What is purulent drainage
Purulent drainage is thick with a yellow, green or brown color, with a pungent, strong, foul, fecal or musty odor liquid or discharge that oozes from a wound. Purulent drainage is a sign of an unhealthy wound and demands treatment. An infected wound may be characterized by increased or sustained pain, redness or swelling, pus discharge, bad odor or non-healing of the wound.
Purulent drainage is easily spotted, as it is thick, and can vary in color from grayish or yellow to green and even brown. Purulent drainage is usually considered a sign of infection.
Purulent wound drainage changes color and thickens because of the number of living and dead germ cells within it, as well as white blood cells in the area. Purulent drainage will often increase as the infection worsens.
With most wounds, a small amount of thin, pale colored exudate is normal. As all wounds are contaminated, with or without necrotic tissue, they will have an odor. Bacteria of different varieties have varying odors, colors and consistencies, and dead tissue in a wound introduces additional bacteria to the affected area. An increase in amount or consistency of exudate along with a change in color signals a cause for concern, as well as changes in odor.
Skin and wound infections interfere with the healing process and can create additional tissue damage. They can affect anyone, but people with underlying conditions are at risk of slower wound healing and greater risk of wound infections. Examples of conditions that increase the risk of wound infections include:
Characteristics of the individual
- Poor blood circulation
- Diabetes
- Weakened/Immune system disorders (e.g., HIV/AIDS, organ transplant recipient, malignancy)
- Low mobility or immobility (e.g., confined to bed, paralysis)
- Malnutrition
- Prior surgeryn
- Radiation therapy or chemotherapyn
- Conditions associated with hypoxia and/or poor tissue perfusion (e.g. anemia, cardiac or respiratory disease, arterial or vascular disease, renal impairment, rheumatoid arthritis, shock)
- Inappropriate antibiotic prophylaxis, particularly in acute wounding
- Alcohol, smoking and drug abuse
Characteristics of the wound
- Acute wounds:
- Contaminated or dirty wounds
- Trauma with delayed treatment
- Pre-existing infection or sepsis
- Spillage from gastro-intestinal tract
- Penetrating wounds over 4 hours
- Inappropriate hair removal
- Operative factors (e.g. long surgical procedure, hypothermia, blood transfusion)
- Chronic wounds:
- Degree of chronicity/duration of wound
- Large wound area
- Deep wound
- Anatomically located near a site of potential contamination (e.g. perineum or sacrum)
- Both wound types:
- Foreign body (e.g. drains, sutures)
- Hematoma
- Necrotic wound tissue
- Impaired tissue perfusion
- Increased exudate or moisture
Characteristics of the environment
- Hospitalization (due to increased risk of exposure to antibiotic resistant organisms)
- Poor hand hygiene and aseptic technique
- Unhygienic environment (e.g. dust, unclean surfaces, mold/mildew in bathrooms)
- Inadequate management of moisture, exudate and edema
- Inadequate pressure off-loading
- Repeated trauma (e.g. inappropriate dressing removal technique)
When infections penetrate deep into the body into tissues such as bone, or when they occur in tissue that has inadequate circulation, they can become difficult to treat and may become chronic infections.
Purulent wound drainage causes
Most cases of infected wounds are caused by bacteria, originating either from the skin, other parts of the body or the outside environment. The skin contains bacteria (normal flora) which are normally harmless if the skin is intact. However, the protective barrier formed by the skin is disrupted when there is a wound, and these normal flora are able to colonize the injured area. This results in further tissue damage and may prolong wound healing by promoting more inflammation, which prolongs the process of wound healing.
The most common bacteria causing wound infection is Staphylococcus aureus and other groups of staphylococci. Contamination from other parts of the body may also cause wound infection. Poor wound dressing techniques and unhygienic conditions may increase the risk for wound infection.
The relationship between the host, the wound and microorganisms in the development of wound infection has been well described in the literature. However, the concept of wound microbial balance and the progression from a state of wound contamination to systemic infection is yet to be established fully.
Purulent wound drainage signs and symptoms
Contamination
Wound contamination is the presence of non-proliferating microbes within a wound at a level that does not evoke a host response. All wounds may acquire micro-organisms. If suitable nutritive and physical conditions are not available for each microbial species, or they are not able to successfully evade host defences, they will not multiply or persist; their presence is therefore only transient and wound healing is not delayed.
Virtually from the time of wounding, all open wounds are contaminated with microbes. Chronic wounds become contaminated from endogenous secretions (i.e. natural flora) and exogenous microbial sources, including poor hand hygiene practised by healthcare clinicians and environmental exposure. Unless compromised, the host defences respond swiftly to destroy bacteria through a process called phagocytosis.
Colonization
Colonization refers to the presence within the wound of microbial organisms that undergo limited proliferation, but do not cause damage to the host or initiate wound infection. Microbial growth occurs at a non-critical level, and wound healing is not impeded or delayed. Sources for microorganisms may be natural flora, exogenous sources or as a result of environmental exposure.
Local infection
Wound infection occurs when bacteria or other microbes move deeper into the wound tissue and proliferate at a rate that invokes a response in the host. Local infection is contained in one location, system or structure. Especially in chronic wounds, local wound infection often presents as subtle signs that can be considered covert signs of infection that may develop into the classic, overt signs of infection.
Local infection signs and symptoms:
- Covert (subtle) signs of local infection:
- Hypergranulation (excessive ‘vascular’ tissue)
- Bleeding, friable granulation
- Epithelial bridging and pocketing in granulation tissue
- Wound breakdown and enlargement
- Delayed wound healing beyond expectations
- New or increasing pain
- Increasing malodor
- Overt (classic) signs of local infection:
- Erythema
- Local warmth
- Swelling
- Purulent discharge
- Delayed wound healing beyond expectations
- New or increasing pain
- Increasing malodor
Spreading infection
Spreading infection describes the invasion of the surrounding tissue by infective organisms that have spread from a wound. Microorganisms proliferate and spread, to a degree that signs and symptoms extend beyond the wound border. Spreading infection may involve deep tissue, muscle, fascia, organs or body cavities.
Spreading infection signs and symptoms:
- Extending in duration +/- erythema
- Lymphangitis
- Crepitus
- Wound breakdown/dehiscence with or without satellite lesions
- Malaise/lethargy or non-specific general deterioration
- Loss of appetite
- Inflammation, swelling of lymph glands
Systemic infection
Systemic infection from a wound affects the body as a whole, with microorganisms spreading throughout the body via the vascular or lymphatic systems. Systemic inflammatory response, sepsis and organ dysfunction are signs of systemic infection.
Systemic infection include:
- Severe sepsis
- Septic shock
- Organ failure
- Death
Purulent wound drainage complications
Infected wounds can have serious local and systemic complications. The most serious local complication of infected wounds is a non-healing wound, which results in significant pain and discomfort for the patient. The infection can also affect the surrounding tissues and may cause a bacterial skin infection (cellulitis) or an acute or chronic bacterial bone infection (osteomyelitis). If the infection spreads to the blood vessels, the bacteria may spread and cause infection in other areas of the body (sepsis or septicemia). Systemic infection from a wound affects the body as a whole, with microorganisms spreading throughout the body via the vascular or lymphatic systems. Systemic inflammatory response, sepsis and organ dysfunction are signs of systemic infection.
Purulent wound drainage diagnosis
Many minor and superficial skin and wound infections are diagnosed by a healthcare practitioner based on a physical examination, signs and symptoms, and experience. A clinical evaluation cannot, however, definitively tell the healthcare practitioner which microbe is causing a wound infection or what treatment is likely to be effective. For that, laboratory testing is required.
Laboratory tests
Examples of common tests include:
- Bacterial culture – This is the primary test used to diagnose a bacterial infection. Results are usually available within 24-48 hours.
- Gram stain – This is usually performed in conjunction with the wound culture. It is a special staining procedure that allows bacteria to be evaluated under the microscope. The results are usually available the same day and provide preliminary information about the microbe that may be causing the infection.
- Antimicrobial susceptibility – A follow-up test to a positive wound culture, this is used to determine the bacteria’s likely susceptibility to certain drugs and helps the healthcare practitioner select appropriate antibiotics for treatment. Results are typically available in about 24 hours. This testing can identify resistant bacteria such as methicillin-resistant Staphylococcus aureus (MRSA).
Purulent drainage treatment
Effective wound management requires holistic assessment of the individual, their wound and the wound care environment to promote host defence and response to infection. For individuals with significant and life-threatening infection (e.g. sepsis), admission to a higher level of monitoring/care and with immediate resuscitation with fluids, oxygen and antibiotics is imperative.
Effective wound infection management
Optimize individual host response:
- Optimize management of comorbidities (e.g. diabetes, tissue perfusion/oxygenation)
- Minimize or eliminate risk factors that increase infection risk where feasible
- Optimize nutritional status and hydration
- Assess and manage other anatomical sites of infection (e.g. urinary tract, chest)
- Treat systemic symptoms (e.g. pain, pyrexia)
- Promote psychosocial support
- Provide appropriate systemic antimicrobial therapy
- Ensure the individual is engaged in development of an personalized management plan
- Promote education by the interdisciplinary wound management team to the individual and their caregivers
Reduce wound microbial load
- Prevent cross infection by implementing universal precautions and aseptic technique
- Facilitate wound drainage
- Ensure peri-wound hygiene and protection
- Manage wound exudate
- Optimize the wound bed:
- Remove necrotic tissue, debris, foreign bodies, wound dressing remnants and slough
- Disrupt biofilm by debriding
- Cleanse the wound with each dressing change
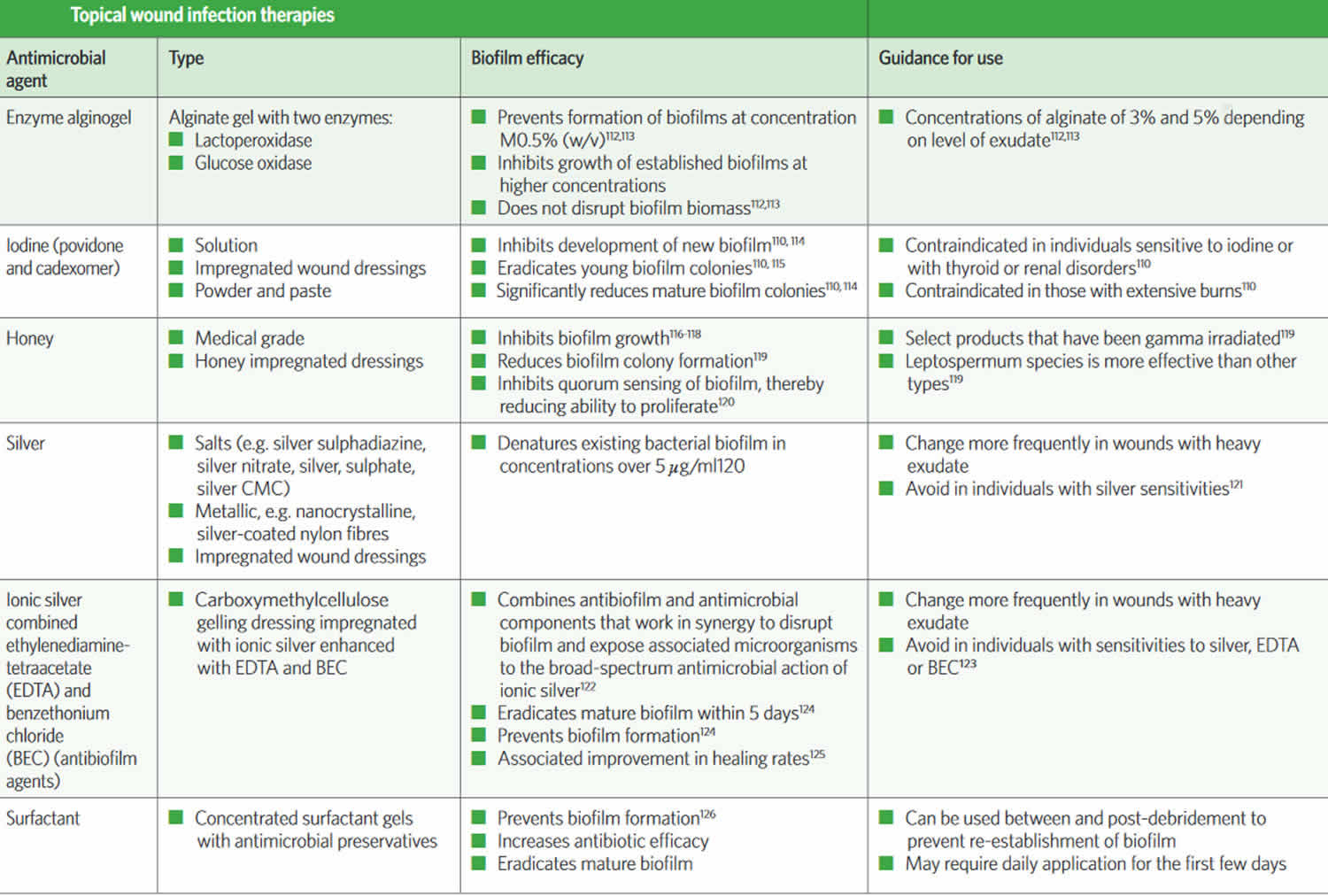
- Use appropriate dressings to manage exudate – a dressing containing an antimicrobial may be considered
- If deemed necessary, consider an appropriate topical antiseptic for a short period for time (e.g. 2 weeks)
Promote environmental and general measures
- Perform wound care in a clean environment
- Determine that the appropriate aseptic technique required is based on risk assessment of the patient, the wound and the environment
- Store equipment and supplies appropriately
- Provide education for the individual and their caregivers
- Regularly review local policies and procedures
The risk of wound infection can be minimized with prompt and proper wound cleansing and treatment. The primary factor that needs to be addressed in wound infections is proper wound care. A wound requires a moist (not wet) environment for proper functioning of the cells responsible for wound healing. It is recommended that dressings should be changed daily (or more often), and that proper precautions (washing hands prior to dressing the wound, sterilized equipment, etc.) during wound dressing be taken in order to minimize the risk of further infection. A number of advanced dressings, which are currently available, require less frequent dressing changes and may provide the added benefit of faster wound healing.
Many superficial bacterial infections and viral infections will resolve on their own without treatment. Other bacterial infections may require only a topical antimicrobial, and some cases require incision and drainage.
The use of antibiotics, whether applied directly to the wound (topical) or taken orally (systemic), should only be given under the direction of a physician. In some cases of severe infection, intravenous antibiotics may be given to combat severe blood infection (sepsis).
Deeper infections, and those that are persistent, typically require antibiotics. The choice is based upon the results of wound culture and antimicrobial susceptibility tests. People with antibiotic-resistant bacteria or with an infection in a location that is difficult for drug therapy to penetrate (such as bone) may require extended treatment and/or treatment with intravenous (IV) medications.
Wounds may also require removal of dead tissue (debridement) and/or drainage, sometimes more than once. Topical antimicrobials and debridement are also used for burn treatment. With extensive injuries, grafting and other surgeries may be required.
Treatment plans can be affected by the presence of underlying conditions that can slow wound healing, such as diabetes, malnutrition, HIV/AIDS, and other disorders that compromise the immune system. A healthcare practitioner may need to perform tests to detect these underlying conditions.
Optimizing host response
Measures to optimize the host response attempt to maximize healing potential by enhancing the ability of the individual to resist infection. This includes addressing systemic and/or intrinsic factors that may have contributed to the development of the wound infection (e.g. optimization of glycemic control and the use of disease-modifying drugs in rheumatoid arthritis). Factors that contribute to wound infection are often the same factors that contributed to the development of the initial wound. Local moisture management, pressure offloading and edema control are recognized as important interventions for maximizing the wound healing environment and decreasing biofilm nutrition.
Infection control in wound care
To prevent further contamination and cross infection, it is important to maintain an aseptic non-touch technique when managing the wound. Performing the aseptic technique during relevant clinical procedures (e.g. changing the wound dressing) protects the individual by reducing exposure to pathogenic microorganisms. Aseptic technique also reduces the risk of cross infection.
A risk assessment should be conducted prior to performing wound management procedures. If it is necessary to touch any area of the wound directly, sterile gloves and equipment are required. Asepsis is supported by standard precautions, including:
- Practising regular and effective hand hygiene
- Appropriate use of sterile and non-sterile gloves
- Use of personal protective equipment (e.g. mask and gown)
- Conducting wound care in a clean environment
- Strategic sequencing of care
- Sharps management
- Environmental controls.
Cleansing infected wounds
Infected wounds should be cleansed thoroughly at each wound dressing change. There is a difference between rinsing a wound and cleansing a wound. Therapeutic wound cleansing exhibits the following characteristics:
- Application of a cleansing solution that has potential to disrupt biofilm and kill planktonic bacteria and other organisms
- Promotion of safety of the wound and the individual
- Availability in a variety of settings (hospital, clinic and home environment)
- Irrigation that is performed at an appropriate pound per square inch pressure
- The periwound being maintained and protected from maceration.
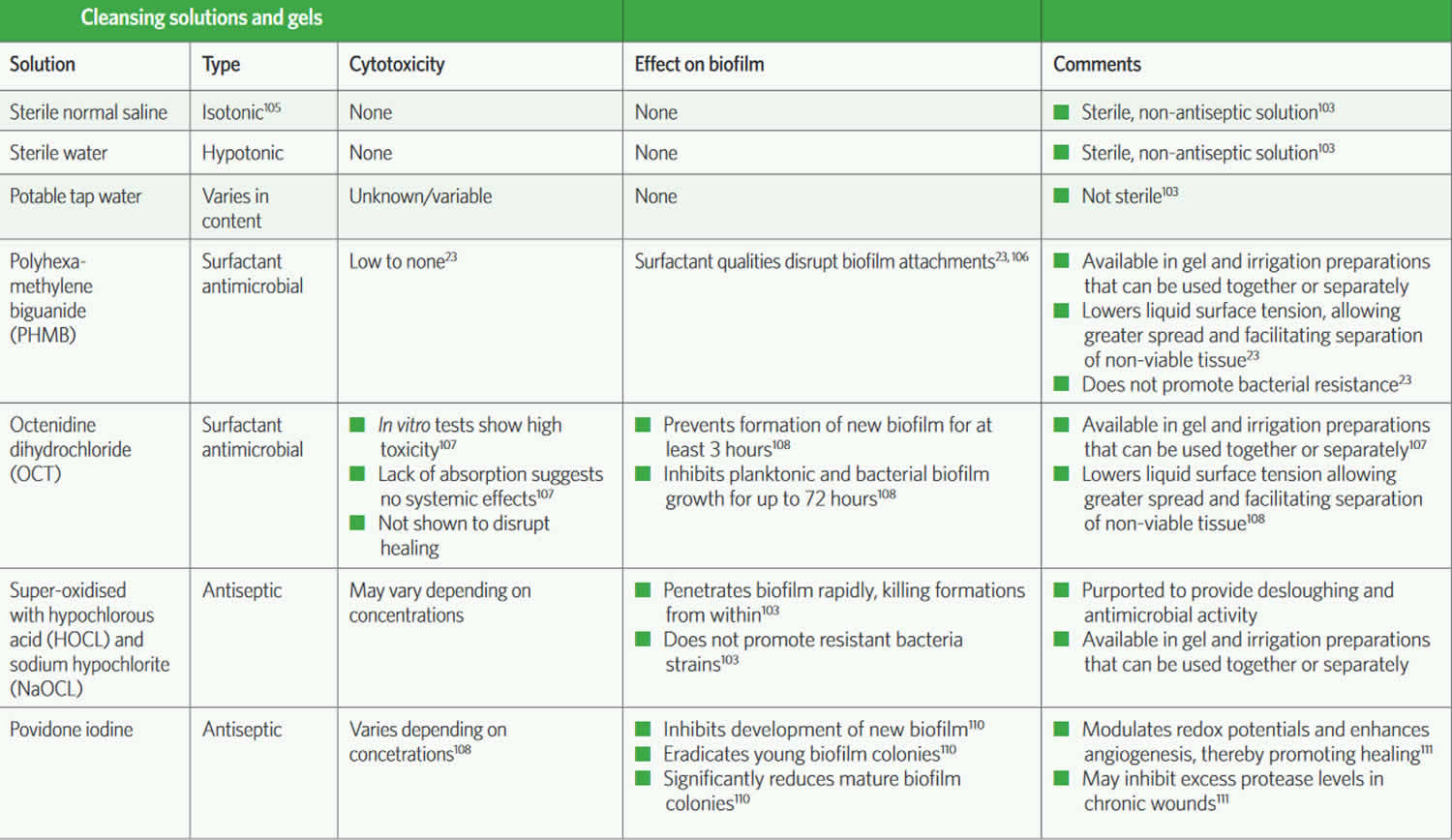
The ideal cleansing agent and the optimal method of wound cleansing has not been established conclusively. There may be a role for judicious irrigation with an antiseptic solution.
Surfactants lower the surface tension between the wound bed and the liquid (or between two liquids), thereby promoting spread of the liquid across the wound bed and facilitating separation of loose, non-viable tissue. This characteristic has been capitalised on in the development of several surfactants that are combined with antimicrobials (e.g. polyhexamethylene biguanide [PMHB] and undecylenamidopropyl betaine; octenidine dihydrochloride and phenoxyethanol; and octenidine and ethylhethylglycerin). The use of these surfactant-containing antimicrobial cleansers or antimicrobial preservative-containing cleansers is useful for disrupting biofilm in the wound.
There are also newer cleansing agents that are super-oxidised and/or have lower concentrations of hypochlorous acid and sodium hypochlorite compared with traditional highly toxic preparations that are no longer recommended. These newer solutions are purported to disrupt biofilm and kill planktonic bacteria and other organisms while being safe for the wound and the individual.
Table 1. Cleansing solutions and gels
Table 2. Topical wound infection therapies