Pulmonary infarction
Pulmonary infarction is a medical term for death of the lung tissue. Pulmonary infarction is usually a complication of another primary disease state, most commonly pulmonary embolism. Pulmonary infarction occurs in the minority (10-15%) of patients with pulmonary embolism 1. Although in a necropsy study of those with lethal pulmonary embolism, 60% of cases developed infarction 2. Moreover, the greater the embolic burden, the higher the likelihood of developing lung infarction 1. Many studies have found that pulmonary infarction is more common in the right lung, however the reason for this is not known 3.
The incidence of pulmonary embolism is approximately 1 in 1000 4. In one study, the 30-day mortality for patients found to have a pulmonary embolism was 31% and the mortality ratio in the first decade after developing a pulmonary embolism was 41% 5. Pulmonary emboli are complicated by pulmonary infarction at a rate of 16% to 31% 6. Studies evaluating hospital length-of-stay and mortality suggest similar prognosis for both pulmonary embolism with infarction and pulmonary embolism without radiographic evidence of infarction 7.
Until recently it was felt that pulmonary infarction was more common in older patients with comorbidities, especially coexisting cardiovascular disease and underlying malignancy, but rare in the young and otherwise healthy. However recent work has questioned the orthodox thinking with evidence that greater patient stature, decreased age and smoking of cigarettes are independent risk factors for developing pulmonary infarction 3. Indeed a recent study showed that heart failure, malignancy and pneumonia were not risk factors for the development of pulmonary infarction 2.
Pulmonary infarction causes
During several prospective and retrospective studies, researchers have investigated the prevalence of pulmonary infarction in association with pulmonary embolism, which is the most common etiology for the development of an infarction 7. Other disease states which can lead to pulmonary infarction include infection 8, malignancy 9, surgical iatrogenesis 10, amyloidosis, sickle cell disease 11, vasculitis 12, among others.
Smoking is a risk factor for all causes of pulmonary infarction including those associated with pulmonary embolism 13. Young age is associated with an increased likelihood while obesity is associated with a reduced likelihood of developing a pulmonary infarction in patients with pulmonary embolism 6.
Early literature suggested that patients with underlying cardiac disease are at greatest risk for developing a pulmonary infarction 14. Healthcare professionals hypothesize this to be due to poor collateral circulation, which in combination with pulmonary thromboembolism resulted in infarction. However, recent literature suggests the opposite is true. Specifically, younger patients without cardiopulmonary disease were found to be more likely to suffer a pulmonary infarction secondary to a pulmonary embolism 6. The authors of this study hypothesized longstanding local tissue hypoxia from chronic cardiopulmonary disease states led to the development of more robust vascular collateralization which protected parenchyma from infarction.
Pulmonary infarction pathophysiology
Lung tissue receives its oxygen supply from three non-redundant sources: deoxygenated blood from pulmonary arteries, oxygenated blood from the bronchial circulation, and direct oxygen diffusion from alveoli 14. Sufficient impedance of these sources can cause infarction and subsequent tissue necrosis. Inflammatory mediators from ischemic parenchyma limit gas exchange following vasoconstriction and bronchoconstriction 15. When ischemia of lung tissue is not reversed infarction ensues. A unilateral infarct occurs in 77% to 87% of pulmonary infarction, with the strongest predilection for the right lower lobe. Multiple studies show a stark predominance of pulmonary infarction in the lower lobes relative to the upper lobes 16. This has been hypothesized to be due to the gravity’s influence on the unique relationship between alveolar pressure, pulmonary arterial pressure, and bronchial arterial pressure 6.
In patients with sickle cell disease, acute chest syndrome was found to be caused by vascular infarction by direct occlusion of sickle-type hemoglobin (HbS) in 16% of cases 17. Vasculitides may result in a pulmonary infarction through antibody deposition, the formation of microaneurysms, or macrophage activation leading to vessel wall inflammation 18. Regardless of the primary etiology, the common end pathway is ischemic lung tissue.
Pulmonary infarction symptoms
Given pulmonary embolism serves as the cause of pulmonary infarction in most cases, it is important to understand the clinical picture representing both conditions. The presenting features of a pulmonary infarction overlap those of pulmonary embolism with a few important distinctions.
In patients with concurrent pulmonary embolism and pulmonary infarction, the following features were present: dyspnea (69% to 78%), chest pain (49% to 70%), swelling or pain in unilateral lower extremity (27% to 31%), fever (5% to 11%), and hemoptysis (4% to 19%) 7. Presenting features in all patients with the diagnosis of pulmonary embolism, regardless of the presence of pulmonary infarction, included dyspnea (72% to 75%), chest pain (36% to 38%), signs of DVT (22% to 33%), hemoptysis (4% to 8%) 19. Thus, pleuritic chest pain and hemoptysis were both more common in patients with pulmonary embolism and pulmonary infarction versus those with pulmonary embolism and no pulmonary infarction. Symptoms noted to have no statistical difference between the 2 groups include cough, syncope, sudden onset dyspnea, signs of DVT, fever, and right ventricular overload.
Among patients incidentally found to have a pulmonary infarction after biopsy of a radiographically discovered lung nodule, 65% of patients had no respiratory complaints, 26% had dyspnea, 7% had chest pain, and 5% had hemoptysis 20. This data highlights the difficulty of diagnosing a pulmonary infarction and emphasizes the importance of considering a broad differential diagnosis for patients who present with symptoms which could be secondary to a pulmonary infarction.
Pulmonary infarction diagnosis
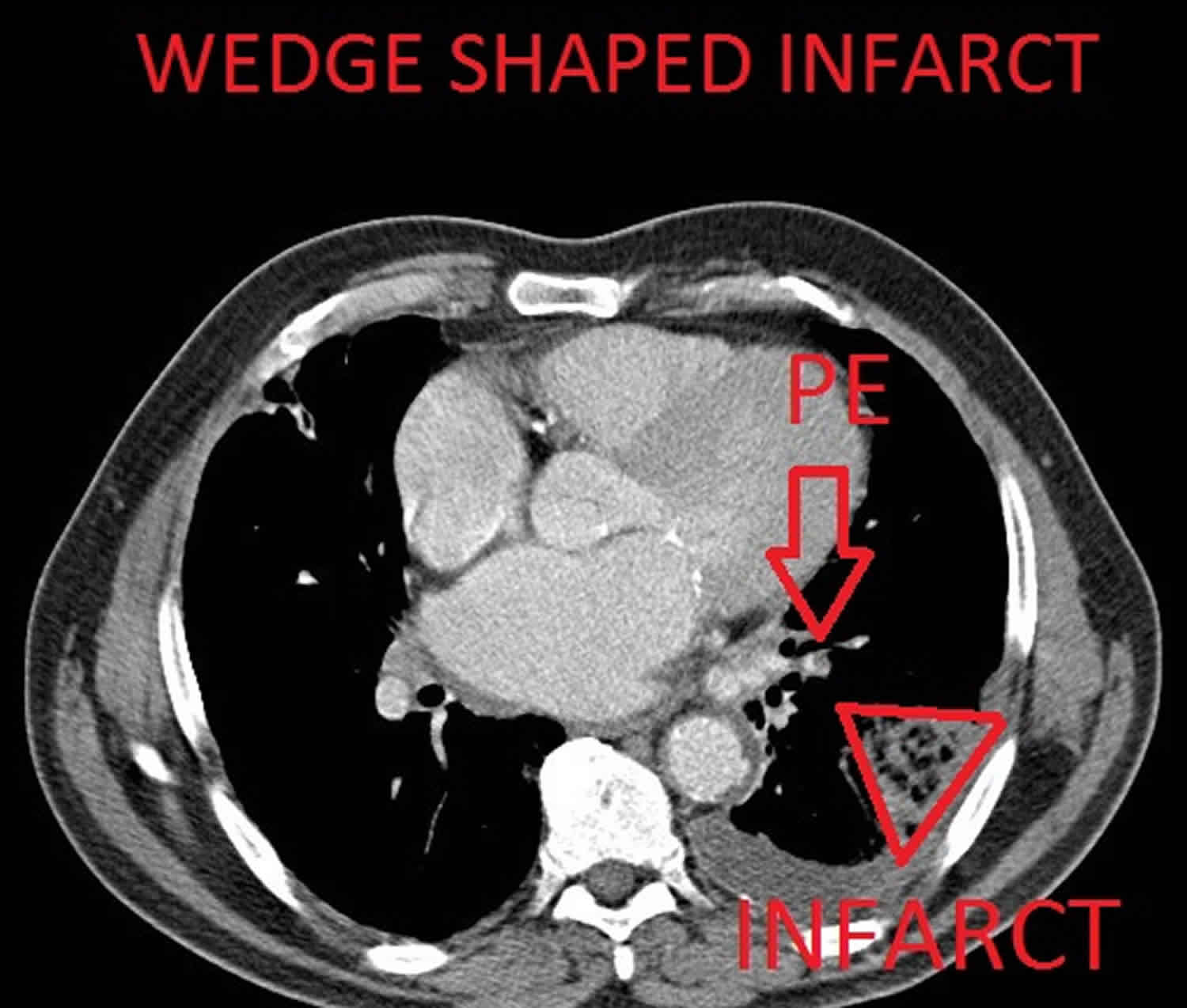
Computed tomography (CT) is the most likely imaging technique which will diagnose pulmonary infarction in combination with the clinical picture. CT findings associated with pulmonary infarction include a feeding vessel or “vessel sign,” central lucency, and a semicircular shape. The finding of air bronchograms made the presence of a pulmonary infarction less likely 6. If a vessel sign with a central lucency and no air bronchogram is present on CT, the specificity for detecting pulmonary infarction is 99% 21.
An x-ray image may be the first clue toward a diagnosis of pulmonary infarction. Hampton’s hump (wedge-shaped consolidation at the lung periphery), Westermark’s sign (radiographic oligemia or increased lucency), and Fleischer sign (prominent pulmonary artery) are specific findings but lack sensitivity to be diagnostically sufficient. Other features such as atelectasis or focal consolidation may be present but are neither sensitive nor specific 22.
In patients suspected of having infective endocarditis, consider that pulmonary infarct is a minor criterion in Dukes Criteria for Infective Carditis. Abnormalities that are seen on diagnostic studies like an electrocardiogram, D-dimer, ventilation/perfusion scan, and echocardiogram play a role in predicting pulmonary infarction and also predict pulmonary embolism.
Pulmonary infarction treatment
As with any patient, signs of respiratory distress or hemodynamic collapse should be addressed immediately with supportive care measures. Patients with pulmonary infarction may develop obstructive shock associated with a pulmonary embolism or cardiorespiratory collapse secondary to persistent hypoxia.
In addition to supportive management, treatment is guided by the underlying condition that has led to the pulmonary infarction. Pulmonary embolism initially requires anticoagulation. In patients requiring admission, heparin or low-molecular-weight heparin are started with the goal of transitioning to warfarin or other oral-anticoagulants for continued outpatient management 23. In patients with hemodynamic instability due to a sub-massive or massive pulmonary embolism, catheter-based fibrinolytics, systemic fibrinolytics, or surgical interventions exist 24. Additionally, there is a growing body of evidence that the lowest risk patients may be discharged directly from the emergency department on new or direct oral anticoagulants 25. Treatment for pulmonary infarction not caused by pulmonary embolism is varied and based upon the cause.
The average time of resolution of pulmonary infarction has not been well studied. However, one retrospective review found that of 32 patients evaluated by CT scanning after pulmonary infarctions with intervals varying from 1 to 69 weeks after initial diagnosis, 10 were found to have continued evidence of pulmonary infarction at an average interval of 10 weeks after the initial diagnosis 7. Additionally, the presence of pulmonary infarction in patients with pulmonary embolism did not alter long-term perfusion deficits determined by lung scintigraphy 19. Thus, there is no standardized recommendation for repeat CT scan to evaluate for resolution of pulmonary infarction and such decisions should be based on the particular clinical status of the patient being evaluated.
Current radiographic technology in the setting of the appropriate clinical picture makes it such that biopsy is rarely used to diagnose pulmonary infarction. A lung biopsy is typically reserved for investigating a pulmonary nodule, suspected mass, interstitial lung disease, or to collect a sample for culture 26.
References- Webb WR, Higgins CB. Thoracic Imaging: Pulmonary and Cardiovascular Radiology, North American Edition. Lippincott Williams & Wilkins. (2010) ISBN:1605479764
- Kirchner J, Obermann A, Stückradt S, Tüshaus C, Goltz J, Liermann D, Kickuth R. Lung Infarction Following Pulmonary Embolism: A Comparative Study on Clinical Conditions and CT Findings to Identify Predisposing Factors. (2015) RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 187 (6): 440-4. doi:10.1055/s-0034-1399006
- Miniati M, Bottai M, Ciccotosto C, Roberto L, Monti S. Predictors of Pulmonary Infarction. (2015) Medicine. 94 (41): e1488. doi:10.1097/MD.0000000000001488
- Wiener RS, Schwartz LM, Woloshin S. Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch. Intern. Med. 2011 May 09;171(9):831-7.
- Søgaard KK, Schmidt M, Pedersen L, Horváth-Puhó E, Sørensen HT. 30-year mortality after venous thromboembolism: a population-based cohort study. Circulation. 2014 Sep 02;130(10):829-36.
- Islam M, Filopei J, Frank M, Ramesh N, Verzosa S, Ehrlich M, Bondarsky E, Miller A, Steiger D. Pulmonary infarction secondary to pulmonary embolism: An evolving paradigm. Respirology. 2018 Mar 25.
- Chengsupanimit T, Sundaram B, Lau WB, Keith SW, Kane GC. Clinical characteristics of patients with pulmonary infarction – A retrospective review. Respir Med. 2018 Jun;139:13-18.
- Morgenthaler TI, Ryu JH, Utz JP. Cavitary pulmonary infarct in immunocompromised hosts. Mayo Clin. Proc. 1995 Jan;70(1):66-8.
- George CJ, Tazelaar HD, Swensen SJ, Ryu JH. Clinicoradiological features of pulmonary infarctions mimicking lung cancer. Mayo Clin. Proc. 2004 Jul;79(7):895-8.
- Terry PB, Buescher PC. Pulmonary Infarction: In the Beginning: The Natural History of Pulmonary Infarction. Chest. 2017 Dec;152(6):1135-1139.
- Knight J, Murphy TM, Browning I. The lung in sickle cell disease. Pediatr. Pulmonol. 1999 Sep;28(3):205-16.
- Yousem SA. The surgical pathology of pulmonary infarcts: diagnostic confusion with granulomatous disease, vasculitis, and neoplasia. Mod. Pathol. 2009 May;22(5):679-85.
- Miniati M. Pulmonary Infarction: An Often Unrecognized Clinical Entity. Semin. Thromb. Hemost. 2016 Nov;42(8):865-869.
- Tsao MS, Schraufnagel D, Wang NS. Pathogenesis of pulmonary infarction. Am. J. Med. 1982 Apr;72(4):599-606.
- Kroegel C, Reissig A. Principle mechanisms underlying venous thromboembolism: epidemiology, risk factors, pathophysiology and pathogenesis. Respiration. 2003 Jan-Feb;70(1):7-30.
- Choi SH, Cha SI, Shin KM, Lim JK, Yoo SS, Lee SY, Lee J, Kim CH, Park JY, Lee DH. Clinical Relevance of Pleural Effusion in Patients with Pulmonary Embolism. Respiration. 2017;93(4):271-278.
- Vichinsky EP, Neumayr LD, Earles AN, Williams R, Lennette ET, Dean D, Nickerson B, Orringer E, McKie V, Bellevue R, Daeschner C, Manci EA. Causes and outcomes of the acute chest syndrome in sickle cell disease. National Acute Chest Syndrome Study Group. N. Engl. J. Med. 2000 Jun 22;342(25):1855-65.
- Emmi G, Silvestri E, Squatrito D, Amedei A, Niccolai E, D’Elios MM, Della Bella C, Grassi A, Becatti M, Fiorillo C, Emmi L, Vaglio A, Prisco D. Thrombosis in vasculitis: from pathogenesis to treatment. Thromb J. 2015;13:15.
- Miniati M, Bottai M, Ciccotosto C, Roberto L, Monti S. Predictors of Pulmonary Infarction. Medicine (Baltimore). 2015 Oct;94(41):e1488.
- Parambil JG, Savci CD, Tazelaar HD, Ryu JH. Causes and presenting features of pulmonary infarctions in 43 cases identified by surgical lung biopsy. Chest. 2005 Apr;127(4):1178-83.
- Revel MP, Triki R, Chatellier G, Couchon S, Haddad N, Hernigou A, Danel C, Frija G. Is It possible to recognize pulmonary infarction on multisection CT images? Radiology. 2007 Sep;244(3):875-82.
- Worsley DF, Alavi A, Aronchick JM, Chen JT, Greenspan RH, Ravin CE. Chest radiographic findings in patients with acute pulmonary embolism: observations from the PIOPED Study. Radiology. 1993 Oct;189(1):133-6.
- Kearon C, Akl EA, Ornelas J, Blaivas A, Jimenez D, Bounameaux H, Huisman M, King CS, Morris TA, Sood N, Stevens SM, Vintch JRE, Wells P, Woller SC, Moores L. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest. 2016 Feb;149(2):315-352.
- Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ, Jenkins JS, Kline JA, Michaels AD, Thistlethwaite P, Vedantham S, White RJ, Zierler BK., American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. American Heart Association Council on Peripheral Vascular Disease. American Heart Association Council on Arteriosclerosis, Thrombosis and Vascular Biology. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011 Apr 26;123(16):1788-830.
- Frank Peacock W, Coleman CI, Diercks DB, Francis S, Kabrhel C, Keay C, Kline JA, Manteuffel J, Wildgoose P, Xiang J, Singer AJ. Emergency Department Discharge of Pulmonary Embolus Patients. Acad Emerg Med. 2018 Sep;25(9):995-1003.
- Raj R, Raparia K, Lynch DA, Brown KK. Surgical Lung Biopsy for Interstitial Lung Diseases. Chest. 2017 May;151(5):1131-1140.