Pure tone audiometry
Pure tone audiometry also called air conduction testing since the sounds go through your outer and middle ear, is a hearing test used to measure hearing sensitivity to identify hearing threshold levels of an individual, enabling determination of the degree, type and configuration of a hearing loss. Pure tone audiometry test helps find the quietest sound you can hear at different pitches, or frequencies. A pure tone audiometry test measures the softest, or least audible, sound that a person can hear. During the pure tone audiometry test, you will wear earphones and hear a range of sounds directed to one ear at a time. The loudness of sound is measured in decibels (dB). A whisper is about 20 dB, loud music ranges 80-120 dB, and a jet engine is about 180 dB. The tone of sound is measured in frequencies (Hz). Low bass tones range 50-60 Hz, high-pitched tones range 10,000 Hz or higher. Normal hearing range is 250-8,000 Hz at 25 dB or lower. Hearing sensitivity is plotted on an audiogram, which is a graph displaying intensity as a function of frequency.
Pure-tone audiometry requires a quiet testing environment with low levels of background noise. Background noise can cause elevated thresholds, especially in low frequencies. To minimize the number of false-positive results, sound levels in the test environment should not exceed American National Standards Institute (ANSI) requirements 1. A quiet booth that features sound-absorptive materials such as carpeting, acoustic foam, or tiles is considered standard practice. Industrial hygienists, biomedical maintenance technicians, and audiologists can evaluate environmental noise levels in the test area using a sound level meter to ensure that ANSI specifications are met.
Pure-tone audiometry is performed with the use of an audiometer. Handheld audiometers have a sensitivity of 92 percent and a specificity of 94 percent in detecting sensorineural hearing impairment 2. There are several types of audiometers available, but all function similarly by allowing the tester to increase and decrease the intensity (loudness, in decibels [dB]) and frequency (pitch, in cycles per second or Hz) of the signal as desired.
Sometimes, it is not possible to use earphones. An example is when a child refuses to wear them. In these cases, sounds come through speakers inside a sound booth. This is sound-field screening. The sounds go into both ears at the same time. This type of testing does not show if there is a hearing loss in only one ear.
You may respond to the sounds by:
- Raising a finger or hand
- Pressing a button and pointing to the ear where you heard the sound
- Saying “yes” to indicate that you heard the sound
Your ears have three distinct parts: the outer, middle, and inner ear (Figures 1 and 2). Pure-tone audiometry involves measuring the peripheral and central auditory systems. Audiometry tests can detect whether you have sensorineural hearing loss (damage to the nerve or cochlea) or conductive hearing loss (damage to the eardrum or the tiny ossicle bones). During an audiometry evaluation, a variety of tests may be performed.
A tympanometry test detects problems such as fluid/wax buildup, perforated eardrum, ossicle bone damage, or tumors in the middle ear. Acoustic reflex testing evaluates the cranial nerves and brainstem.
A word recognition test (also called speech discrimination test) assesses a person’s ability to understand speech from background noise. If your speech discrimination is poor, speech may sound garbled. Word recognition scores can be helpful in predicting the usefulness of a hearing aid.
Additional audiometric testing by an audiologist is recommended for patients whose pure-tone thresholds fall outside the range of normal limits 3.
Pure-tone audiometry is broadly defined as either screening or threshold search:
- Screening audiometry presents tones across the speech spectrum (500 to 4,000 Hz) at the upper limits of normal hearing (25 to 30 dB for adults, and 15 to 20 dB for children) 4. Results are recorded as pass, indicating that the patient’s hearing levels are within normal limits, or refer, indicating that hearing loss is possible and a repeat screening test or a threshold search test is recommended.
- Threshold search audiometry determines the softest sound a patient can hear at each frequency 50 percent of the time. This testing requires more time and expertise than screening audiometry. The American Speech-Language-Hearing Association has a recommended procedure for pure-tone threshold search tests known as the modified Hughson-Westlake method 5. Testing begins with the ear in which the patient perceives to have better hearing. The tester presents a pure tone at a clearly audible level. After the patient responds to the pure-tone signal, the tester decreases intensity by 10 dB and presents the tone again. If the patient responds to this tone, a “down 10” pattern is employed, with the tester decreasing the intensity of the tone by 10 dB and presenting a tone until the patient no longer responds.18 The tester then increases tone intensity by 5 dB until the patient responds. This is the patient’s initial ascending response.
To check for accuracy, the tester should decrease the intensity of the tone by 10 dB one more time to check for no response, then increase the intensity of the signal in 5 dB increments until the patient responds again to the signal. If the patient responds consistently (minimum two out of three responses in ascending order), the tester records the dB level at which the patient responds as the air conduction threshold. After testing the ear that is perceived to have better hearing, the tester then performs the same tests on the patient’s other ear.
Testing should begin at 1,000 Hz, because this frequency is easily heard by most patients and has the greatest test-retest reliability 5. A common frequency sequence for pure-tone threshold search testing is to test at 1,000, 2,000, 3,000, 4,000, 8,000, 1,000 (repeat), 500, and 250 Hz 6.
Degrees of hearing loss
Hearing loss is often described as follows:
- Normal hearing = less than 25 dB (0–25 dB) hearing level. At this level, hearing is within normal limits.
- Mild hearing loss = 26-40 dB hearing level. Mild hearing loss may cause inattention, difficulty suppressing background noise, and increased listening efforts. Patients with this degree of loss may not hear soft speech. Children may be fatigued after listening for long periods.
- Moderate hearing loss = 41-55 dB hearing level. Moderate hearing loss may affect language development, syntax and articulation, interaction with peers, and self-esteem. Patients with this degree of loss have trouble hearing some conversational speech.
- Moderate-severe hearing loss = 56–70 dB hearing level. Moderate-severe hearing loss may cause difficulty with speech and decreased speech intelligibility. Patients with this degree of loss do not hear most conversational-level speech.
- Severe hearing loss = 71-90 dB hearing level. Severe hearing loss may affect voice quality.
- Profound hearing loss = more than 90 dB (>90 dB) hearing level. With profound hearing loss (deafness), speech and language deteriorate.
Ear hearing anatomy
The primary functionality of the middle ear (tympanic cavity) is that of bony conduction of sound via transference of sound waves in the air collected by the auricle to the fluid of the inner ear. The middle ear inhabits the petrous portion of the temporal bone and is filled with air secondary to communication with the nasopharynx via the auditory (eustachian) tube.
The tympanic membrane is an oval, thin, semi-transparent membrane that separates the external and middle ear (tympanic cavity). The tympanic membrane is divided into 2 parts: the pars flaccida and the pars tensa. The manubrium of the malleus is firmly attached to the medial tympanic membrane; where the manubrium draws the tympanic membrane medially, a concavity is formed. The apex of this concavity is called the umbo. The area of the tympanic membrane superior to the umbo is termed the pars flaccida; the remainder of the tympanic membrane is the pars tensa.
Figure 1. Ear anatomy

Figure 2. Middle ear anatomy

Pure tone audiometry test technique
The necessary equipment depends on the testing method used and may include the following:
- Headphones
- Insert earphones
- Speakers
- Bone-conduction oscillator
Patients are usually seated in a comfortable position.
Air conduction
Air conduction test assesses sensitivity when the signal is transmitted through the outer, middle, and inner ear and then through the brain to the cortex. Testing may be performed using headphones, insert earphones, or sound fields.
Headphones are placed over the outer ear. Circumaural headphones have a large cushion and fit around the ear, contacting the head. These generally are used to reduce ambient noise. Supra-aural headphones are more common and rest on the ear or pinna, but they typically provide no ambient noise reduction and may collapse the ear canals.
Insert earphones are transducers housed in a small box approximately 2″ by 3″ by 0.5″. The signal is transmitted down a tube to foam tips, which fit in the ear canal. Insert earphones help reduce collapsing ear canals, and they reduce ambient noise and crossover of auditory stimuli to the nontest ear via skull transmission.
Sound-field (free-field) testing signals are presented via speakers, usually at a 45° azimuth to the patient’s face. This form of testing is used with infants, toddlers, and other individuals with special needs for whom earphone use may be problematic. During sound-field testing, an individual sits in the center of the room, facing forward, halfway between each speaker. Typically, visual-reinforcement audiometry (toys light and animate when the child responds to sound); conditioned-orientation response audiometry (toys on both sides test localization); or play audiometry (various games, eg, dropping a block in response to sound) are used. These conditioned responses to auditory stimulus provide reinforcement that allows for measurable responses and longer interest in the test situation.
In a sound field, the auditory signals are warble tones or bursts of narrow-band noise. Pure tones cannot be used because they can create standing waves in a sound field, which can alter signal intensity.
Sound-field testing may also assess hearing aid benefit. Placing the person in the center of the room (facing the speakers) yields aided thresholds. The difference between aided and unaided thresholds is termed functional gain.
Bone conduction
Bone conduction technique assesses sensitivity when the signal is transmitted through the bones of the skull to the cochlea and then through the auditory pathways of the brain. This type of testing bypasses the outer and middle ear.
A small oscillator is placed on the forehead or more commonly, the mastoid bone. The device stimulates the bones of the skull, which in turn stimulates both cochleae. The oscillator may produce a vibration that is perceived by the patient, thus eliciting a vibrotactile response instead of a response to the auditory stimulus.
Crossover
Crossover occurs when sound presented to the test ear travels across the head to the nontest ear. This occurs at approximately 40 dB for circumaural earphones across all frequencies. When hearing sensitivity is much poorer in the test ear than the nontest ear, the signal may cross over and be perceived in the ear with better hearing, thus yielding a false impression of the intended test ear’s sensitivity.
Insert earphones reduce the crossover by reducing surface contact area.
Masking
Masking presents a constant noise to the nontest ear to prevent crossover from the test ear. The purpose of masking is to prevent the nontest ear from detecting the signal (line busy), so only the test ear can respond.
When a signal is presented to the test ear, the signal may also travel through the head and reach the cochlea on the other side. However the intensity of the signal from the test to the nontest ear can be reduced by the mass of the head. This signal reduction is called interaural attenuation. For bone conduction, the interaural attenuation may be as low as 0 dB because the bones of the skull are very efficient at transmitting sound. Thus, any suspected difference in bone conduction between the test and nontest ears requires masking. Interaural attenuation for air conduction can range between 40 and 80 dB. Masking should be used if the difference in air conduction in one ear and bone conduction in the other ear is 40 dB or greater.
Thresholds obtained with masking in the contralateral ear are called masked thresholds and should represent the true threshold of the test ear. A masking dilemma occurs when masking from the nontest ear crosses over to the test ear and affects threshold testing for the test ear. In this case, a reliable masked threshold cannot be obtained and is referred to as the masking dilemma. This phenomenon generally occurs only in the presence of a substantial conductive component to the hearing loss and is less problematic with the more common use of insert earphones.
Pure tone audiogram
Pure tone audiometry charts the hearing level of different tone frequencies in both ears. The audiogram is a chart of hearing sensitivity with sound frequency charted on the horizontal X-axis and sound intensity on the vertical Y-axis (Figure 3). Sound intensity is the level of sound power measured in decibels (dB); loudness is the perceptual correlate of intensity. Right ear thresholds are manually recorded as a red circle (O) on the audiogram. Left ear thresholds are manually recorded as a blue X (Figures 4 to 7).
For threshold testing intensity, decibels are measured in hearing level (HL), which is based on the standardized average of individuals with normal hearing sensitivity. Hearing level (HL) is not equivalent to sound pressure level (SPL), but the American National Standards Institute (ANSI) has defined a relationship between sound pressure level (SPL) and hearing level (HL) for each audiometric frequency from 250–8000 hertz (Hz).
Degrees of hearing loss:
- Normal hearing = less than 25 dB (0–25 dB) hearing level. At this level, hearing is within normal limits.
- Mild hearing loss = 26-40 dB hearing level. Mild hearing loss may cause inattention, difficulty suppressing background noise, and increased listening efforts. Patients with this degree of loss may not hear soft speech. Children may be fatigued after listening for long periods.
- Moderate hearing loss = 41-55 dB hearing level. Moderate hearing loss may affect language development, syntax and articulation, interaction with peers, and self-esteem. Patients with this degree of loss have trouble hearing some conversational speech.
- Moderate-severe hearing loss = 56–70 dB hearing level. Moderate-severe hearing loss may cause difficulty with speech and decreased speech intelligibility. Patients with this degree of loss do not hear most conversational-level speech.
- Severe hearing loss = 71-90 dB hearing level. Severe hearing loss may affect voice quality.
- Profound hearing loss = more than 90 dB (>90 dB) hearing level. With profound hearing loss (deafness), speech and language deteriorate.
Frequency
Frequency is cycles per unit of time. Pitch is the perceptual correlate of frequency. Frequency is measured in hertz (Hz), which are cycles per second.
Usually frequencies of 250–8000 Hz are used in testing because this range represents most of the speech spectrum, although the human ear can detect frequencies from 20–20,000 Hz. Some children can detect even higher frequencies.
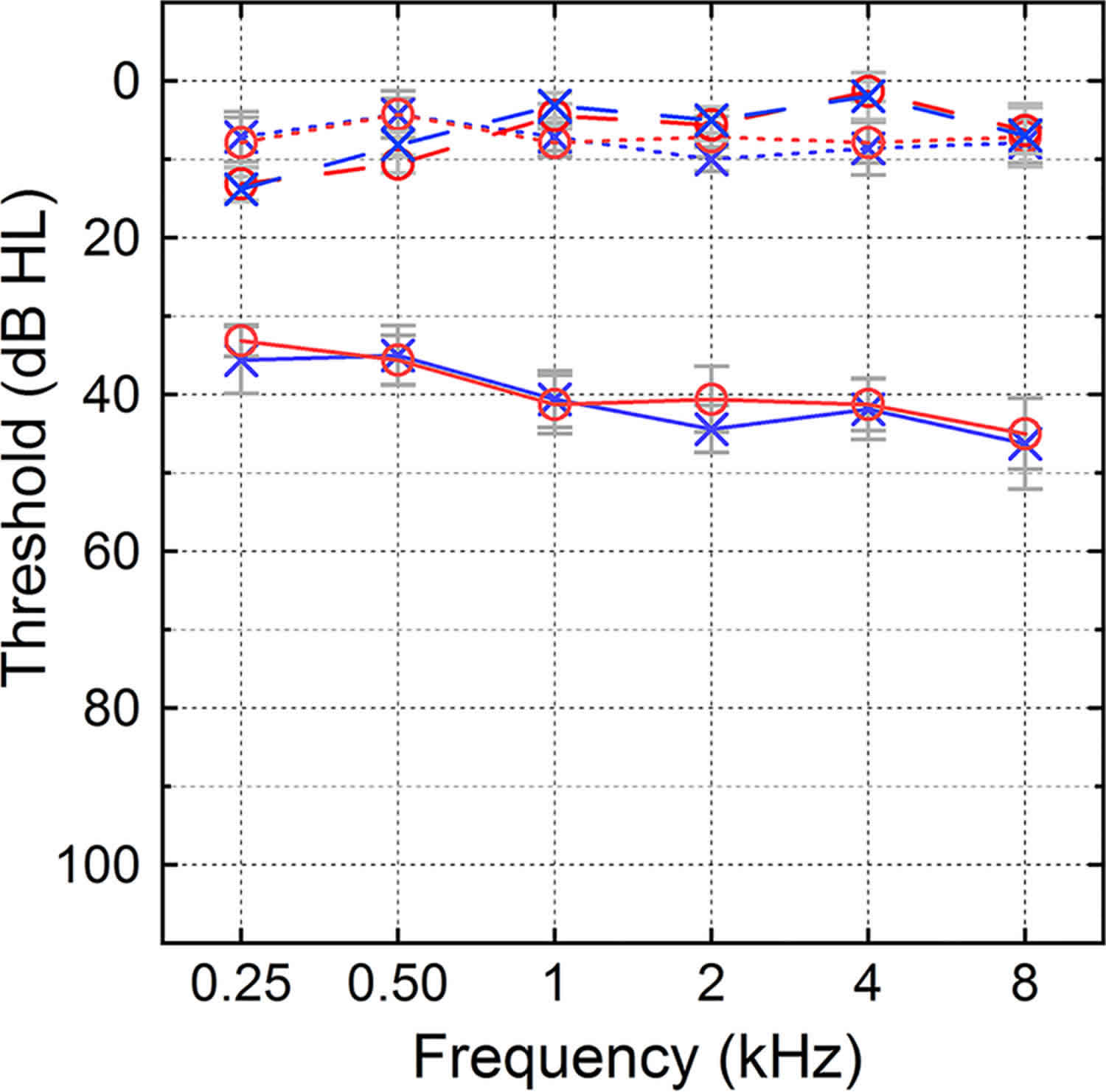
Figure 3. Pure tone audiogram
Pure-tone average
Pure-tone average (PTA) is the average of hearing sensitivity at 500, 1000, and 2000. This average should approximate the speech reception threshold (SRT), within 5 dB, and the speech detection threshold (SDT), within 6–8 dB.
If the speech reception threshold (SRT) is significantly better than the pure-tone average (PTA), the possibility of pseudohypoacusis should be considered. If the pure-tone average (PTA) is significantly better than the speech reception threshold (SRT), the possibility of central involvement should be considered.
Speech reception threshold
The speech reception threshold (SRT) is the softest intensity spondee words that an individual can repeat at least 50% of the time.
Spondees are two-syllable words equally emphasizing both syllables. The word “downtown” is a spondee, with the stressed syllable of “down” followed by another stressed syllable, “town”. In some cases (eg, patients with poor word recognition), a limited set of words may be used.
Speech detection threshold
The speech detection threshold (SDT), also termed the speech awareness threshold (SAT), is the lowest intensity speech stimulus that an individual can detect at least 50% of the time.
Word recognition
Word recognition previously called speech discrimination, is the ability to repeat correctly an open set of monosyllabic words at suprathreshold intensity. Word lists are phonetically balanced (PB), meaning that the speech sounds used occur with the same frequency as in the whole language.
The score represents the percent of words correct for most word recognition tests.
Special considerations affecting audiometry interpretation
Patient history
Patients may feign or exaggerate hearing loss for personal reasons, and may intentionally or unintentionally misreport on testing. Patients with constant, bothersome tinnitus (ringing or buzzing in the ears) often have difficulty discerning pure tones. Many combat veterans have a history of blast exposures, mild concussion, or posttraumatic stress disorder 7. These patients may have difficulty completing audiometry for reasons related to headaches, memory problems, irritability, or fatigue. Taking a history before the hearing test will alert the physician to these possibilities. Supplemental, objective tests such as evoked otoacoustic emissions testing (stimulation of hair cells to produce sound) and patient questionnaires can assist with difficult-to-test populations 8.
Recent noise exposure before pure-tone testing may affect the validity of the test results. Riding a loud motorcycle or listening to music through headphones may result in a temporary hearing threshold shift, and may not reflect the patient’s true hearing thresholds. Patients should minimize or avoid exposure to loud noise for at least 14 hours before pure-tone testing 9.
Physical findings
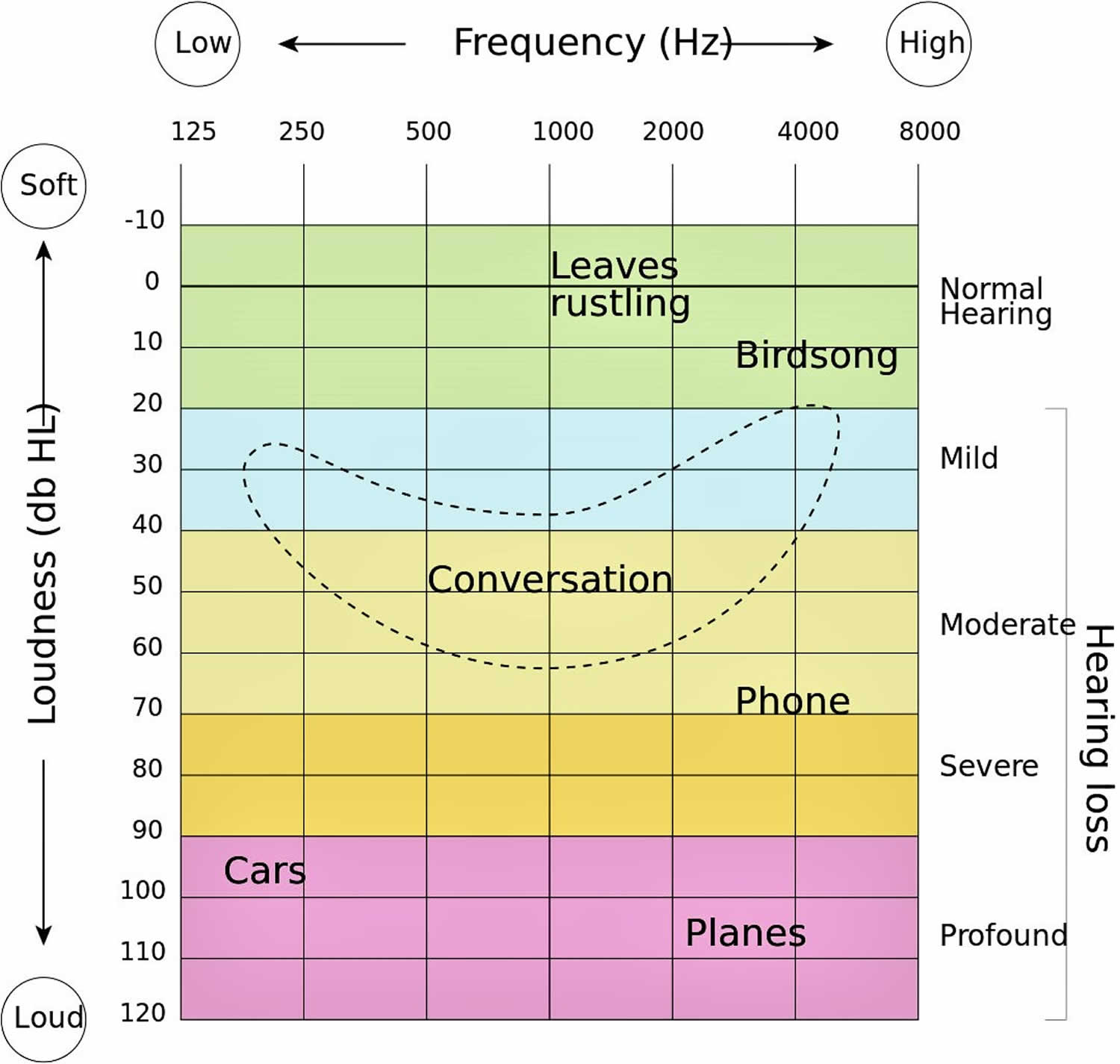
Audiometry results may be affected in patients with anatomic anomalies, such as narrow or collapsing ear canals (stenosis of the ear canal), complete canal occlusion, or absence of an ear canal (atresia). Impacted cerumen (earwax) can cause a conductive hearing loss (Figure 4) that typically resolves following cerumen removal. Collapsed ear canals occur in many older patients whose cartilage has become flaccid. Placing an over-the-ear headphone over already narrow or closed ear canals may add sufficient pressure to collapse the ear canals even further, resulting in a false high-frequency hearing loss. An otoscopic examination should be performed before the hearing test to ensure that the tympanic membrane is at least partially visible.
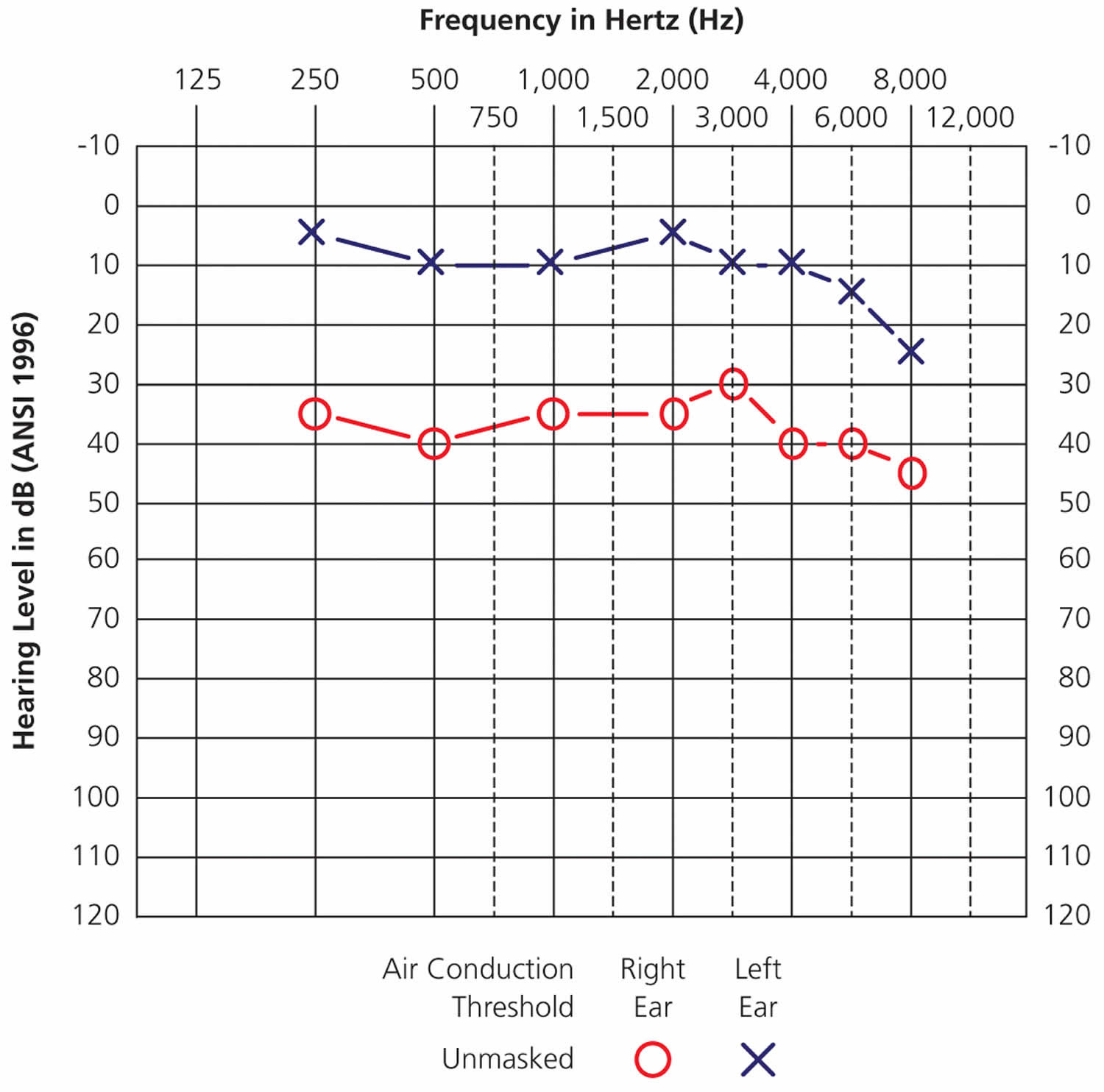
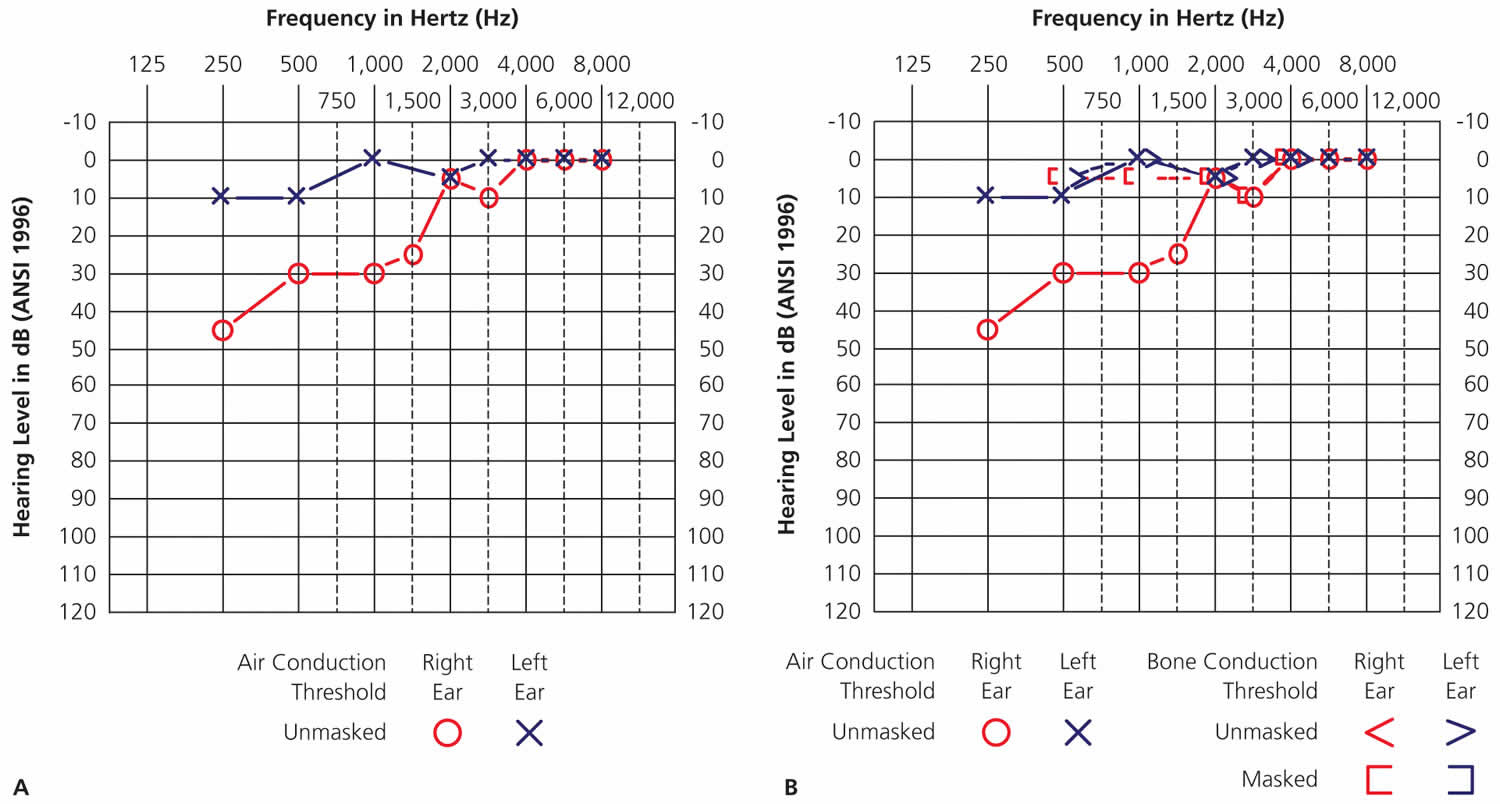
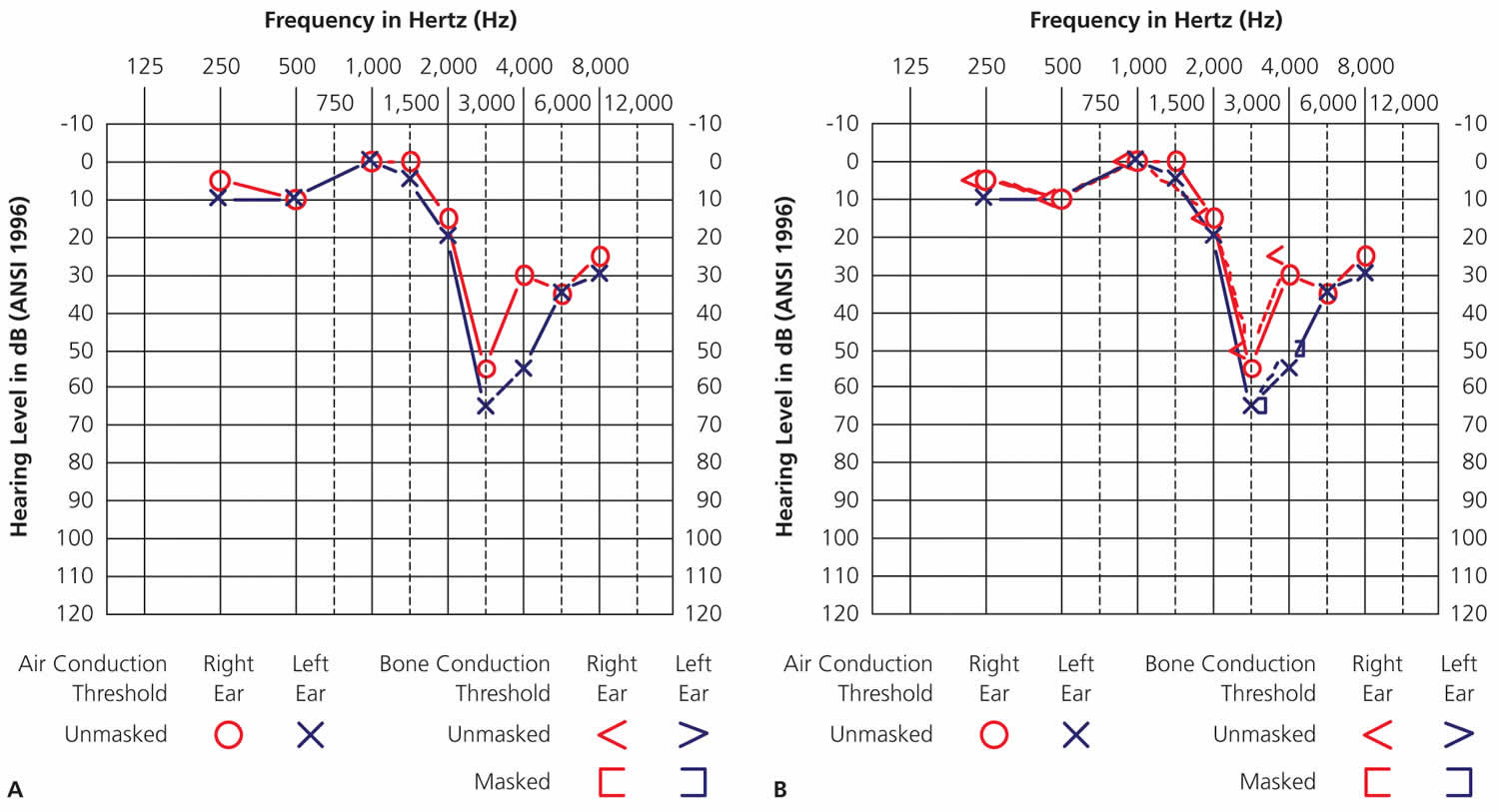
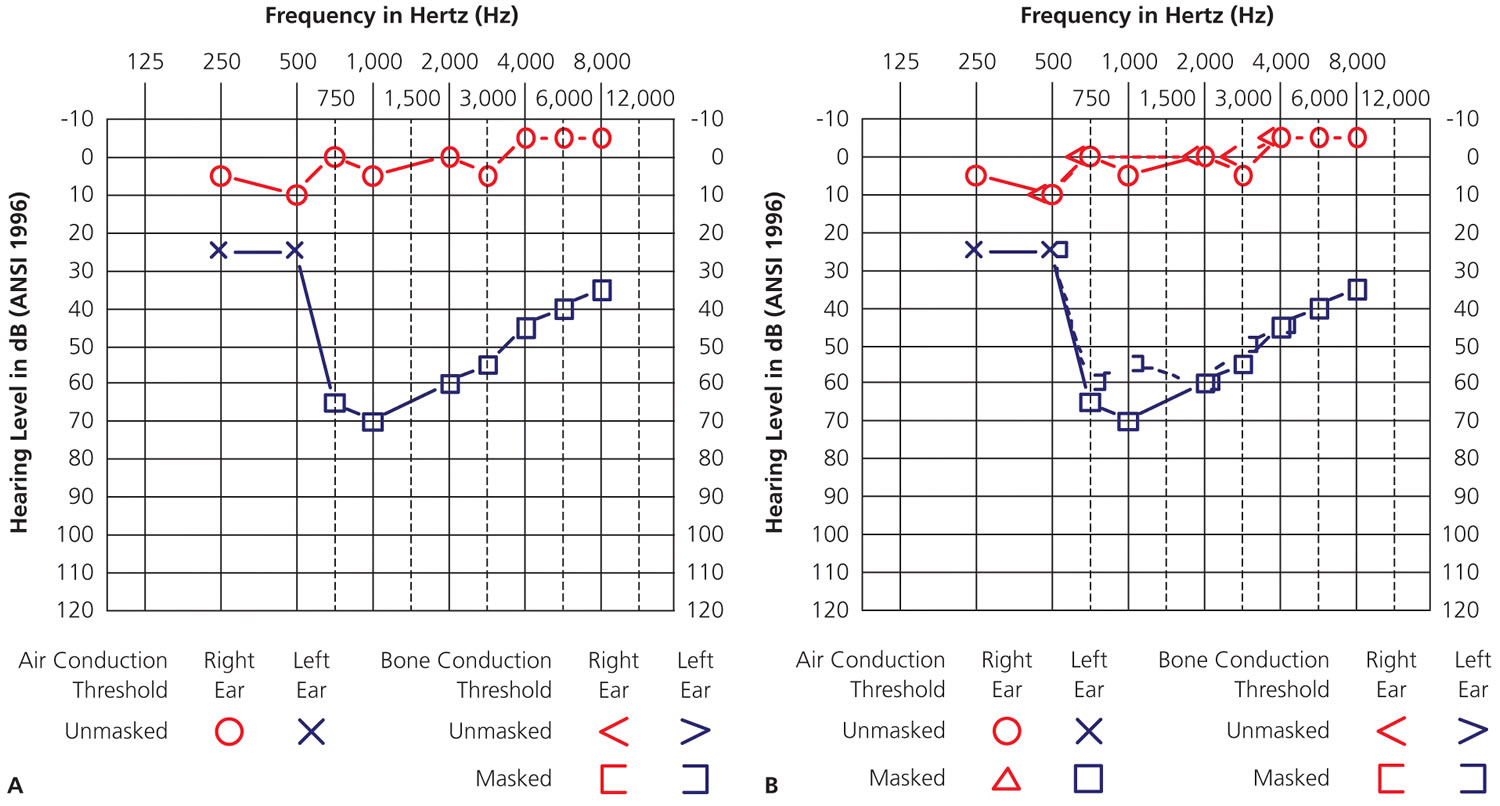
Differentiating conductive hearing loss from sensorineural hearing loss requires bone conduction testing. Audiometry relies on techniques similar to the Weber and Rinne tests to compare air and bone conduction. Bone conduction audiometry measures pure-tone thresholds using a mechanical device that transmits sounds via vibration through the forehead or mastoid bone. Figures 5A and 5B demonstrate differences in air and bone conduction thresholds (an air-bone gap) for a patient with a tympanic membrane rupture 10. Figures 6A and 6B illustrate no air-bone gap for a patient with bilateral hearing loss. Unilateral or asymmetrical hearing loss (Figures 7A and 7B) can be symptomatic of a central nervous system lesion, including vestibular schwannoma (commonly though incorrectly called an acoustic neuroma), and warrants additional evaluation and imaging 11.
If the pure-tone threshold difference or asymmetry between ears at any frequency is equal to or greater than 40 dB, the sound energy from the test ear can stimulate the nontest ear, causing the nontest ear to respond to the stimulus. To prevent this crossover of sound from one ear to the other, narrow band noise is presented to the nontest ear and thresholds are recorded as masked 10. Right ear masked air conduction thresholds are manually recorded as a red triangle on the audiogram. Left ear masked air conduction thresholds are manually recorded as a blue box. Right ear masked bone conductions are manually recorded as a red square bracket (open on the right side). Left ear masked bone conduction thresholds are manually recorded as a blue square bracket (open on the left side). Figures 7A and 7B show masked bone conduction thresholds in the left ear.
Types of hearing loss
Conductive hearing loss
Conductive hearing loss has normal bone-conduction thresholds, but air-conduction thresholds are poorer than normal by at least 10 dB.
Conductive hearing loss is secondary to an outer ear or middle ear abnormality, which can include abnormalities of the tympanic membrane. The abnormality reduces the effective intensity of the air-conducted signal reaching the cochlea, but it does not affect the bone-conducted signal that does not pass through the outer or middle ear.
Examples of abnormalities include occlusion of the external auditory canal by cerumen or a mass, middle ear infection and/or fluid, perforation of the tympanic membrane, or ossicular abnormalities. Pure-tone air-conduction thresholds are poorer than bone-conduction thresholds by more than 10 dB.
Figure 4. Conductive hearing loss audiogram (right ear)
Footnote: Right ear, flat conductive hearing loss across all frequencies due to complete occlusion of the ear canal with cerumen.
Figure 5. Mid-frequency conductive hearing loss (right ear)
Footnote: Right ear bone conduction is better than air conduction. The patient has low- to mid-frequency conductive hearing loss due to tympanic membrane perforation.
Sensorineural hearing loss
Sensorineural hearing loss has bone- and air-conduction thresholds within 10 dB of each other, and thresholds are higher than 25 dB hearing level.
Sensorineural hearing loss is secondary to cochlear abnormalities and/or an abnormality of the auditory nerve or central auditory pathways. Because, in this type of hearing loss, the outer ear and middle ear do not reduce the signal intensity of the air-conducted signal, both air- and bone-conducted signals are effective in stimulating the cochlea. Pure-tone air- and bone-conduction thresholds are within 10 dB.
Examples included presbycusis, noise-induced hearing loss (Figure 6), Ménière disease, and retrocochlear lesions such as vestibular schwannoma (Figure 7).
Figure 6. Sensorineural hearing loss (both ears)
Footnote: Bilateral, noise-induced sensorineural hearing loss. There are no significant differences between air and bone conduction thresholds. The asymmetry at 3,000 Hz and 4,000 Hz (with the left ear worse than the right) reflects this patient’s occupation as a soldier in the infantry and being a right-handed shooter.
Figure 7. Sensorineural hearing loss (left ear)
Footnote: Left ear sensorineural hearing loss due to vestibular schwannoma. With sensorineural hearing loss, there is no significant difference in threshold between air and bone conduction.
Mixed hearing loss
Mixed hearing loss has conductive and sensorineural components.
This type of hearing loss has sensorineural and conductive components. Pure-tone air-conduction thresholds are poorer than bone-conduction thresholds by more than 10 dB, and bone-conduction thresholds are less than 25 dB.
Common auditory disorders
Presbycusis usually manifests as a bilateral and symmetric sensorineural hearing loss. Usually, the higher frequencies are most severely affected. Word recognition may be poorer than predicted from the audiogram. A person with presbycusis may have more difficulty with hearing aids than a younger patient with equivalent hearing loss.
Onset of presbycusis typically occurs in middle-aged or older patients. Hearing loss is secondary to degeneration of the cochlea, cranial nerve VIII (eighth cranial nerve or vestibulocochlear nerve), and/or the central auditory system. The condition is usually slowly progressive.
Otitis media
This condition is marked by fluid in the middle ear space, which may be caused by inflammation of the middle ear lining or inadequate aeration of the middle ear space. Otitis media frequently results in flat or up-sloping conductive hearing loss. Word recognition usually is excellent. With acute otitis media, otalgia or fever may accompany the condition.
Onset can occur at any age, but otitis media is most common in young children 12. Without intervention, the fluid can become more viscous, and greater hearing loss develops as the middle ear mechanism stiffens. In some cases, otitis media can progress to mastoiditis, and/or cholesteatoma.
Noise-induced hearing loss
Exposure to high-intensity noise may cause temporary or permanent hearing loss. Repeated exposure to noise trauma may change a temporary threshold shift (TTS) to a permanent threshold shift (PTS). However permanent threshold shift can occur secondary to a single noise exposure in some cases. Degree and configuration of hearing loss depends on time exposure, sound intensity, and sound frequency characteristics. Noise-induced hearing loss is typically greatest in the 4000- to 6000-Hz region.
With more intense sound, the exposure time before hearing loss may be shorter 13. Noise-induced hearing loss is sensorineural except in certain blast injuries with possible tympanic membrane and middle ear damage.
Onset may occur at any age, and intersubject variability is high even for the same exposure. Hearing loss may be unilateral or bilateral but is usually bilateral. Asymmetric noise exposure (eg, from firearms) may yield asymmetric hearing loss. Degree of hearing loss can vary. Complaints of muffled hearing or tinnitus are common. Hearing loss is secondary to cochlear damage.
Otosclerosis
Otosclerosis causes a slowly progressive conductive or mixed hearing loss. Word recognition is usually excellent when speech is sufficiently loud. The condition is caused by stapedial fixation in the oval window, stiffening the middle ear system.
Onset usually occurs when patients are aged 15–45 years, and otosclerosis is more common in women than in men. One half of patients report a family history of otosclerosis.
Ménière disease
Ménière disease affects the cochlear and vestibular systems. Attacks lasting from 20 minutes to several hours generally include some combination of vertigo, hearing loss, sensation of aural fullness, and tinnitus. Tinnitus and hearing loss may persist between attacks. Hearing loss is usually unilateral, at least in the early stages, and fluctuant, but it typically develops into a permanent sensorineural hearing loss. Many patients report increased sensitivity to loud noises (recruitment) in addition to the listed symptoms. Word recognition is frequently poorer than predicted from pure-tone audiogram.
Onset for approximately one half of patients occurs when aged 40–60 years. Meniere disease is rare in children.
References- American National Standards Institute. Maximum permissible ambient noise levels for audiometric test rooms. ANSI/ASA S3. 1–1999 (R2008).
- Frank T, Petersen DR. Accuracy of a 40 dB HL audioscope and audiometer screening for adults. Ear Hear. 1987;8(3):180–183.
- Bogardus ST Jr, Yueh B, Shekelle PG. Screening and management of adult hearing loss in primary care: clinical applications. JAMA. 2003;289(15):1986–1990.
- Fausti SA, Wilmington DJ, Helt PV, Helt WJ, Konrad-Martin D. Hearing health and care: the need for improved hearing loss prevention and hearing conservation practices. J Rehabil Res Dev. 2005;42(4 Suppl 2):45–62.
- Harrell RW. Pure tone evaluation. In: Katz J, ed. Handbook of Clinical Audiology. 5th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2002:71–87.
- Forzley GJ. Audiometry. In: Pfenninger JL, Fowler GC, eds. Pfenninger & Fowler’s Procedures for Primary Care. 2nd ed. St. Louis, Mo.: Mosby; 2003:409–415.
- Brenner LA, Ivins BJ, Schwab K, et al. Traumatic brain injury, posttraumatic stress disorder, and postconcussive symptom reporting among troops returning from Iraq. J Head Trauma Rehabil. 2010;25(5):307–312.
- Jupiter T. Screening for hearing loss in the elderly using distortion product otoacoustic emissions, pure tones, and a self-assessment tool. Am J Audiol. 2009;18(2):99–107.
- Audiometry Screening and Interpretation. Am Fam Physician. 2013 Jan 1;87(1):41-47. https://www.aafp.org/afp/2013/0101/p41.html
- Katz J, Lezynski J. Clinical masking. In: Katz J, ed. Handbook of Clinical Audiology. 5th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins; 2002:124–141.
- Saliba I, Martineau G, Chagnon M. Asymmetric hearing loss: rule 3,000 for screening vestibular schwannoma. Otol Neurotol. 2009;30(4):515–521.
- Northern JL, Downs MP. Hearing in Children. 4th ed. Baltimore, Md: Lippincott Williams & Wilkins; 1991.
- Occupational Safety and Health Administration. Section III: Chapter 5 https://www.osha.gov/dts/osta/otm/new_noise