Pulmonary edema
Pulmonary edema is a condition caused by an abnormal buildup of fluid in your lungs causing disturbance of the gas exchange that may lead to respiratory failure, shortness of breath (dyspnea) and can be life-threatening 1. This abnormal buildup of fluid in your lungs collects in the many air sacs in the lungs (alveoli), making it difficult for you to breathe. Pulmonary edema is caused by direct injury to the lung tissues or congestive heart failure. But fluid can collect in your lungs for other reasons. These include pneumonia, contact with certain toxins, medications, trauma to the chest wall, and traveling to or exercising at high elevations also known high-altitude pulmonary edema (HAPE) or pulmonary edema of mountaineers. High-altitude pulmonary edema (HAPE) can be fatal if not treated. However, in most cases, heart problems cause pulmonary edema.
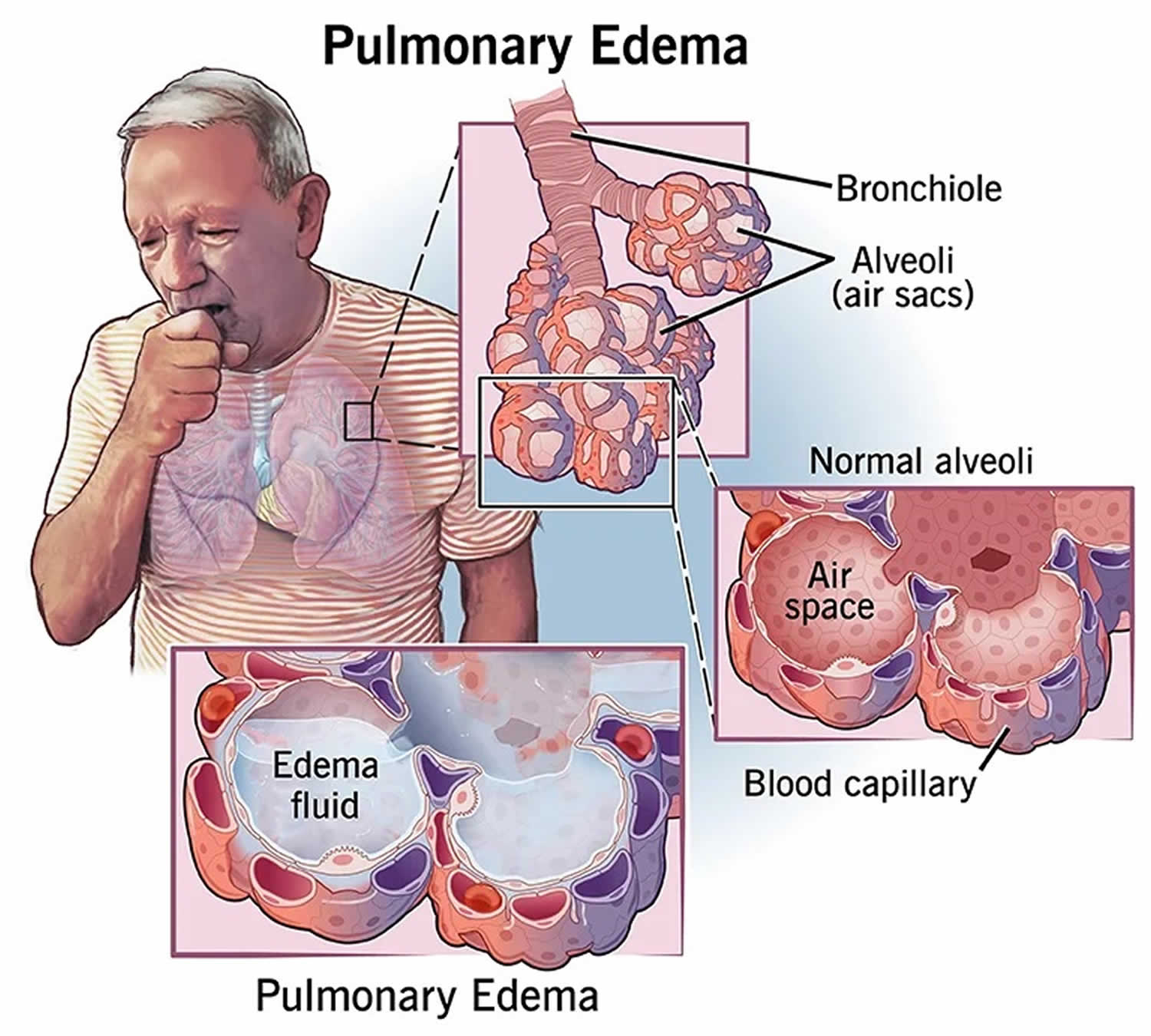
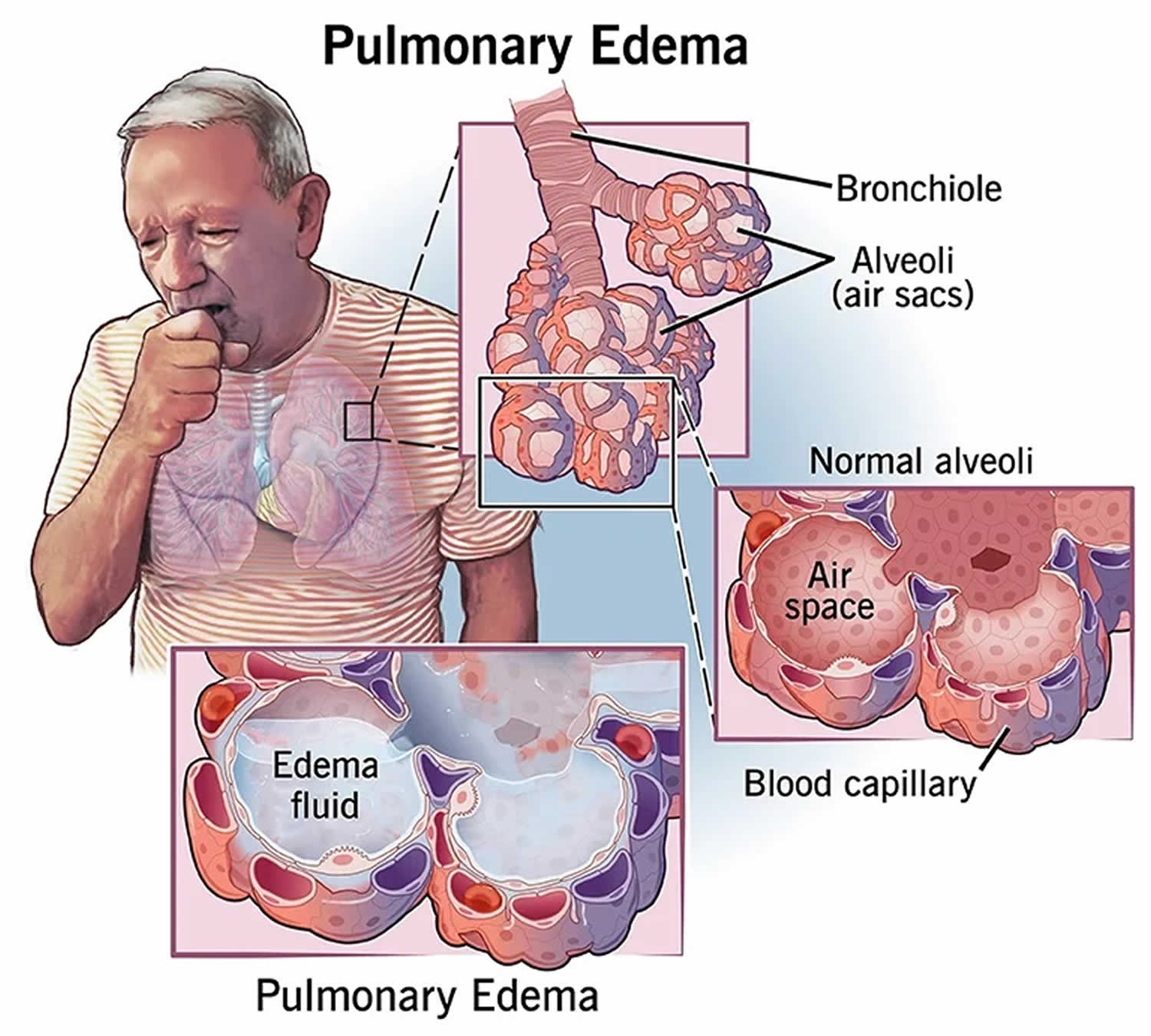
Understanding the relationship between your lungs and your heart can help explain why pulmonary edema may occur. Your lungs contain many small, elastic air sacs called alveoli (Figure 1). With each breath, these air sacs take in oxygen and release carbon dioxide. Typically, this exchange of gases occurs without problems. But sometimes, the alveoli are filled with fluid instead of air. This keeps the bloodstream from taking in oxygen. Typically, blood without oxygen from all over your body enters the right atrium then the right ventricle (Figure 2). From the right ventricle blood without oxygen is pumped through large blood vessels called the pulmonary arteries to the lungs. There, the blood releases carbon dioxide and picks up oxygen as it flows by the alveoli. The oxygen-rich blood then returns to the left atrium through the pulmonary veins. It then flows through the mitral valve into the left ventricle. Finally, it leaves the heart through the body’s main artery (aorta). The heart valves keep blood flowing in the right direction. The aortic valve keeps the blood from flowing backward into the heart. From the aorta, the blood travels to the rest of the body.
Pulmonary edema symptoms may appear suddenly (acute pulmonary edema) or gradually (chronic pulmonary edema). Suddenly appearing symptoms of pulmonary edema include difficulty breathing, feeling of suffocation, and coughing associated with frothy sputum. Gradually appearing symptoms of pulmonary edema include difficulty breathing while lying in bed, shortness of breath during activity, and weight gain (in patients with congestive heart failure).
Pulmonary edema that develops suddenly (acute pulmonary edema) is a medical emergency that needs immediate care. Pulmonary edema can sometimes cause death.
If you have sudden (acute) pulmonary edema, you need immediate treatment. You may need to be treated in the emergency room (ER) or intensive care unit (ICU).
Some treatment options include:
- Oxygen delivered through prongs in your nose.
- Machines that blow air into your lungs through a mask on your face.
- Ventilators or respirators that blow in air through a tube inserted into your windpipe.
- Medications that cause you to urinate more and get rid of fluid or which strengthen your heart.
- Other medications, when congestive heart failure isn’t the cause of your pulmonary edema, such as antibiotics and steroids.
Figure 1. Pulmonary edema
Figure 2. Pulmonary circulation
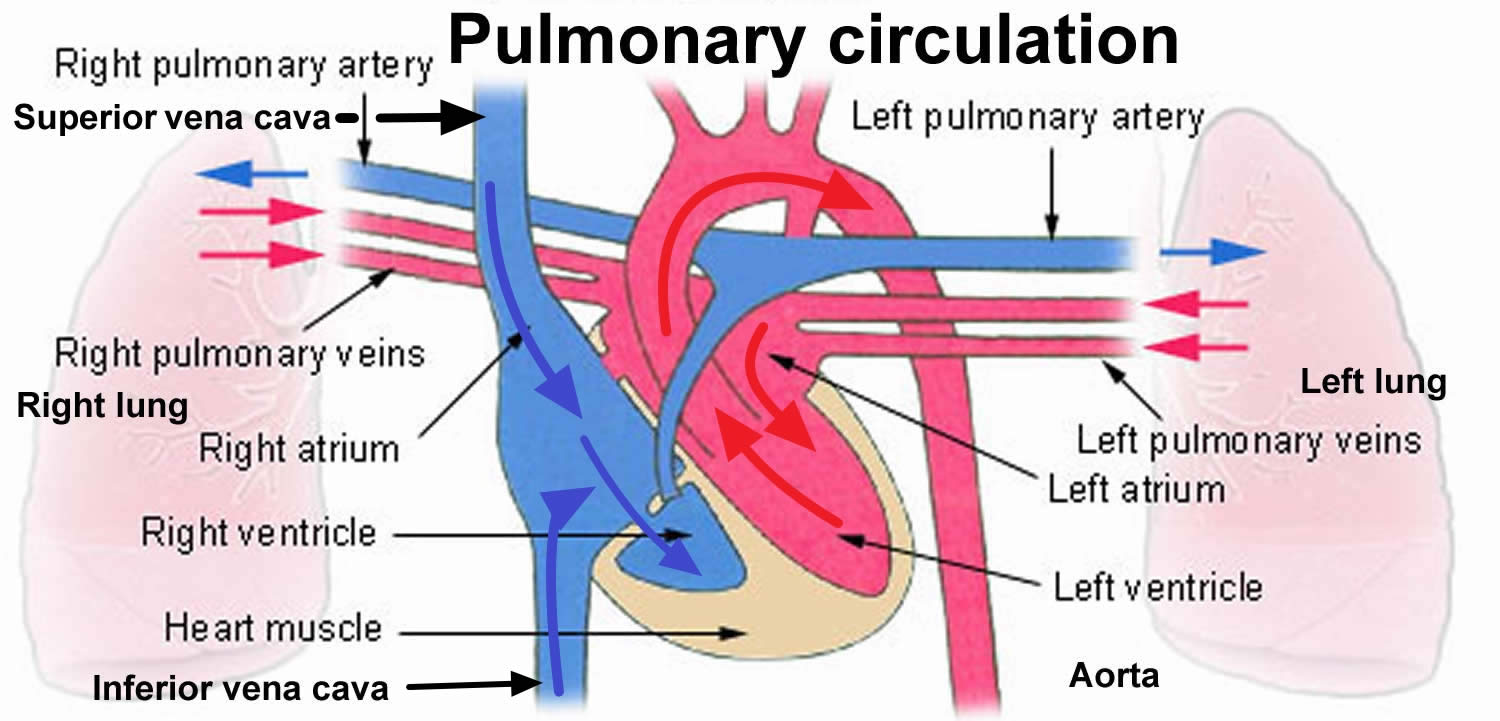
Figure 3. Pulmonary edema chest X-ray
Footnote: Acute pulmonary edema showing alveolar edema (white arrows) and interstitial edema (black arrowheads). Alveolar edema manifests as ill-defined nodular opacities tending to confluence (white arrows). Interstitial edema can be seen as peripheral septal lines – Kerley B lines (black arrowheads).
[Source 2 ]Figure 4. Unilateral pulmonary edema
Footnote: Unilateral pulmonary edema from acute mitral regurgitation. Right upper lobe ground glass alveolar opacity and air bronchogram sign. Differential diagnoses include blood, pus, water and protein. Left lung is clear. No pleural effusions. Cardiac catheterization showed no coronary artery disease and patient had a prosthetic Carpentier Edwards mitral valve placement.
[Source 3 ]Figure 5. Pulmonary edema CT
Footnotes: Bilateral airspace opacification in a central peribronchovascular distribution is seen, associated with smooth interlobular septal thickening (which indicates interstitial edema) and bilateral moderate pleural effusions with underlying segmental basal consolidation/collapse. Mild cardiac enlargement is noted. Reactive mediastinal and right epiphrenic lymphadenopathy and mild cirrhotic changes of the liver are also seen.
[Source 4 ]Pulmonary edema that comes on suddenly (acute pulmonary edema) is life-threatening. Call your local emergency services number or emergency medical help if you have any of the following acute symptoms:
- Shortness of breath, especially if it comes on suddenly
- Trouble breathing or a feeling of suffocating (dyspnea)
- A bubbly, wheezing or gasping sound when breathing
- Coughing up phlegm that looks pink or has blood in it
- Breathing difficulty with a lot of sweating
- A blue or gray color to the skin
- Confusion
- A big drop in blood pressure that causes lightheadedness, dizziness, weakness or sweating
- A sudden worsening of any of pulmonary edema symptoms
Don’t drive yourself to the hospital. Instead, call your local emergency services number or emergency medical care and wait for help.
What’s the difference between pulmonary edema and pneumonia?
Both pulmonary edema and pneumonia involve a buildup of fluid in your lungs. An infection causes pneumonia. The infection can be viral, bacterial or fungal. These organisms can cause infected fluid to fill your air sacs. An infection doesn’t cause pulmonary edema, and the fluid is typically thinner and watery.
What’s the difference between pulmonary edema and pleural effusion?
Pleural effusion is when abnormal amounts of fluid buildup outside of your lungs in the pleura, which is a lining around your lungs. The pleura sits between your lungs and the inside of your chest wall, and usually only has a thin rim of fluid inside it. Pleural effusion is commonly caused by pneumonia, congestive heart failure or cancer. Unlike pulmonary edema, the fluid sits outside of your lungs and can compress your lungs, which are spongy.
Does pulmonary edema require hospitalization?
Pulmonary edema is a serious condition. If you have acute (sudden) pulmonary edema, you need immediate treatment. You may be treated in the emergency room (ER) or intensive care unit (ICU). Chronic pulmonary edema may require hospitalization as well.
Can pulmonary edema cause sudden death?
Severe cases of pulmonary edema can be life-threatening if you don’t receive treatment right away. With immediate treatment, your chances of recovery are higher.
Pulmonary edema causes
The causes of pulmonary edema vary. The causes of pulmonary edema can be broken down into two groups: cardiogenic (heart-related) or noncardiogenic (not heart-related), depending on where the problem starts.
- Cardiogenic pulmonary edema (volume-overload pulmonary edema) if a heart problem causes the pulmonary edema. Most often, the fluid buildup in your lungs is due to a heart condition. Cardiogenic pulmonary edema arises due to a rapid elevation in the hydrostatic pressure of the pulmonary capillaries. This is typically seen in disorders involving left ventricular systolic and diastolic function (acute myocarditis including other causes of non-ischemic cardiomyopathy, heart attack), valvular function (aortic/mitral regurgitation and stenosis in the moderate to the severe range), rhythm (atrial fibrillation with a rapid ventricular response, ventricular tachycardia, high degree, and third-degree heart block) 5.
- Noncardiogenic pulmonary edema if pulmonary edema is not heart related. Noncardiogenic pulmonary edema is caused by lung injury with a resultant increase in pulmonary vascular permeability leading to the movement of fluid, rich in proteins, to the alveolar and interstitial compartments. Acute lung injury with severe hypoxemia is referred to as acute respiratory distress syndrome (ARDS) and is seen in various conditions directly affecting the lungs, such as pneumonia, inhalational injury, or indirectly, such as sepsis, acute pancreatitis, severe trauma with shock, multiple blood transfusions 6.
- Sometimes, pulmonary edema can be caused by both a heart problem and a nonheart problem.
More than 1 million patients are admitted each year with a diagnosis of pulmonary edema secondary to cardiac causes (heart failure) 7. An estimated 190,000 patients are diagnosed with acute lung injury each year 8. About 1.5 to 3.5 cases/100,000 population are diagnosed with acute respiratory distress syndrome (ARDS) 9.
Cardiogenic pulmonary edema means fluid backs up in your lungs from a heart problem. The most common cause of cardiogenic pulmonary edema is congestive heart failure. When a diseased or overworked left lower heart chamber (left ventricle) can’t pump out enough of the blood it gets from the lungs, pressures in the heart go up. The increased pressure pushes fluid through the blood vessel walls into the air sacs in your lungs.
Medical conditions that can cause heart failure and lead to pulmonary edema include 10:
- Coronary artery disease. Over time, the arteries that supply blood to the heart muscle can become narrow from fatty deposits (plaques). A slow narrowing of the coronary arteries can weaken the left ventricle. Sometimes, a blood clot forms in one of these narrowed arteries. The clot blocks blood flow and damages part of the heart muscle, resulting in a heart attack. A damaged heart muscle can no longer pump as well as it should.
- Cardiomyopathy. This term means heart muscle damage. With cardiomyopathy, the heart must pump harder, and pressures rise. Then the heart might not be able to work harder when needed, such as during exercise or with an infection or a rise in blood pressure. When the left ventricle can’t keep up with the demands that are placed on it, fluid backs up into the lungs.
- Heart valve problems. Narrowing (stenosis) of the aortic or mitral heart valves or a valve that leaks (regurgitation) or doesn’t close properly affects blood flow into the heart. A valve leak that develops suddenly might cause sudden and severe pulmonary edema.
- High blood pressure (hypertension). Untreated or uncontrolled high blood pressure can enlarge the heart.
- Fluid in the pericardium (pericardial effusion), a lining around your heart.
- Other heart problems. Inflammation of the heart muscle (myocarditis), heart problems present at birth (congenital heart defects) and abnormal heart rhythms (arrhythmias) also may cause pulmonary edema.
- Kidney disease. High blood pressure due to narrowed kidney arteries (renal artery stenosis) or fluid buildup due to kidney disease can cause pulmonary edema.
- Chronic health conditions. Thyroid disease and a buildup of iron (hemochromatosis) or protein (amyloidosis) also may contribute to heart failure and cause pulmonary edema.
Pulmonary edema that is not caused by increased pressures in the heart is called noncardiogenic pulmonary edema.
Noncardiogenic pulmonary edema isn’t caused by increased blood flow in your lungs due to a backup from heart problems. Instead, the blood vessels in your lungs become inflamed or injured. The blood vessels then become leaky, and fluid goes into your air sacs.
Causes of noncardiogenic pulmonary edema include 11, 10:
- Acute respiratory distress syndrome (ARDS). This serious disorder occurs when the lungs suddenly fill with fluid. Many conditions can cause acute respiratory distress syndrome (ARDS), including severe injury (trauma), widespread infection (sepsis), pneumonia and severe bleeding.
- Drug reaction or drug overdose. Many drugs — ranging from aspirin to illegal drugs such as heroin and cocaine — are known to cause pulmonary edema.
- Blood clot in the lungs (pulmonary embolism). A blood clot moving from the blood vessels in the legs to the lungs can cause pulmonary edema.
- Exposure to certain toxins. Inhaling toxins or breathing in some stomach contents when vomiting (aspiration) causes intense irritation of the small airways and air sacs, resulting in fluid buildup.
- High altitudes. Pulmonary edema has been seen in mountain climbers, skiers, hikers and other people who travel to high elevations, usually above 8,200 feet (about 2,500 meters). Air sacs in the lungs, called alveoli, take in oxygen and release carbon dioxide. In high-altitude pulmonary edema (HAPE), it’s believed that blood vessels in the lungs squeeze together (constrict), increasing pressure. This causes fluid to leak from the blood vessels to the lung tissues and eventually into the air sacs. High-altitude pulmonary edema (HAPE) generally occurs in those who don’t take the days or weeks needed to become used to the elevation. But people who live at high altitudes can get HAPE with no elevation change if they have a respiratory illness.
- Near drowning (asphyxiation pulmonary edema). Inhaling water causes fluid buildup in the lungs.
- Immersion pulmonary edema (IPE) also called swimming-induced pulmonary edema (SIPE) or scuba divers pulmonary edema (SDPE). Swimming-induced pulmonary edema (SIPE) occurs when competitive swimmers and divers develop lung injuries because their lung capillaries burst 12, 13, 14, 12, 15. Cases range from young, fit, military swimmers 13, 16, who have undergone careful medical screening, to older recreational athletes and divers with preexisting cardiopulmonary disease 17. While the exact pathophysiology of swimming-induced pulmonary edema (SIPE) remains uncertain, it is believed to include a combination of intense physical exertion, immersion in cold water, and overhydration, resulting in central pooling of blood, increased pulmonary arterial pressure, capillary damage, and subsequent pulmonary edema 18, 19, 20, 21, 22. Cold water is believed to be a major contributing factor to the underlying pathophysiology. However, there have been numerous case reports and studies with individuals diving in tropical waters of 30 to 35 °C. The majority of the incidence of immersion pulmonary edema (IPE) in warm water was diving-related, but it has been seen with extreme exertion and overhydration in swimmers 23. Swimming-induced pulmonary edema (SIPE) is characterized by acute onset of shortness of breath (dyspnea), cough, and occasionally coughing up blood (hemoptysis), and is associated with water immersion 24. The hallmark of SIPE has been described in the literature as a cough with a “frothy pink” sputum production 25. SIPE typically occurs in otherwise healthy individuals 12, 13, 26. A key feature in the majority of cases is a rapid resolution of symptoms within 48 hours. Initial management requires safe water evacuation to prevent drowning and to perform a preliminary assessment 27, 28, 29. Symptoms usually begin to resolve after exiting the water and management may be supportive. Supplementary oxygen is important. The affected individual is often transferred to hospital for further investigations and management. The prognosis is generally excellent when treated, though fatal cases have been reported 30. Recurrent episodes are unpredictable and are not uncommon 24. It has been proposed as a probable cause of unexplained death during swimming training in triathletes 31.
- Negative pressure pulmonary edema. A blocked upper airway causes negative pressure in the lungs from trying to breathe through the blockage. With treatment, most people with this type of pulmonary edema recover in about 24 hours.
- Neurogenic pulmonary edema (NPE) can occur after a head injury, seizure or brain surgery 32. The most common causes are subarachnoid hemorrhage 33, 34, 35, 36, 37, cerebral hemorrhage 38, traumatic brain injury (TBI) 39 and seizures 40, 41, 42.
- Smoke inhalation. Smoke from a fire contains chemicals that damage the membrane between the air sacs and the capillaries. The damage allows fluid to enter the lungs.
- Transfusion-related lung injury (TRALI). Transfusion-related acute lung injury (TRALI) is defined as new acute lung injury that occurs during or within six hours of blood transfusion, not explained by another acute lung injury risk factor 43. Blood transfusions may cause fluid overload in the left ventricle, leading to pulmonary edema.
- Fluid overload
- Pulmonary edema with acute asthma
- Postobstructive pulmonary edema / postintubation pulmonary edema/negative pressure pulmonary edema
- Heroin-induced pulmonary edema
- Pulmonary edema following administration of cytokines
- Reperfusion pulmonary edema
- Pulmonary edema following lung transplantation
- Re-expansion pulmonary edema
- Post-pneumonectomy pulmonary edema
- Post lung volume reduction pulmonary edema
- Viral illnesses. Viruses such as the hantavirus and dengue virus can cause pulmonary edema.
Risk factors for pulmonary edema
Heart failure and other heart conditions that raise pressure in your heart increase the risk of pulmonary edema. Risk factors for heart failure include:
- Irregular heart rhythms (arrhythmias)
- Alcohol use
- Congenital heart disease
- Coronary artery disease
- Diabetes
- Heart valve disease
- High blood pressure
- Sleep apnea
Some nervous system conditions and lung damage due to near drowning, drug use, inhaling smoke, viral illnesses and blood clots also raise your risk of developing pulmonary edema.
People who travel to high-altitude locations above 8,200 feet (about 2,500 meters) are more likely to develop high-altitude pulmonary edema (HAPE). It usually affects those who don’t take the time — a few days to a week or more — to get used to the elevation 44, 45, 46, 47. It occurs when the body has not had time to adjust to less oxygen — being young or physically fit does not decrease the risk. Children who already have pulmonary hypertension and structural heart defects may be more likely to get HAPE.
Whether or not you get high-altitude pulmonary edema (HAPE) could depend on:
- your height above sea level
- the time you took to make the ascent
- whether or not you have any problems affecting your heart and lungs
High altitudes can be very dangerous for people who have:
- Sickle cell anemia
- Chronic obstructive pulmonary disease (COPD)
- Severe emphysema
- Severe heart disease
Pulmonary edema pathophysiology
The causes of pulmonary edema can be broken down into two groups: cardiogenic (heart-related) or noncardiogenic (not heart-related). The resultant pathology of increased extravascular fluid content in the lung remains common to all forms of pulmonary edema. However, the underlying mechanism leading to the pulmonary edema arises from the disruption of various complex physiologic processes, maintaining a delicate balance of filtration of fluid and solute across the pulmonary capillary membrane. This imbalance can be from one or more of the following factors 9:
- Increase in intravascular hydrostatic pressure transmitted in a retrograde fashion to the pulmonary microvasculature
- Increase in interstitial hydrostatic pressure
- Endothelial injury and disruption of epithelial barriers
- Decrease in oncotic pressure due to underlying hepatic, renal, malnutrition, and other protein-losing states.
- Lymphatic insufficiency
- Increased negative interstitial pressure
The underlying pathology is at the microvascular level due to the increase in pulmonary vascular pressure. In addition to this, the capillaries also become leaky, causing the formation of edema. The imbalance between the hydrostatic and oncotic forces and the enhanced permeability of the pulmonary capillaries results in pulmonary edema 40. The rate of fluid filtration is determined by the differences in the hydrostatic and oncotic pressures between the pulmonary capillaries and interstitial space 48, 6, 49. The capillaries become permeable due to underlying causes such as sepsis, pancreatitis, etc. The relationship between hydrostatic and oncotic forces in relation to net fluid filtration is best explained by Ernest Starling’s equation 9.
The Starling’s equation:
- Q = K(Pcap – Pis) – l(Pcap – Pis)
where Q is net fluid filtration; K is a constant called the filtration coefficient; Pcap is capillary hydrostatic pressure, which tends to force fluid out of the capillary; Pis is hydrostatic pressure in the interstitial fluid, which tends to force fluid into the capillary; l is the reflection coefficient, which indicates the effectiveness of the capillary wall in preventing protein filtration; the second Pcap is the colloid osmotic pressure of plasma, which tends to pull fluid into the capillary; and the second Pis is the colloid osmotic pressure in the interstitial fluid, which pulls fluid out of the capillary. The net filtration of fluid may increase with changes in different parameters of the Starling equation.
Cardiogenic pulmonary edema pathophysiology
Cardiogenic pulmonary edema is defined as pulmonary edema due to increased capillary hydrostatic pressure secondary to elevated pulmonary venous pressure. Cardiogenic pulmonary edema reflects the accumulation of fluid with a low-protein content in the lung interstitium and alveoli as a result of cardiac dysfunction 50.
Pulmonary edema can be caused by the following major pathophysiologic mechanisms:
- Imbalance of Starling forces – ie, increased pulmonary capillary pressure, decreased plasma oncotic pressure, increased negative interstitial pressure
- Damage to the alveolar-capillary barrier
- Lymphatic obstruction
- Idiopathic (unknown) mechanism
Increased hydrostatic pressure leading to pulmonary edema may result from many causes, including excessive intravascular volume administration, pulmonary venous outflow obstruction (eg, mitral stenosis or left atrial myxoma), and left ventricular failure secondary to systolic or diastolic dysfunction of the left ventricle. Cardiogenic pulmonary edema leads to progressive deterioration of alveolar gas exchange and respiratory failure. Without prompt recognition and treatment, a patient’s condition can deteriorate rapidly.
The progression of fluid accumulation in cardiogenic pulmonary edema can be identified as three distinct physiologic stages.
- Stage 1. In stage 1, elevated LA pressure causes distention and opening of small pulmonary vessels. At this stage, blood gas exchange does not deteriorate, or it may even be slightly improved.
- Stage 2. In stage 2, fluid and colloid shift into the lung interstitium from the pulmonary capillaries, but an initial increase in lymphatic outflow efficiently removes the fluid. The continuing filtration of liquid and solutes may overpower the drainage capacity of the lymphatics. In this case, the fluid initially collects in the relatively compliant interstitial compartment, which is generally the perivascular tissue of the large vessels, especially in the dependent zones. The accumulation of liquid in the interstitium may compromise the small airways, leading to mild hypoxemia. Hypoxemia at this stage is rarely of sufficient magnitude to stimulate tachypnea. Tachypnea at this stage is mainly the result of the stimulation of juxtapulmonary capillary (J-type) receptors, which are nonmyelinated nerve endings located near the alveoli. J-type receptors are involved in reflexes modulating respiration and heart rates.
- Stage 3. In stage 3, as fluid filtration continues to increase and the filling of loose interstitial space occurs, fluid accumulates in the relatively noncompliant interstitial space. The interstitial space can contain up to 500mL of fluid. With further accumulations, the fluid crosses the alveolar epithelium in to the alveoli, leading to alveolar flooding. At this stage, abnormalities in gas exchange are noticeable, vital capacity and other respiratory volumes are substantially reduced, and hypoxemia becomes more severe.
Neurogenic pulmonary edema pathophysiology
Neurogenic pulmonary edema pathophysiology is not completely understood 51, 52. Because the most common neurological events are associated with increased intracranial pressure, intracranial hypertension is considered a key etiologic factor.
Within the central nervous system (CNS), the sites responsible for the development of neurogenic pulmonary edema are not fully clarified 53.
The central nervous system (CNS) disturbance will cause a sympathetic overflow leading to a state of systemic vasoconstriction. This will cause pooling of the blood from the systemic circulation to the pulmonary circulation, hence eliciting an increase in the pulmonary capillary hydrostatic pressure. That change of pressure will mediate the leakage of intravascular fluid to both the alveoli and the pulmonary interstitial space through 2 mechanisms: (1) change of pressure across the alveolar bed dictated by Starling forces, (2) the changes in permeability on the capillary walls.
For a more comprehensive understanding of the pathophysiology of the neurogenic pulmonary edema (NPE), it is important to understand 3 different sectors 52.
- Central Nervous System
- Structural: The injured central nervous system (CNS) will initiate a state of sympathetic overflow. Specific centers in the CNS (if stimulated) manage autonomic sympathetic system activation. Centers responsible for autonomic contribution to the pathogenesis of neurogenic pulmonary edema are located in specific areas of the central nervous system (CNS), called trigger zones for neurogenic pulmonary edema. These include rostral ventrolateral medulla, area postrema, nuclei of the solitary tract, nuclei of A1 and A5, and the medial reticulated nucleus, and the dorsal motor vagus nucleus.
- Chemical: The role of neurotransmitters is not clear in the pathogenesis of neurogenic pulmonary edema. Experimental studies relate NMDA receptors and GABA receptors activity in neurogenic pulmonary edema trigger zones to affect the sympathetic flow following central nervous system (CNS) insult.
- Physiological: Raised intracranial pressure (ICP) is a common encounter in central nervous system (CNS) injuries. The abrupt increase in intracranial pressure (ICP) will lead to the Cushing triad (increased blood pressure [BP], irregular breathing, and bradycardia). These physiological changes along with sympathetic overflow facilitate the development of pulmonary edema. Experimental studies on animals showed an increase in pulmonary artery pressure and extravascular pulmonary fluid in response to increased ICP.
- Autonomic Nervous System
- Sympathetic overflow: The sympathetic system is the key player in the pathogenesis of neurogenic pulmonary edema. The sudden over-activation of the neurogenic pulmonary edema trigger zones (either due to direct injury/irritation, activation of ascending neural pathways or as a response to the raised ICP) prompts sympathetic overflow and an outburst of catecholamines initiating 3 important pathophysiological responses; systemic vasoconstriction, increased blood pressure, and increased venous return.
- Parasympathetic contribution: The 10th cranial nerve (CN X) vagus provides the parasympathetic supply to the lungs and heart. Although the effect of vagus nerve rule on the heart during CNS injury is fairly elicited, yet the correlation of vagus nerve with the development of neurogenic pulmonary edema is strongly debatable and lacks clear supporting evidence. It is worth to mention that the hypothetical rationalization of the correlation of the vagus nerve activity to neurogenic pulmonary edema pathogenesis is the question of whether bradycardia is an essential or accessory factor in the development of pulmonary edema.
- Cardiovascular and Pulmonary Systems
- Sympathetic overflow and catecholamines-surge result in an increase of systemic resistance, venous return, and BP. Knowing this, the proposed theory of the development of neurogenic pulmonary edema falls into one of three supposed explanation:
- Hemodynamic changes: Increased functional demand on the cardiac muscle due to the aforementioned outcomes of the sympathetic overflow will cause the movement of blood from the systemic highly resistant circulation to the less resistant pulmonary circulation, resulting in an increase in pulmonary capillary positive hydrostatic pressure leading the movement of fluid from the capillaries to the lung tissue and interstitial space.
- Neurogenic myocardial injury: Mainly dictated by the sudden catecholamine surge. The increase in systemic BP and venous return will cause an overload on the heart. As the left ventricle fails to meet that loading change functionally, accumulation of blood in the ventricle occurs, causing cardiac damage, hence diastolic dysfunction. This will lead to pulmonary vascular congestion, hereafter pulmonary edema.
- Increased pulmonary capillary permeability is governed by 2 possible causes:
- Direct (humoral): Damage to the pulmonary capillaries endothelium in direct response to the catecholamines regardless of hemodynamic changes 54, 55, 56, 57
- Indirect (physical): Damage to the capillary bed as a mechanical response to the abrupt rise in the pulmonary capillary hydrostatic pressure 58, 59, 60
- Sympathetic overflow and catecholamines-surge result in an increase of systemic resistance, venous return, and BP. Knowing this, the proposed theory of the development of neurogenic pulmonary edema falls into one of three supposed explanation:
Pulmonary edema prevention
You may be able to prevent pulmonary edema by managing existing heart or lung conditions and following a healthy lifestyle. For example, controlling cholesterol and blood pressure can help lower your risk of heart disease. Follow these tips to keep your heart healthy:
- Eat a healthy diet rich in fresh fruits, vegetables, whole grains, fat-free or low-fat dairy, and a variety of proteins. Limit saturated fats and trans fats, added sugars, and sodium.
- Don’t smoke. It’s always a healthy idea to stop smoking. For help with quitting, talk to a health care provider.
- Get regular exercise. Healthy adults should get at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity a week, or a combination of the two. If you’re not used to exercise, start out slowly and build up gradually. Be sure to get your care provider’s OK before starting an exercise program.
- Limit salt and alcohol. Salt helps the body retain fluid. In some people with damage in the left ventricle of the heart, too much salt might trigger congestive heart failure. A dietician can help with cutting salt by showing how to determine the salt content in foods and create a nutritious, good-tasting diet. In general, most people should consume less than 2,300 milligrams a day of salt (sodium). Ask your doctor what level is safe for you.
- Manage stress.
- Manage weight. Being even slightly overweight increases the risk of cardiovascular disease. But losing even small amounts of weight can lower blood pressure and cholesterol and reduce the risk of diabetes.
- Keep blood pressure under control. For high blood pressure, take medications as prescribed and check blood pressure regularly. Record the results. A health care provider can help set a target blood pressure.
- Manage other medical conditions. Address underlying medical conditions. For example, controlling glucose levels if you have diabetes.
- Avoid the cause of your condition. If pulmonary edema results from drug use or high altitudes, for example, avoiding using drugs or being in high altitudes can help prevent more lung damage.
High-altitude pulmonary edema (HAPE) prevention
There are 3 important things you can do to prevent high-altitude illness 61.
- To prevent high-altitude pulmonary edema (HAPE), take your time traveling to higher altitudes. It takes several days for your body to fully adjust to lower amounts of oxygen at high altitudes. This is true even for people who are healthy. Most people can safely go from sea level to an altitude of 8,000 feet in a few days. Once you reach 8,200 feet (about 2,500 meters), you shouldn’t go up more than 1,000 to 2,000 feet (about 300 to 360 meters) per day. The higher you get, the longer it takes your body to adjust. Plan your trip so your body has time to get used to the high altitude before you start your physical activity.
- Sleep at a low altitude, if possible. For example, if you ski at 10,000 feet (3048 meters) during the day, sleep at a lower elevation at night. This lets your body rest and recover while you sleep.
- Hydrate before, during, and after you travel. Dehydration can increase your risk of high-altitude illness. You should drink extra water several days before and after you travel. Make sure you pack enough water while you’re active. Avoid or limit the amount of alcohol you consume.
- Some climbers take prescription medications such as acetazolamide or nifedipine (Procardia) to help prevent symptoms of HAPE. To prevent HAPE, start taking the medication at least one day before ascent. Ask your health care provider how long you need to take the medication after you’ve arrived at your high-altitude destination.
Pulmonary edema signs and symptoms
Pulmonary edema symptoms may appear suddenly or develop over time. Symptoms depend on the type of pulmonary edema.
Sudden (acute) pulmonary edema symptoms
Sudden (acute) pulmonary edema symptoms may include:
- Difficulty breathing (dyspnea) or extreme shortness of breath that worsens with activity or when lying down
- A feeling of suffocating or drowning that worsens when lying down
- A cough that produces frothy sputum that may have blood in it
- A rapid, irregular heartbeat (palpitations)
- Anxiety, restlessness or a feeling that something bad is about to happen
- Cold, clammy skin
- Wheezing or gasping for breath
Long-term (chronic) pulmonary edema signs and symptoms
Long-term (chronic) pulmonary edema signs and symptoms may include:
- Awakening at night with a cough or breathless feeling that may be relieved by sitting up
- Difficulty breathing with activity or when lying flat
- Fatigue
- More shortness of breath than usual when you’re physically active
- New or worsening cough
- Rapid weight gain
- Swelling in the legs and feet
- Wheezing
High-altitude pulmonary edema (HAPE) signs and symptoms
High-altitude pulmonary edema (HAPE) can occur in adults and children who travel to or exercise at high altitudes. Altitude sickness is caused by low oxygen levels in the air at altitudes above about 2,500 meters (8,200 ft) 61, 45, 46. Symptoms are similar to those that occur with acute pulmonary edema and can include:
- Headache, which may be the first symptom
- Shortness of breath with activity, which becomes shortness of breath at rest
- Not being able to exercise as much as you once could
- Dry cough, at first
- Later, a cough that produces frothy sputum that may look pink or have blood in it
- A very fast heartbeat (tachycardia)
- Weakness
- Chest pain
- Low fever
Symptoms of high-altitude pulmonary edema (HAPE) tend to get worse at night.
If you have these symptoms, go to a lower altitude right away until the symptoms disappear and get medical help. Symptoms that are ignored or left untreated can be life threatening. Breathing oxygen from a tank can help. Do not continue to climb higher.
It is best not to drink alcohol or take sedatives or sleeping pills because they interfere with the body’s adaptation to high altitude.
Pulmonary edema complications
Complications of pulmonary edema depend on the cause. In general, if pulmonary edema continues, the pressure in the pulmonary artery can rise (pulmonary hypertension). Eventually, the heart becomes weak and begins to fail, and pressures in the heart and lungs go up.
Pulmonary edema complications may include:
- Breathing difficulty
- Swelling of the legs, feet and belly area
- Buildup of fluid in the membranes that surround the lungs (pleural effusion)
- Congestion and swelling of the liver
Immediate treatment is necessary for acute pulmonary edema to prevent death.
Pulmonary edema diagnosis
People who have breathing problems should see a doctor. Be sure to tell him or her about the conditions you were in when you had the symptoms. Your doctor will do a physical exam to see if you have fluid in your lungs. Your doctor listen to your heart and lungs with a stethoscope. Your doctor be examining you for:
- Increased or decreased heart rate or blood pressure.
- Increased respiratory rate.
- Abnormal heart sounds.
- Crackling sounds or wheezing/whistling sounds in your lungs.
- Swelling of your body.
- Gray or bluish skin.
Based on the severity of your symptoms, he or she may order tests. Tests may include a chest X-ray, brain scan, or electrocardiogram (ECG). These help diagnose the type of illness and decide on a treatment plan.
Tests that can help diagnose pulmonary edema or determine the reason for fluid in your lungs include:
- Chest X-ray. A chest X-ray can confirm the diagnosis of pulmonary edema and exclude other possible causes of shortness of breath. It’s usually the first test done when a health care provider suspects pulmonary edema.
- Chest computerized tomography (CT) scan. A chest computed tomography (CT) scan gives more details about the condition of the lungs. It can help a provider diagnose or rule out pulmonary edema.
- Pulse oximetry. A sensor is attached to a finger or ear. It uses light to determine how much oxygen is in the blood.
- Arterial blood gas test. This test measures the amount of oxygen and carbon dioxide in the blood.
- Brain-type natriuretic peptide (BNP) blood test. Increased levels of B-type natriuretic peptide (BNP) may signal a heart condition. Brain-type natriuretic peptide (BNP) is secreted by the heart muscle cells (cardiac myocytes) of the left ventricles in response to stretching caused by increased ventricular blood volume or increased intracardiac pressures. Elevated BNP levels correlate with left ventricular end-diastolic pressure as well as pulmonary occlusion pressure and can be seen in patients with congestive heart failure 6. BNP levels less than 100 pg/ml suggest heart failure is less likely, and levels greater than 500 pg/ml suggest a high likelihood of heart failure. Levels between 100 and 500 pg/ml do not help in the diagnosis of heart failure and are often seen in critically ill patients 6.
- Troponin elevation is commonly noted in patients with damage to heart muscle cells (cardiac myocytes), such as acute coronary syndrome. They, however, are also noted to be elevated in patients with severe sepsis 6.
- Other blood tests. Blood tests to diagnose pulmonary edema and its causes also usually include a complete blood count, metabolic panel to check kidney function and thyroid function test.
- Hypoalbuminemia (≤3.4 g/dL) is an independent marker of increased in-hospital and post-discharge mortality for patients presenting in acute decompensated heart failure 62. Low albumin in isolation does not lead to pulmonary edema as there is a concurrent drop in pulmonary interstitial and plasma albumin levels preventing the creation of a transpulmonary oncotic pressure gradient 63.
- Obtaining serum electrolyte levels, including renal function, serum osmolarity, toxicology screening, help in patients with pulmonary edema due to toxic ingestion. Obtaining lipase and amylase levels help diagnose acute pancreatitis.
- Electrocardiogram (ECG or EKG). This painless test detects and records the timing and strength of the heart’s signals. It uses small sensors (electrodes) attached to the chest and sometimes to the arms or legs. Wires attach the sensors to a machine, which displays or prints results. An electrocardiogram (ECG) can show signs of heart wall thickening or previous heart attack. A portable device such as a Holter monitor may be used to continuously monitor the heartbeat at home.
- Echocardiogram. An echocardiogram uses sound waves (ultrasound) to create pictures of the beating heart. It can identify areas of poor blood flow, heart valve issues and heart muscle that is not working properly. An echocardiogram can help diagnose fluid around the heart (pericardial effusion).
- Cardiac catheterization and coronary angiogram. This test may be done if other tests don’t show the cause of pulmonary edema, or when there’s also chest pain. It helps health care providers see blockages in the heart arteries. A long, flexible tube (catheter) is inserted in a blood vessel, usually in the groin or wrist. It’s guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video.
- Ultrasound of the lungs. This painless test uses sound waves to measure blood flow through the lungs. It can quickly reveal signs of fluid buildup and plural effusions.
Plain radiograph
The chest radiograph (chest X-ray) remains the most practical and useful method of radiologically assessing and quantifying pulmonary edema 64, 65.
A mnemonic to remember the radiographic signs of pulmonary edema is ABCDE 66:
- A: alveolar opacification
- B: batwinging
- C: cardiomegaly
- D: diffuse interstitial thickening (septal lines) and diversion (vascular upper zone diversion, cephalisation)
- E: effusions (pleural)
Features useful for broadly assessing pulmonary edema on a plain chest radiograph include 67:
- upper lobe pulmonary venous diversion (stag’s antler sign)
- increased cardiothoracic ratio/cardiac silhouette size: useful for assessing for an underlying cardiogenic cause or association
- features of pulmonary interstitial edema:
- peribronchial cuffing and perihilar haze
- septal (Kerley) lines
- thickening of interlobar fissures
- features of pulmonary alveolar edema:
- air space opacification classically in a batwing distribution
- may have air bronchograms
- pleural effusions and fluid in interlobar fissures (including ‘vanishing’ pulmonary pseudotumor)
There is a general progression of signs on a plain radiograph that occurs as the pulmonary capillary wedge pressure (PCWP) increases (see pulmonary edema grading below). Whether all or only some of these features can be appreciated on the plain chest radiograph, depend on the specific cause 1. Pulmonary edema is usually a bilateral process, but it may uncommonly appear to be unilateral in certain situations and pathologies (unilateral pulmonary edema).
One pulmonary edema grading based on chest radiograph appearances and pulmonary capillary wedge pressure (PCWP) is as follows 68:
- Grade 0: normal chest radiograph, pulmonary capillary wedge pressure (PCWP) 8-12 mmHg
- Grade 1: shows evidence of upper lobe diversion on a chest radiograph, pulmonary capillary wedge pressure (PCWP) 13-18 mmHg
- Grade 2: shows interstitial edema on a chest radiograph, pulmonary capillary wedge pressure (PCWP) 19-25 mmHg
- Grade 3: shows alveolar edema on a chest radiograph, pulmonary capillary wedge pressure (PCWP) greater than 25 mmHg
Pulmonary edema CT
Interstitial pulmonary edema is most commonly demonstrated by the following CT signs 69:
- ground glass opacification
- bronchovascular bundle thickening (due to increased vascular diameter and/or peribronchovascular thickening)
- interlobular septal thickening
Alveolar edema is demonstrated by airspace consolidation in addition to the above findings.
Pleural effusions are a frequent accompanying finding in cardiogenic/hydrostatic pulmonary edema.
Pulmonary edema ultrasound
Pulmonary edema ultrasound is a newer technique that is non-invasive and does not involve radiation exposure. It is most commonly used in intensive care units, emergency rooms, and operating rooms. It helps detect the accumulation of extravascular lung water (EVLW) ahead of the clinical manifestations 70.
The appearance of pulmonary edema is defined as a function of the perturbation of the air-fluid level in the lung, a spectrum of appearances coined the alveolar-interstitial syndromes.
As subpleural interlobular septa thicken among air-filled alveoli, they create a medium in which incident ultrasound waves will reverberate within, creating a short path reverberation artifact. Referred to as B-lines, these are pathological when more than three appear, garnering the title lung rockets, and consistent with thickened interlobular septa. When spaced 7 mm apart they correlate with radiographic interstitial edema and when 3 mm apart with ground glass opacification. When surrounding alveoli become fluid-filled, the resultant interface assumes a tissue-like pattern. The tissue-like sign and shred sign are pathognomonic 71.
Pulmonary artery catheterization
Often considered a gold standard in the determination of the cause of pulmonary edema, it is an invasive test that helps monitor systemic vascular resistance, cardiac output, and filling pressures. This test may be done if other tests don’t show the cause of pulmonary edema, or when there’s also chest pain. It helps health care providers see blockages in the heart arteries. A long, flexible tube (catheter) is inserted in a blood vessel, usually in the groin or wrist. It’s guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video. An elevated pulmonary artery occlusion pressure over 18 mm Hg is helpful in the determination of cardiogenic pulmonary edema 6.
Transpulmonary thermodilution
It is an invasive testing modality performed in patients typically undergoing major cardiac, vascular, or thoracic surgeries. They are also used in septic shock and monitors several hemodynamic indices such as cardiac index, mixed venous oxygen saturation, stroke volume index, and extravascular lung water (EVLW) 70.
Pulmonary edema treatment
The first treatment for acute pulmonary edema is oxygen. Oxygen flows through a face mask or a flexible plastic tube with two openings (nasal cannula) that deliver oxygen to each nostril. This should ease some symptoms. A health care provider will monitor your the oxygen level. Sometimes it may be necessary to assist your breathing with a machine such as a mechanical ventilator or one that provides positive airway pressure 11, 9.
Depending on the severity of the condition and the reason for the pulmonary edema, treatment might include one or more of the following medications:
- Diuretics (water pills). Diuretics, such as furosemide (Lasix), decrease the pressure caused by excess fluid in the heart and lungs. Diuretics remain the mainstay of treatment, and furosemide (Lasix) being the most commonly used medication. Higher doses are associated with more improvement in dyspnea; however, also associated with transient worsening of kidney function 72.
- Blood pressure drugs. These help manage high or low blood pressure, which can occur with pulmonary edema. A doctor may also prescribe medications that lower the pressure going into or out of your heart. Examples of such medicines are nitroglycerin (Nitromist, Nitrostat, others) and nitroprusside (Nitropress). IV nitroglycerin (NTG) is the drug of choice, and it lowers preload and pulmonary congestion. Nitroglycerin should only be used when the systolic blood pressure (SBP) is > 110 mm Hg. Nesiritide is a recombinant brain natriuretic peptide (BNP) that has vasodilatory properties. It has been shown to reduce pulmonary capillary wedge pressure (PCWP) and filling pressures significantly, but no subsequent improvement in dyspnea has been noted 73. Newer drugs like serelaxin, a recombinant human form of relaxin, induced nitric oxide activation, which causes vasodilation. Clevidipine is an ultra-short-acting calcium channel blocker, initiated very early in the presentation, has been associated with reduced length of stay, improved dyspnea, and less frequent ICU admission 74.
- Inotropes. Inotropes such as dobutamine and dopamine improve heart pumping function and maintain blood pressure. This type of medication is given through an IV for people in the hospital with severe heart failure. Significant adverse events include tachyarrhythmias, ischemia, and hypotension. Milrinone is an IV inotrope with vasodilatory properties but is associated with an increase in post-discharge mortality 75.
- Morphine (MS Contin, Infumorph, others). Morphine reduces systemic vascular resistance and acts as an analgesic and anxiolytic. It has been used in the management of pulmonary edema secondary to acute coronary syndrome. This narcotic may be taken by mouth or given through an IV to relieve shortness of breath and anxiety. However, it may cause respiratory depression needing intubation, and generally not recommended 72. Some doctors believe that the risks of morphine may outweigh the benefits. They’re more likely to use other drugs.
- Other medications, when congestive heart failure isn’t the cause of your pulmonary edema, such as antibiotics and steroids.
It is important to diagnose and treat, if possible, any nervous system problems or causes of heart failure. Treatment of neurogenic pulmonary edema (NPE) centers on resolution of central nervous system (CNS) injury and ventilation support 76. Specific treatments have been proposed like endothelin converting enzyme inhibitors or sympathectomy which has been successfully tested in rats 77, 78; however, the evidence is insufficient for its use as a human treatment 79, and seizure control is essential as the only preventable treatment.
High-altitude pulmonary edema (HAPE) treatment
It’s important to treat high-altitude pulmonary edema (HAPE) as soon as symptoms begin. Oxygen is the usually the first treatment. If oxygen isn’t available, a portable hyperbaric chamber can imitate going down to a lower elevation until it’s possible to move to a lower altitude.
Treatments for high-altitude pulmonary edema (HAPE) also include:
- Immediately going down to a lower altitude. For someone in high altitudes who has mild symptoms of high-altitude pulmonary edema (HAPE), going down 1,000 to 3,000 feet (about 300 to 1,000 meters) as quickly as possible can help. Someone with severe HAPE might need rescue assistance to get off the mountain.
- Stopping exercise, drinking water and staying warm. Physical activity and cold can make pulmonary edema worse.
- Medication. Some climbers take prescription medications such as acetazolamide or nifedipine (Procardia) to help treat or prevent symptoms of HAPE. To prevent HAPE, they start taking the medication at least a day before going higher. Nifedipine (calcium channel blocker) counteracts the hypoxia-mediated vasoconstriction of the pulmonary vasculature. This leads to the lowering of the pulmonary arterial pressure with subsequent improvements in gas exchange, exercise capability, and chest radiography 80. Nifedipine is only used as a prophylactic strategy when altitude acclimatization cannot be achieved in high-risk individuals and situations, including a rapid rate of ascent, extreme physical exertion, recent respiratory tract infection, and low altitude of native place of residence 81.
If your symptoms are severe, continue to go down to a lower altitude until you’re no longer sick. If your symptoms don’t improve or get worse, call a doctor or go to the nearest hospital. You will need medical treatment.
Don’t ignore signs of high-altitude illness. Symptoms that are ignored or left untreated can be life threatening. Don’t go higher until you feel better and your symptoms have gone away completely. Once your body adjusts, it should eventually get used to the low oxygen level. Over time, you shouldn’t get sick anymore. This is helpful for people who move to a higher altitude to live.
Neurogenic pulmonary edema treatment
Neurogenic pulmonary edema treatment consists of two interventions: treating the underlying neurological injury to reduce intracranial pressure (ICP) to control sympathetic hyperactivity related to the lung injury, and supportive treatment for pulmonary edema 82, 83, 84, 85, 86. Within the supportive treatment of pulmonary impairment, monitoring of body fluids is difficult because maintaining adequate fluid volume is required for cerebral resuscitation, but the approach to neurogenic pulmonary edema (NPE) requires fluid restriction 82, 83, 84, 85. In this context, real-time lung ultrasound allows an assessment of respiratory failure, quantification and monitoring of pulmonary interstitial fluid, contributing to the management of liquid therapy 87. Another viable intervention is the transpulmonary thermodilution technique, which consists of administering a saline solution at low temperature through a central venous catheter, then measuring the change in blood temperature and using this to construct a thermodilution curve that allows the calculation of hemodynamic parameters such as cardiac output and the pulmonary extravascular water index 88.
Supportive care involves adequate ventilation to provide sufficient oxygenation to prevent hypoxia and hypercapnia 83, 84, 85, 86. Therefore, the invasive or noninvasive ventilation technique must be individualized according to the severity of the patient’s cardio-pulmonary and neurological affectation 82, 83. Since patients present a life-threatening condition, it is important to be strict in the non-invasive monitoring of blood pressure, pulse oximetry, electrocardiography, echocardiography, radiography, among others 85, 86. Extracorporeal membrane oxygenation can be used in patients with acute respiratory failure in whom mechanical ventilation and other therapies do not provide adequate gas exchange 89.
The usefulness of pharmacotherapy is varied, although no drug has been officially approved for routine use 82, 84, 86. Hemodynamic instability with consequent organ hypoperfusion, metabolic acidosis, and progression of inflammation can be managed with vasoactive drugs 90, 91, 92. Milrinone is used to increase cardiac output and is recommended when systolic blood pressure is > 90 mmHg. Dobutamine is preferred in those patients with blood pressure < 90 mmHg to increase cardiac output 90, 91, 92. Other drugs that could be used according to the patient’s context include diuretics such as furosemide, osmotic diuretics, and alpha-adrenergic blockers 93, 94.
Swimming-induced pulmonary edema treatment
Treatment for patients with swimming-induced pulmonary edema consists primarily of supportive measures such as removing the patient from the wet and/or cold environment and providing supplemental oxygen 95. Diuretics are typically not necessary because patients tend to show relief of symptoms soon after being placed on supplemental oxygen 96.
Pulmonary edema survival rate
Pulmonary edema survival rates depend on the cause of the pulmonary edema and how quickly you receive treatment. If you have acute (sudden) pulmonary edema, you need immediate treatment. Severe acute respiratory distress syndrome (ARDS) carries a 40% mortality rate. Hospital mortality has decreased from 60% from 1967 through 1981 to the range of 30% to 40% in the 1990s 97, 98. In-hospital mortality rates for patients with cardiogenic pulmonary edema are difficult to assign because the causes and severity of the disease vary considerably. In a high-acuity setting, in-hospital death rates are as high as 15-20% 99. Heart attack (myocardial infarction) associated hypotension, and a history of frequent hospitalizations for cardiogenic pulmonary edema generally increase the mortality risk.
High-altitude pulmonary edema (HAPE) recurs in 60% of patients who ascend above 4500 meters and have a previous diagnosis of HAPE 100. Prognosis is poor in neurogenic pulmonary edema (NPE) as this condition is associated with an insult to the central nervous system (CNS) with the mortality rate of 60% to 100% 101, 76, 102. Neurogenic pulmonary edema may complicate subarachnoid and intracerebral hemorrhage in 30 to 70% of patients and may recur after initial resolution 103, 84. However, there are no statistics concerning neurogenic pulmonary edema (NPE) in the context of other neurologic conditions such as epilepsy 76. Ischemia-reperfusion injury or reperfusion pulmonary edema (also known as reimplantation response) accounts for 25% of the mortality after lung transplantation 104, 105. Mortality from transfusion-related lung injury (TRALI) is 5 to 10%; however, it can reach 47% in critically ill patients 106.
References- Gluecker T, Capasso P, Schnyder P, Gudinchet F, Schaller MD, Revelly JP, Chiolero R, Vock P, Wicky S. Clinical and radiologic features of pulmonary edema. Radiographics. 1999 Nov-Dec;19(6):1507-31; discussion 1532-3. doi: 10.1148/radiographics.19.6.g99no211507
- Acute pulmonary edema. https://radiopaedia.org/cases/3011/play?lang=us
- Unilateral pulmonary edema from acute mitral regurgitation. https://radiopaedia.org/cases/49315/play?lang=us
- Pulmonary edema. https://radiopaedia.org/cases/99924/play?lang=us
- Ghofrani HA. Lungenödem [Pulmonary edema]. Internist (Berl). 2004 May;45(5):565-72. German. doi: 10.1007/s00108-004-1175-x
- Ware LB, Matthay MA. Clinical practice. Acute pulmonary edema. N Engl J Med. 2005 Dec 29;353(26):2788-96. doi: 10.1056/NEJMcp052699
- Go AS, Mozaffarian D, Roger VL, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation. 2013 Jan 1;127(1):e6-e245. doi: 10.1161/CIR.0b013e31828124ad. Epub 2012 Dec 12. Erratum in: Circulation. 2013 Jan 1;127(1):doi:10.1161/CIR.0b013e31828124ad. Erratum in: Circulation. 2013 Jun 11;127(23):e841.
- Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD. Incidence and outcomes of acute lung injury. N Engl J Med. 2005 Oct 20;353(16):1685-93. doi: 10.1056/NEJMoa050333
- Malek R, Soufi S. Pulmonary Edema. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557611
- Pulmonary edema. https://www.mayoclinic.org/diseases-conditions/pulmonary-edema/symptoms-causes/syc-20377009
- Clark SB, Soos MP. Noncardiogenic Pulmonary Edema. [Updated 2022 Oct 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542230
- Wilmshurst PT, Nuri M, Crowther A, Webb-Peploe MM. Cold-induced pulmonary oedema in scuba divers and swimmers and subsequent development of hypertension. Lancet. 1989 Jan 14;1(8629):62-5. doi: 10.1016/s0140-6736(89)91426-8
- Shupak A, Weiler-Ravell D, Adir Y, Daskalovic YI, Ramon Y, Kerem D. Pulmonary oedema induced by strenuous swimming: a field study. Respir Physiol. 2000 Jun;121(1):25-31. doi: 10.1016/s0034-5687(00)00109-2
- Wilmshurst P., Nuri M., Crowther A., Betts J., Webb-Peploe N. Forearm vascular responses in subjects who develop recurrent pulmonary oedema when scuba diving: a new syndrome. Br Heart J. 1981;45(A349):439.
- Hageman SM, Chakraborty RK, Murphy-Lavoie HM. Immersion Pulmonary Edema. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499853
- Adir Y, Shupak A, Gil A, Peled N, Keynan Y, Domachevsky L, Weiler-Ravell D. Swimming-induced pulmonary edema: clinical presentation and serial lung function. Chest. 2004 Aug;126(2):394-9. doi: 10.1378/chest.126.2.394
- Peacher DF, Martina SD, Otteni CE, Wester TE, Potter JF, Moon RE. Immersion pulmonary edema and comorbidities: case series and updated review. Med Sci Sports Exerc. 2015 Jun;47(6):1128-34. doi: 10.1249/MSS.0000000000000524
- Bove AA. Pulmonary Aspects of Exercise and Sports. Methodist Debakey Cardiovasc J. 2016 Apr-Jun;12(2):93-7. doi: 10.14797/mdcj-12-2-93
- Hopkins SR, Schoene RB, Henderson WR, Spragg RG, Martin TR, West JB. Intense exercise impairs the integrity of the pulmonary blood-gas barrier in elite athletes. Am J Respir Crit Care Med. 1997 Mar;155(3):1090-4. doi: 10.1164/ajrccm.155.3.9116992
- MacIver DH, Clark AL. The vital role of the right ventricle in the pathogenesis of acute pulmonary edema. Am J Cardiol. 2015 Apr 1;115(7):992-1000. doi: 10.1016/j.amjcard.2015.01.026
- Pendergast DR, Moon RE, Krasney JJ, Held HE, Zamparo P. Human Physiology in an Aquatic Environment. Compr Physiol. 2015 Sep 20;5(4):1705-50. doi: 10.1002/cphy.c140018
- Kumar M, Thompson PD. A literature review of immersion pulmonary edema. Phys Sportsmed. 2019 May;47(2):148-151. doi: 10.1080/00913847.2018.1546104
- Castagna O, de Maistre S, Schmid B, Caudal D, Regnard J. Immersion pulmonary oedema in a healthy diver not exposed to cold or strenuous exercise. Diving Hyperb Med. 2018 Mar 31;48(1):40-44. doi: 10.28920/dhm48.1.40-44
- Grünig H, Nikolaidis PT, Moon RE, Knechtle B. Diagnosis of Swimming Induced Pulmonary Edema-A Review. Front Physiol. 2017 Aug 31;8:652. doi: 10.3389/fphys.2017.00652
- Shearer D, Mahon RT. Brain natriuretic peptide levels in six basic underwater demolitions/SEAL recruits presenting with swimming induced pulmonary edema (SIPE). J Spec Oper Med. 2009 Summer;9(3):44-50. doi: 10.55460/MPGH-O4NQ
- Weiler-Ravell D, Shupak A, Goldenberg I, Halpern P, Shoshani O, Hirschhorn G, Margulis A. Pulmonary oedema and haemoptysis induced by strenuous swimming. BMJ. 1995 Aug 5;311(7001):361-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2550430/pdf/bmj00604-0025.pdf
- Smith R, Ormerod JOM, Sabharwal N, Kipps C. Swimming-induced pulmonary edema: current perspectives. Open Access J Sports Med. 2018 Jul 27;9:131-137. doi: 10.2147/OAJSM.S140028
- Ruggeri P, Glossop A, Esquinas AM. Prehospital Management of Swimming-Induced Pulmonary Edema: Is CPAP the Best Lifeguard? Chest. 2022 Aug;162(2):e108-e109. doi: 10.1016/j.chest.2022.03.048
- Borza ML, Blonien NE. Swimming-Induced Pulmonary Edema found in a U.S. Navy Basic Underwater Demolition/SEAL Recruit. Cureus. 2022 Sep 21;14(9):e29417. doi: 10.7759/cureus.29417
- Edmonds C. The evolution of scuba divers pulmonary edema. Undersea Hyperb Med. 2016 Mar-Apr;43(2):83-91.
- Moon RE, Martina SD, Peacher DF, Kraus WE. Deaths in triathletes: immersion pulmonary oedema as a possible cause. BMJ Open Sport Exerc Med. 2016 Aug 29;2(1):e000146. doi: 10.1136/bmjsem-2016-000146
- Baumann A, Audibert G, McDonnell J, Mertes PM. Neurogenic pulmonary edema. Acta Anaesthesiol Scand. 2007 Apr;51(4):447-55. doi: 10.1111/j.1399-6576.2007.01276.x
- Guo L, Yang X, Yang B, Tang G, Li C. Prevalence, in-hospital mortality, and factors related to neurogenic pulmonary edema after spontaneous subarachnoid hemorrhage: a systematic review and meta-analysis. Neurosurg Rev. 2023 Jul 11;46(1):169. doi: 10.1007/s10143-023-02081-6
- Fontes RB, Aguiar PH, Zanetti MV, Andrade F, Mandel M, Teixeira MJ. Acute neurogenic pulmonary edema: case reports and literature review. J Neurosurg Anesthesiol. 2003 Apr;15(2):144-50. doi: 10.1097/00008506-200304000-00013
- Lee VH, Oh JK, Mulvagh SL, Wijdicks EF. Mechanisms in neurogenic stress cardiomyopathy after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2006;5(3):243-9. doi: 10.1385/NCC:5:3:243
- Wartenberg KE, Mayer SA. Medical complications after subarachnoid hemorrhage: new strategies for prevention and management. Curr Opin Crit Care. 2006 Apr;12(2):78-84. doi: 10.1097/01.ccx.0000216571.80944.65
- Sharma D. Perioperative Management of Aneurysmal Subarachnoid Hemorrhage. Anesthesiology. 2020 Dec 1;133(6):1283-1305. doi: 10.1097/ALN.0000000000003558. Erratum in: Anesthesiology. 2021 Apr 1;134(4):672.
- Gonçalves V, Silva-Carvalho L, Rocha I. Cerebellar haemorrhage as a cause of neurogenic pulmonary edema – case report. Cerebellum. 2005;4(4):246-9. doi: 10.1080/14734220500325863
- Qin SQ, Sun W, Wang HB, Zhang QL. Neurogenic pulmonary edema in head injuries: analysis of 5 cases. Chin J Traumatol. 2005 Jun;8(3):172-4, 178.
- Suhail Najim M, Ali Mohammed Hammamy R, Sasi S. Neurogenic Pulmonary Edema Following a Seizure: A Case Report and Literature Review. Case Rep Neurol Med. 2019 Oct 9;2019:6867042. doi: 10.1155/2019/6867042
- Reuter-Rice K, Duthie S, Hamrick J. Neurogenic pulmonary edema associated with pediatric status epilepticus. Pediatr Emerg Care. 2011 Oct;27(10):957-8. doi: 10.1097/PEC.0b013e3182309eac
- Simon R. P. Neurogenic pulmonary edema. Neurologic Clinics. 1993;11(2):309–323. doi: 10.1016/S0733-8619(18)30155-5
- Toy P, Lowell C. TRALI–definition, mechanisms, incidence and clinical relevance. Best Pract Res Clin Anaesthesiol. 2007 Jun;21(2):183-93. doi: 10.1016/j.bpa.2007.01.003
- Savioli G, Ceresa IF, Gori G, Fumoso F, Gri N, Floris V, Varesi A, Martuscelli E, Marchisio S, Longhitano Y, Ricevuti G, Esposito C, Caironi G, Giardini G, Zanza C. Pathophysiology and Therapy of High-Altitude Sickness: Practical Approach in Emergency and Critical Care. J Clin Med. 2022 Jul 6;11(14):3937. doi: 10.3390/jcm11143937
- Gudbjartsson T, Sigurdsson E, Gottfredsson M, Bjornsson OM, Gudmundsson G. [High altitude illness and related diseases – a review]. Laeknabladid. 2019 Nov;105(11):499-507. Icelandic. https://www.laeknabladid.is/tolublod/2019/11/nr/7173
- Fiore DC, Hall S, Shoja P. Altitude illness: risk factors, prevention, presentation, and treatment. Am Fam Physician. 2010 Nov 1;82(9):1103-10. https://www.aafp.org/pubs/afp/issues/2010/1101/p1103.html
- Hackett PH, Roach RC. High-altitude illness. N Engl J Med. 2001 Jul 12;345(2):107-14. doi: 10.1056/NEJM200107123450206
- Murray JF. Pulmonary edema: pathophysiology and diagnosis. Int J Tuberc Lung Dis. 2011 Feb;15(2):155-60, i. https://docserver.ingentaconnect.com/deliver/connect/iuatld/10273719/v15n2/s3.pdf
- Sibbald WJ, Anderson RR, Holliday RL. Pathogenesis of pulmonary edema associated with the adult respiratory distress syndrome. Can Med Assoc J. 1979 Feb 17;120(4):445-50. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1818907/pdf/canmedaj01440-0055.pdf
- Cardiogenic Pulmonary Edema. https://emedicine.medscape.com/article/157452-overview#showall
- Šedý J, Zicha J, Kunes J, Jendelová P, Syková E. Mechanisms of neurogenic pulmonary edema development. Physiol Res. 2008;57(4):499-506. doi: 10.33549/physiolres.931432
- Al-Dhahir MA, M Das J, Sharma S. Neurogenic Pulmonary Edema. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532984
- Neurogenic Pulmonary Edema. https://emedicine.medscape.com/article/300813-overview#a5
- Kerr NA, de Rivero Vaccari JP, Abbassi S, Kaur H, Zambrano R, Wu S, Dietrich WD, Keane RW. Traumatic Brain Injury-Induced Acute Lung Injury: Evidence for Activation and Inhibition of a Neural-Respiratory-Inflammasome Axis. J Neurotrauma. 2018 Sep 1;35(17):2067-2076. doi: 10.1089/neu.2017.5430
- Lou M, Chen X, Wang K, Xue Y, Cui D, Xue F. Increased intracranial pressure is associated with the development of acute lung injury following severe traumatic brain injury. Clin Neurol Neurosurg. 2013 Jul;115(7):904-8. doi: 10.1016/j.clineuro.2012.09.001
- Colice GL. Neurogenic pulmonary edema. Clin Chest Med. 1985 Sep;6(3):473-89.
- Simon RP. Neurogenic pulmonary edema. Neurol Clin. 1993 May;11(2):309-23.
- Ducker TB, Simmons RL. Increased intracranial pressure and pulmonary edema. 2. The hemodynamic response of dogs and monkeys to increased intracranial pressure. J Neurosurg. 1968 Feb;28(2):118-23. doi: 10.3171/jns.1968.28.2.0118
- Bahloul M, Chaari AN, Kallel H, Khabir A, Ayadi A, Charfeddine H, Hergafi L, Chaari AD, Chelly HE, Ben Hamida C, Rekik N, Bouaziz M. Neurogenic pulmonary edema due to traumatic brain injury: evidence of cardiac dysfunction. Am J Crit Care. 2006 Sep;15(5):462-70.
- Mayer SA, Lin J, Homma S, Solomon RA, Lennihan L, Sherman D, Fink ME, Beckford A, Klebanoff LM. Myocardial injury and left ventricular performance after subarachnoid hemorrhage. Stroke. 1999 Apr;30(4):780-6. doi: 10.1161/01.str.30.4.780
- Li Y, Zhang Y, Zhang Y. Research advances in pathogenesis and prophylactic measures of acute high altitude illness. Respir Med. 2018 Dec;145:145-152. https://doi.org/10.1016/j.rmed.2018.11.004
- Bonilla-Palomas JL, Gámez-López AL, Moreno-Conde M, López-Ibáñez MC, Anguita-Sánchez M, Gallego de la Sacristana A, García-Catalán F, Villar-Ráez A. Hypoalbuminemia in acute heart failure patients: causes and its impact on hospital and long-term mortality. J Card Fail. 2014 May;20(5):350-8. doi: 10.1016/j.cardfail.2014.01.016
- Taylor AE. Capillary fluid filtration. Starling forces and lymph flow. Circ Res. 1981 Sep;49(3):557-75. doi: 10.1161/01.res.49.3.557
- Milne EN, Pistolesi M, Miniati M, Giuntini C. The radiologic distinction of cardiogenic and noncardiogenic edema. AJR Am J Roentgenol. 1985 May;144(5):879-94. doi: 10.2214/ajr.144.5.879
- Pistolesi M, Miniati M, Milne EN, Giuntini C. The chest roentgenogram in pulmonary edema. Clin Chest Med. 1985 Sep;6(3):315-44.
- Pulmonary edema signs (mnemonic). https://radiopaedia.org/articles/pulmonary-edema-signs-mnemonic?lang=us
- Pulmonary edema. https://radiopaedia.org/articles/pulmonary-oedema?lang=us
- Pulmonary edema grading. https://radiopaedia.org/articles/pulmonary-oedema-grading?lang=us
- Komiya K, Ishii H, Murakami J, Yamamoto H, Okada F, Satoh K, Takahashi O, Tobino K, Ichikado K, Johkoh T, Kadota J. Comparison of chest computed tomography features in the acute phase of cardiogenic pulmonary edema and acute respiratory distress syndrome on arrival at the emergency department. J Thorac Imaging. 2013 Sep;28(5):322-8. doi: 10.1097/RTI.0b013e31828d40b2
- Assaad S, Kratzert WB, Shelley B, Friedman MB, Perrino A Jr. Assessment of Pulmonary Edema: Principles and Practice. J Cardiothorac Vasc Anesth. 2018 Apr;32(2):901-914. doi: 10.1053/j.jvca.2017.08.028
- Lichtenstein DA. BLUE-protocol and FALLS-protocol: two applications of lung ultrasound in the critically ill. Chest. 2015 Jun;147(6):1659-1670. doi: 10.1378/chest.14-1313
- Chioncel O, Collins SP, Ambrosy AP, Gheorghiade M, Filippatos G. Pulmonary Oedema-Therapeutic Targets. Card Fail Rev. 2015 Apr;1(1):38-45. doi: 10.15420/CFR.2015.01.01.38
- Publication Committee for the VMAC Investigators (Vasodilatation in the Management of Acute CHF). Intravenous nesiritide vs nitroglycerin for treatment of decompensated congestive heart failure: a randomized controlled trial. JAMA. 2002 Mar 27;287(12):1531-40. doi: 10.1001/jama.287.12.1531. Erratum in: JAMA 2002 Aug 7;288(5):577.
- Peacock WF, Chandra A, Char D, Collins S, Der Sahakian G, Ding L, Dunbar L, Fermann G, Fonarow GC, Garrison N, Hu MY, Jourdain P, Laribi S, Levy P, Möckel M, Mueller C, Ray P, Singer A, Ventura H, Weiss M, Mebazaa A. Clevidipine in acute heart failure: Results of the A Study of Blood Pressure Control in Acute Heart Failure-A Pilot Study (PRONTO). Am Heart J. 2014 Apr;167(4):529-36. doi: 10.1016/j.ahj.2013.12.023
- Cuffe MS, Califf RM, Adams KF Jr, Benza R, Bourge R, Colucci WS, Massie BM, O’Connor CM, Pina I, Quigg R, Silver MA, Gheorghiade M; Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) Investigators. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: a randomized controlled trial. JAMA. 2002 Mar 27;287(12):1541-7. doi: 10.1001/jama.287.12.1541
- Romero Osorio OM, Abaunza Camacho JF, Sandoval Briceño D, Lasalvia P, Narino Gonzalez D. Postictal neurogenic pulmonary edema: Case report and brief literature review. Epilepsy Behav Case Rep. 2017 Sep 28;9:49-50. doi: 10.1016/j.ebcr.2017.09.003
- Herbst C, Tippler B, Shams H, Simmet T. A role for endothelin in bicuculline-induced neurogenic pulmonary oedema in rats. Br J Pharmacol. 1995 Jul;115(5):753-60. doi: 10.1111/j.1476-5381.1995.tb14997.x
- Poulat P, Couture R. Increased pulmonary vascular permeability and oedema induced by intrathecally injected endothelins in rat. Eur J Pharmacol. 1998 Mar 5;344(2-3):251-9. doi: 10.1016/s0014-2999(97)01569-0
- Dutta G, Demetis S. Neurogenic pulmonary edema associated with underlying lung disease after a breakthrough seizure. Case Rep Med. 2012;2012:560942. doi: 10.1155/2012/560942
- Bärtsch P, Maggiorini M, Ritter M, Noti C, Vock P, Oelz O. Prevention of high-altitude pulmonary edema by nifedipine. N Engl J Med. 1991 Oct 31;325(18):1284-9. doi: 10.1056/NEJM199110313251805
- Rashid H, Hashmi SN, Hussain T. Risk factors in high altitude pulmonary oedema. J Coll Physicians Surg Pak. 2005 Feb;15(2):96-9.
- Saracen A, Kotwica Z, Woźniak-Kosek A, Kasprzak P. Neurogenic pulmonary edema in aneurysmal subarachnoid hemorrhage. Adv Exp Med Biol. 2016;952:35–39. doi: 10.1007/5584_2016_70
- Abraham MK, Chang WW. Subarachnoid hemorrhage. Emerg Med Clin North Am. 2016;34(4):901–916. doi: 10.1016/j.emc.2016.06.011
- Piazza O, Venditto A, Tufano R. Neurogenic pulmonary edema in subarachnoid hemorrage. Panminerva Med. 2011 Sep;53(3):203-10. https://www.minervamedica.it/en/journals/panminerva-medica/article.php?cod=R41Y2011N03A0203
- Yamagishi T, Ochi N, Yamane H, Takigawa N. Neurogenic pulmonary edema after subarachnoid hemorrhage. J Emerg Med. 2014;46(5):683–684. doi: 10.1016/j.jemermed.2013.11.094
- Muehlschlegel S. Subarachnoid Hemorrhage. Continuum (Minneap Minn). 2018 Dec;24(6):1623-1657. doi: 10.1212/CON.0000000000000679
- Williamson CA, Co I, Pandey AS, Gregory Thompson B, Rajajee V. Accuracy of daily lung ultrasound for the detection of pulmonary edema following subarachnoid hemorrhage. Neurocrit Care. 2016;24(2):189–196. doi: 10.1007/s12028-015-0161-6
- Mutoh T, Kazumata K, Ueyama-Mutoh T, Taki Y, Ishikawa T. Transpulmonary thermodilution-based management of neurogenic pulmonary edema after subarachnoid hemorrhage. Am J Med Sci. 2015;350(5):415–419. doi: 10.1097/MAJ.0000000000000561
- Hwang GJ, Sheen SH, Kim HS, Lee HS, Lee TH, Gim GH, et al. Extracorporeal membrane oxygenation for acute life-threatening neurogenic pulmonary edema following rupture of an intracranial aneurysm. J Korean Med Sci. 2013;28(6):962–964. doi: 10.3346/jkms.2013.28.6.962
- Ridenti FAS. Neurogenic pulmonary edema: a current literature review. Rev Bras Ter intensiva. 2012;24(1):91–96. doi: 10.1590/S0103-507X2012000100014
- Lo-Cao E, Hall S, Parsell R, Dandie G, Fahlström A. Neurogenic pulmonary edema. Am J Emerg Med. 2020;S0735–6757(20):31080–31089.
- Davison DL, Terek M, Chawla LS. Neurogenic pulmonary edema. Crit Care. 2012;16(2):212. doi: 10.1186/cc11226
- Muroi C, Keller M, Pangalu A, Fortunati M, Yonekawa Y, Keller E. Neurogenic pulmonary edema in patients with subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2008;20(3):188–192. doi: 10.1097/ANA.0b013e3181778156
- Davison DL, Chawla LS, Selassie L, Tevar R, Junker C, Seneff MG. Neurogenic pulmonary edema: successful treatment with IV phentolamine. Chest. 2012;141(3):793–795. doi: 10.1378/chest.11-0789
- Tyagi R, Sharad Tendolkar M, Handa A. Swimming-induced pulmonary edema with review of literature. Med J Armed Forces India. 2022 Oct;78(4):485-488. doi: 10.1016/j.mjafi.2021.01.008
- Lund KL, Mahon RT, Tanen DA, Bakhda S. Swimming-induced pulmonary edema. Ann Emerg Med. 2003 Feb;41(2):251-6. doi: 10.1067/mem.2003.69
- Milberg JA, Davis DR, Steinberg KP, Hudson LD. Improved Survival of Patients With Acute Respiratory Distress Syndrome (ARDS): 1983-1993. JAMA. 1995;273(4):306–309. doi:10.1001/jama.1995.03520280052039
- Zambon M, Vincent JL. Mortality rates for patients with acute lung injury/ARDS have decreased over time. Chest. 2008 May;133(5):1120-7. doi: 10.1378/chest.07-2134
- Cardiogenic Pulmonary Edema. https://emedicine.medscape.com/article/157452-overview#a7
- Korzeniewski K, Nitsch-Osuch A, Guzek A, Juszczak D. High altitude pulmonary edema in mountain climbers. Respir Physiol Neurobiol. 2015 Apr;209:33-8. doi: 10.1016/j.resp.2014.09.023
- Raja HM, Herwadkar AV, Paroutoglou K, Lilleker JB. Neurogenic pulmonary oedema complicating a lateral medullary infarct. BMJ Case Rep. 2018 Jul 26;2018:bcr2018225437. doi: 10.1136/bcr-2018-225437
- Felman AH. Neurogenic pulmonary edema. Observations in 6 patients. Am J Roentgenol Radium Ther Nucl Med. 1971 Jun;112(2):393-6. doi: 10.2214/ajr.112.2.393
- Muroi C, Keller M, Pangalu A, Fortunati M, Yonekawa Y, Keller E. Neurogenic pulmonary edema in patients with subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2008 Jul;20(3):188-92. doi: 10.1097/ANA.0b013e3181778156
- Yabuki H, Watanabe T, Oishi H, Katahira M, Kanehira M, Okada Y. Muse Cells and Ischemia-Reperfusion Lung Injury. Adv Exp Med Biol. 2018;1103:293-303. doi: 10.1007/978-4-431-56847-6_16
- Collins J, Kuhlman JE, Love RB. Acute, life-threatening complications of lung transplantation. Radiographics. 1998 Jan-Feb;18(1):21-43; discussion 43-7. doi: 10.1148/radiographics.18.1.9460107
- Kim J, Na S. Transfusion-related acute lung injury; clinical perspectives. Korean J Anesthesiol. 2015 Apr;68(2):101-5. doi: 10.4097/kjae.2015.68.2.101