Renin activity
Renin is an enzyme that controls aldosterone production. Renin converts angiotensinogen to inactive angiotensin 1 1. Angiotensin 1 then is converted to the active octapeptide angiotensin 2 in the lungs and kidneys by angiotensin converting enzymes (ACE). Angiotensin 2 is a potent vasopressor responsible for hypertension of renal origin. Angiotensin 2 also stimulates the zona glomerulosa of the adrenal cortex to release aldosterone. Angiotensin 2 is an octapeptide that is activated by type-1 G protein-coupled angiotensin 2 receptors. These receptors have different functions depending on the types of cells that contain the receptor. However, it has five primary functions that include: increasing aldosterone, increasing sodium-hydrogen exchange within the proximal renal tubule, increasing thirst drive within the hypothalamus, increasing antidiuretic hormone, and acting on G protein-coupled receptors that activate IP3/Ca2+ second messenger systems within arterioles to cause vasoconstriction. Aldosterone then undergoes its actions within the kidney. Aldosterone is a hormone that plays an important role in maintaining normal sodium and potassium concentrations in blood and in controlling blood volume and blood pressure.
Renin is enzymes released by the juxtaglomerular apparatus of the kidneys into the renal vein in response to:
- Hyperkalemia (increased potassium).
- Sodium depletion (low sodium).
- Hypovolemia (low plasma volume).
- Decreased kidney blood perfusion (low blood pressure).
Renin release is suppressed when there is:
- Loss of potassium.
- Increased blood volume.
- An acute increase in blood pressure.
Angiotensin 1 is converted to angiotensin 2 in the lung where there is an abundance of the angiotensin-converting enzyme (ACE).
- Angiotensin 2 is the potent vasopressor agent responsible for the renal type of hypertension.
- Angiotensin 2 also release aldosterone from the adrenal cortex.
- Angiotensin 2 + aldosterone both leads to :
- Hypertension.
- Increase in the blood volume.
- Serum sodium.
The renin + aldosterone regulate:
- Sodium and potassium balance.
- Blood pressure.
- Blood volume.
The release of aldosterone from the adrenal glands is regulated via the renin-angiotensin 2-aldosterone system. This system is initially activated via a decrease in the mean arterial blood pressure to increase the blood pressure. The decrease in blood pressure is initially sensed within the afferent arterioles of the kidney. Prorenin is then released by mechanoreceptors and is converted to renin by the juxtaglomerular cells (JG cells). The renal juxtaglomerular cells can also release renin after sympathetic stimulation of their beta one receptor.
The kidneys release renin when there is a drop in glomerular blood pressure or a decrease in sodium concentration at the macula densa at the distal tubules in the kidney or by stimulation of sympathetic outflow to the kidney, such as in renal vascular diseases 1. Renin cleaves the blood protein angiotensinogen to form angiotensin 1, which is then converted by a second enzyme to angiotensin 2. Angiotensin 2 causes blood vessels to constrict, and it stimulates aldosterone production. Overall, this raises blood pressure and keeps sodium and potassium at normal levels.
A variety of conditions can lead to aldosterone overproduction (hyperaldosteronism, usually just called aldosteronism) or underproduction (hypoaldosteronism). Since renin and aldosterone are so closely related, both substances are often tested together to identify the cause of an abnormal aldosterone.
The most common test to assess disturbances of the aldosterone pathway is the aldosterone: renin ratio. This determines whether there is an isolated aldosterone problem or there is a disturbance within renin angiotensin system. If an aldosterone problem is suspected, and the results show no elevation in either aldosterone or renin, then congenital adrenal hyperplasia is suspected. If both aldosterone and renin are increased, and their ratio is less than 10, then the differential includes renovascular hypertension. If the renin value is normal, the aldosterone level is elevated, and the ratio is greater than 30, the differential includes Conns syndrome. This can be confirmed with a salt suppression test, an MRI of the adrenal glands, and adrenal vein sampling.
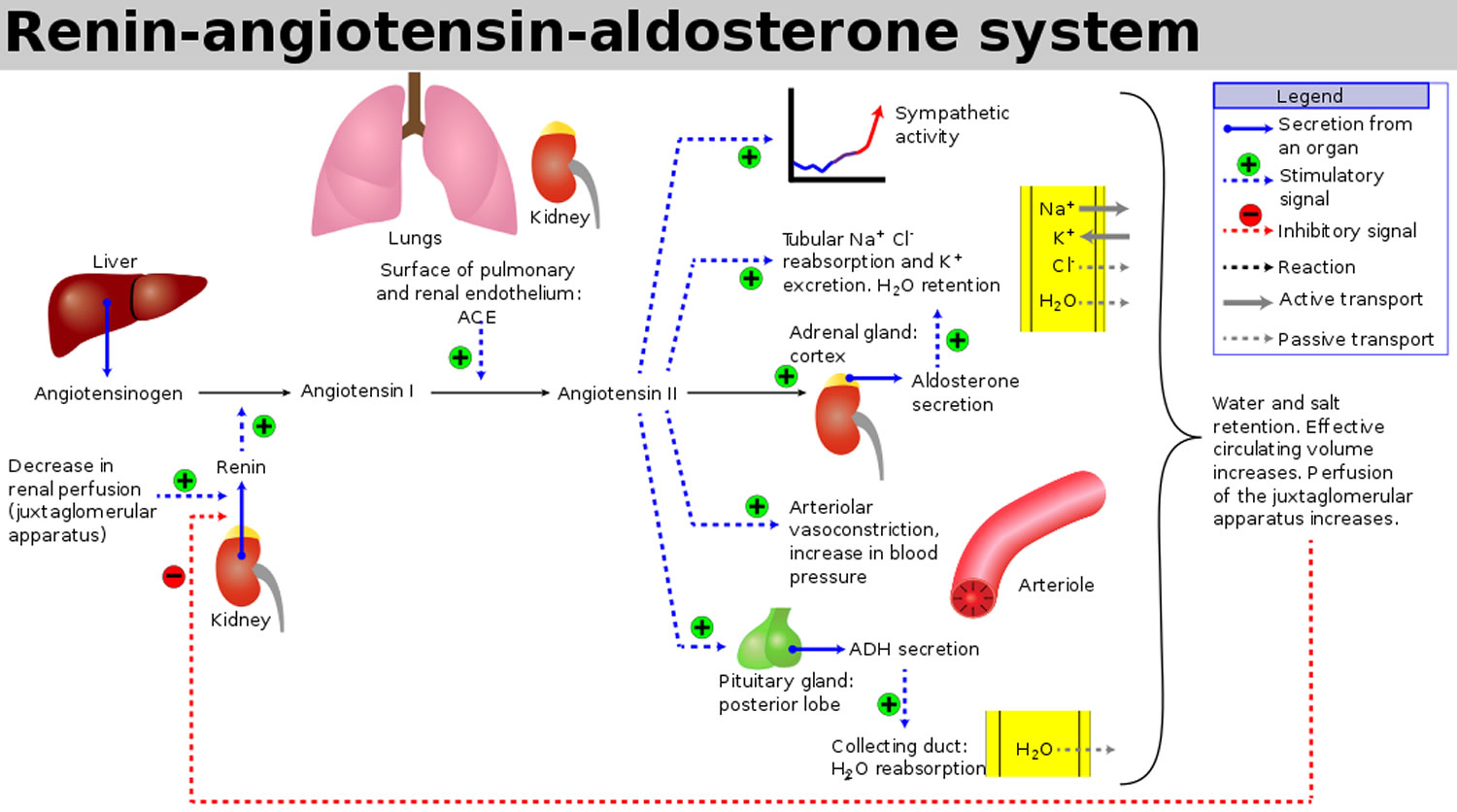
Figure 1. Renin angiotensin aldosterone system
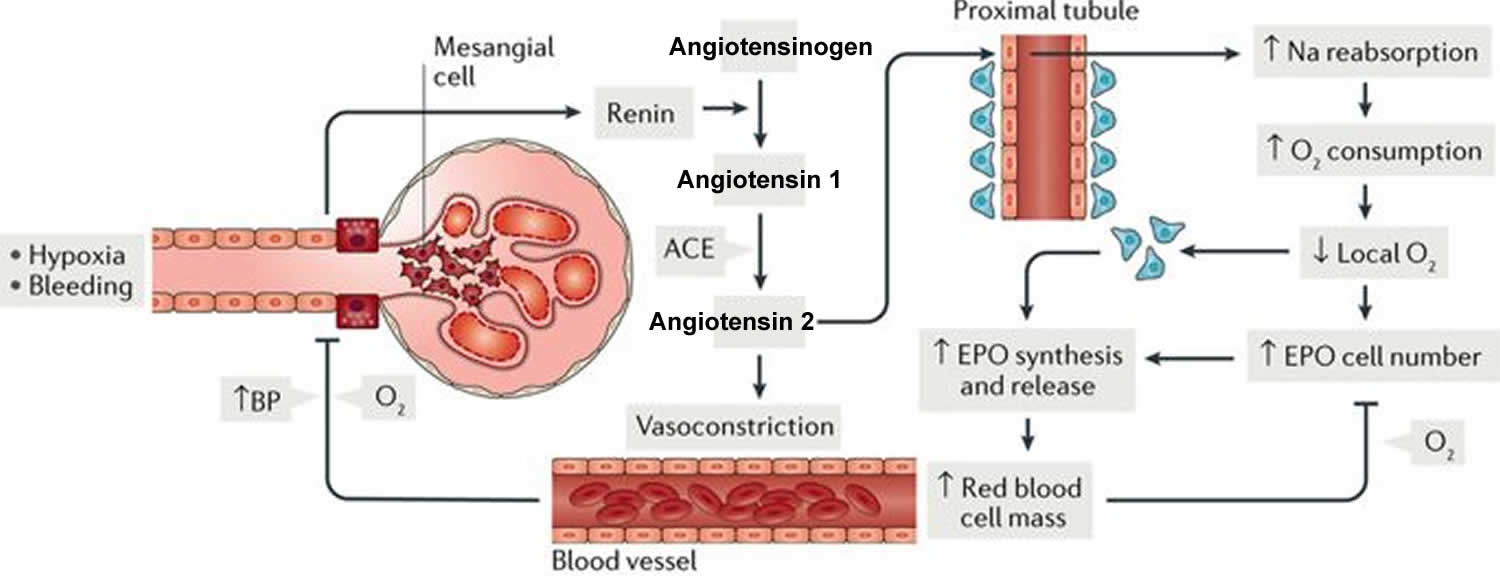
Figure 2. Renin angiotensin aldosterone system mechanism of action
Plasma renin activity test
Plasma renin activity test are used to investigate causes of primary aldosteronism (eg, adrenal adenoma/carcinoma and adrenal cortical hyperplasia) and secondary aldosteronism (renovascular disease, salt depletion, potassium loading, cardiac failure with ascites, pregnancy, Bartter syndrome)
Aldosterone and renin tests are used to evaluate whether the adrenal glands are producing appropriate amounts of aldosterone and to distinguish between the potential causes of excess or deficiency. Aldosterone may be measured in the blood or in a 24-hour urine sample, which measures the amount of aldosterone removed in the urine in a day. Renin is always measured in blood.
These tests are most useful in testing for primary aldosteronism, also known as Conn syndrome, which causes high blood pressure. If the test is positive, aldosterone production may be further evaluated with stimulation and suppression testing.
Both aldosterone and renin levels are highest in the morning and vary throughout the day. They are affected by the body’s position, by stress, and by a variety of prescribed medications.
A blood sample is drawn by needle from a vein in the arm to measure blood aldosterone and/or renin. Some healthcare practitioners prefer 24-hour urine collection for aldosterone since blood aldosterone levels vary throughout the day and are affected by position. In some cases, blood is collected from the renal (for renin) or adrenal (for aldosterone) veins by insertion of a catheter; this is done in the hospital at major medical centers by a specially trained radiologist.
For a blood aldosterone and renin measurement, the healthcare practitioner may ask you to be upright or lying down for a period of time (e.g., 15-30 minutes) prior to sample collection. You may also be instructed to avoid certain beverages, foods, or medications before the test. Follow any instructions you are given.
What is Bartter syndrome?
Bartter syndrome is a group of rare congenital disorders that affect the kidney’s ability to reabsorb sodium. People with Bartter syndrome lose too much sodium through the urine. This causes a rise in the level of the aldosterone and makes the kidneys remove too much potassium from the body. The syndrome is therefore associated with high levels of renin and aldosterone in the blood, increased blood pH (alkalosis), and high levels of potassium, calcium, and chloride in the urine.
The syndrome, which is usually diagnosed in early childhood, can be caused by mutations in at least one of five genes, and genetic testing can confirm a diagnosis. There are different types of Bartter syndrome, defined based upon which gene is the cause of the condition.
Signs and symptoms will vary depending on the type of Bartter syndrome. The antenatal form (appears before birth) can be life-threatening. The classical form found in infants and young children usually causes failure to thrive, constipation, muscle cramping and weakness as well as dehydration, increased urine production, and weakened bones.
The condition cannot be cured, but a few treatments are available, such as keeping an affected person’s blood potassium from being abnormally low through a potassium-rich diet or by taking supplements. While, with treatment, prognosis is good, those affected must be careful to maintain fluid and electrolyte balance. Kidney failure is a possible complication of Bartter syndrome.
Normal renin levels in blood
Normal plasma renin levels 2:
- 0-2 years: 4.6 ng/mL/hour (mean) Range: 1.4-7.8 ng/mL/hour
- 3-5 years: 2.5 ng/mL/hour (mean) Range: 1.5-3.5 ng/mL/hour
- 6-8 years: 1.4 ng/mL/hour (mean) Range: 0.8-2.0 ng/mL/hour
- 9-11 years: 1.9 ng/mL/hour (mean) Range: 0.9-2.9 ng/mL/hour
- 12-17 years: 1.8 ng/mL/hour (mean) Range: 1.2-2.4 ng/mL/hour
Mean data not standardized as to time of day or diet. Infants were supine, children sitting.
Sodium-depleted, upright (peripheral vein specimen)
- 18-39 years: 10.8 ng/mL/hour (mean)
- 2.9-24.0 ng/mL/hour (range)
- > or =40 years: 5.9 ng/mL/hour (mean)
- 2.9-10.8 ng/mL/hour (range)
Sodium-replete, upright (peripheral vein specimen)
- 18-39 years: 1.9 ng/mL/hour (mean)
- < or =0.6-4.3 ng/mL/hour (range)
- > or =40 years: 1.0 ng/mL/hour (mean)
- < or =0.6-3.0 ng/mL/hour (range).
The amount of salt in your diet and medications, such as over-the-counter pain relievers of the non-steroid class, diuretics, beta blockers, steroids, angiotensin-converting enzyme (ACE) inhibitors, and oral contraceptives can affect the test results. Some of these drugs are used to treat high blood pressure. Stress, exercise, and pregnancy can also affect the test results. Your healthcare provider will tell you if you should change the amount of sodium (salt) you ingest in your diet, your use of diuretics or other medications, or your exercise routine before aldosterone testing.
Licorice may mimic aldosterone properties and should be avoided for at least two weeks before the test because it can decrease aldosterone results. This refers only to the actual products of the licorice plant (hard licorice); most soft licorice and other forms of licorice sold in North America do not actually contain licorice. Check the package label if you are uncertain, or bring a package with you to ask the healthcare practitioner.
Aldosterone levels become very low with severe illness, so testing should not be done at times when someone is very ill.
When is renin activity test and aldosterone test ordered?
A blood aldosterone test and a renin test are usually ordered together when someone has high blood pressure, especially if the person also has low potassium. Even if potassium is normal, testing may be done if typical medications do not control the high blood pressure or if hypertension develops at an early age. Primary aldosteronism is a potentially curable form of hypertension, so it is important to detect and treat it properly.
Aldosterone and renin tests are used to evaluate whether the adrenal glands are producing appropriate amounts of aldosterone and to distinguish between the potential causes of excess or deficiency. Aldosterone may be measured in the blood or in a 24-hour urine sample, which measures the amount of aldosterone removed in the urine in a day. Renin is always measured in blood.
Both aldosterone and renin levels are highest in the morning and vary throughout the day. They are affected by the body’s position, by stress, and by a variety of prescribed medications. Late p.m. levels can be up to 30% lower than early a.m. levels. Supine values are on average 50% lower than upright collections. Sodium deplete subjects have significantly elevated serum aldosterone levels, potentially exceeding the upper limit of the salt replete upright reference range by several fold. To account for these variables, at least in part, it is recommended that plasma renin activity is measured concomitantly. In situations of physiological variability, Plasma renin activity should be altered in the same direction as aldosterone.
Normal aldosterone level
- Age 0-30 days: 17-154 ng/dL
- Age 31 days-11 months: 6.5-86 ng/dL
- Age 1-10 years:
- Age < or =40 ng/dL (supine)
- Age < or =124 ng/dL (upright)
- Age > or =11 years: < or =21 ng/dL (a.m. peripheral vein specimen)
An serum aldosterone/plasma renin activity ratio is a screening test to detect primary aldosteronism in high-risk, hypertensive individuals. To determine the ratio, blood levels of aldosterone and renin are measured and a calculation is done by dividing the aldosterone result by the renin result. The serum aldosterone/plasma renin activity ratio is considered the most reliable screening for primary aldosteronism, though it is not straightforward to interpret. Anything that could interfere with the test, such as medications, posture, sodium intake, and plasma potassium, needs to be taken into account before the test to avoid false positives or false negatives. Other tests, like suppression tests, are used to confirm the diagnosis after screening.
A high ratio of serum aldosterone in ng/dL to plasma renin activity in ng/mL per hour, is a positive screening test result, a finding that warrants further testing. A serum aldosterone:plasma renin activity ratio > or =20 and serum aldosterone of > or =15 ng/dL indicates probable primary aldosteronism.
Note that angiotensin converting enzyme (ACE) inhibitors have the potential to “falsely elevate” plasma renin activity. Therefore, in a patient treated with an ACE-inhibitor, the findings of a detectable plasma renin activity level or a low serum aldosterone:plasma renin activity ratio do not exclude the diagnosis of primary aldosteronism. In addition, a strong predictor for primary aldosteronism is a plasma renin activity level undetectably low in a patient taking an ACE-inhibitor.
Renal disease, such as unilateral renal artery stenosis, results in elevated renin and aldosterone levels. Renal venous catheterization may be helpful. A positive test is a renal venous renin ratio (affected:normal) above 1.5.
Aldosterone levels are occasionally ordered, along with other tests, when a healthcare practitioner suspects that someone has adrenal insufficiency or Addison disease. One of those tests, the aldosterone stimulation test, also called adrenocorticotropic hormone (ACTH) stimulation, tests aldosterone and cortisol to determine if someone has Addison disease, low pituitary function, or a pituitary tumor. A normal result is a cortisol increase and an increase in aldosterone after stimulation by ACTH (adrenocorticotropic hormone).
Aldosterone stimulation and suppression tests?
Aldosterone suppression tests are used to confirm a diagnosis of primary aldosteronism. There are a few different types of suppression tests:
- You may be instructed to follow a high-salt diet for three days, then have your aldosterone and sodium in your urine measured.
- You may have a saline (salt) solution administered through a vein (intravenous, IV) and then have your aldosterone level measured.
- You may follow a high-salt diet and be administered a synthetic corticosteroid called fludrocortisone, then have your aldosterone level measured.
In healthy people who are on a high-salt diet or who are administered saline or fludrocortisone, their aldosterone level will be suppressed.
The aldosterone stimulation test, also called ACTH stimulation, tests aldosterone and cortisol to determine if someone has adrenal insufficiency (Addison disease), low pituitary function, or a pituitary tumor. This test involves measuring aldosterone and cortisol before and after an injection of synthetic ACTH. A normal result is an increase in aldosterone and cortisol after stimulation by ACTH.
What does abnormal plasma renin activity test result mean?
The table below indicates the changes in renin, aldosterone, and cortisol that occur with different disorders.
Table 1. The table below indicates the changes in renin, aldosterone, and cortisol that occur with different disorders.
| Disease | Aldosterone | Cortisol | Renin |
|---|---|---|---|
| Primary aldosteronism (Conn syndrome) | High | Normal | Low |
| Secondary aldosteronism | High | Normal | High |
| Adrenal insufficiency (Addison disease) | Low | Low | High |
| Cushing syndrome | Low | High | Low |
Primary aldosteronism (Conn syndrome) is caused by the overproduction of aldosterone by the adrenal glands, usually by a benign tumor of one of the glands. The high aldosterone level increases reabsorption of sodium (salt) and loss of potassium by the kidneys, often resulting in an electrolyte imbalance. Signs and symptoms include high blood pressure, headache, and muscle weakness, especially if potassium levels are very low.
Lower than normal blood potassium (hypokalemia) in someone with hypertension suggests the need to look for aldosteronism. Sometimes, to determine whether only one or both adrenal glands are affected, blood may be taken from both of the adrenal veins and testing is done to determine whether there is a difference in the amount of aldosterone (and sometimes cortisol) produced by each of the adrenal glands.
Secondary aldosteronism, which is more common than primary aldosteronism, is caused by anything that leads to excess aldosterone, other than a disorder of the adrenal glands. It could be caused by any condition that decreases blood flow to the kidneys, decreases blood pressure, or lowers sodium levels. Secondary aldosteronism may be seen with congestive heart failure, cirrhosis of the liver, kidney disease, and toxemia of pregnancy (pre-eclampsia). It is also common in dehydration. In these conditions, the cause of aldosteronism is usually obvious.
The most important cause of secondary aldosteronism is narrowing of the blood vessels that supply the kidney, termed renal artery stenosis. This causes high blood pressure due to high renin and aldosterone and may be cured by surgery or angioplasty. Sometimes, to see if only one kidney is affected, a catheter is inserted through the groin and blood is collected directly from the veins draining the kidney (renal vein renin levels). If the value is significantly higher in one side, this indicates where the narrowing of the artery is present.
Low aldosterone (hypoaldosteronism) usually occurs as part of adrenal insufficiency. It causes dehydration, low blood pressure, a low blood sodium level, and a high potassium level. When infants lack an enzyme needed to make cortisol, a condition called congenital adrenal hyperplasia, this can decrease production of aldosterone in some cases.
Elevated renin levels
Elevated renin level is seen in:
- Secondary aldosteronism with malignant hypertension.
- Chronic renal failure.
- Renovascular hypertension.
- Salt losing status due to GI diseases.
- Renin producing tumor of the kidney.
- Pheochromocytoma.
- Few patients with essential hypertension around 15%.
- Reduced plasma volume due to low sodium.
- Drugs like diuretics.
- Addison disease.
- Cirrhosis.
- Hyperkalemia.
- Hemorrhage.
Low renin levels
Low renin level is seen in:
- Unilateral renal artery stenosis.
- Primary aldosteronism (98%).
- Congenital adrenal hyperplasia with 17- hydroxy deficiency.
- Administration of salt-retaining steroids.
- Scott JH, Dunn RJ. Physiology, Aldosterone. [Updated 2019 May 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470339
- Stalker HP, Holland NH, Kotchen JM, Kotchen TA: Plasma renin activity in healthy children. J Pediatr 1976;89:256-258