What is promethazine
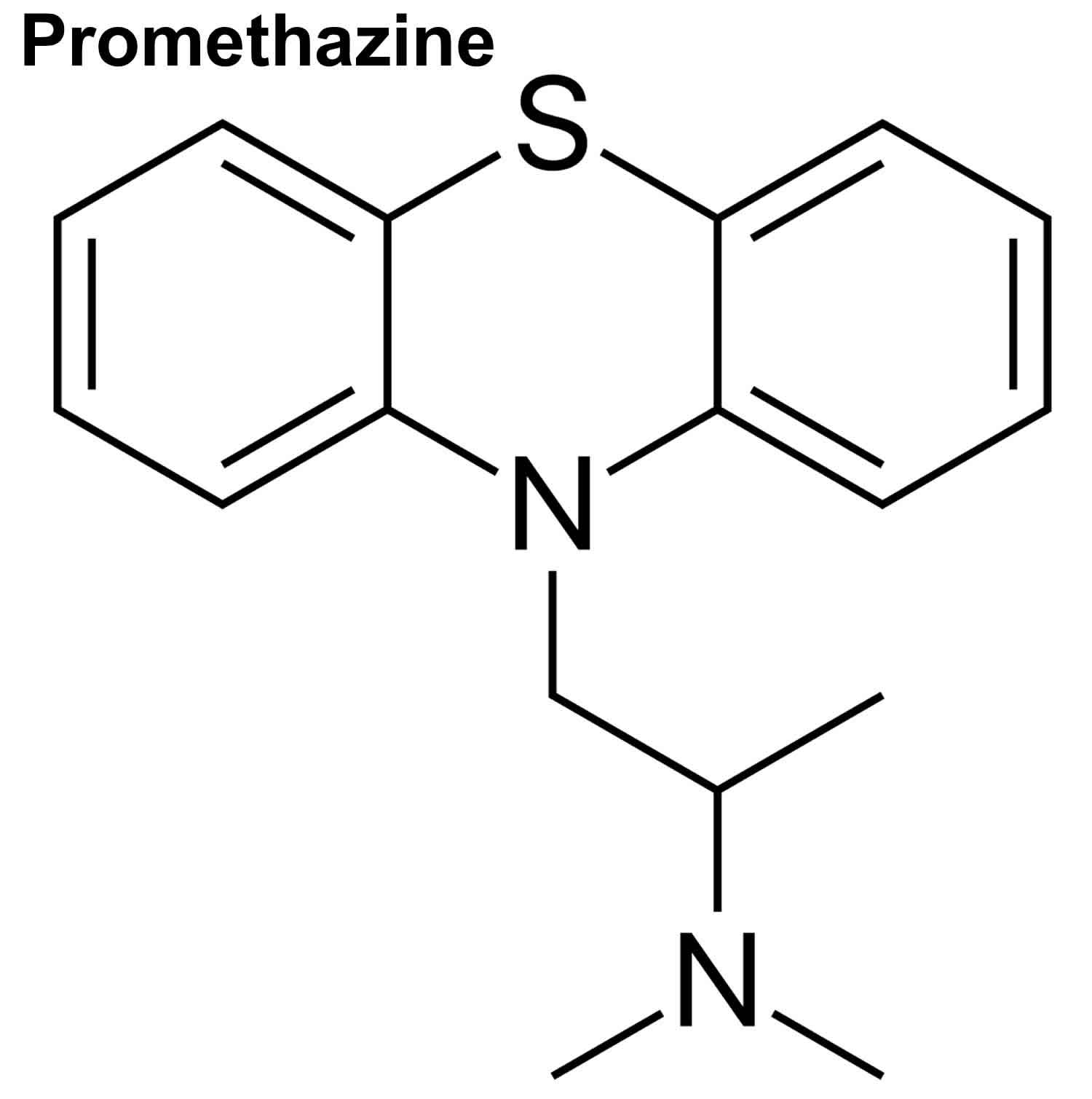
Promethazine is an antihistamine medicine that is used to relieve the symptoms of allergic reactions such as allergic rhinitis (runny nose and watery eyes caused by allergy to pollen, mold or dust), allergic conjunctivitis (red, watery eyes caused by allergies), allergic skin reactions, and allergic reactions to blood or plasma products. Promethazine is known as a drowsy (sedating) antihistamine. Promethazine is more likely to make you feel sleepy than other antihistamines. Promethazine is used with other medications to treat anaphylaxis (sudden, severe allergic reactions) and the symptoms of the common cold such as sneezing, cough, and runny nose. Promethazine is also used to relax and sedate patients before and after surgery, during labor, and at other times. Promethazine is also used to prevent and control nausea and vomiting that may occur after surgery, and with other medications to help relieve pain after surgery. Promethazine is also used to prevent and treat motion sickness. Promethazine helps control symptoms, but will not treat the cause of the symptoms or speed recovery. Promethazine is in a class of medications called phenothiazines.
You can buy promethazine from pharmacies, where it’s often sold as Phenergan® and Promethegan®, Avomine or Sominex. Promethazine is also available on prescription.
You can also buy promethazine mixed with other medicines, such as paracetamol, dextromethorphan, pholcodine or pseudoephedrine, to treat coughs and colds or pain.
Promethazine antagonizes the central and peripheral effects of histamine mediated by histamine H1 receptors. The effects of promethazine include bronchoconstriction, vasodilation and spasmodic contractions of gastrointestinal smooth muscle. In addition, promethazine binds to muscarinic receptors, resulting in anticholinergic and antiemetic activities.
Promethazine comes as a tablet and syrup (liquid) to take by mouth and as a suppository to use rectally.When promethazine is used to treat allergies, it is usually taken one to four times daily, before meals and/or at bedtime. When promethazine is used to relieve cold symptoms, it is usually taken every 4 to 6 hours as needed. When promethazine is used to treat motion sickness, it is taken 30 to 60 minutes before travel and again after 8 to 12 hours if needed. On longer trips, promethazine is usually taken in the morning and before the evening meal on each day of travel. When promethazine is used to treat or prevent nausea and vomiting it is usually taken every 4 to 6 hours as needed. Promethazine may also be taken at bedtime the night before surgery to relieve anxiety and produce quiet sleep. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take promethazine exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Promethazine suppositories are for rectal use only. Do not try to swallow the suppositories or insert in any other part of your body.
If you are taking promethazine liquid, do not use a household spoon to measure your dose. Use the measuring spoon or cup that came with the medication or use a spoon made especially for measuring medication.
To insert a promethazine suppository, follow these steps:
- If the suppository feels soft, hold it under cold, running water for 1 minute. Remove the wrapper.
- Dip the tip of the suppository in water.
- Lie down on your left side and raise your right knee to your chest. (A left-handed person should lie on the right side and raise the left knee.)
- Using your finger, insert the suppository into the rectum, about 1/2 to 1 inch (1.25 to 2.5 centimeters) in children who are 2 years of age older and 1 inch (2.5 centimeters) in adults. Hold it in place for a few moments.
- Stand up after about 15 minutes. Wash your hands thoroughly and resume your normal activities.
Promethazine key facts
- Avoid drinking alcohol while taking promethazine. Alcohol increases the risks of side effects.
- To help you sleep, you’ll usually take promethazine 20 minutes before you go to bed. It normally takes about 30 minutes to work.
- For preventing travel sickness, you can usually take promethazine the night before a long journey or 1 to 2 hours before a short journey.
- Common side effects include feeling sleepy, headaches, nightmares and feeling dizzy, restless or confused.
- Promethazine is known by the brand names Avomine, Phenergan and Sominex.
- When promethazine is mixed with other medicines, it’s also known by the brand names Day & Night Nurse, Fedril and Night Nurse.
Promethazine may cause breathing to slow or stop, and may cause death in children. Promethazine should not be given to babies or children who are younger than 2 years old and should be given with caution to children who are 2 years of age or older. Combination products containing promethazine and codeine should not be given to children younger than 16 years old. Promethazine should not routinely be used to treat vomiting in children; it should only be used in specific cases when a doctor decides that it is needed. Tell your child’s doctor if your child has any condition that affects his/her breathing such as lung disease, asthma, or sleep apnea (stops breathing for short periods of time during sleep). Tell your doctor or pharmacist about all the medications your child is taking, especially barbiturates such as phenobarbital (Luminal), medications for anxiety, narcotic medications for pain, sedatives, sleeping pills, and tranquilizers. Call your child’s doctor immediately and get emergency medical treatment if your child has difficulty breathing, wheezes, slows or pauses in breathing, or stops breathing.
Talk to your doctor about the risks of giving promethazine to your child.
How long does promethazine take to work?
Promethazine will start to make you feel sleepy around 20 minutes after you take it and may work for up to 12 hours.
If you’re taking promethazine for a cough or cold, allergies or nausea, your symptoms should start to improve within 20 minutes. Promethazine should work for around 4 to 6 hours.
What’s the difference between promethazine and other antihistamines?
Promethazine is known as a drowsy (sedating) antihistamine as it makes you sleepy.
Non-drowsy antihistamines are less likely to have this effect. These include cetirizine, fexofenadine and loratadine.
Most people prefer to take a non-drowsy antihistamine as it’s less likely to interfere with their everyday routine.
You might choose to take a drowsy antihistamine, however, if you’re having problems falling asleep, or if symptoms like itching or coughing are keeping you awake.
There isn’t enough information available to say whether one antihistamine is better than another for treating allergies.
You may need to try a few different medicines to find what works best for you. Ask your pharmacist or doctor for advice if you’re unsure.
Can I take more than one antihistamine at a time?
Do not take 2 antihistamines together unless you have been advised to by your doctor.
You can take 2 different antihistamines at a time. If you have a severe itchy skin rash, your doctor may recommend 2 different antihistamines together for a few days.
A non-drowsy antihistamine (such as cetirizine, fexofenadine or loratadine) during the day, and a drowsy antihistamine at night if itching is making it difficult to sleep.
Do not take another drowsy antihistamine together with promethazine. It’ll make you very tired and sleepy.
Other drowsy antihistamines include chlorphenamine (Piriton) and diphenhydramine (Nytol Original).
How long can I take promethazine for?
You should only take promethazine for a short time, unless your doctor says it’s OK for you to take it for longer.
Speak to your pharmacist or doctor before taking promethazine for longer than the medicine leaflet recommends.
Ask them for advice if you’re unsure how long you should take promethazine for.
Is promethazine addictive?
It’s unlikely that you’ll get addicted to promethazine. But it’s best that you only take it for a very short time, unless your doctor tells you to take it for longer.
Not a lot is known about taking promethazine for a long time, so there’s more chance of having side effects.
If you have bought a medicine containing promethazine, do not take it for longer than recommended on the packet without speaking to your pharmacist or doctor first.
If you have taken promethazine for a long time and suddenly stop taking it, it’s possible you might feel dizzy, sweaty or sick, have a racing heart and have trouble sleeping.
Coming off promethazine slowly can help prevent this.
Speak to your doctor if you have taken promethazine for a long time and want to stop taking it.
Will promethazine help me sleep?
Yes. If you take it for insomnia or take it at night time, promethazine will help you sleep.
If you take it during the day for other conditions, such as allergies, it might cause daytime sleepiness, too.
Can lifestyle changes help me sleep better?
Promethazine will only help you sleep while you’re taking it, so there are a number of things you can do instead to help yourself have a good night’s sleep:
- set regular times for going to bed and waking up
- relax before bedtime – try taking a warm bath or listening to calming music
- use thick curtains or blinds, an eye mask and earplugs to stop you being woken up by light and noise
- avoid caffeine, cigarettes or vapes, alcohol, heavy meals and exercise for a few hours before bed time
- don’t watch TV or use phones, tablets or computers before going to bed
- don’t nap during the day
- make a list of your worries and any ideas for how to solve them before you go to bed – this can help you forget about them until the morning
Can I drink alcohol with promethazine?
Do not drink alcohol while you’re taking promethazine.
Alcohol and promethazine together can make you sleep very deeply.
You won’t be able to breathe properly and may have difficulty waking up.
Is there any food or drink I need to avoid?
You can eat normally while taking promethazine. But avoid alcohol and drinks that contain caffeine, like coffee, cola, or energy drinks.
Caffeine has the opposite effect to promethazine on your body and stops it working.
Is it dangerous to take promethazine with recreational drugs?
Yes, it’s dangerous to take promethazine with recreational drugs. This is because it can slow or stop your heart and lungs.
Mixing promethazine and codeine in large amounts slows down the central nervous system (brain and spinal cord), which can slow breathing and heart rate.
It’s even more dangerous when taken with alcohol or other drugs and has caused people to die.
Can I take promethazine with painkillers?
Yes, you can take promethazine together with painkillers, such as acetaminophen (paracetamol) or ibuprofen.
If you take promethazine with painkillers that contain codeine (such as co-codamol or other prescription painkillers), you may feel very tired and sleepy.
Do not drive, ride a bike or operate machinery or tools if this happens to you.
It’s important to check the packaging or label of your medicine carefully. This is because some promethazine products already contain a painkiller.
Do not take extra painkillers if this is the case, as there’s a risk of overdose.
Speak to your pharmacist if you’re not sure whether a medicine already contains a painkiller.
Can I drive or ride a bike with promethazine?
Do not drive a car or ride a bike if promethazine makes you sleepy during the daytime, gives you blurred vision or makes you feel dizzy, clumsy or unable to concentrate or make decisions.
This may be more likely when you first start taking promethazine, but could happen at any time (for example, when starting another medicine).
It’s an offence to drive a car if your ability to drive safely is affected. It’s your responsibility to decide if it’s safe to drive. If you’re in any doubt, do not drive.
Will promethazine affect my fertility?
There’s no firm evidence to suggest that taking promethazine will reduce fertility in either men or women.
But speak to a pharmacist or your doctor before taking it if you’re trying to get pregnant.
Will promethazine affect my contraception?
Promethazine doesn’t affect any type of contraception, including the combined pill and emergency contraception.
Can lifestyle changes help with hayfever and other allergies?
If you have hay fever, it’ll help if you don’t spend too much time outside if the pollen count is high.
Tips for when you’re outside:
- don’t cut grass or walk on grass
- wear wraparound sunglasses to stop pollen getting into your eyes
- put Vaseline around your nostrils to help trap pollen
- shower and change your clothes after you have been outside to wash off pollen
Tips for when you’re inside:
- keep windows and doors shut as much as possible
- vacuum regularly and dust with a damp cloth
- don’t keep fresh flowers in the house
- don’t smoke or be around smoke as it makes hay fever symptoms worse
The best way to prevent any sort of allergic reaction is to avoid the substance that you’re allergic to, if you can.
Promethazine precautions
Before taking promethazine:
- tell your doctor and pharmacist if you are allergic to promethazine, other phenothiazines (certain medications used to treat mental illness, nausea, vomiting, severe hiccups, and other conditions) or any other medications. Also tell your doctor and pharmacist if you have ever had an unusual or unexpected reaction when you took promethazine, another phenothiazine, or any other medication. Ask your doctor or pharmacist if you do not know if a medication you are allergic to is a phenothiazine.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements and herbal products you are taking or plan to take. Be sure to mention any of the following: antidepressants (‘mood elevators’) such as amitriptyline (Elavil), amoxapine (Asendin), clomipramine (Anafranil), desipramine (Norpramin), doxepin (Adapin, Sinequan), imipramine (Tofranil), nortriptyline (Aventyl, Pamelor), protriptyline (Vivactil), and trimipramine (Surmontil); antihistamines; azathioprine (Imuran);barbiturates such as phenobarbital (Luminal); cancer chemotherapy; epinephrine (Epipen); ipratropium (Atrovent)medications for anxiety, irritable bowel disease, mental illness, motion sickness, Parkinson’s disease, seizures, ulcers, or urinary problems; monoamine oxidase (MAO) inhibitors such as isocarboxazid (Marplan), phenelzine (Nardil), tranylcypromine (Parnate), and selegiline (Eldepryl, Emsam, Zelapar); narcotics and other pain medication; sedatives; sleeping pills;and tranquilizers. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- tell your doctor if you have or have ever had an enlarged prostate (a male reproductive gland); glaucoma (a condition in which increased pressure in the eye can lead to gradual loss of vision); seizures; ulcers; blockage in the passage between the stomach and intestine; blockage in the bladder; asthma or other lung disease; sleep apnea; cancer;any condition that affects the production of blood cells in your bone marrow; or heart or liver disease. If you will be giving promethazine to a child, also tell the child’s doctor if the child has any of the following symptoms before he or she receives the medication: vomiting, listlessness, drowsiness, confusion, aggression, seizures, yellowing of the skin or eyes, weakness, or flu-like symptoms. Also tell the child’s doctor if the child has not been drinking normally, has had excessive vomiting or diarrhea, or appears dehydrated.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking promethazine, call your doctor.
talk to your doctor about the risks and benefits of taking promethazine if you are 65 years of age or older. Older adults should not usually take promethazine because it is not as safe as other medications that can be used to treat the same conditions. - if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking promethazine.
- you should know that promethazine may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you. If you are giving promethazine to a child, watch the child to be sure he or she does not get hurt while riding a bike or participating in other activities that could be dangerous.
- ask your doctor about the safe use of alcohol while you are taking this medication. Alcohol can make the side effects of promethazine worse.
- plan to avoid unnecessary or prolonged exposure to sunlight and to wear protective clothing, sunglasses, and sunscreen. Promethazine may make your skin sensitive to sunlight.
Who can and can’t take promethazine
Promethazine can be taken by most adults and children aged 2 years and above.
Promethazine isn’t suitable for some people. Tell your doctor or pharmacist if you:
- have had an allergic reaction to promethazine or any other medicines in the past
- have an eye problem called primary angle closure glaucoma
- have problems peeing or emptying your bladder
- have epilepsy or any other health problem that causes fits
- have an intolerance to, or can’t absorb, some sugars, such as lactose or sorbitol
- are due to have an allergy test. Promethazine can affect your results, so you may need to stop taking it a few days before your test. Ask the clinic where you are due to have your allergy test.
- are unable to have any alcohol. Some liquid promethazine products contain a very small amount of alcohol, so check the ingredients and the packaging carefully.
- are trying to get pregnant. Promethazine can affect home pregnancy tests. If you think you’re pregnant, speak to your doctor so they can arrange a blood test instead.
Serious side effects, such as convulsions, are more likely to occur in younger patients and would be of greater risk to infants than to older children or adults. Also, nightmares or unusual excitement, nervousness, restlessness, or irritability may be more likely to occur in children.
The use of promethazine is not recommended in children who have a history of difficulty in breathing while sleeping or a family history of sudden infant death syndrome (SIDS), or in children under 2 years of age.
Children or adolescents who show signs of Reye’s syndrome should not be given this medicine.
Uncontrolled movements that may occur with Promethazine may be mistakenly confused with symptoms of Reye’s syndrome.
Promethazine pregnancy and breastfeeding
Your doctor may want to prescribe promethazine for morning sickness when other treatments haven’t worked.
Pregnant women have taken promethazine with no harmful effects to the mother or baby. But for safety it’s best to take it for the shortest possible time.
Can taking promethazine made it harder for me to get pregnant?
There are no studies looking at whether taking promethazine could make it harder to get pregnant.
I just found out I am pregnant. Should I stop taking promethazine?
Talk with your healthcare provider before making any changes to your medications. If you are experiencing nausea and vomiting that is affecting your daily life, please contact your healthcare provider. The combination of doxylamine succinate (an antihistamine) and pyridoxine hydrochloride (vitamin B6) has been shown to be an effective nausea and vomiting during pregnancy treatment. It is recommended as a first-line treatment by the American Congress of
Obstetricians and Gynecologists and several medical organizations in Canada.
Can promethazine increase the chance for a miscarriage?
One small study did not notice an increased chance for miscarriage among women taking promethazine.
Can use of promethazine during pregnancy cause birth defects?
This would be unlikely. The majority of studies do not suggest that promethazine would increase the chance for birth defects when used during the 1st trimester.
Can use of promethazine cause other pregnancy complications?
The use of promethazine late in pregnancy might increase the chance of respiratory depression (slow breathing rate) in newborn babies.
Can I breastfeed while using promethazine?
There is no data on the use of promethazine while breastfeeding. Promethazine passes into breast milk in small amounts. Because promethazine can cause sleepiness in adults, it may do the same for a nursing baby. For this reason it may not be a preferred antihistamine for long-term use during breastfeeding. If you use promethazine routinely while breastfeeding, monitor your baby for sedation and lack of energy and report any of these symptoms to your health care provider. It is possible, but not proven, that promethazine could lower the amount of milk a woman makes. If you are having trouble producing milk, consider meeting with a lactation specialist. Be sure to talk to your healthcare providers about all of your breastfeeding questions.
It’s usually safe to take similar antihistamines like loratadine or cetirizine while you’re breastfeeding.
If you need a drowsy antihistamine to help you sleep, your doctor may recommend chlorphenamine.
But speak to your doctor before taking any antihistamine if your baby was premature, had a low birth weight, or has health problems.
What if the father of the baby takes promethazine?
There is no evidence suggesting that a man’s promethazine use would cause problems conceiving a baby or problems during pregnancy. In general, exposures that fathers have are unlikely to increase risks to a pregnancy.
Cautions with other medicines
Some medicines and promethazine interfere with each other and increase the chance of having side effects.
Tell your doctor or pharmacist if you are taking any other medicines, including medicines that you get without a prescription from your pharmacy, supermarket or health food shop.
Some medicines and promethazine may interfere with each other. These include:
- anticholinergic medicines, including medicines for stomach spasm
- anticonvulsants or medicines for epilepsy/fits/seizures
- beta blockers such as propranolol, medicines used to lower blood pressure
- bromocriptine, a medicine used to treat Parkinson’s disease, acromegaly or to prevent lactation
- central nervous system depressants (medicines that cause drowsiness or sleepiness) such as sedatives, tranquillisers, barbiturates, antihistamines, general anaesthetics and alcohol
- levodopa (medicine for Parkinson’s disease)
- metrizamide, a contrast agent, injected into the spinal cord before an x-ray
- monoamine oxidase (MAO) inhibitors (medicine for depression), such as phenelzine
- phenothiazines (medicine for thought disorder)
- quinidine, a medicine for rapid or irregular heartbeat
- medicines to treat cold and flu
- appetite suppressants
- tricyclic antidepressants (medicine for depression)
- any medicine that makes you drowsy, gives you a dry mouth, or makes it difficult for you to pee. Taking promethazine might make these side effects worse.
These medicines may be affected by promethazine or may affect how well it works. You may need different amounts of your medicine, or you may need to take different medicines.
Your doctor or pharmacist has more information on medicines to be careful with or avoid while being treated with this medicine.
If you’re taking a cough or cold remedy or a painkiller containing promethazine, check carefully what the other ingredients are.
For example, promethazine often comes mixed with paracetamol. If you take 2 medicines that both contain paracetamol, there’s a risk of overdose.
Ask your pharmacist for advice before you take this medicine together with any other painkillers or medicines.
Mixing promethazine with herbal remedies and supplements
There might be a problem taking some herbal remedies and supplements alongside promethazine, especially ones that cause side effects such as sleepiness, a dry mouth or making it difficult to pee.
Ask your pharmacist for advice.
What does promethazine do?
Promethazine is a medicine called an antihistamine. It’s classed as a drowsy (sedating) antihistamine. Promethazine is a phenothiazine derivative with antiemetic, sedative and antihistaminic properties. Promethazine antagonizes the central and peripheral effects of histamine mediated by histamine H1 receptors. The effects of promethazine include bronchoconstriction, vasodilation and spasmodic contractions of gastrointestinal smooth muscle. In addition, promethazine binds to muscarinic receptors, resulting in anticholinergic and antiemetic activities.
When you come into contact with something you’re allergic to, such as pollen or animal hair, your body produces a chemical called histamine. This can cause symptoms such as a runny nose or skin rashes.
Promethazine blocks the effects of histamine in your brain and this reduces symptoms.
It enters the brain in large quantities and this can make you feel drowsy.
Promethazine also blocks the effects of a chemical called dopamine, and this stops you feeling sick.
How is promethazine different from other cough and cold remedies?
Promethazine blocks the effects of a natural chemical called acetylcholine. This can help dry up a cough or runny nose, but can also cause side effects such as a dry mouth and dry nose.
Some cough and cold remedies claim to suppress your cough or stop you bringing up phlegm. Although some people find them helpful, they’re not usually recommended. This is because there’s little evidence that they’re any more effective than simple home remedies and they’re not suitable for everyone.
What is promethazine used for?
Promethazine is used to relieve the symptoms of allergic reactions such as allergic rhinitis (runny nose and watery eyes caused by allergy to pollen, mold or dust), allergic conjunctivitis (red, watery eyes caused by allergies), allergic skin reactions, and allergic reactions to blood or plasma products. Promethazine is known as a drowsy (sedating) antihistamine. Promethazine is more likely to make you feel sleepy than other antihistamines. Promethazine is used with other medications to treat anaphylaxis (sudden, severe allergic reactions) and the symptoms of the common cold such as sneezing, cough, and runny nose.
Promethazine is used for:
- sedation (to help sleep) for short-term sleep problems (insomnia) – including when a cough or cold, or itching, is keeping you awake at night
- allergies, including hay fever and hives (urticaria)
- feeling and being sick (vomiting) – due to morning sickness, travel sickness or vertigo
- cough and cold symptoms, such as coughing and a runny nose
Promethazine is also used to relax and sedate patients before and after surgery, during labor, and at other times. Promethazine is also used to prevent and control nausea and vomiting that may occur after surgery and with other medications to help relieve pain after surgery. Promethazine is also used to prevent and treat motion sickness.
Promethazine dosage
Promethazine comes in 10mg, 20mg and 25mg tablets and a liquid that you swallow.
If you’re taking liquid promethazine, follow the instructions that come with the medicine for how much to take.
If you’re taking promethazine tablets, your dose depends on why you’re taking it:
- short-term insomnia – you’ll usually take 20 to 50mg at night
- hay fever – you’ll usually take 10mg twice a day to 20mg 3 times a day
- hives – you’ll usually take 10mg twice a day to 20mg 3 times a day
- preventing travel sickness – 25mg taken 1 to 2 hours before a short journey or 25mg the night before a long journey
- treating travel sickness – take 25mg as soon as possible and 25mg the same evening, followed by 25mg the following evening (if you need it)
- morning sickness and vertigo – the dose can vary from 25mg a day to 25mg 4 times a day
Promethazine comes mixed with other ingredients for cough and cold symptoms – the usual dose depends on the type of medicine you’re taking.
Check the instructions on the packaging carefully, or ask your pharmacist or doctor if you’re unsure.
Doses are lower for children. Your doctor will use your child’s age to work out the right dose.
How to take promethazine
You can take promethazine tablets, capsules and liquid with or without food.
Always take your promethazine tablets or capsules with a drink of water. Swallow them whole. Do not chew them.
Liquid medicines containing promethazine come with a plastic syringe or spoon to help you measure out the right dose.
If you don’t have a syringe or spoon, ask your pharmacist for one. Do not use a kitchen teaspoon as you won’t get the right amount.
To insert a promethazine suppository, follow these steps:
- If the suppository feels soft, hold it under cold, running water for 1 minute. Remove the wrapper.
- Dip the tip of the suppository in water.
- Lie down on your left side and raise your right knee to your chest. (A left-handed person should lie on the right side and raise the left knee.)
- Using your finger, insert the suppository into the rectum, about 1/2 to 1 inch (1.25 to 2.5 centimeters) in children who are 2 years of age older and 1 inch (2.5 centimeters) in adults. Hold it in place for a few moments.
- Stand up after about 15 minutes. Wash your hands thoroughly and resume your normal activities.
Adult Dose for Allergic Reaction
Uses:
- Allergic conjunctivitis due to inhalant allergens and foods
- Amelioration of allergic reactions to blood or plasma
- Dermographism
- In anaphylaxis as an adjunct to epinephrine and other standard measures after the acute symptoms have been controlled
- Mild, uncomplicated allergic skin manifestations of urticaria and angioedema
- Other uncomplicated allergic condition of the immediate type when oral therapy is impossible or contraindicated
- Perennial and seasonal allergic rhinitis
- Vasomotor rhinitis
Oral or Rectal:
- 6.25 to 12.5 mg orally or rectally before meals and at bedtime, if necessary, OR 25 mg orally or rectally once a day at bedtime
Parenteral:
- 25 mg IM or IV once, and may be repeated within 2 hours if necessary
Comments:
- Once treatment begins, the dose should be reduced to the smallest effective amount needed to control symptoms.
- Minor transfusion and/or amelioration of allergic reactions may be controlled with 25 mg doses.
Adult Dose for Allergic Rhinitis
Uses:
- Allergic conjunctivitis due to inhalant allergens and foods
- Amelioration of allergic reactions to blood or plasma
- Dermographism
- In anaphylaxis as an adjunct to epinephrine and other standard measures after the acute symptoms have been controlled
- Mild, uncomplicated allergic skin manifestations of urticaria and angioedema
- Other uncomplicated allergic condition of the immediate type when oral therapy is impossible or contraindicated
- Perennial and seasonal allergic rhinitis
- Vasomotor rhinitis
Oral or Rectal:
- 6.25 to 12.5 mg orally or rectally before meals and at bedtime, if necessary, OR 25 mg orally or rectally once a day at bedtime
Parenteral:
- 25 mg IM or IV once, and may be repeated within 2 hours if necessary
Comments:
- Once treatment begins, the dose should be reduced to the smallest effective amount needed to control symptoms.
- Minor transfusion and/or amelioration of allergic reactions may be controlled with 25 mg doses.
Adult Dose for Anaphylaxis
Uses:
- Allergic conjunctivitis due to inhalant allergens and foods
- Amelioration of allergic reactions to blood or plasma
- Dermographism
- In anaphylaxis as an adjunct to epinephrine and other standard measures after the acute symptoms have been controlled
- Mild, uncomplicated allergic skin manifestations of urticaria and angioedema
- Other uncomplicated allergic condition of the immediate type when oral therapy is impossible or contraindicated
- Perennial and seasonal allergic rhinitis
- Vasomotor rhinitis
Oral or Rectal:
- 6.25 to 12.5 mg orally or rectally before meals and at bedtime, if necessary, OR 25 mg orally or rectally once a day at bedtime
Parenteral:
- 25 mg IM or IV once, and may be repeated within 2 hours if necessary
Comments:
- Once treatment begins, the dose should be reduced to the smallest effective amount needed to control symptoms.
- Minor transfusion and/or amelioration of allergic reactions may be controlled with 25 mg doses.
Adult Dose for Urticaria
Uses:
- Allergic conjunctivitis due to inhalant allergens and foods
- Amelioration of allergic reactions to blood or plasma
- Dermographism
- In anaphylaxis as an adjunct to epinephrine and other standard measures after the acute symptoms have been controlled
- Mild, uncomplicated allergic skin manifestations of urticaria and angioedema
- Other uncomplicated allergic condition of the immediate type when oral therapy is impossible or contraindicated
- Perennial and seasonal allergic rhinitis
- Vasomotor rhinitis
Oral or Rectal:
- 6.25 to 12.5 mg orally or rectally before meals and at bedtime, if necessary, OR 25 mg orally or rectally once a day at bedtime
Parenteral:
- 25 mg IM or IV once, and may be repeated within 2 hours if necessary
Comments:
- Once treatment begins, the dose should be reduced to the smallest effective amount needed to control symptoms.
- Minor transfusion and/or amelioration of allergic reactions may be controlled with 25 mg doses.
Adult Dose for Light Sedation
Uses:
- For sedation and relief of apprehension and to produce light sleep from which the patient can be easily aroused
- Preoperative, postoperative, and obstetric (during labor) sedation
Oral or Rectal:
- 25 to 50 mg orally or rectally once
Parenteral:
- Early stages of labor: 50 mg IM or IV once
- Nighttime sedation: 25 to 50 mg IM or IV once
Comments:
- Oral and rectal formulations may be used for nighttime, presurgical, or obstetrical sedation.
- Sedative doses may be given the night before surgery.
- Preoperative doses should be given with appropriate doses of an analgesic/hypnotic and an atropine-like agent.
Adult Dose for Sedation
Uses:
- For sedation and relief of apprehension and to produce light sleep from which the patient can be easily aroused
- Preoperative, postoperative, and obstetric (during labor) sedation
Oral or Rectal:
- 25 to 50 mg orally or rectally once
Parenteral:
- Early stages of labor: 50 mg IM or IV once
- Nighttime sedation: 25 to 50 mg IM or IV once
Comments:
- Oral and rectal formulations may be used for nighttime, presurgical, or obstetrical sedation.
- Sedative doses may be given the night before surgery.
- Preoperative doses should be given with appropriate doses of an analgesic/hypnotic and an atropine-like agent.
Adult Dose for Motion Sickness
Use:
Active and prophylactic treatment of motion sickness
Oral and Rectal:
- 25 mg orally, or rectally once, then 12.5 to 25 mg every 4 to 6 hours as needed
Parenteral:
- 12.5 to 25 mg IM or IV every 4 hours as needed
Prophylaxis:
- Initial day: 25 mg orally or rectally 30 to 60 minutes before traveling, then 8 to 12 hours as needed
- Succeeding days of travel: 25 mg orally or rectally upon rising, with the dose repeated before the evening meal
Comment:
Oral formulations are preferred; however, rectal or parenteral formulations may be given if oral formulations are not tolerated.
Adult Dose for Nausea and Vomiting
Uses:
- Prevention and control of nausea and vomiting associated with certain types of anesthesia and surgery
- Antiemetic therapy in postoperative patients
Treatment:
- 12.5 to 25 mg IM, IV, orally, or rectally every 4 hours as needed
Prophylaxis:
- Oral and Rectal: 25 mg orally every 4 to 6 hours as needed
Comments:
- Parenteral or rectal formulations may be used when patients cannot tolerate oral formulations.
- Prophylactic doses may be used to prevent nausea and vomiting during surgery and the postoperative period.
Adult Dose for Opiate Adjunct
Uses:
- Administered IV as an adjunct to anesthesia or analgesia with reduced amounts of meperidine of other narcotic analgesics in special surgical situations (e.g., repeated bronchoscopy, ophthalmic surgery, poor-risk patients)
- Therapy adjunctive to meperidine or other analgesics for control of postoperative pain
Parenteral:
- Pre- or postoperative use: 25 to 50 mg IM or IV once
- Established labor: 25 to 75 mg IM or IV, repeated up to 2 times in 4-hour intervals
- Maximum dose: 100 mg every 24 hours
Comments:
- The average parenteral dose given during established labor is 50 mg.
- Preoperative doses should be given with appropriate doses of an analgesic/hypnotic and an atropine-like agent.
Pediatric Dose for Allergic Reaction
Uses:
- Perennial and seasonal allergic rhinitis
- Vasomotor rhinitis
- Allergic conjunctivitis due to inhalant allergens and foods
- Mild, uncomplicated allergic skin manifestations of urticaria and angioedema
- Amelioration of allergic reactions to blood or plasma
- Dermographism
- Adjunctive therapy to epinephrine and other standard measures for anaphylactic reactions, after acute manifestations have been controlled
2 years and older
Oral or Rectal:
- 6.25 to 12.5 mg orally or rectally before meals and at bedtime, as necessary OR 25 mg orally or rectally once a day at bedtime
Parenteral:
- 12.5 mg IM or IV once, and may be repeated within 2 hours if necessary
Comments:
- Once treatment begins, the dose should be reduced to the smallest effective amount needed to control symptoms.
- Minor transfusion and/or amelioration of allergic reactions may be controlled with 12.5 mg doses.
Pediatric Dose for Motion Sickness
Use:
- Active and prophylactic treatment of motion sickness
2 years and older
Treatment:
- Parenteral: 6.25 to 12.5 mg IM or IV every 4 hours a day
Treatment and prevention:
- Oral and Rectal: 12.5 to 25 mg orally or rectally 2 times a day
Comments:
- The initial dose should be given 30 to 60 minutes before anticipated travel, and may be repeated in 8 to 12 hours as needed.
- Subsequent doses on succeeding days of travel should be given on rising and again before the evening meal.
Pediatric Dose for Nausea and Vomiting
Uses:
- Prevention and control of nausea and vomiting associated with certain types of anesthesia and surgery
- Antiemetic therapy in postoperative patients
2 years and older
Treatment:
- Oral or Rectal: 1.1 mg/kg orally or rectally every 4 to 6 hours as needed
- Maximum dose: 25 mg
- Parenteral: 6.25 to 12.5 mg IM or IV every 4 hours as needed
- Prophylaxis: Up to 25 mg orally or rectally every 4 to 6 hours as needed
Comments:
- This drug should not be used to treat nausea and vomiting of unknown etiology.
- Doses should be adjusted to the age and severity of the patient.
Pediatric Dose for Light Sedation
Uses:
- Preoperative, postoperative, or obstetric sedation
- Relief of apprehension and production of light sleep from which the patient can be easily aroused
2 years and older
- Preoperative medication: 1.1 mg/kg IM, IV, orally, or rectally once
- Maximum dose: Up 25 mg
- Sedation and/or adjunctive use with analgesics: 12.5 to 25 mg IM, IV, orally, or rectally once
Comments:
- Sedative doses may be given the night before surgery.
- Preoperative doses should be given with appropriate doses of an analgesic/hypnotic and an atropine-like agent.
Pediatric Dose for Sedation
Uses:
- Preoperative, postoperative, or obstetric sedation
- Relief of apprehension and production of light sleep from which the patient can be easily aroused
2 years and older
- Preoperative medication: 1.1 mg/kg IM, IV, orally, or rectally once
- Maximum dose: Up 25 mg
- Sedation and/or adjunctive use with analgesics: 12.5 to 25 mg IM, IV, orally, or rectally once
Comments:
- Sedative doses may be given the night before surgery.
- Preoperative doses should be given with appropriate doses of an analgesic/hypnotic and an atropine-like agent.
Renal Dose Adjustments
Data not available
Liver Dose Adjustments
Use with caution.
Dose Adjustments
65 years and older: Elderly patients should be given lower initial doses and should be closely monitored for adverse events.
What should I do if I forget a dose?
For travel sickness, take it as soon as you remember.
For anything else, skip the missed dose and take your next dose at the usual time.
Never take 2 doses at the same time. Never take an extra dose to make up for a forgotten one.
If you forget doses often, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
What if I take too much promethazine?
Too much promethazine can be dangerous.
If you have accidentally taken too much promethazine, you may:
- feel very sleepy
- have a very fast, uneven or pounding heartbeat (palpitations)
- have breathing problems
In serious cases, you can become unconscious or have fits and may need emergency treatment in hospital.
If your child takes too much promethazine, they may also:
- move unsteadily or stumble
- have uncontrolled movements, especially in their hands or feet
- see or hear things that aren’t there (hallucinations)
- have an uneven heartbeat
Call your doctor straight away if you take too much promethazine by accident
If you need to go to a hospital accident and emergency (A&E) department, do not drive yourself – get someone else to drive you or call for an ambulance.
Take the promethazine packet or leaflet inside it, plus any remaining medicine, with you.
Promethazine side effects
Promethazine can cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- dry mouth
- drowsiness
- listlessness
- difficulty falling asleep or staying asleep
- nightmares
- dizziness
- ringing in ears
- blurred or double vision
- loss of coordination
- nausea
- vomiting
- nervousness
- restlessness
- hyperactivity
- abnormally happy mood
- stuffy nose
- itching
Promethazine can sometimes make your skin more sensitive to sunlight. Keep out of direct or strong sunlight and follow sun safety advice.
If you’re over 65, you’re more likely to experience side effects such as:
- feeling confused
- dry mouth
- blurred vision
- difficulty peeing
Children are more likely to experience side effects such as feeling restless or excited.
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately:
- wheezing
- slowed breathing
- breathing stops for a short time
- bruising or bleeding that’s more than normal
- muscle stiffness or shaking, or unusual face or tongue movements
- fever
- sweating
- stiff muscles
- decreased alertness
- fast or irregular pulse or heartbeat
- faintness
- abnormal or uncontrollable movements
- hallucinations (seeing things or hearing voices that do not exist)
- confusion
- overwhelming or unmanageable fear or emotion
- seizures
- uncontrollable shaking of a part of the body
- unusual bruising or bleeding
- sore throat, fever, chills, and other signs of infection
- uncontrolled eye movements
- tongue sticking out
- abnormal neck position
- inability to respond to people around you
- yellowing of the skin or eyes (jaundice) – these can be signs of liver problems
- rash
- hives
- swelling of the face, eyes, lips, tongue, throat, arms, hands, feet, ankles, or lower legs
- hoarseness
- difficulty breathing or swallowing
These aren’t all the side effects of promethazine. For a full list, see the leaflet inside your medicine packet. Call your doctor if you experience any unusual problems while you are taking promethazine.
Serious allergic reaction
In rare cases, it’s possible to have a serious allergic reaction (anaphylaxis) to promethazine.
Contact a doctor straight away if:
- you get a skin rash that may include itchy, red, swollen, blistered or peeling skin
- you’re wheezing
- you get tightness in the chest or throat
- you have trouble breathing or talking
- your mouth, face, lips, tongue or throat start swelling
These are warning signs of a serious allergic reaction. A serious allergic reaction is an emergency.
How to cope with side effects
What to do about:
- feeling sleepy during the daytime – this usually wears off 12 hours after a dose. Do not drive or use tools or machinery if you’re feeling this way.
- nightmares – speak to your pharmacist or doctor if these don’t go away or are troubling you
- feeling dizzy or unsteady on your feet, or having difficulty concentrating – stop what you’re doing and sit or lie down until you feel better. If the feeling
- doesn’t go away or is troubling you, do not take any more medicine and speak to a pharmacist or your doctor.
- headaches – make sure you rest and drink plenty of fluids. Talk to your doctor if the headaches last longer than a week or are severe.
Promethazine overdose
In case of overdose, call the poison control helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help. If the victim has collapsed, had a seizure, has trouble breathing, or can’t be awakened, immediately call your local emergency services number.
Symptoms of promethazine overdose may include:
- difficulty breathing
- slowed or stopped breathing
- dizziness
- lightheadedness
- fainting
- loss of consciousness
- fast heartbeat
- tight muscles that are difficult to move
- loss of coordination
- continuous twisting movements of the hands and feet
- dry mouth
- wide pupils (black circles in the middle of the eyes)
- flushing
- nausea
- constipation
- abnormal excitement or agitation
- nightmares
Bladder and kidneys
- Urinary hesitancy
- Inability to urinate
Heart and blood vessels
- Rapid heartbeat
- Weakness from low blood pressure
Nervous system
- Drowsiness or even coma
- Agitation, confusion, excitation, disorientation
- Depression
- Nervousness, hallucinations
- Fever
- Unsteadiness
- Seizures
- Tremor (unintentional trembling)
Other:
- Flushed skin
- Involuntary tongue movement
- Large (dilated) pupils with vision difficulty
- Muscle stiffness in face or neck
What to expect at the emergency room
The health care provider will measure and monitor the person’s vital signs, including temperature, pulse, breathing rate, and blood pressure. Symptoms will be treated as appropriate. The person may receive:
- Activated charcoal
- Airway support, including oxygen, breathing tube through the mouth (intubation),and ventilator (breathing machine)
- Blood and urine tests
- Chest x-ray
- ECG (electrocardiogram, or heart tracing)
- Fluids through the vein (intravenous or IV)
- Laxative
- Medicines to treat symptoms
Promethazine overdose prognosis
If the person survives the first 24 hours, recovery is likely. People who experience heart rhythm irregularities and seizures are at highest risk for a serious outcome. Few people actually die from promethazine overdose.