Pityriasis amiantacea
Pityriasis amiantacea also known as tinea amintacea, asbestos scalp, porrigo amiantacea, tinea asbestina or keratosis follicularis amiantacea, is a scalp disorder in which there is excessive scaling of the scalp. Pityriasis amiantacea presents with thick, silvery or yellowish, asbestos-like scales wrapping around and binding down tufts of hair 1. The scales may resemble asbestos, giving rise to the term amiantacea – the French word for asbestos is ‘amiante’. Clinically, all pityriasis amiantacea cases present with dry, scaly lesions that may be circumscribed or diffuse, with associated itch (pruritus), redness (erythema) and nonscarring hair loss (alopecia) 2. The essential features responsible for the asbestos like scaling are diffuse hyperkeratosis and parakeratosis together with follicular keratosis, which surrounds each hair with a sheath of horn 3. Histopathology demonstrates extensive spongiosis, acanthosis, hyperkeratosis, parakeratosis, follicular keratosis, and mixed inflammatory cell infiltrate 4. Pityriasis amiantacea may occur at any age including children but is usually observed during teenage years and young adults. Pityriasis amiantacea usually begins during teenage years and progresses to more typical psoriasis in 2-15% of pediatric patients 1. It is observed in both genders, with female predominance (60%–70%) 1.
Jean-Louis-Marc Alibert in 1832 first described pityriasis amiantacea as “la porrigine amiantace’e” because its scales reminded him of the mica-like substance observed in young birds. Since then, several names including tinea amintacea, asbestos scalp, tinea asbestina, or keratosis follicularis amiantacea have been used to describe pityriasis amiantacea 1.
Pityriasis amiantacea is typically considered to be a reactive condition to several inflammatory diseases rather than a specific diagnosis. Common conditions that may present with pityriasis amiantacea include 5:
- Scalp psoriasis
- Seborrheic dermatitis
- Atopic dermatitis
- Tinea capitis.
Head lice and lichen simplex should also be considered. Pityriasis amiantacea may also be observed as a sequel or complication of streptococcal infection and lichen simplex 3.
When no underlying cause is found, the condition is often called idiopathic pityriasis amiantacea.
Some authors suggest that pityriasis amiantacea is a possible complication in infants with seborrheic dermatitis 6. Others are emphatic in pointing out that the reaction is more common among children although it can occur at any age 7. The prospective study of 85 pityriasis amiantacea cases revealed a mean age diagnosis of 23.8 years in the interval ranging from 5 to 63 – thus encompassing children and adolescents, with a female predominance 1. In this study 8, psoriasis accounted for 35.3% of the cases; aggregated seborrheic dermatitis and atopic eczema for 34.2%; tinea capitis – diagnosed by mycological examination – for 12.9% of cases.
Figure 1. Pityriasis amiantacea (scalp psoriasis)
Footnote: Focal masses of thick, adherent, asbestos like yellow brown scales over fronto-parietal and vertex region of scalp.
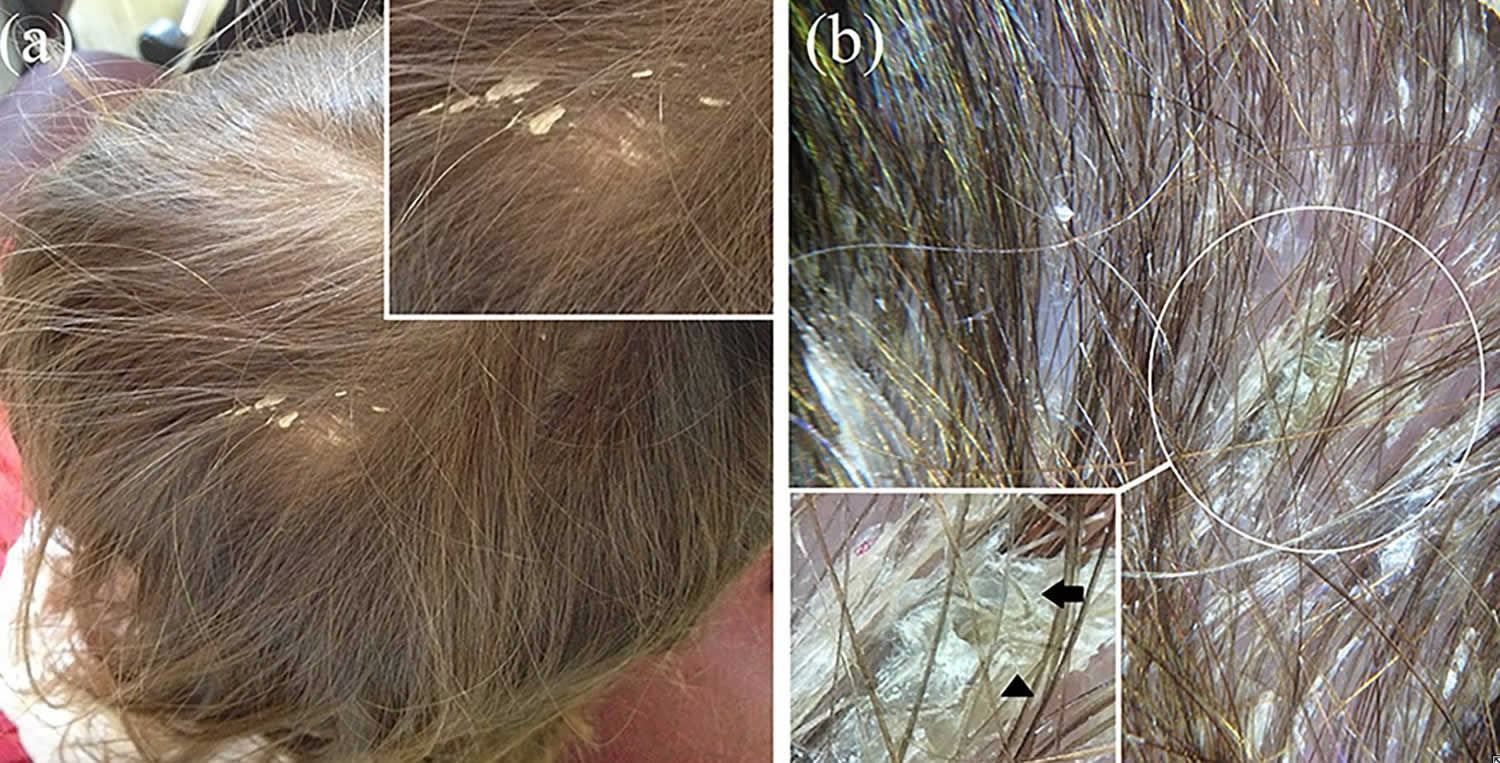
[Source 2 ]Figure 2. Pityriasis amiantacea (tinea capitis)
Footnote: Physical examination shows thick, whitish, asbestos-like scales surrounding and binding the hair on the right parietal region of the scalp (better visible in the box) (a). Polarized light dermoscopic examination displays white scales and compact white keratotic material adhering to tufts of hair (asbestos-like scaling) without erythema; “question mark” (black arrow in the box) and “zigzag” (hair shaft bent at more than one point—black arrowhead in the box) hairs are also visible (b).
[Source 5 ]Is pityriasis amiantacea contagious?
It depends on the underlying cause of pityriasis amiantacea. Pityriasis amiantacea is a reaction pattern rather than a specific diagnosis. Common conditions that may present with pityriasis amiantacea include:
- Scalp psoriasis
- Seborrheic dermatitis
- Atopic dermatitis
- Tinea capitis.
Head lice and lichen simplex should also be considered. Pityriasis amiantacea may also be observed as a sequel or complication of streptococcal infection and lichen simplex 3.
When no underlying cause is found, the condition is often called idiopathic pityriasis amiantacea.
Microorganisms’ role in pityriasis amiantacea development has been debated. Staphylococci are isolated as colonizers in up to 97% of the pityriasis amiantacea patients, more commonly Staphylococcus aureus, followed by coagulase-negative staphylococci and micrococci 1. In addition, diverse species of fungus, including Microsporum canis, Trichophyton violaceum, Trichophyton rubrum, Trichophyton schoenleinii, and Trichophyton verrucosum, have been demonstrated in some reports 9. These microorganisms could be also implicated in the maintenance of the disease, producing epidermal cell differentiation inhibitors, leading to perpetuate the disease 10. Thus, the use of antibiotics plays a fundamental role in the treatment and/or prevention of pityriasis amiantacea recurrences 9. The most commonly used antibiotic is ketoconazole 2% shampoo and oral griseofulvin (10 mg/kg). These medications have been associated with removal of scales after 2–3 months of treatment 10.
In addition to the antimicrobial therapy, patients with pityriasis amiantacea require topical oil-based products to facilitate removal of the thick scales and crusts. Salicylic acid 5%–10% ointment is the most commonly employed. In severe cases, high-potency topical corticosteroids are beneficial (betamethasone dipropionate 0.1% solution) 11. In extensive and persistent disease, topical and oral retinoids are usually necessary taking precautions because of their teratogenicity 1.
Pityriasis amiantacea causes
Pityriasis amiantacea is a reaction pattern rather than a specific diagnosis. Common conditions that may present with pityriasis amiantacea include:
- Scalp psoriasis
- Seborrheic dermatitis
- Atopic dermatitis
- Tinea capitis.
Head lice and lichen simplex should also be considered. Pityriasis amiantacea may also be observed as a sequel or complication of streptococcal infection and lichen simplex 3.
When no underlying cause is found, the condition is often called idiopathic pityriasis amiantacea.
Several factors have been implicated in pityriasis amiantacea development such as drugs, anxiety, and abrupt changes in the environmental conditions 12. Some descriptive data support a probable participation of tumor necrosis factor-alpha (TNF-α) and interferon-α in the pathogenesis of pityriasis amiantacea 12. In patients with Crohn’s disease treated with TNF-α inhibitors, a stimulation of alternative pro-inflammatory pathways, including up-regulation of the IL-1 family, potential generation of autoreactive T cells, and keratinocyte proliferation, was observed 13.
Other medications associated with the development of pityriasis amiantacea include the inhibitor of the mutated BRAF gene (vemurafenib) for melanoma 14. A careful understanding of these drug reactions could provide insights to prevent the development of pityriasis amiantacea lesions and also to allow an early diagnosis and management. However, one must keep in mind that cutaneous adverse effects can appear with variable time lapse. In case studies, the authors observed that pityriasis amiantacea was triggered after the use of valproic acid, a glycogen synthase kinase-3β (GSK-3β) inhibitor that stabilizes cytoplasmic β-catenin and facilitates the activation of the Wnt/β-catenin pathway 15. Valproic acid was started to manage a chronic epileptic disorder. Valproic acid GSK-3β inhibition promotes keratinocyte growth, especially in hair follicles, where its participation is critical for enhancing the proliferative activity of the dermal papilla and promoting the elongation of the hair shaft 16. This proliferative capacity has made valproic acid a candidate for the treatment of alopecia 15. Indirectly, valproic acid is also able to induce alkaline phosphatase similar to minoxidil 17. In addition, valproic acid also induces growth factors such as insulin-like growth factor-1, fibroblast growth factor-10, and the follicular stem cell markers keratin-15 and CD34 18. However, because of the rarity of pityriasis amiantacea, no cases of the association of pityriasis amiantacea with valproic acid have been published 19.
Microorganisms’ role in pityriasis amiantacea development has been debated. Staphylococci are isolated as colonizers in up to 97% of the pityriasis amiantacea patients, more commonly Staphylococcus aureus, followed by coagulase-negative staphylococci and micrococci 1. In addition, diverse species of fungus, including Microsporum canis, Trichophyton violaceum, Trichophyton rubrum, Trichophyton schoenleinii, and Trichophyton verrucosum, have been demonstrated in some reports 9. These microorganisms could be also implicated in the maintenance of the disease, producing epidermal cell differentiation inhibitors, leading to perpetuate the disease 10. Thus, the use of antibiotics plays a fundamental role in the treatment and/or prevention of pityriasis amiantacea recurrences 9. The most commonly used antibiotic is ketoconazole 2% shampoo and oral griseofulvin (10 mg/kg). These medications have been associated with removal of scales after 2–3 months of treatment 10.
In addition to the antimicrobial therapy, patients with pityriasis amiantacea require topical oil-based products to facilitate removal of the thick scales and crusts. Salicylic acid 5%–10% ointment is the most commonly employed. In severe cases, high-potency topical corticosteroids are beneficial (betamethasone dipropionate 0.1% solution) 11. In extensive and persistent disease, topical and oral retinoids are usually necessary taking precautions because of their teratogenicity 1.
Table 1. Identifying the cause of pityriasis amiantacea
| Skin condition | Description |
| Psoriasis | Well-defined red scaly plaques on elbows and knees (chronic plaque psoriasis) Red shiny patches in skin folds (flexural psoriasis) Nail pitting, yellowing or thickening due to nail psoriasis Psoriatic arthritis |
| Seborrheic dermatitis | Patches similar to psoriasis but less well-defined and less red Scale tends to be yellowish in color Affects eyebrows, nasal crease, behind the ears and chest |
| Atopic dermatitis | Usually starts in infancy Skin folds of arms and legs often affected May have generally itchy dry skin Flare-ups result in red, blistered, scratched patches |
| Tinea capitis | Fungal culture reveals dermatophyte fungus Localized scaly bald patches Broken off or loose hairs There may be cervical lymph node enlargement |
| Head lice | Egg cases on hair shaft (nits) and scurrying lice Prominent on back of neck and behind ears There may be cervical lymph node enlargement |
| Lichen simplex | Localized itchy dry patch of skin Often at back or one side of scalp Thickened, darkened plaques with broken-off hairs due to scratching |
Pityriasis amiantacea differential diagnosis
Pityriasis amiantacea differential diagnosis include:
- Scalp psoriasis
- Seborrheic dermatitis
- Atopic dermatitis
- Tinea capitis
Other concretions around the hair shaft:
- White piedra – many soft, fluffy white or light brown nodules are seen; more commonly affects pubic hair, axillary hair, beard and mustache area. Scalp is occasionally involved.
- Black piedra – usually affects scalp hair. Small compact black nodular concretions, often multiple on one hair, are seen.
- Trichomycosis axillaris – long, thin yellow or orange concretions may spiral around hair shafts of axillary or pubic hair.
- Nits (head lice) – nits adhere to the proximal portions of affected hair. They are small and white. Associated adult lice attach to any portion of the hair shaft.
Pityriasis amiantacea prevention
Pityriasis amiantacea is a reaction pattern rather than a specific diagnosis. Common conditions that may present with pityriasis amiantacea include:
- Scalp psoriasis
- Seborrheic dermatitis
- Atopic dermatitis
- Tinea capitis.
Head lice and lichen simplex should also be considered.
When no underlying cause is found, the condition is often called idiopathic pityriasis amiantacea.
Therefore, pityriasis amiantacea cannot be prevented.
Pityriasis amiantacea signs and symptoms
Pityriasis amiantacea is characterized by thick scales wrapping around and binding down tufts of hair. The scaling may be localized or generalized depending on the underlying condition and its duration.
Pityriasis amiantacea may be complicated by secondary staphylococccal infection (impetiginization), when the skin becomes sticky, oozy and crusted. Temporary or permanent hair loss (alopecia) may also occur.
If the underlying skin condition is not clear, the entire skin should be examined to uncover the cause of pityriasis amiantacea. This enables targeted therapy against the specific disease and prevents long term complications such as permanently bald areas.
Pityriasis amiantacea diagnosis
Skin and hair samples for mycology and bacterial culture may be useful. Skin biopsy is rarely necessary.
Pityriasis amiantacea treatment
Pityriasis amiantacea treatment depends on the specific underlying disease.
- Mineral or vegetable oils especially olive oil may help to loosen the adherent scales.
- Washable leave-on creams or wash-off shampoos containing salicylic acid, coal tar and sulphur may be of help in reducing the scaling and inflammation, e.g. coconut compound ointment.
- Intermittent courses of topical steroids are useful for psoriasis and various types of dermatitis, often as lotions or gels.
- Antifungal shampoo (e.g. ketoconazole or ciclopirox) is often prescribed and may be helpful for underlying seborrhoeic dermatitis.
- Oral antifungal agents are necessary for confirmed tinea capitis infection.
- Oral antibiotics may be prescribed for bacterial infection.
Idiopathic pityriasis amiantacea often clears completely with treatment and does not recur. Tinea capitis may be cured by appropriate antifungal treatments. However, pityriasis amiantacea or less severe scalp scaling tends to persist or reappear when it is due to a chronic skin condition such as psoriasis or seborrhoeic dermatitis.
References- Abdel-Hamid IA, Agha SA, Moustafa YM, El-Labban AM. Pityriasis amiantacea: a clinical and etiopathologic study of 85 patients. Int J Dermatol. 2003;42(4):260–4. doi: 10.1046/j.1365-4362.2003.01755.x
- Gupta LK, Khare AK, Masatkar V, Mittal A. Pityriasis amiantacea. Indian Dermatol Online J. 2014;5(Suppl 1):S63-S64. doi:10.4103/2229-5178.144550 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4252962
- Paller AS, Mancini AJ. Hurwitz Clinical Pediatric Dermatology. A Textbook of Skin Disorders of Childhood and Adolescence. 3rd ed. Philadelphia: Elsevier-Saunders; 2006. Papulosquamous and related disorders; pp. 85–106.
- Knight AG. Pityriasis amiantacea: A clinical and histopathological investigation. Clin Exp Dermatol. 1977;2:137–43.
- Errichetti E, Stinco G. Dermoscopy as a useful supportive tool for the diagnosis of pityriasis amiantacea-like tinea capitis. Dermatol Pract Concept. 2016;6(3):63-65. Published 2016 Jul 31. doi:10.5826/dpc.0603a13 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5006556
- Sampaio ALB, Mameri A, Jeunon T, Ramos-e-Silva M, Nunes AP, Carneiro S. Dermatite seborreica. An Bras Dermatol. 2011;86:1061–1074.
- Pereira JM. Belda W, Junior, Di Chiacchio N, Criado PR. Tratado de Dermatologia. 2. ed. São Paulo: Editora Atheneu; 2014. Tricologia – Avaliação dos pelos, doenças congênitas e hereditárias; pp. 945–990.
- Amorim GM, Fernandes NC. Pityriasis amiantacea: a study of seven cases. An Bras Dermatol. 2016;91(5):694-696. doi:10.1590/abd1806-4841.20164951 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5087242
- Ginarte M, Pereiro M, Jr, Fernández-Redondo V, Toribio J. Case reports. Pityriasis amiantacea as manifestation of tinea capitis due to microsporum canis. 2004;43:93–6.
- Verardino GC, Azulay-Abulafia L, Macedo PM, Jeunon T. Pityriasis amiantacea: Clinical-dermatoscopic features and microscopy of hair tufts. An Bras Dermatol. 2012;87:142–5.
- Amorim GM, Fernandes NC. Pityriasis amiantacea: A study of seven cases. An Bras Dermatol. 2016;91:694–6.
- Shiiya C, Nomura Y, Fujita Y, Nakayama C, Shimizu H. Psoriasis vulgaris with fibrokeratoma from pityriasis amiantacea. JAAD Case Rep. 2017;3:243–5.
- Ring DS, Kaplan DL. Pityriasis amiantacea: A report of 10 cases. Arch Dermatol. 1993;129:913–4.
- Bilgiç Ö. Vemurafenib-induced pityriasis amiantacea: A case report. Cutan Ocul Toxicol. 2016;35:329–31.
- Lee SH, Yoon J, Shin SH, Zahoor M, Kim HJ, Park PJ, et al. Valproic acid induces hair regeneration in murine model and activates alkaline phosphatase activity in human dermal papilla cells. PLoS One. 2012;7:e34152
- Jo SJ, Choi SJ, Yoon SY, Lee JY, Park WS, Park PJ, et al. Valproic acid promotes human hair growth in in vitro culture model. J Dermatol Sci. 2013;72:16–24.
- Wiltse J. Mode of action: Inhibition of histone deacetylase, altering WNT-dependent gene expression, and regulation of beta-catenin – developmental effects of valproic acid. Crit Rev Toxicol. 2005;35:727–38.
- Chou YC, Chao FH, Chou YH. Rapid development of severe skin rash after adding valproic acid in a case of bipolar depression treated with low-dose lamotrigine. J Formos Med Assoc. 2014;113:195–6.
- Diaz-Perez JA, Joyce JC, Cibull TL, Victor TA. Development of Pityriasis Amiantacea after Valproic Acid Therapy. Int J Trichology. 2018;10(5):237-239. doi:10.4103/ijt.ijt_53_18 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6290282