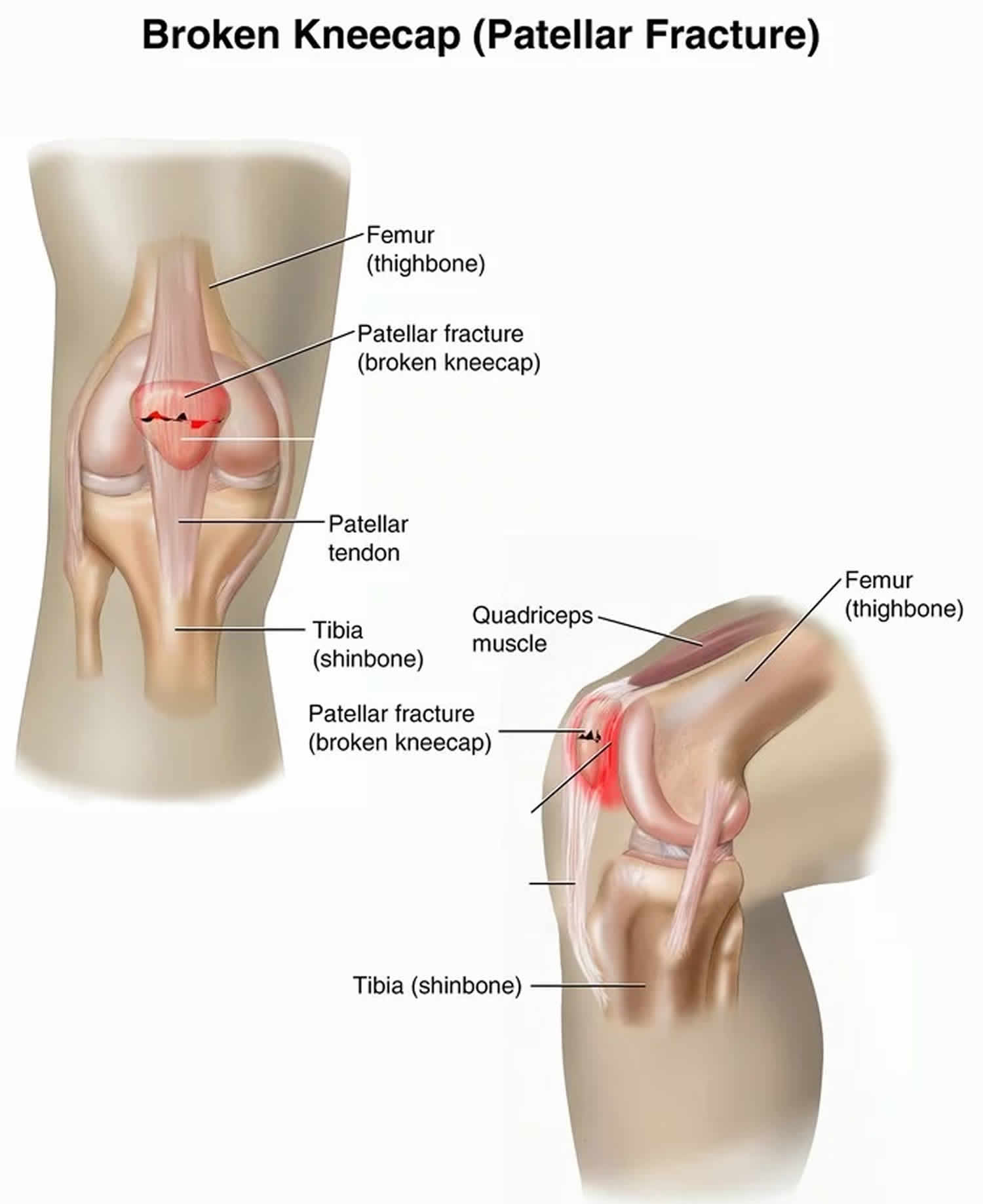
A patella fracture is a break in the patella or kneecap, the small bone that sits at the front of your knee (see Figures 1 and 2). Patella fracture occurs most often from a fall directly onto the kneecap. Because the patella acts as a shield for your knee joint, it is vulnerable to fracture if you fall directly onto your knee or hit it against the dashboard in a vehicle collision. A patellar fracture is a serious injury that can make it difficult or even impossible to straighten your knee or walk.
Some simple patellar fractures can be treated by wearing a cast or splint until the bone heals. In most patellar fractures, however, the pieces of bone move out of place when the injury occurs. For these more complicated fractures, surgery is needed to restore and stabilize the kneecap and allow for the return of function.
Fractures of the patella account for approximately 1% of all fractures 1. They occur more commonly in males. Open injuries account for 6% to 9% of patella fractures and are commonly associated with other injuries given the high energy mechanism 2. In a small percentage of the population, a secondary ossification center in the patella, most commonly at the superolateral patellar edge, may fail to fuse, resulting in a bipartite patella 3. On radiographs, they may be mistaken for a fracture. In 50% of patients with this condition, the bipartite patella is found in both knees 3.
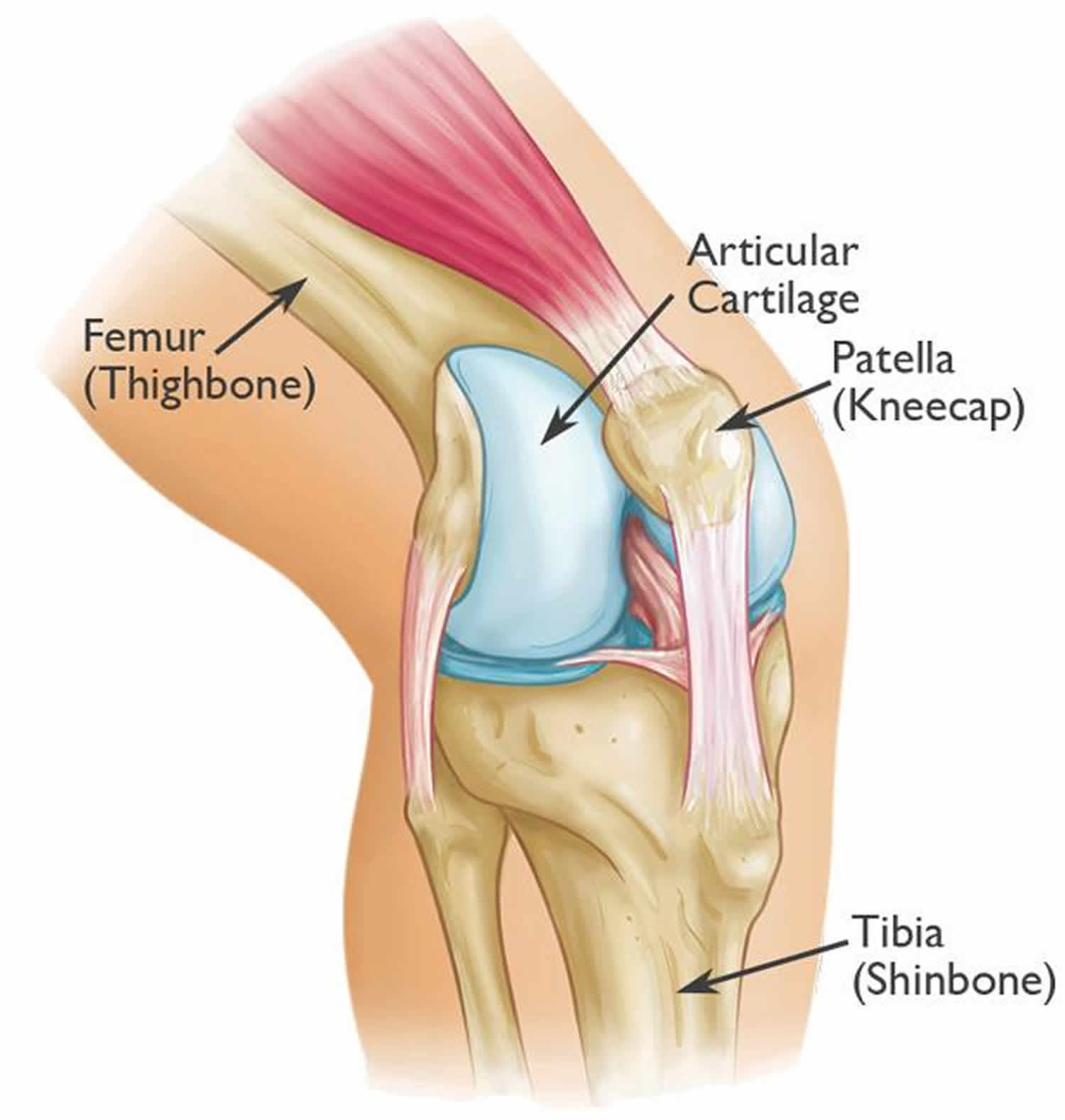
The patella (kneecap) is the largest sesamoid bone in your human body 4 and is one of 3 bones that make up the knee joint. The patella is a small bone located in front of the knee joint — where the thighbone (femur) and shinbone (tibia) meet. It protects the knee and connects the muscles in the front of the thigh to the tibia.
The patella (kneecap) runs in a groove at the end of the femur (thigh bone) and is covered by very thick articular cartilage on its undersurface. The posterior aspect of the patella contains a thick cartilage layer, which is the thickest cartilage in your body and this cartilage helps the bones glide easily along each other as you move your knee. A vertical ridge separates the medial and lateral facets of the articular surface and articulates with the femoral trochlea 1. The patella protects the front (anterior) aspect of your knee joint, serves as the insertion for the quadriceps tendon, and functions as a fulcrum to maximize the efficiency of the extensor mechanism 5. The patella (kneecap) has a very important function with the ability to straighten the knee. The inferior pole of the patella attaches to the patella tendon. The patellar retinaculum is formed by contributions from the fascia lata, vastus medialis, and vastus lateralis. The patella receives centripetal blood supply from the geniculate arteries, with the superior vessels lying anterior to the quadriceps tendon and the inferior vessels passing posterior to the patellar tendon 6. The most important blood supply to the patella penetrates the inferior pole along the fat pad below the patella.
Figure 1. Patella
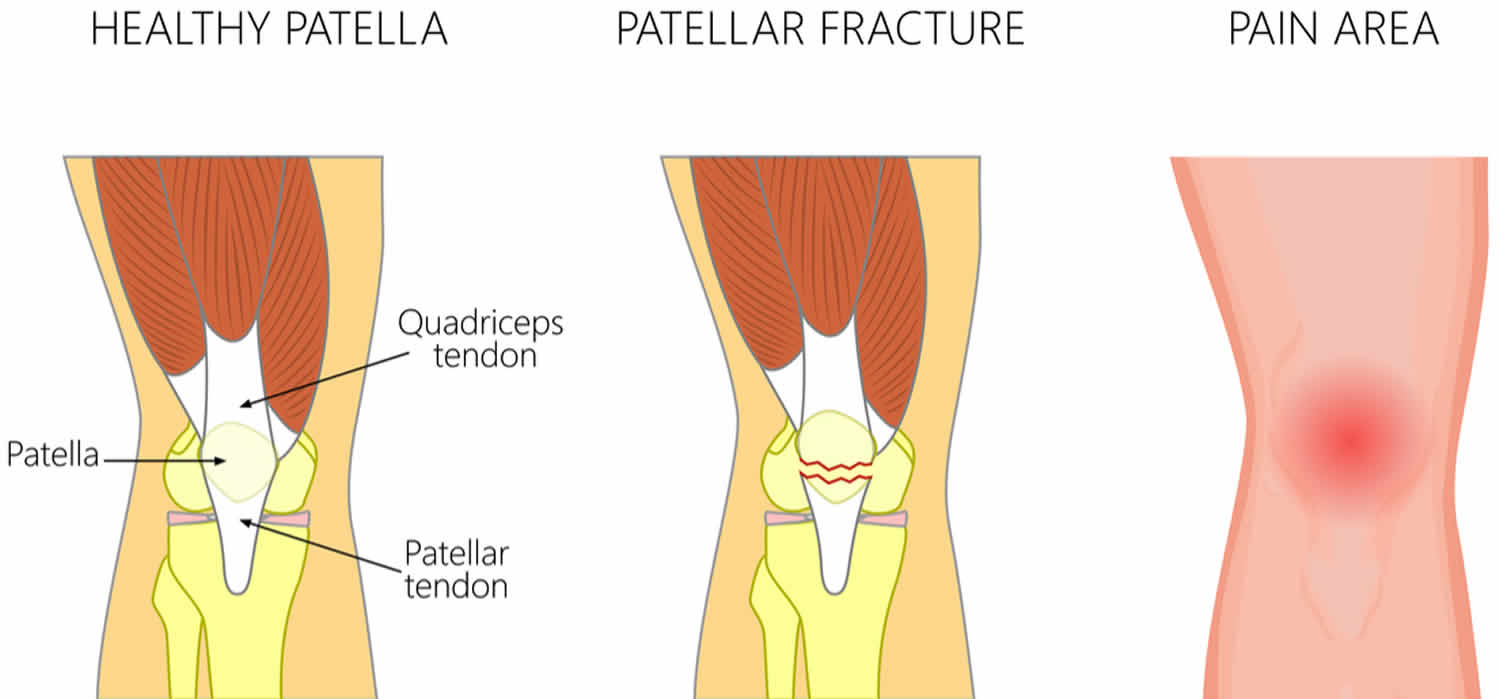
Figure 2. Patella fracture
Patella fracture types
The patella can fracture in many ways. A fracture may be a simple, clean, two-piece break or the bone can break into many pieces.
A break can occur at the top, center, or lower part of the bone. Sometimes, fractures occur in more than one area of the kneecap.
Stable patella fracture
Stable patella fracture is nondisplaced. The pieces of bone may remain in contact with each other or be separated by just a millimeter or two. In a stable fracture, the bones usually stay in place during healing.
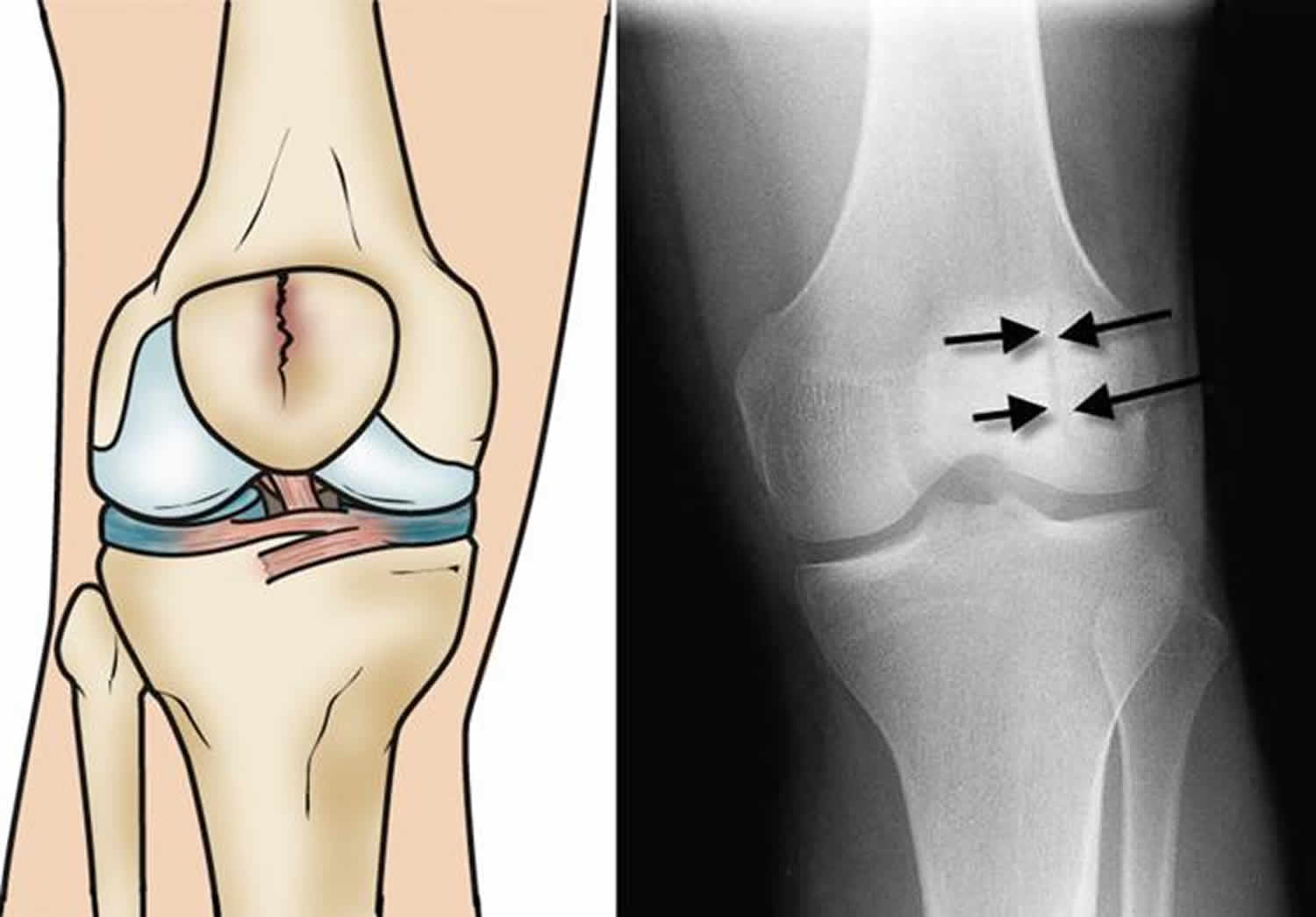
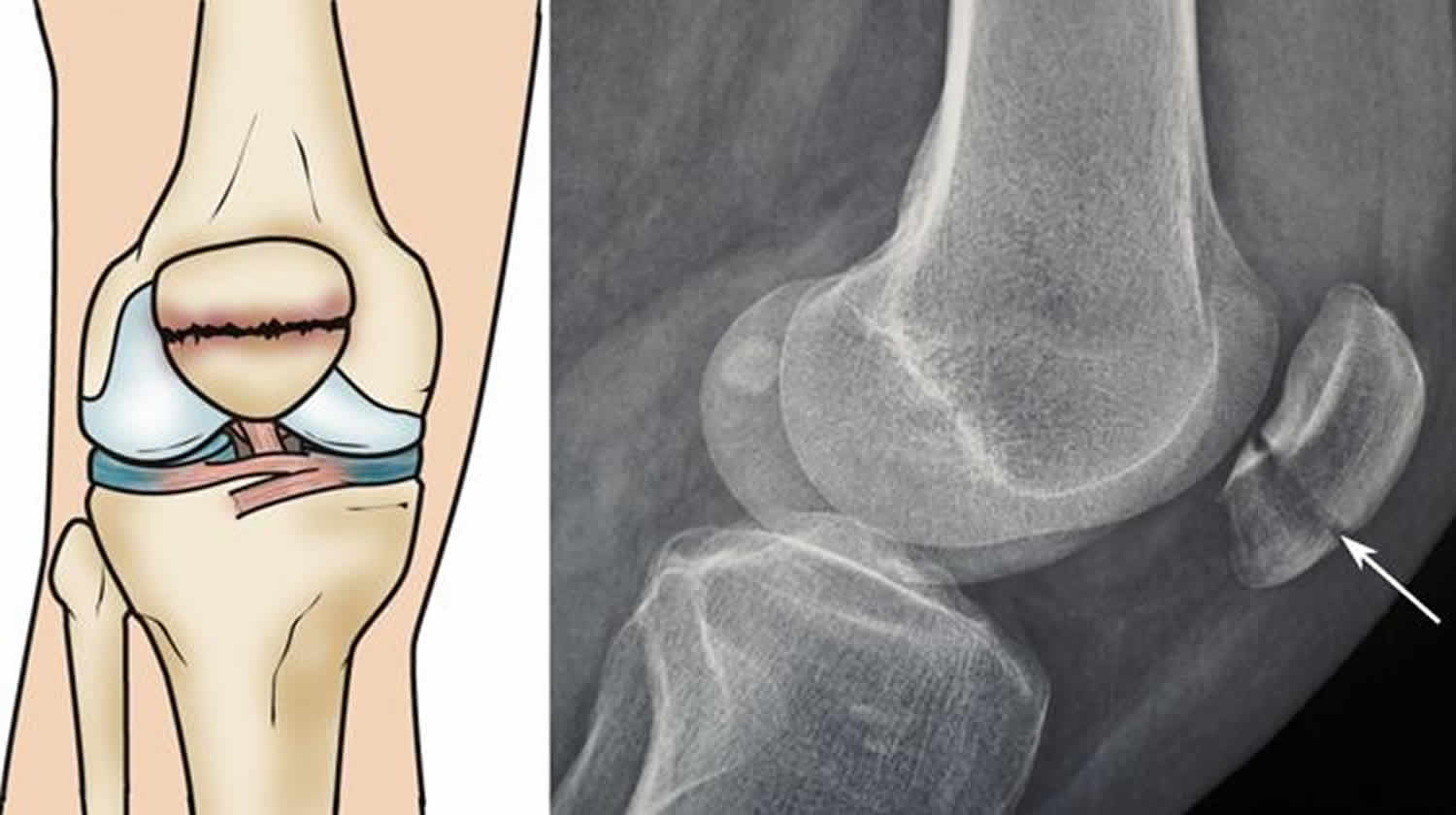
Figure 3. Stable patella fracture (illustration and x-ray show a vertical, stable fracture of the patella)
Displaced patella fracture
In a displaced patella fracture, the broken ends of the bone are separated and do not line up correctly. The normally smooth joint surface may also be disrupted. This type of fracture often requires surgery to put the pieces of bone back together.
Figure 4. Displaced patella fracture
Footnote: Illustration and x-ray show a front (left) and side (right) view of a two-part fracture across the patella (transverse fracture) with slight displacement between the broken pieces of bone.
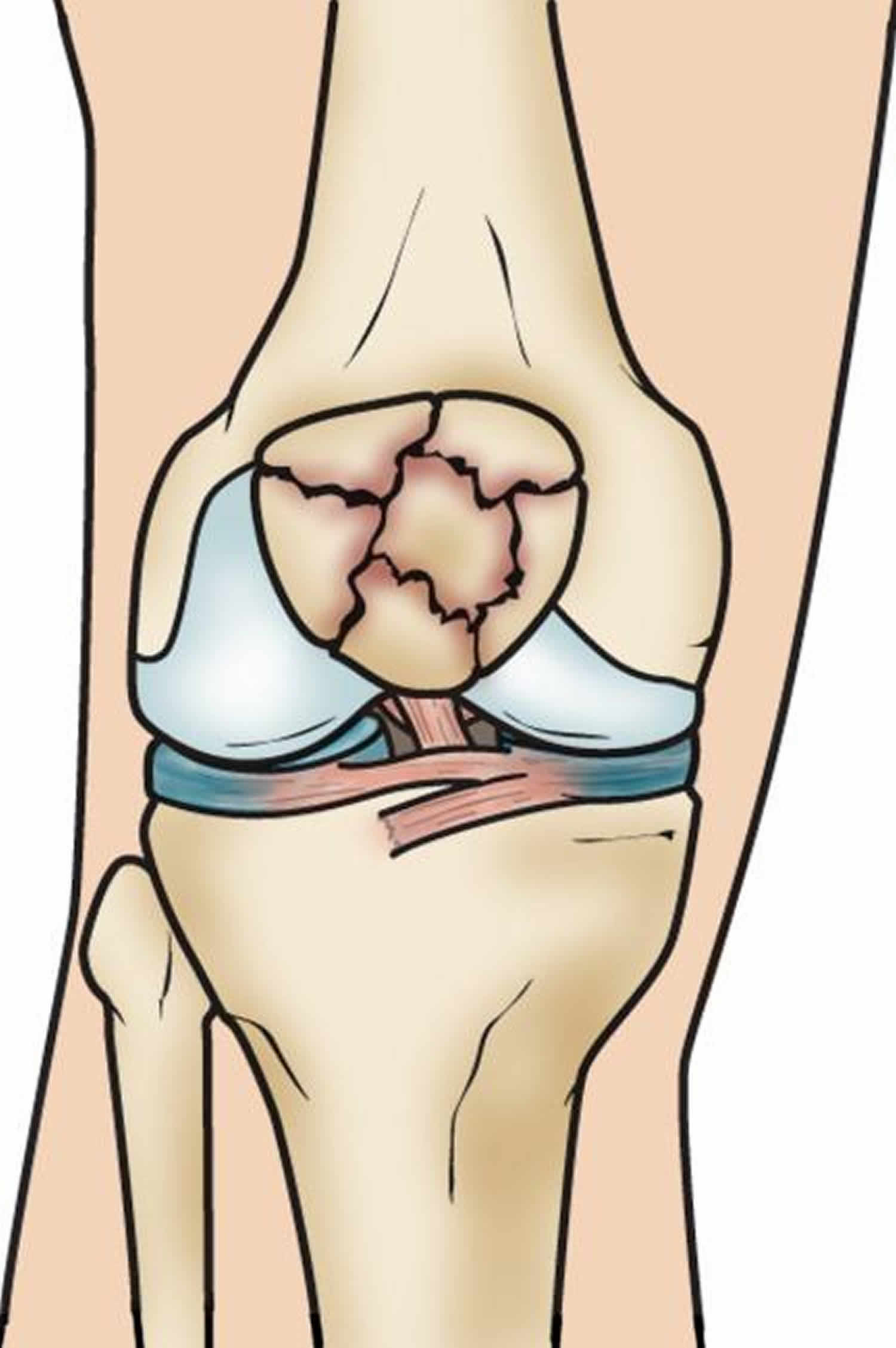
Comminuted patella fracture
In comminuted patella fracture, the bone shatters into three or more pieces. Depending on the specific pattern of the fracture, a comminuted fracture may be either stable or unstable.
Figure 5. Comminuted patella fracture
Open patella fracture
In an open patella fracture, the bone breaks in such a way that bone fragments stick out through the skin or a wound penetrates down to the bone. An open fracture often involves damage to the surrounding soft tissues and may take a longer time to heal.
Open fractures are particularly serious because, once the skin is broken, there is a higher risk for infection in both the wound and the bone. Immediate treatment is required to prevent infection.
Patella fracture causes
The cause of a fractured patella are either direct injuries (eg falling on the knee) or indirect injuries (eg sudden contraction of the quadriceps muscle). This most commonly occurs in males between the ages of 20-50 years old.
Patella fractures are most often caused by:
- Falling directly onto the knee
- Receiving a sharp blow to the knee, such as might occur during a head-on vehicle collision if your kneecap is driven into the dashboard
The patella can also be fractured indirectly. For example, a sudden contraction of the quadriceps muscle in the knee can pull apart the patella.
Risk factors for patella fracture
These can increase your chance of a patella fracture:
- Advanced age
- Postmenopause
- Decreased muscle mass
- Osteoporosis (decreased bone mass)
- Participation in contact sports (eg, football, soccer)
- Obesity, which places strain on muscles, bones, tendons, and ligaments
- Violence, such as car or car-pedestrian accidents.
Patella fracture prevention
As patella fracture usually caused by trauma some form of protective padding over the knees can be helpful. This is especially true for those people who engage in activities and sports that might lead them to fall on their knees, such as skateboarders and handball players.
Patella fracture symptoms
The most common symptoms of a patellar fracture are pain, swelling and tenderness in the front ofyour knee. Other symptoms may include:
- Bruising
- Inability to straighten the knee or keep it extended in a straight leg raise
- Inability to walk
If the fracture is completely across the patella a gap may be felt in the kneecap.
Patella fracture complications
Patella fracture complications include:
- Stiffness of your knee
- Infection if there is an open wound
- Increased chance of osteoarthritis
Patella fracture diagnosis
After discussing your symptoms and medical history, your doctor will examine your knee. The edges of the fracture can often be felt through the skin, particularly if the fracture is displaced.
During the exam, your doctor will check for hemarthrosis. In this condition, blood from the fractured bone ends collects inside the joint space, causing painful swelling. If you have a large amount of blood in your knee, your doctor may drain it to help relieve your pain.
Your doctor will also order x-rays to help diagnose your fracture.
X-rays
X-rays provide images of dense structures, such as bone. Your doctor will order x-rays from a number of different angles to look for a fracture and to view the alignment of the bones.
Radiographic evaluation with anteroposterior (AP) and lateral knee radiographs should be obtained. Lateral views are useful to assess for displacement of the patellar fragments. Advanced imaging of patellar fractures is rarely warranted. Imaging of bipartite patella most commonly demonstrates a fragment at the superolateral pole. They can be differentiated from acute fractures by the appearance of smooth edges. Imaging of the contralateral knee may reveal a bilateral bipartite patella in up to 50% of cases 3.
Although rare, a person may be born with extra bones in the patella that have not grown together. This condition is called bipartite patella and it can be mistaken for a fracture. X-rays will help to identify bipartite patella. Since many people have the condition in both knees, your doctor may take an x-ray of your other knee, as well.
Patella fracture treatment
Patella fracture treatment can be either non-surgical or surgical.
Nonsurgical treatment
If the pieces of bone are not out of place (displaced), you may not need surgery. Nonoperative management is indicated for minimally displaced fractures (less than 2 to 3 mm of step-off and less than 1 to 4 mm fracture gap) with the extensor mechanism in continuity 7. Your doctor may place your knee in a cast or splint to keep your knee straight and help prevent motion in your leg. This will keep the broken ends of bone in proper position while they heal. This cast may need to be worn for six weeks. After that, you will wear a knee brace and do physical therapy. You may need to use a cane or a crutch .
Depending upon your specific fracture, you may be allowed to bear weight on your leg while wearing a cast or brace. With some fractures, however, weight bearing is not allowed for 6 to 8 weeks. Your doctor will talk with you about restrictions on weight bearing.
Patients with displaced patellar fractures who are not medically or psychologically fit for surgery may also undergo a trial of nonoperative treatment. A long-leg splint, knee immobilizer, or hinged knee brace locked in extension can be used to stabilize the fracture while allowing early weight-bearing.
Your doctor may also recommend pain medication to reduce pain and swelling.
Physical therapy is recommended after the pain subsides to work on the active and active-assisted range of motion. Repeat radiographs should be obtained a week after initiation of motion exercises to evaluate for fracture displacement. Approximately six weeks after your initial injury, your doctor may start you on resistance exercises.
Patella fracture surgery
If the pieces of bone are out of place (displaced), you will most likely need surgery. Fractured patella bones that are not close together often have difficulty healing or may not heal. The thigh muscles that attach to the top of the patella are very strong and can pull the broken pieces out of place during healing.
There are two kinds of surgery that are commonly used to treat this injury:
- Open reduction-internal fixation (ORIF)—The doctor uses pins and screws to put the broken pieces back together. Open reduction and internal fixation are indicated for open fractures, substantially displaced fractures, and fractures with a loss of extensor function.
- Patellectomy—The doctor removes part of the kneecap or the entire kneecap. Every attempt should be made to preserve the patella; however, resection of all (total patellectomy) or part of the patella (partial patellectomy) may be indicated in certain situations. Biomechanical studies have demonstrated that removal of the patella decreases the quadriceps strength by 50% 8. Partial patellectomy is indicated for severely comminuted fractures of the superior or inferior pole that comprise less than 40% of the patellar height and are not amenable to fixation 9. This is performed by excising the fracture fragment and advancing the quadriceps or patellar tendon via suture tunnels or suture anchors.
Timing of surgery. If the skin around your fracture has not been broken, your doctor may recommend waiting until any abrasions have healed before having surgery.
Open fractures have an increased risk of infection and are scheduled for surgery as soon as possible, usually within hours. During surgery, the cuts from the injury and the surfaces of the bone are thoroughly cleaned out. The bone will typically be repaired during the same surgery. Antibiotic treatment are also indicated for open fractures.
Postoperatively, similar to nonoperative treatment, patients are placed in a hinged knee brace locked in extension and are allowed to weight-bear as tolerated after surgical fixation. Early knee motion is usually begun at the first follow-up visit to prevent stiffness. As the pain diminishes, knee motion is progressed, and isometric strengthening of the quadriceps is initiated. The rehabilitation protocol may vary after a partial patellectomy or a tenuous fixation by delaying knee motion to ensure adequate healing.
Patella fracture surgical procedures
The type of procedure performed often depends on the type of patella fracture you have. Before the surgery, your doctor will discuss your procedure with you, as well as any potential complications.
Transverse patella fracture
These two-part fractures are most often fixed in place using screws or pins and wires and a “figure-of-eight” configuration tension band. The figure-of-eight band presses the two pieces together.
This procedure is best for treating fractures that are located near the center of the patella. Fracture pieces at the ends of the kneecap are too small for this procedure. Breaks that are in many pieces can be overcompressed by the tension band.
Another approach to a transverse fracture is to secure the bones using small screws or small screws and small plates.
Comminuted patella fracture
In some patella fractures, the top or more commonly, the bottom of the patella is broken into several small pieces. This type of fracture occurs when the kneecap is first pulled apart from the injury, and is then crushed when the patient falls on it. Because the bone fragments are too small to be fixed back into place, your doctor will remove them (patellectomy). He or she will then attach the loose patellar tendon back to the remaining patellar bone.
If the kneecap is broken in many pieces at its center and the pieces are separated, your doctor may use a combination of wires and screws to fix it. Removing small portions of the kneecap that cannot be reconstructed may also have good results. Complete removal of the kneecap is a last resort in treating a comminuted fracture.
Patella fracture surgery complications
Postoperative complications include symptomatic hardware or implant failure 2 and wire migration 10 and knee stiffness 11. Nonunion and infection are rare complications but are more likely in open fractures 12. The rate of osteonecrosis of the patella following fractures is reportedly as high as 25%; however, this has not significantly affected clinical outcomes 6.
Patella fracture recovery
How long it takes to recover after a patella fracture will depend upon a number of factors, including:
- The severity of your injury
- Whether your treatment was surgical or nonsurgical
- The time needed for rehabilitation
Most patients will be able to return to their normal activities within 3 to 6 months. For patients with severe fractures, the return to activity may take longer.
Your doctor may suggest some lifestyle changes to help protect your knee and prevent future problems. This may include avoiding activities that involve repetitive deep knee bending or squatting. Climbing stairs or ladders should be avoided, as well.
Pain management
Most fractures hurt moderately for a few days to a couple of weeks. Many patients find that using ice, elevating the affected leg, and taking simple, non-prescription medications for pain relief are all that are needed to relieve pain.
If your pain is severe, your doctor may suggest a prescription-strength medication, such as an opioid, for a few days.
Be aware that although opioids help relieve pain after surgery, opioid dependency and overdose has become a critical public health issue. For this reason, opioids are typically prescribed for a short period of time. It is important to use opioids only as directed by your doctor. As soon as your pain begins to improve, stop taking opioids.
Rehabilitation
Whether your treatment is surgical or nonsurgical, rehabilitation will play a vital role in getting you back to your daily activities.
Because treatment for a patellar fracture can sometimes require keeping your leg immobilized in a cast for a long period of time, your knee may become stiff and your thigh muscles may become weak.
During rehabilitation, your doctor or a physical therapist will provide you with specific exercises to help:
- Improve range of motion in your knee
- Strengthen your leg muscles
- Decrease stiffness
Weight Bearing
Your doctor will tell you when you can begin to bear weight on your leg. Initial weight-bearing exercise is usually limited to gently touching your toe to the floor. As your injury heals and your muscles strengthen, you will gradually be able to put more weight on your leg.
Patella fracture long term complications
Even after successful treatment, some patients with patellar fractures may experience long-term complications.
Posttraumatic arthritis
Posttraumatic arthritis is a type of arthritis that develops after an injury. Even when your bones heal normally, the articular cartilage covering the bones can be damaged, leading to pain and stiffness over time. Severe arthritis occurs in a small percentage of patients with patellar fractures. Mild to moderate arthritis—a condition called chondromalacia patella—is much more common.
Muscle weakness
Some patients may have permanent weakness of the quadriceps muscle in the front of the thigh after a fracture. Some loss of motion in the knee, including both straightening (extension) and bending (flexion), is also common. This loss of motion is not usually disabling.
Chronic pain
Long-term pain in the front of the knee is common with patellar fractures. While the cause of this pain is not completely understood, it is likely that it is related to posttraumatic arthritis, stiffness, and muscle weakness. Some patients find that they are more comfortable wearing a knee brace or support.
References- Boström A. Fracture of the patella. A study of 422 patellar fractures. Acta Orthop Scand Suppl. 1972;143:1-80.
- Anand S, Hahnel JC, Giannoudis PV. Open patellar fractures: high energy injuries with a poor outcome? Injury. 2008 Apr;39(4):480-4.
- Atesok K, Doral MN, Lowe J, Finsterbush A. Symptomatic bipartite patella: treatment alternatives. J Am Acad Orthop Surg. 2008 Aug;16(8):455-61.
- Luo TD, Pilson H. Patella Fractures. [Updated 2019 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513330
- Kaufer H. Mechanical function of the patella. J Bone Joint Surg Am. 1971 Dec;53(8):1551-60.
- Scapinelli R. Blood supply of the human patella. Its relation to ischaemic necrosis after fracture. J Bone Joint Surg Br. 1967 Aug;49(3):563-70.
- Melvin JS, Mehta S. Patellar fractures in adults. J Am Acad Orthop Surg. 2011 Apr;19(4):198-207.
- Carpenter JE, Kasman RA, Patel N, Lee ML, Goldstein SA. Biomechanical evaluation of current patella fracture fixation techniques. J Orthop Trauma. 1997 Jul;11(5):351-6.
- Böstman O, Kiviluoto O, Nirhamo J. Comminuted displaced fractures of the patella. Injury. 1981 Nov;13(3):196-202.
- Choi HR, Min KD, Choi SW, Lee BI. Migration to the popliteal fossa of broken wires from a fixed patellar fracture. Knee. 2008 Dec;15(6):491-3.
- Smith ST, Cramer KE, Karges DE, Watson JT, Moed BR. Early complications in the operative treatment of patella fractures. J Orthop Trauma. 1997 Apr;11(3):183-7
- Catalano JB, Iannacone WM, Marczyk S, Dalsey RM, Deutsch LS, Born CT, Delong WG. Open fractures of the patella: long-term functional outcome. J Trauma. 1995 Sep;39(3):439-44.