Pulpitis
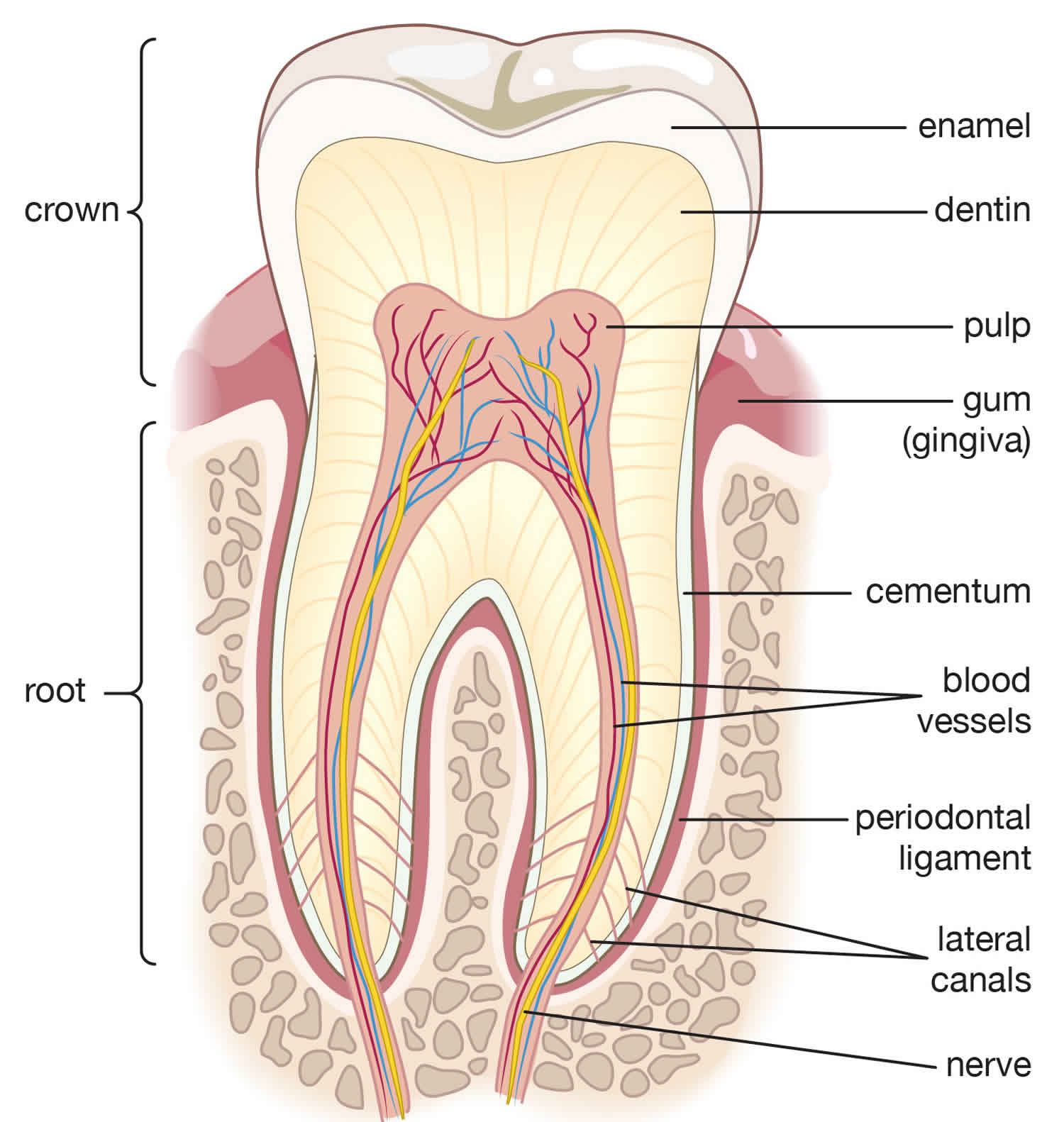
Pulpitis is inflammation of the dental pulp resulting from untreated caries, trauma, or multiple restorations. The dental pulp contains the blood vessels, the nerves and connective tissue inside a tooth and provides the tooth’s blood and nutrients. Pulpitis is mainly caused by infection by bacteria which itself is a secondary development tooth decay.
Pulpitis principal symptom is pain. Pulpitis diagnosis is based on clinical findings, and results of x-rays and pulp vitality tests. Treatment involves removing decay, restoring the damaged tooth, and sometimes doing root canal therapy or extracting the tooth.
Pulpitis is designated as:
- Reversible pulpitis: Usually, reversible pulpitis results from dental caries. That means that the pulp’s inflammation is a response to an irritant. When that irritant is removed, the pulp will return to its normal, healthy state. Pulpitis begins as limited inflammation, and the tooth can be saved by removing any decay and applying a filling to the tooth, and the pulp’s inflammation will go away.
- Irreversible pulpitis: Swelling inside the rigid encasement of the dentin compromises circulation, making the pulp necrotic, which predisposes to infection.
Pulpitis can occur when:
- Dental caries or tooth decay progresses deeply into the dentin
- A tooth requires multiple invasive procedures
- Trauma disrupts the lymphatic and blood supply to the pulp
Infectious complications of pulpitis include apical periodontitis, periapical abscess, cellulitis, and (rarely) osteomyelitis of the jaw. Spread from maxillary teeth may cause purulent sinusitis, meningitis, brain abscess, orbital cellulitis, and cavernous sinus thrombosis.
Spread from mandibular teeth may cause Ludwig angina, parapharyngeal abscess, mediastinitis, pericarditis, empyema, and jugular thrombophlebitis.
Pulpitis key points
- Pulpitis is inflammation of the dental pulp due to deep cavities, trauma, or extensive dental repair.
- Sometimes infection develops (eg, periapical abscess, cellulitis, osteomyelitis).
- Pulpitis may be reversible or irreversible.
- In reversible pulpitis, the pulp is not necrotic, a cold or sweet stimulus causes pain that typically lasts 1 or 2 seconds, and repair requires only drilling and filling.
- In irreversible pulpitis, the pulp is becoming necrotic, the stimulus (often heat) causes pain that typically lasts minutes, and root canal or extraction is needed.
- Pulpal necrosis is a later stage of irreversible pulpitis; the pulp does not respond to hot or cold but often responds to percussion, and root canal or extraction is needed.
Figure 1. Tooth anatomy
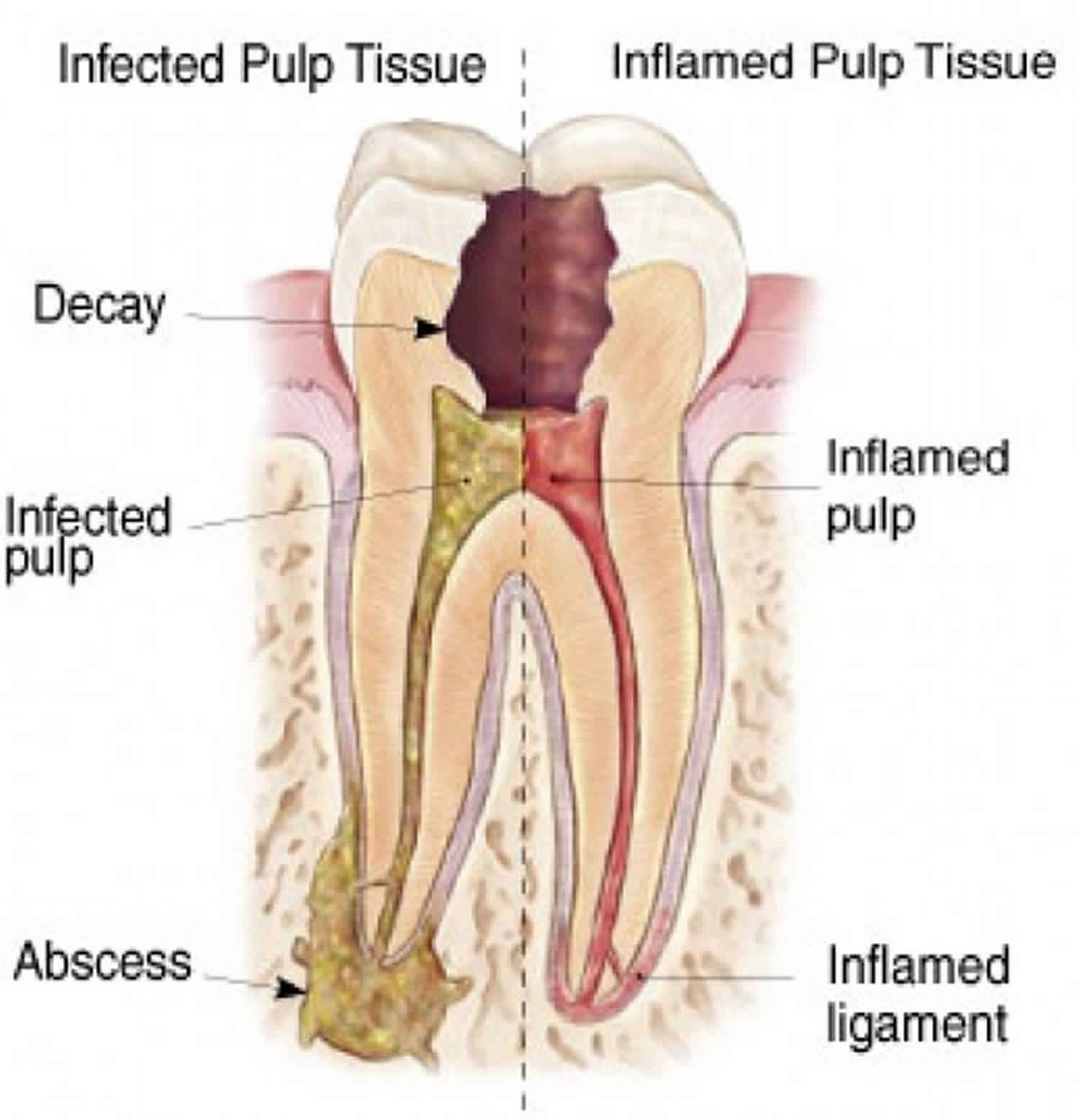
Stages of tooth decay
- Demineralization: During this stage, white or light brown spots begin to develop on the surface of the tooth. This usually occurs on teeth in the back of the mouth. Because of the location and shape of these teeth, food can get easily trapped within the cusps of teeth. As food remains, it develops into harmful bacteria. The longer this bacteria remains on teeth, the more likely that demineralization will occur. Although you may experience some dental sensitivity at this stage, side effects are generally minimal. The tooth can be remineralized and strengthened with a deeper dental cleaning, fluoride treatment, and dental sealants.
- Enamel decay: Although enamel is one of the strongest substances in the body, it is susceptible to damage. As bacteria linger on teeth, they will begin to erode the enamel, causing small holes, known as cavities. During this stage, you may feel even more dental sensitivity or have difficulty chewing on the affected side of your mouth.
- Dentin decay: The layer directly under the enamel is known as dentin. If enamel decay is left untreated, the cavity will continue to widen and deepen, causing more surface damage to the tooth. At this stage, patients generally experience stronger symptoms, such as intensified sensitivity and tooth pain, making simple tasks, such as biting and chewing uncomfortable. Although a tooth-colored filling can often repair a tooth at this stage, more aggressive treatments, such as a dental crown may be necessary.
- Pulpitis (pulp decay): Once bacteria penetrate the inner chamber of the tooth, the roots have been compromised. The pulp chamber also houses your nerves. Most patients experience severe, persistent pain that can radiate to different areas of the face and jaw. Conservative treatments include root canal therapy and a crown to protect and strengthen the tooth. In some cases a tooth extraction may be necessary.
- Abscess growth: Once an abscess develops, the tooth is no longer functional and it can place surrounding teeth and gums in danger of further decay and gum disease. Symptoms at this stage are debilitating and the tooth may need to be extracted.
Pulpitis causes
There are quite a few different ways that dental pulp can become inflamed. The most common cause is deep cavities which expose the pulp to bacteria. Tooth pulpitis occurs when the pulp is irritated or develops an infection.
Some other ways that dental pulp can become inflamed or infected include:
- Injuries or impact around the head or mouth
- A cracked or fractured tooth that exposes the pulp layer
- Using too much de-sensitizing toothpaste
- Grinding teeth (bruxism) causing teeth to crack or enamel and dentin to wear away
- A bad bite, or malocclusion, which can cause extra wear on certain teeth
Although uncommon, it is also possible to get tooth pulp inflammation from routine dental visits. For example:
- Pulpitis after a filling can occur due to teeth being exposed to extreme heat when setting the materials.
- The heat caused by tooth polishing may cause inflammation.
- Dental pulp can be exposed to bacteria during a filling treatment.
- Pulpitis after having a crown fitted; this process can irritate the pulp and compromise the nerve.
Pulpitis prevention
Since most cases of pulpitis result from dental caries, that means that preventing pulpitis is really an endeavor to prevent tooth decay. In order to keep your teeth healthy and free from caries, the most important thing to do is to follow proper oral hygiene practices. These include:
- Brushing your teeth twice a day, including the gums and tongue
- Flossing your teeth twice a day
- Replacing your toothbrush every 3 months
- Eating a healthy, balanced diet full of calcium and vitamins
- Avoiding sugary, starchy foods
- Visiting the dentist twice a year for regular cleanings
- Asking your dentist about regular fluoride treatments
By doing all that you can to keep your teeth healthy, you’re also working to keep pulpitis at bay. Of course, not all pulpitis is preventable. If trauma occurs to your teeth, pulpitis may occur despite your best efforts.
Pulpitis symptoms
Symptoms can vary depending on the type and severity of the pulpitis.
Reversible pulpitis symptoms
In reversible pulpitis, pain occurs when a stimulus (usually cold or sweet) is applied to the tooth. When the stimulus is removed, the pain ceases within 1 to 2 seconds.
Irreversible pulpitis symptoms
Compared with the symptoms for reversible pulpitis, the symptoms of irreversible pulpitis are more severe and varied. There are many different symptoms, including:
- Continuous tooth pain, usually dull or throbbing in nature
- A tooth that hurts when touched
- Prolonged pain or sensitivity after exposure to heat, cold, or sugar
- Pain and sensitivity in the jaw around the tooth
- Swelling of the jaw or face
- Fever
- Tooth pain so severe that it may awaken you at night
- Tooth abscesses, in severe cases
In irreversible pulpitis, pain occurs spontaneously or lingers minutes after the stimulus (usually heat, less frequently cold) is removed. A patient may have difficulty locating the tooth from which the pain originates, even confusing the maxillary and mandibular arches (but not the left and right sides of the mouth). The pain may then cease for several days because of pulpal necrosis. When pulpal necrosis is complete, the pulp no longer responds to hot or cold but often responds to percussion. As infection develops and extends through the apical foramen, the tooth becomes exquisitely sensitive to pressure and percussion. A periapical (dentoalveolar) abscess elevates the tooth from its socket, and the tooth feels “high” when the patient bites down.
Pulpitis diagnosis
Pulpitis diagnosis is based on the history and physical examination, which makes use of provoking stimuli (application of heat, cold, and/or percussion). Your dentist may also use an electrical pulp tester to evaluate whether the pulp is alive but not whether it is healthy. The dentist will put a drop of conducting paste on the to-be-tested tooth, and they will then use the pulp tester to deliver small electrical currents to the tooth. If the pulp is normal, it will have a mild response to the current that does not linger once the test is removed. If there is pulpitis, there will be a more intense, painful reaction to the electrical current compared with normal teeth. If the pain is mild and disappears after a few seconds, this generally indicates the presence of reversible pulpitis. If the test causes severe pain that lingers longer than 30 seconds, it is likely that the tooth has irreversible pulpitis. If the tooth does not react at all to the electrical currents, that means the pulp has likely necrotized.
If a stimulus and/or electrical pulp tests reveals that your tooth shows a prolonged painful reaction to stimuli, that means it is likely irreversible pulpitis. Your dentist will likely perform x-rays to confirm the diagnosis. X-rays help determine whether inflammation has extended beyond the tooth apex and help exclude other conditions.
Pulpitis treatment
Since there are several different types of pulpitis, there are also several possible treatments. Your dentist will complete some tests to see whether your tooth can still be saved with reversible pulpitis treatment, or whether you need a tooth extracted for irreversible pulpitis treatment.
Reversible pulpitis treatment
In reversible pulpitis, pulp vitality can be maintained if the tooth is treated, usually by caries removal, and then restored.
During reversible pulpitis treatment, your dentist will remove any cavities and add a filling to stop the pulp being exposed.
Similarly, tooth pulpitis caused by a crack in the tooth can also be treated with a filling, or perhaps a crown.
Irreversible pulpitis treatment
In irreversible pulpitis, the pulpitis and its complications require endodontic (root canal) therapy or tooth extraction. In endodontic therapy, an opening is made in the tooth and the pulp is removed. The root canal system is thoroughly debrided, shaped, and then filled with gutta-percha. After root canal therapy, adequate healing is manifested clinically by resolution of symptoms and radiographically by bone filling in the radiolucent area at the root apex over a period of months. If patients have systemic signs of infection (eg, fever), an oral antibiotic is prescribed (amoxicillin 500 mg every 8 hours; for patients allergic to penicillin, clindamycin 150 mg or 300 mg every 6 hours). If symptoms persist or worsen, root canal therapy is usually repeated in case a root canal was missed, but alternative diagnoses (eg, temporomandibular disorder, occult tooth fracture, neurologic disorder) should be considered.
Very rarely, subcutaneous or mediastinal emphysema develops after compressed air or a high-speed air turbine dental drill has been used during root canal therapy or extraction. These devices can force air into the tissues around the tooth socket that dissects along fascial planes. Acute onset of jaw and cervical swelling with characteristic crepitus of the swollen skin on palpation is diagnostic. Treatment usually is not required, although prophylactic antibiotics are sometimes given.