Primary ciliary dyskinesia
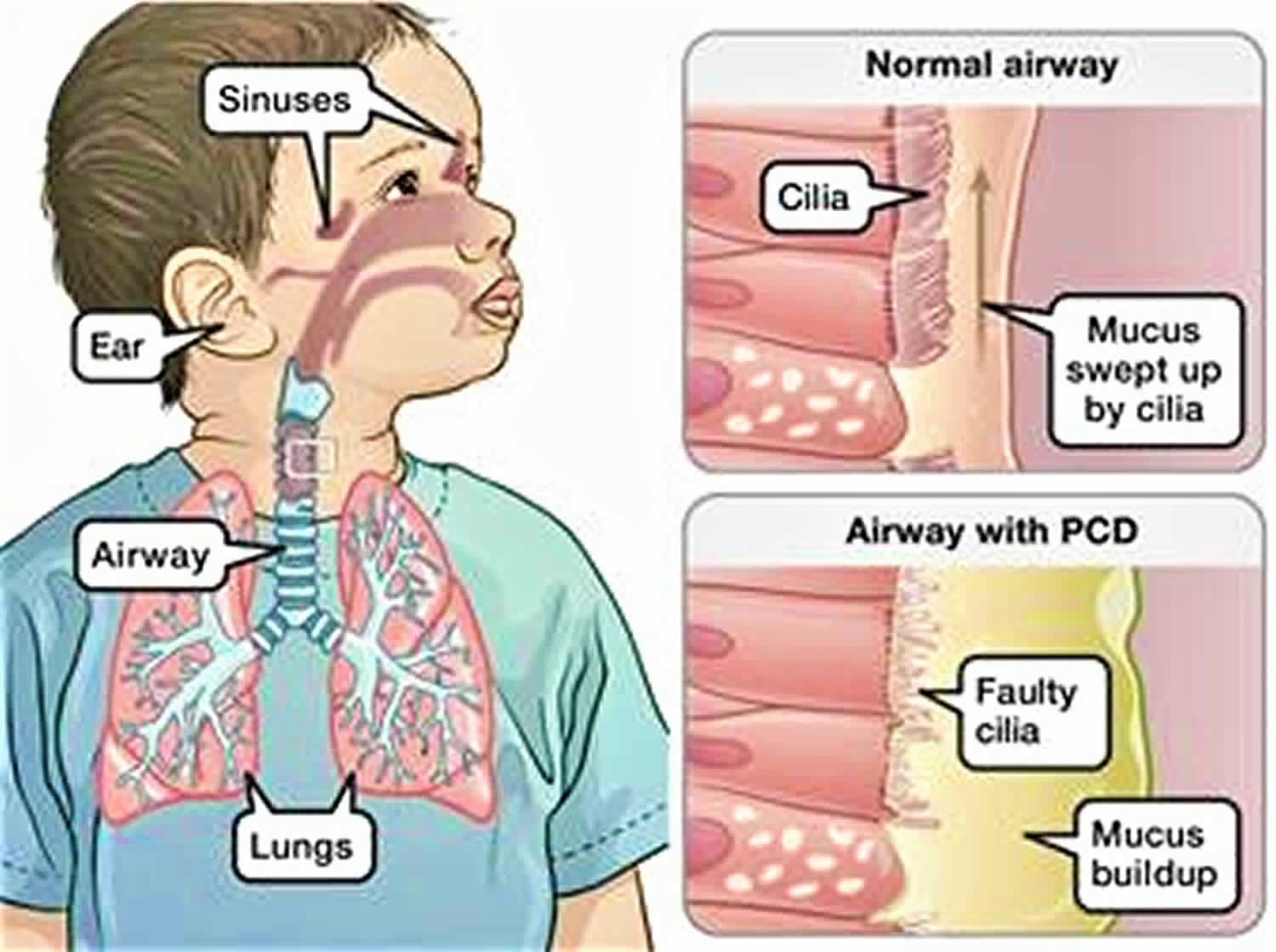
Primary ciliary dyskinesia also called immotile cilia syndrome, is a rare inherited disorder which affects the movement of tiny hair-like structures on body cells, known as cilia. Cilia normally move together in wave-like motions. They carry mucus (a slimy substance) toward the mouth to be coughed or sneezed out of the body. The mucus contains inhaled dust, bacteria, and other small particles. If the cilia don’t work well, bacteria stay in your airways. This can cause breathing problems, infections, and other disorders. Primary ciliary dyskinesia is characterized by chronic respiratory tract infections, abnormally positioned internal organs, and the inability to have children (infertility). Some people who have primary ciliary dyskinesia have breathing problems from the moment of birth. The signs and symptoms of primary ciliary dyskinesia are caused by abnormal cilia and flagella. Cilia are microscopic, finger-like projections that stick out from the surface of cells. Cilia are found in the linings of the airway, the reproductive system, and other organs and tissues. Flagella are tail-like structures, similar to cilia, that propel sperm cells forward.
It is thought that about 1/16,000 – 1/20,000 people have primary ciliary dyskinesia. The incidence is higher in Norway and Japan. In the United States, it is estimated that about 12,000 to 17,000 people have primary ciliary dyskinesia 1.
About half of all people who have primary ciliary dyskinesia have Kartagener’s syndrome 2, 3, 4. Kartagener’s syndrome involves three disorders: chronic sinusitis, bronchiectasis and situs inversus. Chronic sinusitis is a condition in which the sinuses are infected or inflamed. The sinuses are hollow air spaces around the nasal passages. Bronchiectasis is a condition in which damage to the airways causes them to widen and become flabby and scarred. Situs inversus is a condition in which the internal organs (for example, the heart, stomach, spleen, liver, and gallbladder) are in opposite positions from where they normally are. Situs inversus can occur without primary ciliary dyskinesia. In fact, only 25 percent of people who have the condition also have primary ciliary dyskinesia. By itself, situs inversus may not affect your health. However, in primary ciliary dyskinesia, it’s a sign of Kartagener’s syndrome.
In the respiratory tract, cilia move back and forth in a coordinated way to move mucus towards the throat. This movement of mucus helps to eliminate fluid, bacteria, and particles from the lungs. Most babies with primary ciliary dyskinesia experience breathing problems at birth, which suggests that cilia play an important role in clearing fetal fluid from the lungs. Beginning in early childhood, affected individuals develop frequent respiratory tract infections. Without properly functioning cilia in the airway, bacteria remain in the respiratory tract and cause infection. People with primary ciliary dyskinesia also have year-round nasal congestion and a chronic cough. Chronic respiratory tract infections can result in a condition called bronchiectasis, which damages the passages, called bronchi, leading from the windpipe to the lungs and can cause life-threatening breathing problems.
Some individuals with primary ciliary dyskinesia have abnormally placed organs within their chest and abdomen. These abnormalities arise early in embryonic development when the differences between the left and right sides of the body are established. About 50 percent of people with primary ciliary dyskinesia have a mirror-image reversal of their internal organs (situs inversus totalis). For example, in these individuals the heart is on the right side of the body instead of on the left. Situs inversus totalis does not cause any apparent health problems. When someone with primary ciliary dyskinesia has situs inversus totalis, they are often said to have Kartagener syndrome.
Approximately 12 percent of people with primary ciliary dyskinesia have a condition known as heterotaxy syndrome or situs ambiguus, which is characterized by abnormalities of the heart, liver, intestines, or spleen. These organs may be structurally abnormal or improperly positioned. In addition, affected individuals may lack a spleen (asplenia) or have multiple spleens (polysplenia). Heterotaxy syndrome results from problems establishing the left and right sides of the body during embryonic development. The severity of heterotaxy varies widely among affected individuals.
Primary ciliary dyskinesia can also lead to infertility. Vigorous movements of the flagella are necessary to propel the sperm cells forward to the female egg cell. Because their sperm do not move properly, males with primary ciliary dyskinesia are usually unable to father children. Infertility occurs in some affected females and is likely due to abnormal cilia in the fallopian tubes.
Another feature of primary ciliary dyskinesia is recurrent ear infections (otitis media), especially in young children. Otitis media can lead to permanent hearing loss if untreated. The ear infections are likely related to abnormal cilia within the inner ear.
Rarely, individuals with primary ciliary dyskinesia have an accumulation of fluid in the brain (hydrocephalus), likely due to abnormal cilia in the brain.
There is no specific treatment for primary ciliary dyskinesia 5. Treatment is focused on the symptoms. People with primary ciliary dyskinesia may be treated with chest physical therapy and breathing exercises to help remove excess mucous. Other treatments may include inhalants to help with breathing, and antibiotics to help treat and prevent infections. Surgery may be necessary to correct heart defects, and to remove damaged lung tissue. For people with severe lung and airway damage, lung transplant may be an option. Males with infertility may want to consider using donor sperm or intracytoplasmic sperm injection (ICSI) to have children. People with primary ciliary dyskinesia should avoid smoking and exposure to smoke in general. In addition, regular exercise can strengthen the lungs and may improve lung function 6.
Is there a support group for individuals and families with primary ciliary dyskinesia?
There are several online support groups for families and individuals with Primary Ciliary Dyskinesia:
- The Primary Ciliary Dyskinesia Family Support Group (http://pcdsupport.org.uk/) offers an “Online Community” feature on their website where people can post questions and discuss living with this condition.
- The Primary Ciliary Dyskinesia Foundation (https://pcdfoundation.org/) offers a forum for sharing information and resources.
Primary ciliary dyskinesia causes
Primary ciliary dyskinesia can result from mutations in many different genes 7. No single faulty gene causes all cases of primary ciliary dyskinesia. Rather, many genes are associated with primary ciliary dyskinesia. These genes provide instructions for making proteins that form the inner structure of cilia and produce the force needed for cilia to bend. Coordinated back and forth movement of cilia is necessary for the normal functioning of many organs and tissues. The movement of cilia also helps establish the left-right axis (the imaginary line that separates the left and right sides of the body) during embryonic development.
Mutations in the genes that cause primary ciliary dyskinesia result in defective cilia that move abnormally or are unable to move (immotile). Because cilia have many important functions within the body, defects in these cell structures cause a variety of signs and symptoms. If the cilia don’t work well, bacteria stay in your airways. This can cause breathing problems, infections, and other disorders.
Mutations in the DNAI1 and DNAH5 genes account for up to 30 percent of all cases of primary ciliary dyskinesia. Mutations in the other genes associated with primary ciliary dyskinesia are found in only a small percentage of cases. In many people with primary ciliary dyskinesia, the cause of the disorder is unknown.
Primary ciliary dyskinesia inheritance pattern
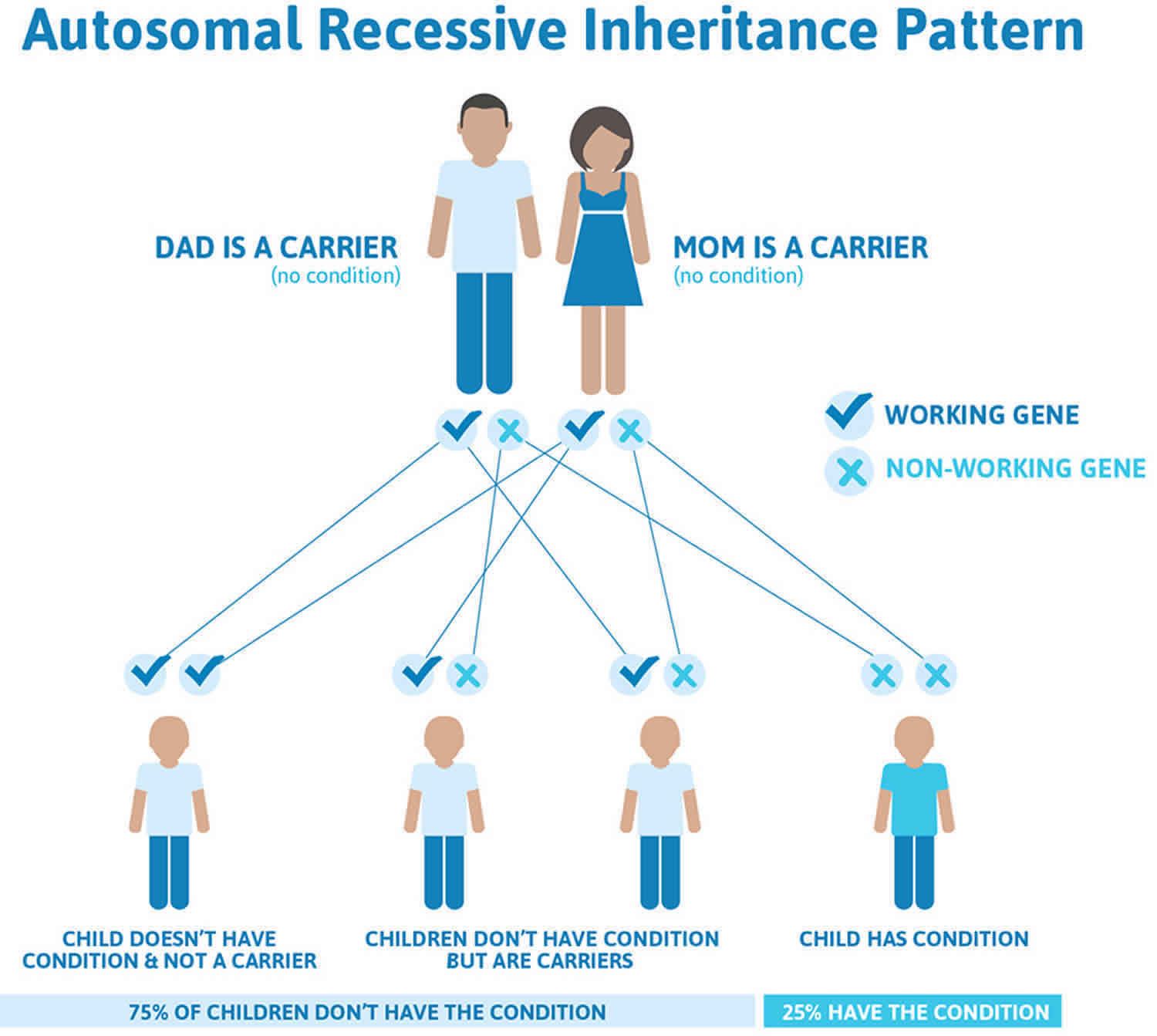
Primary ciliary dyskinesia is inherited in an autosomal recessive pattern, which means both copies of the gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
It is rare to see any history of autosomal recessive conditions within a family because if someone is a carrier for one of these conditions, they would have to have a child with someone who is also a carrier for the same condition. Autosomal recessive conditions are individually pretty rare, so the chance that you and your partner are carriers for the same recessive genetic condition are likely low. Even if both partners are a carrier for the same condition, there is only a 25% chance that they will both pass down the non-working copy of the gene to the baby, thus causing a genetic condition. This chance is the same with each pregnancy, no matter how many children they have with or without the condition.
- If both partners are carriers of the same abnormal gene, they may pass on either their normal gene or their abnormal gene to their child. This occurs randomly.
- Each child of parents who both carry the same abnormal gene therefore has a 25% (1 in 4) chance of inheriting a abnormal gene from both parents and being affected by the condition.
- This also means that there is a 75% ( 3 in 4) chance that a child will not be affected by the condition. This chance remains the same in every pregnancy and is the same for boys or girls.
- There is also a 50% (2 in 4) chance that the child will inherit just one copy of the abnormal gene from a parent. If this happens, then they will be healthy carriers like their parents.
- Lastly, there is a 25% (1 in 4) chance that the child will inherit both normal copies of the gene. In this case the child will not have the condition, and will not be a carrier.
These possible outcomes occur randomly. The chance remains the same in every pregnancy and is the same for boys and girls.
Figure 1 illustrates autosomal recessive inheritance. The example below shows what happens when both dad and mum is a carrier of the abnormal gene, there is only a 25% chance that they will both pass down the abnormal gene to the baby, thus causing a genetic condition.
Figure 1. Primary ciliary dyskinesia autosomal recessive inheritance pattern
People with specific questions about genetic risks or genetic testing for themselves or family members should speak with a genetics professional.
Resources for locating a genetics professional in your community are available online:
- The National Society of Genetic Counselors (https://www.findageneticcounselor.com/) offers a searchable directory of genetic counselors in the United States and Canada. You can search by location, name, area of practice/specialization, and/or ZIP Code.
- The American Board of Genetic Counseling (https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor/) provides a searchable directory of certified genetic counselors worldwide. You can search by practice area, name, organization, or location.
- The Canadian Association of Genetic Counselors (https://www.cagc-accg.ca/index.php?page=225) has a searchable directory of genetic counselors in Canada. You can search by name, distance from an address, province, or services.
- The American College of Medical Genetics and Genomics (http://www.acmg.net/ACMG/Genetic_Services_Directory_Search.aspx) has a searchable database of medical genetics clinic services in the United States.
Primary ciliary dyskinesia symptoms
Primary ciliary dyskinesia causes respiratory disease that mainly affects the sinuses, ear canals and lungs. One sign that you might have primary ciliary dyskinesia is if you have chronic (ongoing) infections in one or more of these areas. You may have continuous nasal congestion and coughing. More than 75% of full-term infants with primary ciliary dyskinesia have trouble breathing right after birth (neonatal respiratory distress) and require extra oxygen. On-going (chronic) airway infections begin in early childhood and can lead to permanent damage (bronchiectasis). Nasal congestion, sinus infections, and ear infections also begin in early childhood and continue throughout adulthood. Nearly all people with primary ciliary dyskinesia will cough frequently 5.
About 50% of people with primary ciliary dyskinesia will have abnormalities in the placement of their body organs, known as situs abnormalities 8. An example is having the heart on the right side of the chest instead of the left side. Situs abnormalities can include situs inversus totalis (mirror-image reversal of the internal organs with no apparent symptoms) or heterotaxy, where the organs are abnormally arranged. People with heterotaxy often have congenital heart defects. Almost all males with primary ciliary dyskinesia are infertile because of abnormal movement of the sperm. The symptoms of primary ciliary dyskinesia can vary and not everyone with primary ciliary dyskinesia has the same symptoms 5.
Primary ciliary dyskinesia signs and symptoms vary and may include:
- Ear, nose, and paranasal sinuses
- Chronic persistent runny nose with mucus and pus discharge, sensation of local fullness, and sinus pain
- Recurrent sinusitis. The sinuses are hollow air spaces around the nasal passages. Chronic sinusitis is a condition in which the sinuses are infected or inflamed.
- Anosmia, nasal character of speech, and halitosis
- Recurrent acute middle ear infections (acute otitis media)
- Chronic otitis media
- Hearing loss
- CNS – Hydrocephalus in a few cases
- Reproductive system – fertility problems in men and women. Male infertility (common) 9
- In men, primary ciliary dyskinesia can affect cilia-like structures that help sperm cells move. Because the sperm cells don’t move well, men who have the disease usually are unable to father children.
- Fertility problems also occur in some women who have primary ciliary dyskinesia. These problems likely are due to faulty cilia in the fallopian tubes. The fallopian tubes carry eggs from the ovaries to the uterus.
- Lungs (lower respiratory tract)
- Respiratory distress (breathing problems) in newborns
- Chronic productive cough
- Bronchospastic symptoms (eg, wheeze and cough), usually responsive to bronchodilator therapy
- Recurrent or persistent collapse of part or all of a lung (atelectasis) or pneumonia
Some people who have primary ciliary dyskinesia have abnormally placed organs and congenital heart defects.
When do symptoms occur?
The symptoms and severity of primary ciliary dyskinesia vary from person to person. If you or your child has primary ciliary dyskinesia, you may have serious sinus, ear, and/or lung infections. If the disease is mild, it may not show up until the teen or adult years.
The symptoms and severity of primary ciliary dyskinesia also vary over time. Sometimes, you may have few symptoms. Other times, your symptoms may become more severe.
Some people who have primary ciliary dyskinesia have breathing problems when they’re born and need extra oxygen for several days. Afterward, airway infections are common.
Diagnosing primary ciliary dyskinesia in children can be hard. This is because some primary ciliary dyskinesia symptoms—such as ear infections, chronic cough, and runny nose—are common in children, even if they don’t have primary ciliary dyskinesia. Also, the disease may be confused with another condition, such as cystic fibrosis.
A correct and early diagnosis of primary ciliary dyskinesia is very important. It will allow you or your child to get the proper treatment to keep your airways and lungs as healthy as possible. An early diagnosis and proper treatment also can prevent or delay ongoing and long-term lung damage.
Primary ciliary dyskinesia complications
Frequent bronchiectasis exacerbations with recurrent infections are a complication for patients with primary ciliary dyskinesia. Other complications include recurrent ear infections, chronic sinusitis, and infertility 10, 11.
Primary ciliary dyskinesia differential diagnosis
Primary ciliary dyskinesia differential diagnosis include the following 12, 13:
- Cystic fibrosis
- Foreign body aspiration
- Idiopathic interstitial pneumonia
- Idiopathic nasal polyposis
- Immunosuppression
- Cancer
- Post-infectious bronchiectasis
- Severe atopy
- Tracheobronchomegaly
Primary ciliary dyskinesia diagnosis
Your doctor or your child’s doctor will diagnose primary ciliary dyskinesia based on signs and symptoms and test results.
If your primary care doctor thinks that you may have primary ciliary dyskinesia or another lung disorder, he or she may refer you to a pulmonologist. This is a doctor who specializes in diagnosing and treating lung diseases and conditions.
Your doctor will look for signs and symptoms that point to primary ciliary dyskinesia, such as:
- Respiratory distress (breathing problems) at birth
- Chronic sinus, middle ear, and/or lung infections
- Situs inversus (internal organs in positions opposite of what is normal)
Your doctor also may ask whether you have a family history of primary ciliary dyskinesia. primary ciliary dyskinesia is an inherited disease. “Inherited” means the disease is passed from parents to children through genes. A family history of primary ciliary dyskinesia suggests an increased risk for the disease.
Diagnostic tests
If the doctor thinks that you or your child might have primary ciliary dyskinesia, he or she may recommend tests to confirm the diagnosis.
Genetic testing
Researchers have found many gene defects associated with primary ciliary dyskinesia. Genetic testing can show whether you have faulty genes linked to the disease.
Genetic testing is done using a blood sample. The sample is taken from a vein in your body using a needle. The blood sample is checked at a special genetic testing laboratory (lab).
Electron microscopy
Doctors can use a special microscope, called an electron microscope, to look at samples of your airway cilia. This test can show whether your cilia are faulty.
An ear, nose, and throat (ENT) specialist or a pulmonologist (lung specialist) will take samples of your cilia. He or she will brush the inside of your nose or remove some cells from your airways.
The doctor will send the samples to a lab. There, a pathologist will look at them under an electron microscope. (A pathologist is a doctor who specializes in identifying diseases by studying cells and tissues under a microscope.)
Other tests
Sometimes doctors use one or more of the following tests to help diagnose primary ciliary dyskinesia. These tests are less complex than genetic testing and electron microscopy, and they can be done in a doctor’s office.
However, these tests don’t give a final diagnosis. Based on the test results, doctors may recommend the more complex tests.
Video microscopy. For this test, a pulmonologist brushes the inside of your nose to get a sample of cilia. Then, he or she looks at the cilia under a microscope to see how they move. Abnormal movement of the cilia may be a sign of primary ciliary dyskinesia.
Radiolabeled particles. For this test, you breathe in tiny particles that have a small amount of radiation attached to them. When you breathe out, your doctor will test how well your cilia can move the particles.
If you breathe out a smaller than normal number of particles, your cilia may not be working well. This could be a sign of primary ciliary dyskinesia.
Nasal nitric oxide. This test measures the level of nitric oxide (a gas) when you breathe out. In people who have primary ciliary dyskinesia, the level of nitric oxide is very low compared with normal levels. Doctors don’t know why people who have primary ciliary dyskinesia breathe out such low levels of nitric oxide.
Semen analysis. This test is used for adult men. In men, primary ciliary dyskinesia can affect cilia-like structures that help sperm cells move. As a result, men who have primary ciliary dyskinesia may have fertility problems. “Fertility” refers to the ability to have children. For this test, a sample of semen is checked under a microscope. Abnormal sperm may be a sign of primary ciliary dyskinesia.
Tests for other conditions. Your doctor also might want to do tests to rule out diseases and disorders that have symptoms similar to those of primary ciliary dyskinesia. For example, you may have tests to rule out cystic fibrosis or immune disorders.
Primary ciliary dyskinesia treatment
Unfortunately, no treatment is available yet to fix faulty airway cilia. Cilia are tiny, hair-like structures that line the airways. Thus, treatment for primary ciliary dyskinesia focuses on which symptoms and complications you have.
The main goals of treating primary ciliary dyskinesia are to:
- Control and treat lung, sinus, and ear infections
- Remove trapped mucus from the lungs and airways
Primary ciliary dyskinesia patients should be managed in centers that specialize in primary ciliary dysfunction and chronic pulmonary diseases 14, 15.
Specialists involved
Many doctors may help care for someone who has primary ciliary dyskinesia. For example, a neonatologist may suspect primary ciliary dyskinesia or another lung disorder if a newborn has breathing problems at birth. A neonatologist is a doctor who specializes in treating newborns.
A pediatrician may suspect primary ciliary dyskinesia if a child has chronic (ongoing) sinus, ear, and/or lung infections. A pediatrician is a doctor who specializes in treating children. This type of doctor provides children with ongoing care from an early age and treats conditions such as ear infections and breathing problems.
An otolaryngologist also called an ear, nose, and throat (ENT) specialist, may help diagnose and treat primary ciliary dyskinesia. This type of doctor treats ear, nose, and throat disorders. If a child has chronic sinus or ear infections, an ENT specialist may be involved in the child’s care.
A pulmonologist may help diagnose or treat lung problems related to primary ciliary dyskinesia. This type of doctor specializes in diagnosing and treating lung diseases and conditions. Most people who have primary ciliary dyskinesia have lung problems at some point in their lives.
A pathologist is a doctor who specializes in identifying diseases by studying cells and tissues under a microscope. This type of doctor may help diagnose primary ciliary dyskinesia by looking at cilia under a microscope.
A pathologist also may look at mucus samples to see what types of bacteria are causing infections. This information can help your doctor decide which treatments to prescribe.
Primary ciliary dyskinesia patients should be evaluated by a pulmonologist two to four times per year with spirometry and surveillance cultures of sputum 13. A chest radiograph should be completed at the time of diagnosis and during acute respiratory exacerbations. At least once after diagnosis, a chest CT, preferably a high-resolution CT scan, to evaluate for bronchiectasis should be considered 16.
Unlike cystic fibrosis, the lung clearance index does not seem to be a helpful monitoring tool for patients with primary ciliary dyskinesia 13. Additionally, children with primary ciliary dyskinesia should be evaluated by an ear-nose-throat specialist one to two times per year and as needed in adults. An audiology assessment should be performed since there is a high incidence of recurrent otitis media with chronic middle ear effusions and associated complications of conductive hearing loss 17. Patients should be monitored for chronic rhinosinusitis and nasal polyps. Prevention of acute exacerbations of bronchiectasis from bacterial infections is a mainstay of treatment as it slows down the progression of the disease 14. Prevention of exacerbations is achieved by aiding the body in clearing secretions, thus reducing the microbial load. This is obtained by daily chest physiotherapy and effective airway hydration 16.
While there are many similarities between the treatment of cystic fibrosis (CF) and primary ciliary dyskinesia, it has been found that certain mucolytic agents, such as DNase, while effective in CF, are not effective for primary ciliary dyskinesia 13. When prevention fails and acute exacerbations occur, antibiotics are the mainstay of treatment and should be started even when symptoms appear mild. Obtaining regular sputum samples helps guide antibiotic choice for empiric coverage during an acute exacerbation. Pseudomonas aeruginosa should always be considered, and patients may require IV antibiotics for such infections. For recurrent exacerbations, prevention with chronic antibiotic suppression, such as azithromycin, can effectively reduce the number of infections 18. Primary ciliary dyskinesia patients should receive influenza vaccination and pneumococcal vaccination as indicated.
A bilateral lung transplant may be necessary for patients with end-stage respiratory disease 19. Symptomatic treatment of chronic rhinosinusitis is characterized by nasal saline lavage and intranasal glucocorticoids. Endoscopic sinus surgery has been shown to improve chronic rhinosinusitis 20. The use of tympanostomy tubes in these patients as a management strategy for recurrent otitis media continues to be debated, as many patients will improve symptoms with conservative therapy 21. It is crucial to provide patients with counseling on impaired fertility. Gene editing has been proposed as a possible future treatment for primary ciliary dysfunction. Ex vivo gene repair by site-specific recombination has been found to rescue ciliary beating, which could have tremendous application in primary ciliary dysfunction patients 14.
Treatments for breathing and lung problems
Standard treatments for breathing and lung problems in people who have primary ciliary dyskinesia are chest physical therapy (chest physical therapy), exercise, and medicines.
One of the main goals of these treatments is to get you to cough. Coughing clears mucus from the airways, which is important for people who have primary ciliary dyskinesia. For this reason, your doctor also may advise you to avoid medicines that suppress coughing.
Chest physical therapy
Chest physical therapy also called chest clapping or percussion. Chest physical therapy involves pounding your chest and back over and over with your hands or a device to loosen the mucus from your lungs so that you can cough it up.
You might sit down or lie on your stomach with your head down while you do chest physical therapy. Gravity and force help drain the mucus from your lungs.
Some people find chest physical therapy hard or uncomfortable to do. Several devices have been made to help with chest physical therapy, such as:
- An electric chest clapper, known as a mechanical percussor.
- An inflatable therapy vest that uses high-frequency airwaves. The airwaves force the mucus that’s deep in your lungs toward your upper airways so you can cough it up.
- A small hand-held device that you breathe out through. The device causes vibrations that dislodge the mucus.
- A mask that creates vibrations to help break the mucus loose from your airway walls.
Breathing techniques also may help dislodge mucus so you can cough it up. These techniques include forcing out a couple of short breaths or deeper breaths and then doing relaxed breathing. This may help loosen the mucus in your lungs and open your airways.
Exercise
Aerobic exercise that makes you breathe harder helps loosen the mucus in your airways so you can cough it up. Exercise also helps improve your overall physical condition.
Talk with your doctor about what types and amounts of exercise are safe for you or your child.
Medicines
If you have primary ciliary dyskinesia, your doctor may prescribe antibiotics, bronchodilators, or anti-inflammatory medicines. These medicines help treat lung infections, open up the airways, and reduce swelling.
Antibiotics are the main treatment to prevent or treat lung infections. Your doctor may prescribe oral or intravenous (IV) antibiotics.
Oral antibiotics often are used to treat mild lung infections. For severe or hard-to-treat infections, you may be given IV antibiotics through a tube inserted into a vein.
To help decide which antibiotics you need, your doctor may send mucus samples to a pathologist. The pathologist will try to find out which bacteria are causing the infection.
Bronchodilators help open the airways by relaxing the muscles around them. You inhale these medicines. Often, they’re taken just before chest physical therapy to help clear mucus from your lungs. You also may take bronchodilators before inhaling other medicines into your lungs.
Anti-inflammatory medicines can help reduce swelling in your airways that’s caused by ongoing infections. These medicines may be inhaled or oral.
Treatments for sinus and ear infections
To treat infections, your doctor may recommend saline nasal washes and anti-inflammatory nasal spray. If these treatments aren’t enough, you may need medicines, such as antibiotics. If antibiotics don’t work, surgery may be an option.
Tympanostomy is a procedure in which small tubes are inserted into the eardrums to help drain mucus from the ears. This procedure may help children who have hearing problems caused by primary ciliary dyskinesia.
Nasal or sinus surgery may help drain the sinuses and provide short-term relief of symptoms. However, the long-term benefits of this treatment are unclear.
Treatments for advanced lung disease
People who have primary ciliary dyskinesia may develop a serious lung condition called bronchiectasis. Bronchiectasis often is treated with medicines, hydration (drinking plenty of fluids), and chest physical therapy.
If bronchiectasis severely affects part of your lung, surgery may be used to remove that area of lung.
In very rare cases, if other treatments haven’t worked, lung transplant may be an option for severe lung disease. A lung transplant is surgery to remove a person’s diseased lung and replace it with a healthy lung from a deceased donor.
Living with primary ciliary dyskinesia
If you or your child has primary ciliary dyskinesia, try to learn as much as you can about the disease. Work closely with your doctors or your child’s doctors to learn how to manage primary ciliary dyskinesia.
Ongoing care
You’ll need ongoing care to check your lung function and your general health. Ask your doctor how often you should schedule followup visits.
Your doctor will likely recommend periodic chest x rays and lung function tests. He or she will use the test results and information about your symptoms to plan your treatment.
Make sure to report new or worsening symptoms, such as increased coughing, to your doctor right away. This will allow him or her to find out whether you have an infection and what’s causing it. Your doctor can then prescribe medicine to prevent the infection from worsening.
Also, certain vaccines can lower your risk for some infections. Talk with your doctor about which vaccines may benefit you.
If your child has primary ciliary dyskinesia, encourage him or her to learn about the disease and take an active role in his or her treatment.
Healthy lifestyle
Between medical checkups, you can practice good self-care and follow a healthy lifestyle. An important part of a healthy lifestyle is following a healthy diet.
A healthy diet includes a variety of fruits, vegetables, and whole grains. It also includes lean meats, poultry, fish, beans, and fat-free or low-fat milk or milk products. A healthy diet is low in saturated fat, trans fat, cholesterol, sodium (salt), and added sugar.
Another important part of a healthy lifestyle is to quit smoking or not start smoking. Talk to your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke.
If you have a child who has primary ciliary dyskinesia, avoid smoking anywhere your child spends time, including the home and car. Encourage your child to never start smoking.
Other steps you can take to follow a healthy lifestyle include:
- Washing your hands often to lower your risk of infection.
- Being physically active and drinking lots of fluids. Talk with your doctor about what types and amounts of activity are safe for you or your child.
- Doing chest physical therapy (as your doctor recommends).
- Avoiding medicines that suppress coughing. (Coughing helps clear mucus from your airways.)
Other concerns
Adults who have primary ciliary dyskinesia can expect to have normal sex lives. However, men and women who have the disease may have fertility problems. “Fertility” refers to the ability to have children. Fertility treatments may help some people who have primary ciliary dyskinesia.
If you have primary ciliary dyskinesia and fertility concerns, talk with your doctor. He or she can advise you about available treatment options.
People who have primary ciliary dyskinesia should still have protected sex to avoid sexually transmitted diseases.
Emotional issues and support
Living with primary ciliary dyskinesia may cause fear, anxiety, depression, and stress. Talk about how you feel with your health care team. Talking to a professional counselor also can help. If you’re very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
Genetic counseling
You may want to consider genetic counseling if you have:
- A family history of primary ciliary dyskinesia and you’re planning to have children
- A child who has primary ciliary dyskinesia and are planning to have more children
A genetic counselor can explain the risk (likelihood) of having children who have the disease. He or she also can help explain the choices that are available.
You can find information about genetic counseling from health departments, neighborhood health centers, and medical centers.
Primary ciliary dyskinesia prognosis
Many people who have primary ciliary dyskinesia have normal lifespans. People with primary ciliary dyskinesia can often continue to live an active lifestyle, particularly when compliant with the management guidelines outlined above. Given the high variability of the disease, it is difficult to predict the type of decline in lung function any patient will experience 13. However, there are studies suggesting aggressive airway clearance and the use of antibiotics early may slow the course of primary ciliary dyskinesia disease. One study found that about 60% of the patients with primary ciliary dyskinesia had stable pulmonary function tests (PFTs) in a 30-year longitudinal study. About 30% of the patients in this study suffered from a decrease in lung function 22.
The long-term outlook for people with primary ciliary dyskinesia is dependent on severity of respiratory symptoms. Generally, primary ciliary dyskinesia is not thought to be life-threatening, but severe lung and airway disease can lead to permanent damage. About 25 percent of people who have primary ciliary dyskinesia may develop respiratory failure, a life-threatening condition. A small number of people who have primary ciliary dyskinesia need lung transplants.
Ear infections that occur frequently can lead to hearing loss, which is sometimes permanent. Early diagnosis and treatment seems to improve long-term outcomes 6.
Scientists continue to study the faulty genes that cause primary ciliary dyskinesia. Further studies of the disease will likely lead to earlier diagnoses, better treatments, and improved outcomes.
References- Zariwala MA, Knowles MR, Leigh MW. Primary Ciliary Dyskinesia. 2007 Jan 24 [Updated 2015 Sep 3]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1122
- Tadesse A, Alemu H, Silamsaw M, Gebrewold Y. Kartagener’s syndrome: a case report. J Med Case Rep. 2018 Jan 10;12(1):5. doi: 10.1186/s13256-017-1538-2
- Nonaka S, Tanaka Y, Okada Y, Takeda S, Harada A, Kanai Y, Kido M, Hirokawa N. Randomization of left-right asymmetry due to loss of nodal cilia generating leftward flow of extraembryonic fluid in mice lacking KIF3B motor protein. Cell. 1998 Dec 11;95(6):829-37. doi: 10.1016/s0092-8674(00)81705-5. Erratum in: Cell 1999 Oct 1;99(1):117.
- McManus IC, Mitchison HM, Chung EM, Stubbings GF, Martin N. Primary ciliary dyskinesia (Siewert’s/Kartagener’s syndrome): respiratory symptoms and psycho-social impact. BMC Pulm Med. 2003 Nov 27;3:4. doi: 10.1186/1471-2466-3-4
- Mirra V, Werner C, Santamaria F. Primary ciliary dyskinesia: An update on clinical aspects, genetics, diagnosis, and future treatment strategies. Front Pediatr. Jun 2017; 5:135. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5465251
- Sharpiro AJ, Zariwala MA, Ferkol T, Davis SD, Sagel, SD, et al. (The Genetic Disorders of Mucociliary Clearance Consortium). Diagnosis, Monitoring, and Treatment of Primary Ciliary Dyskinesia: PCD Foundation Consensus Recommendations Based on State of the Art Review. Pedia Pulmon. 2016; 51:115-132. https://onlinelibrary.wiley.com/doi/epdf/10.1002/ppul.23304
- Primary ciliary dyskinesia. https://ghr.nlm.nih.gov/condition/primary-ciliary-dyskinesia
- Knowles M, Zariwala MA, Leigh M. Primary ciliary dyskinesia. Clin Chest Med. 2016; 37(3):449-461. https://www.ncbi.nlm.nih.gov/pubmed/27514592
- Afzelius BA, Eliasson R. Male and female infertility problems in the immotile-cilia syndrome. Eur J Respir Dis Suppl. 1983. 127:144-7.
- Knowles MR, Daniels LA, Davis SD, Zariwala MA, Leigh MW. Primary ciliary dyskinesia. Recent advances in diagnostics, genetics, and characterization of clinical disease. Am J Respir Crit Care Med. 2013 Oct 15;188(8):913-22. doi: 10.1164/rccm.201301-0059CI
- Lucas JS, Burgess A, Mitchison HM, Moya E, Williamson M, Hogg C; National PCD Service, UK. Diagnosis and management of primary ciliary dyskinesia. Arch Dis Child. 2014 Sep;99(9):850-6. doi: 10.1136/archdischild-2013-304831
- Bush A, Payne D, Pike S, Jenkins G, Henke MO, Rubin BK. Mucus properties in children with primary ciliary dyskinesia: comparison with cystic fibrosis. Chest. 2006 Jan;129(1):118-23. doi: 10.1378/chest.129.1.118
- Kapania EM, Stern BM, Sharma G. Ciliary Dysfunction. [Updated 2022 Nov 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448201
- Mirra V, Werner C, Santamaria F. Primary Ciliary Dyskinesia: An Update on Clinical Aspects, Genetics, Diagnosis, and Future Treatment Strategies. Front Pediatr. 2017 Jun 9;5:135. doi: 10.3389/fped.2017.00135
- Lobo LJ, Zariwala MA, Noone PG. Primary ciliary dyskinesia. QJM. 2014 Sep;107(9):691-9. doi: 10.1093/qjmed/hcu063
- Barbato A, Frischer T, Kuehni CE, Snijders D, Azevedo I, Baktai G, Bartoloni L, Eber E, Escribano A, Haarman E, Hesselmar B, Hogg C, Jorissen M, Lucas J, Nielsen KG, O’Callaghan C, Omran H, Pohunek P, Strippoli MP, Bush A. Primary ciliary dyskinesia: a consensus statement on diagnostic and treatment approaches in children. Eur Respir J. 2009 Dec;34(6):1264-76. doi: 10.1183/09031936.00176608
- Piatti G, De Santi MM, Torretta S, Pignataro L, Soi D, Ambrosetti U. Cilia and Ear. Ann Otol Rhinol Laryngol. 2017 Apr;126(4):322-327. doi: 10.1177/0003489417691299
- Kobbernagel HE, Buchvald FF, Haarman EG, Casaulta C, Collins SA, Hogg C, Kuehni CE, Lucas JS, Moser CE, Quittner AL, Raidt J, Rosthøj S, Sørensen AL, Thomsen K, Werner C, Omran H, Nielsen KG. Efficacy and safety of azithromycin maintenance therapy in primary ciliary dyskinesia (BESTCILIA): a multicentre, double-blind, randomised, placebo-controlled phase 3 trial. Lancet Respir Med. 2020 May;8(5):493-505. doi: 10.1016/S2213-2600(20)30058-8
- Tkebuchava T, Niederhäuser U, Weder W, von Segesser LK, Bauersfeld U, Felix H, Lachat M, Turina MI. Kartagener’s syndrome: clinical presentation and cardiosurgical aspects. Ann Thorac Surg. 1996 Nov;62(5):1474-9. doi: 10.1016/0003-4975(96)00493-6
- Alanin, MC, Aanaes, K, Høiby, N, et al. Sinus surgery can improve quality of life, lung infections, and lung function in patients with primary ciliary dyskinesia. Int Forum Allergy Rhinol. 2017; 7: 240– 247. https://doi.org/10.1002/alr.21873
- Majithia A, Fong J, Hariri M, Harcourt J. Hearing outcomes in children with primary ciliary dyskinesia–a longitudinal study. Int J Pediatr Otorhinolaryngol. 2005 Aug;69(8):1061-4. doi: 10.1016/j.ijporl.2005.02.013
- Marthin JK, Petersen N, Skovgaard LT, Nielsen KG. Lung function in patients with primary ciliary dyskinesia: a cross-sectional and 3-decade longitudinal study. Am J Respir Crit Care Med. 2010 Jun 1;181(11):1262-8. doi: 10.1164/rccm.200811-1731OC