What is selegiline
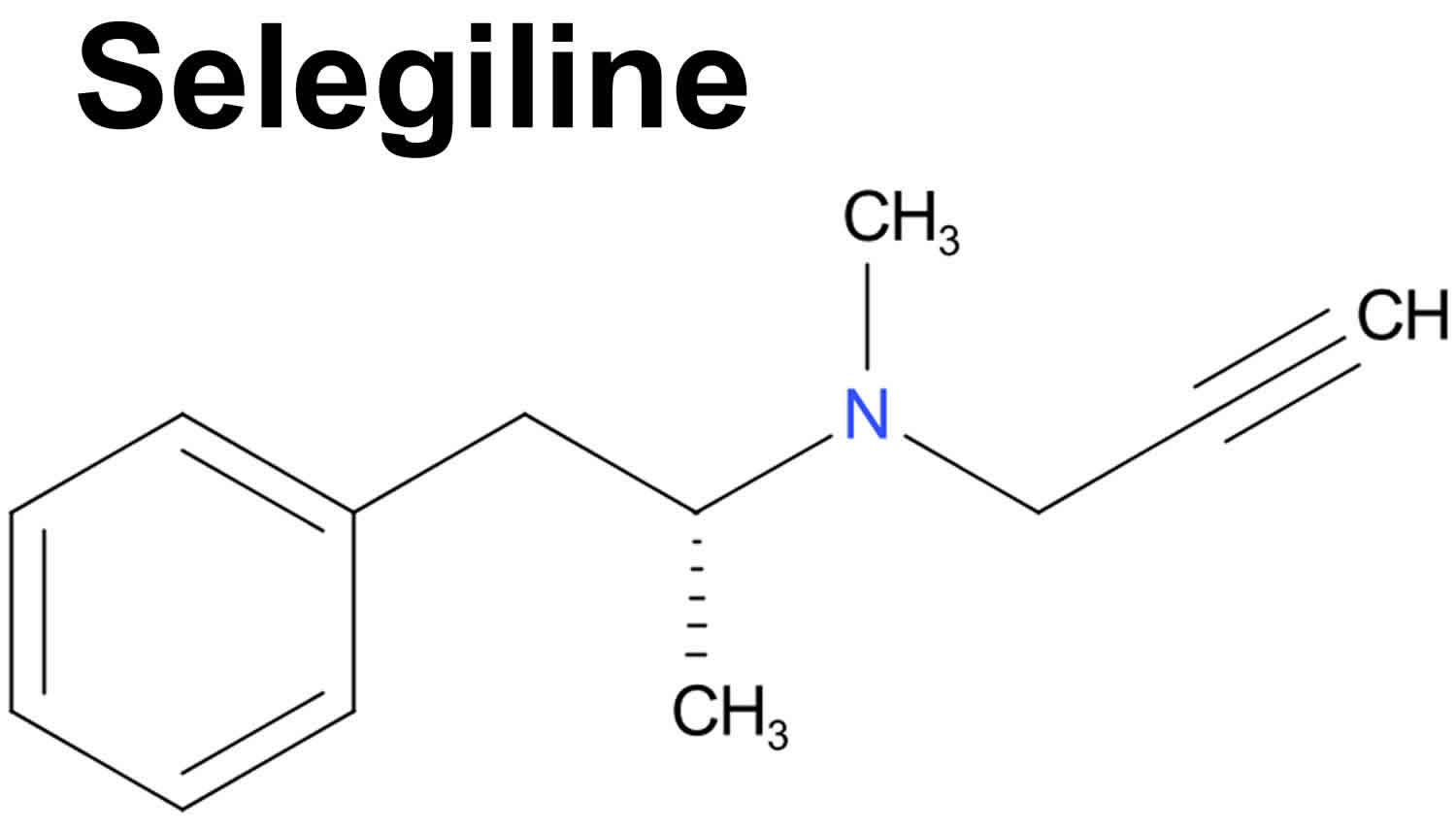
Selegiline is in a group of medications called monoamine oxidase type B (MAO-B) inhibitors. Selegiline prevents the breakdown of a chemical in your brain called dopamine. Selegiline works by increasing the amount of dopamine (a natural substance that is needed to control movement) in the brain. Low levels of dopamine chemical are associated with Parkinson’s disease. Selegiline is used together with with levodopa (L-dopa) or levodopa and carbidopa combination (Sinemet) to treat symptoms of Parkinson’s disease (a disorder of the nervous system that causes difficulties with movement, muscle control, and balance). Selegiline may help people with Parkinson’s disease by decreasing the dose of levodopa/carbidopa needed to control symptoms, stopping the effects of levodopa/carbidopa from wearing off between doses, and increasing the length of time that levodopa/carbidopa will continue to control symptoms.
Selegiline may help to control the symptoms of Parkinson’s disease, but it will not cure Parkinson’s disease. Do not stop taking selegiline without talking with your doctor. If you suddenly stop taking medications for Parkinson’s disease such as selegiline, you may experience fever, sweating, stiff muscles, and loss of consciousness. Call your doctor if you experience these or other unusual symptoms after you stop taking selegiline.
Selegiline is available only with your doctor’s prescription.
Selegiline is available in the following dosage forms:
- Tablet, Disintegrating
- Capsule
- Tablet
Selegiline comes as a capsule and an orally disintegrating (dissolving) tablet to take by mouth. The capsule is usually taken twice a day with breakfast and with lunch. The orally disintegrating tablet is usually taken once a day before breakfast without food, water, or other liquids. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take selegiline exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor. If you take too much selegiline, you may experience a sudden and dangerous increase in your blood pressure.
If you are taking the orally disintegrating tablet, do not remove the blister that contains the tablets from the outer pouch until you are ready to take a dose. When it is time for your dose, remove the blister card from the outer pouch and use dry hands to peel open one blister. Do not try to push the tablet through the foil. Place the tablet on your tongue and wait for it to dissolve. Do not swallow the tablet. Do not eat or drink anything for 5 minutes before you take the tablet and for 5 minutes after you take the tablet.
If you are taking the orally disintegrating tablet, your doctor may start you on a low dose of selegiline and increase your dose after six weeks.
Tell your doctor if you experience nausea, stomach pain, or dizziness. Your doctor may decrease your dose of levodopa/carbidopa during your treatment with selegiline, especially if you experience these symptoms or other unusual symptoms. Follow these directions carefully and ask your doctor or pharmacist if you do not know how much medication you should take. Do not change the doses of any of your medications unless your doctor tells you that you should.
Special precautions
Before taking selegiline:
- tell your doctor and pharmacist if you are allergic to selegiline, or any other medications.
- Do not take selegiline if you have used meperidine (eg, Demerol®) or an MAO inhibitor (MAOI) (eg, isocarboxazid, phenelzine, tranylcypromine, Marplan®, Nardil®, or Parnate®) within the past 14 days. If you do, you may develop agitation, confusion, restlessness, stomach or intestinal symptoms, sudden high body temperature, extremely high blood pressure, or severe convulsions.
- Do not take cyclobenzaprine, dextromethorphan (Robitussin®, Pediacare®), St. John’s wort, or pain medicines (e.g, methadone, propoxyphene, tramadol, Darvon®, Dolophine®, Ultram®) while you are using this medicine. Using these medicines together can cause unwanted effects.
- Selegiline may cause a condition called serotonin syndrome when used together with certain MAO inhibitors (e.g, phenelzine, rasagiline, tranylcypromine) and medicines to treat depression (e.g., amitriptyline, doxepin, fluoxetine, fluvoxamine, nortriptyline, paroxetine, sertraline, Elavil®, Luvox®, Pamelor®, Paxil®, Prozac®, or Zoloft®). Symptoms of serotonin syndrome include: anxiety, restlessness, fast heartbeat, fever, sweating, muscle spasms, twitching, nausea, vomiting, diarrhea, seeing or hearing things that are not there.
- tell your doctor if you are taking, have recently taken, or plan to take any of the following prescription and nonprescription medications: dextromethorphan (Robitussin); meperidine (Demerol); methadone (Dolophine), propoxyphene (Darvon); tramadol (Ultram, in Ultracet); and other medications that contain selegiline (Eldepryl, Emsam, Zelapar). Your doctor may tell you not to take selegiline if you are taking or have recently taken any of these medications. If you stop taking selegiline, your doctor may tell you not to take these medications until at least 14 days have passed since you last took selegiline.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, nutritional supplements, and herbal products you are taking. Be sure to mention any of the following: antidepressants such as amitriptyline (Elavil) and imipramine (Tofranil); carbamazepine (Carbatrol, Equetro); medications for cough and cold symptoms or for weight loss; nafcillin; phenobarbital; phenytoin (Dilantin); selective serotonin reuptake inhibitors such as citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft); and rifampin (Rifadin, Rimactane). Your doctor may need to change the doses of your medications or monitor you more carefully for side effects.
- tell your doctor if you have or have ever had liver or kidney disease.
- if you have phenylketonuria (PKU; an inherited condition in which a special diet must be followed to prevent mental retardation), you should know that the orally disintegrating tablets contain phenylalanine.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while taking selegiline, call your doctor.
- you should know that selegiline may cause dizziness, lightheadedness, and fainting when you get up too quickly from a lying position. This is more common when you first start taking selegiline. To avoid this problem, get out of bed slowly, resting your feet on the floor for a few minutes before standing up.
Drug Interactions
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is not recommended. Your doctor may decide not to treat you with this medication or change some of the other medicines you take.
- Amitriptyline
- Amoxapine
- Amphetamine
- Apraclonidine
- Atomoxetine
- Benzphetamine
- Brimonidine
- Bupropion
- Carbamazepine
- Carbinoxamine
- Citalopram
- Clomipramine
- Codeine
- Cyclobenzaprine
- Cyproheptadine
- Desipramine
- Desvenlafaxine
- Deutetrabenazine
- Dexfenfluramine
- Dexmethylphenidate
- Dextroamphetamine
- Dextromethorphan
- Diethylpropion
- Doxylamine
- Duloxetine
- Ephedrine
- Escitalopram
- Fenfluramine
- Fluoxetine
- Fluvoxamine
- Furazolidone
- Guanadrel
- Guanethidine
- Hydroxytryptophan
- Imipramine
- Iproniazid
- Isocarboxazid
- Isometheptene
- Levomethadyl
- Levomilnacipran
- Linezolid
- Lisdexamfetamine
- Maprotiline
- Mazindol
- Meperidine
- Methamphetamine
- Methotrimeprazine
- Methyldopa
- Methylene Blue
- Methylphenidate
- Milnacipran
- Mirtazapine
- Moclobemide
- Nefopam
- Nialamide
- Nortriptyline
- Opipramol
- Paroxetine
- Phendimetrazine
- Phenelzine
- Phenmetrazine
- Phentermine
- Phenylalanine
- Phenylephrine
- Phenylpropanolamine
- Procarbazine
- Propoxyphene
- Protriptyline
- Pseudoephedrine
- Rasagiline
- Reserpine
- Safinamide
- Sertraline
- Sibutramine
- St John’s Wort
- Sumatriptan
- Tapentadol
- Tetrabenazine
- Tramadol
- Tranylcypromine
- Trazodone
- Trimipramine
- Tryptophan
- Venlafaxine
- Vilazodone
- Vortioxetine
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Alfentanil
- Alizapride
- Amineptine
- Amisulpride
- Amitriptylinoxide
- Atropine
- Benzhydrocodone
- Bromperidol
- Buprenorphine
- Buspirone
- Butorphanol
- Clovoxamine
- Dibenzepin
- Difenoxin
- Dihydrocodeine
- Diphenoxylate
- Dolasetron
- Domperidone
- Dothiepin
- Doxepin
- Droperidol
- Ethchlorvynol
- Femoxetine
- Fentanyl
- Fluspirilene
- Frovatriptan
- Granisetron
- Guarana
- Haloperidol
- Hydrocodone
- Hydromorphone
- Iobenguane I 123
- Iobenguane I 131
- Kava
- Levorphanol
- Licorice
- Lithium
- Lofepramine
- Lorcaserin
- Ma Huang
- Mate
- Melitracen
- Mephentermine
- Metaraminol
- Metaxalone
- Methadone
- Metoclopramide
- Metopimazine
- Midodrine
- Morphine
- Morphine Sulfate Liposome
- Nalbuphine
- Naratriptan
- Nefazodone
- Oxycodone
- Oxymetazoline
- Oxymorphone
- Palonosetron
- Penfluridol
- Pentazocine
- Pimozide
- Reboxetine
- Remifentanil
- Sufentanil
- Sulpiride
- Sultopride
- Tianeptine
- Tiapride
- Tyrosine
- Valbenazine
- Veralipride
- Ziprasidone
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acarbose
- Chlorpropamide
- Desogestrel
- Dienogest
- Dopamine
- Drospirenone
- Estradiol Cypionate
- Estradiol Valerate
- Ethinyl Estradiol
- Ethynodiol Diacetate
- Etonogestrel
- Ginseng
- Glimepiride
- Glipizide
- Glyburide
- Insulin
- Insulin Aspart, Recombinant
- Insulin Bovine
- Insulin Degludec
- Insulin Detemir
- Insulin Glargine, Recombinant
- Insulin Glulisine
- Insulin Lispro, Recombinant
- Levonorgestrel
- Medroxyprogesterone Acetate
- Mestranol
- Metformin
- Nateglinide
- Norelgestromin
- Norethindrone
- Norgestimate
- Norgestrel
- Repaglinide
- Tolazamide
- Tolbutamide
Other Interactions
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following is usually not recommended, but may be unavoidable in some cases. If used together, your doctor may change the dose or how often you use this medicine, or give you special instructions about the use of food, alcohol, or tobacco.
- Avocado
- Bitter Orange
- Tyramine Containing Food
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Dyskinesia (abnormal muscle movements) or
- Hypertension (high blood pressure) or
- Mental illness (eg, psychosis) or
- Postural hypotension (dizziness, lightheadedness, or fainting when getting up from a lying or sitting position)—Use with caution. May make these
- conditions worse.
- Kidney disease, severe—Use is not recommended in patients with this condition.
- Liver disease—Use with caution. Higher blood levels of selegiline may result, and cause an increase in side effects.
- Phenylketonuria (PKU)—The disintegrating tablet contains phenylalanine, which can make this condition worse.
Dietary precautions
When selegiline is taken at doses of 10 mg or less per day for the treatment of Parkinson’s disease, there are no restrictions on food or beverages you eat or drink. However, the chance exists that dangerous reactions, such as sudden high blood pressure, may occur if doses higher than those used for Parkinson’s disease are taken with certain foods, beverages, or other medicines.
While you are using selegiline and for 14 days after you stop, you must not eat tyramine containing foods listed below. Eating these foods while you are using selegiline can raise your blood pressure to dangerous levels.
Tyramine is an amino acid that helps regulate blood pressure. Tyramine occurs naturally in your body and it’s found in certain foods. Monoamine oxidase inhibitors (MAOIs) medicine like selegiline, block an enzyme known as monoamine oxidase, which breaks down excess tyramine in your body. Blocking this enzyme helps relieve depression.
If you take selegiline (a monoamine oxidase inhibitor) and you eat high-tyramine foods, tyramine can quickly reach dangerous levels. This can cause a serious spike in blood pressure and require emergency treatment.
Avoid consuming foods that are high in tyramine if you take selegiline (a monoamine oxidase inhibitor). You may need to continue following a low-tyramine diet for a few weeks after you stop the medication.
Tyramine is naturally found in small amounts in protein-containing foods. As these foods age, the tyramine levels increase. Tyramine amounts can vary among foods due to different processing, storage and preparation methods. You can’t reduce the amount of tyramine in a food by cooking it.
Examples of foods high in tyramine include:
- Strong or aged cheeses, such as aged cheddar, Swiss and parmesan; blue cheeses such as Stilton and Gorgonzola; and Camembert. Cheeses made from pasteurized milk — such as American cheese, cottage cheese, ricotta, farmer cheese and cream cheese — are less likely to contain high levels of tyramine.
- Cured meats, which are meats treated with salt and nitrate or nitrite, such as dry-type summer sausages, pepperoni and salami.
- Smoked or processed meats, such as hot dogs, bologna, bacon, corned beef or smoked fish.
- Pickled or fermented foods, such as sauerkraut, kimchee, caviar, tofu or pickles.
- Sauces, such as soy sauce, shrimp sauce, fish sauce, miso and teriyaki sauce.
- Soybeans and soybean products.
- Snow peas, broad beans (fava beans) and their pods.
- Dried or overripe fruits, such as raisins or prunes, or overripe bananas or avocados.
- Meat tenderizers or meat prepared with tenderizers.
- Yeast-extract spreads, such as Marmite, brewer’s yeast or sour dough bread.
- Alcoholic beverages, such as beer — especially tap or homebrewed beer — red wine, sherry and liqueurs.
- Combination foods that contain any of the above ingredients.
- Improperly stored foods or spoiled foods. While you’re taking selegiline (a monoamine oxidase inhibitor), your doctor may recommend eating only fresh foods — not leftovers or foods past their freshness dates.
It’s wise to learn the emergency signs of a rapid and severe rise in blood pressure (hypertensive crisis), which may include:
- Severe headache
- Nausea and vomiting
- Sweating and severe anxiety
- Nosebleeds
- Fast heartbeat
- Chest pain
- Changes in vision
- Shortness of breath
- Confusion
Rarely, a severe increase in blood pressure can lead to bleeding in the brain (hemorrhagic stroke).
If you take an MAOI, be prepared. Ask your doctor:
- For a list of foods to avoid — make sure you understand exactly what’s safe for you and what isn’t
- What to do if you accidently eat or drink something with too much tyramine, so you have a plan in place
Selegiline uses
Selegiline is an inhibitor of monamine oxidase (MAO) used in the treatment of depression and as adjunctive therapy in combination with levodopa and carbidopa in the therapy of Parkinson disease (sometimes called shaking palsy or paralysis agitans). Selegiline works to increase and extend the effects of levodopa, and may help to slow the progress of Parkinson’s disease.
Selegiline for depression
Transdermal selegiline is used to treat depression. Selegiline works by increasing the amount of dopamine in your brain to maintain mental balance.
Transdermal selegiline comes as a patch to apply to the skin. It is usually applied once a day and left in place for 24 hours. Remove your old selegiline patch and apply a new patch at around the same time every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Use transdermal selegiline exactly as directed. Do not apply more patches or apply patches more often than prescribed by your doctor.
Your doctor may start you on a low dose of transdermal selegiline and gradually increase your dose, not more often than once every 2 weeks.
Transdermal selegiline controls depression but does not cure it. Your condition may begin to improve after you have used transdermal selegiline for one week or longer. However, you should continue to use transdermal selegiline even if you feel well. Do not stop using transdermal selegiline without talking to your doctor.
Apply selegiline patches to dry, smooth skin anywhere on your upper chest, your back (between your neck and your waist), your upper thigh, or the outer surface of your upper arm. Choose an area where the patch will not be rubbed by tight clothing. Do not apply selegiline patches to skin that is hairy, oily, irritated, broken, scarred, or calloused.
After you apply a selegiline patch, you should wear it all the time until you are ready to remove it and put on a fresh patch. If the patch loosens or falls off before it is time to replace it, try to press it back in place with your fingers. If the patch cannot be pressed back on, dispose of it and apply a fresh patch to a different area. Replace the fresh patch at your regularly scheduled patch change time.
- Do NOT cut selegiline patches.
While you are wearing a selegiline patch, protect the patch from direct heat such as heating pads, electric blankets, heat lamps, saunas, hot tubs, and heated water beds. Do not expose the patch to direct sunlight for very long.
To use selegiline patches, follow these steps:
- Choose the area where you will apply the patch. Wash the area with soap and warm water. Rinse off all of the soap and dry the area with a clean towel.
- Open the protective pouch and remove the patch.
- Peel the first piece of liner off the sticky side of the patch. A second strip of liner should remain stuck to the patch.
- Press the patch firmly onto your skin with the sticky side down. Be careful not to touch the sticky side with your fingers.
- Remove the second strip of protective liner and press the rest of the sticky side of the patch firmly against your skin. Be sure that the patch is pressed flat against the skin with no bumps or folds and that it is firmly attached.
- Wash your hands with soap and water to remove any medicine that may have gotten on them. Do not touch your eyes until you have washed your hands.
- After 24 hours, peel the patch off slowly and gently. Fold the patch in half with the sticky sides together and dispose of it safely, so that is out of reach of children and pets. Children and pets can be harmed if they chew on, play with, or wear used patches.
- Wash the area that was under the patch with mild soap and warm water to remove any residue. If necessary, you can use baby oil or a medical adhesive removal pad to remove residue that will not come off with soap and water. Do not use alcohol, nail polish remover, or other solvents.
- Apply a new patch to a different area immediately by following steps 1 to 6.
A small number of children, teenagers, and young adults (up to 24 years of age) who took antidepressants (‘mood elevators’) such as transdermal selegiline during clinical studies became suicidal (thinking about harming or killing oneself or planning or trying to do so). Children, teenagers, and young adults who take antidepressants to treat depression or other mental illnesses may be more likely to become suicidal than children, teenagers, and young adults who do not take antidepressants to treat these conditions. However, experts are not sure about how great this risk is and how much it should be considered in deciding whether a child or teenager should take an antidepressant. Children younger than 18 years of age should not normally take transdermal selegiline, but in some cases, a doctor may decide that transdermal selegiline is the best medication to treat a child’s condition.
You should know that your mental health may change in unexpected ways when you take transdermal selegiline or other antidepressants even if you are an adult over age 24. You may become suicidal, especially at the beginning of your treatment and any time that your dose is increased or decreased. You, your family, or your caregiver should call your doctor right away if you experience any of the following symptoms: new or worsening depression; thinking about harming or killing yourself, or planning or trying to do so; extreme worry; agitation; panic attacks; difficulty falling asleep or staying asleep; aggressive behavior; irritability; acting without thinking; severe restlessness; and frenzied abnormal excitement. Be sure that your family or caregiver knows which symptoms may be serious so they can call the doctor when you are unable to seek treatment on your own.
Your healthcare provider will want to see you often while you are taking transdermal selegiline, especially at the beginning of your treatment. Be sure to keep all appointments for office visits with your doctor.
The doctor or pharmacist will give you the manufacturer’s patient information sheet (Medication Guide) when you begin treatment with transdermal selegiline. Read the information carefully and ask your doctor or pharmacist if you have any questions. You also can obtain the Medication Guide from the FDA website: https://www.fda.gov/Drugs/DrugSafety/ucm085729.htm
No matter what your age, before you take an antidepressant, you, your parent, or your caregiver should talk to your doctor about the risks and benefits of treating your condition with an antidepressant or with other treatments. You should also talk about the risks and benefits of not treating your condition. You should know that having depression or another mental illness greatly increases the risk that you will become suicidal. This risk is higher if you or anyone in your family has or has ever had bipolar disorder (mood that changes from depressed to abnormally excited) or mania (frenzied, abnormally excited mood) or has thought about or attempted suicide. Talk to your doctor about your condition, symptoms, and personal and family medical history. You and your doctor will decide what type of treatment is right for you.
Transdermal selegiline precations
Before using selegiline patch:
- tell your doctor and pharmacist if you are allergic to selegiline or any other medications.
- tell your doctor if you are taking, have recently taken, or plan to take any of the following prescription and non-prescription medications, herbal products, or nutritional supplements: amphetamines (stimulants, ‘uppers’) such as amphetamine (in Adderall), benzphetamine (Didrex), dextroamphetamine (Dexedrine, Dextrostat, in Adderall), and methamphetamine (Desoxyn);antidepressants such as amitriptyline (Elavil) and imipramine (Tofranil); buproprion (Wellbutrin, Zyban); buspirone (BuSpar); carbamazepine (Tegretol); cyclobenzaprine (Flexeril); dextromethorphan (Robitussin); medications for cough and cold symptoms or for weight loss; meperidine (Demerol); methadone (Dolophine); mirtazapine (Remeron); other monoamine oxidase inhibitors such as isocarboxazid (Marplan), phenelzine (Nardil), oral selegiline (Eldepryl, Zelapar), and tranylcypromine (Parnate); oxcarbazepine (Trileptal); pentazocine (Talwin); propoxyphene (Darvon); selective serotonin reuptake inhibitors such as citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft); selective serotonin and norepinephrine reuptake inhibitors (SSNRIs) such as duloxetine (Cymbalta) and venlafaxine (Effexor); St. John’s wort; tramadol (Ultram, in Ultracet); and tyramine supplements. Your doctor may tell you not to use transdermal selegiline until 1 or more weeks have passed since you last took one of these medications. If you stop using transdermal selegiline, your doctor will probably tell you not to take any of these medications until at least two weeks have passed since you stopped using transdermal selegiline.
- tell your doctor and pharmacist what other prescription and nonprescription medications and vitamins you are taking or plan to take. Your doctor may need to change the doses of your medications or monitor you carefully for side effects.
- you should know that selegiline may remain in your body for several weeks after you stop using the medication. During the first few weeks after your treatment ends, tell your doctor and pharmacist that you have recently stopped using selegiline before you start taking any new medications.
- tell your doctor if you have or have ever had pheochromocytoma (a tumor on a small gland near the kidneys). Your doctor may tell you that you should not use transdermal selegiline.
- tell your doctor if you tend to get dizzy or faint and if you have or have ever had seizures, a heart attack, or heart disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you become pregnant while using transdermal selegiline, call your doctor.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are using transdermal selegiline.
- you should know that transdermal selegiline may make you drowsy. Do not drive a car or operate machinery until you know how this medication affects you.
- talk to your doctor about the safe use of alcoholic beverages while you are using transdermal selegiline.
- you should know that transdermal selegiline may cause dizziness, lightheadedness, and fainting when you get up too quickly from a lying position. This is more common when you first start using transdermal selegiline. To avoid this problem, get out of bed slowly, resting your feet on the floor for a few minutes before standing up.
Special dietary instructions – avoid Tyramine containing foods
Selegiline in patch form (Emsam) delivers the medication through your skin. If you use the lowest dose of the patch, you may not need to be as strict with the foods you eat, but check with your doctor or pharmacist.
You may need to follow a special diet during your treatment with transdermal selegiline. This depends on the strength of the patches you are using. If you are using the 6 mg/24 hour patch, you may continue your normal diet.
If you are using the 9 mg/24 hour patch or the 12 mg/24 hour patch, you may experience a serious reaction if you eat foods that are high in tyramine during your treatment. Tyramine is found in many foods, including meat, poultry, fish, or cheese that has been smoked, aged, improperly stored, or spoiled; certain fruits, vegetables, and beans; alcoholic beverages; and yeast products that have fermented. Your doctor or dietitian will tell you which foods you must avoid completely, and which foods you may eat in small amounts. Follow these directions carefully. Ask your doctor or dietitian if you have any questions about what you may eat and drink during your treatment.
Selegiline dosage
Adult dose for Parkinson’s Disease
Use: Adjunct in the management of Parkinson’s disease patients being treated with levodopa-carbidopa who exhibit deterioration in the quality of their response to this therapy.
- Oral tablet
- Recommended dose: 5 mg orally twice a day
- Maximum dose: 10 mg orally per day
- Oral disintegrating tablet
- Initial dose: 1.25 mg orally once a day for at least 6 weeks. After 6 weeks, the dose may be increased to 2.5 mg orally once a day if needed.
- Maintenance dose: 1.25 to 2.5 mg orally once a day
- Maximum dose: 2.5 mg orally once a day
Comments:
- After two to three days of treatment, an attempt may be made to reduce the dose of concomitant levodopa-carbidopa by 10% to 30%. Further reductions may be possible during continued selegiline therapy.
What should I do if I forget a dose?
Take the missed dose as soon as you remember it. However, if it is almost time for your next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Adult dose for Depression
Use: Treatment of major depressive disorder
- Initial dose: Apply one 6 mg/24 hours transdermal patch to intact skin once every 24 hours
- Maintenance dose: One 6 mg/24 hours to 12 mg/24 hours transdermal patch applied to the skin once a day
- Maximum dose: 12 mg/24 hours transdermal patch applied to the skin once a day
Comments:
- Episodes of depression may require several months or more of sustained pharmacologic therapy
- If dose adjustments are necessary, they should be made in increments of 3 mg/24 hours at intervals of at least 2 weeks
- Full antidepressant effect may be delayed
What should I do if I forget a dose?
If you forget to change your patch after 24 hours, remove the old patch, apply a new patch as soon as you remember and continue your regular dosing schedule. Do not apply an extra patch to make up for a missed dose.
Selegiline side effects
Selegiline may cause dryness of the mouth. For temporary relief, use sugarless candy or gum, melt bits of ice in your mouth, or use a saliva substitute. However, if your mouth continues to feel dry for more than 2 weeks, check with your medical doctor or dentist. Continuing dryness of the mouth may increase the chance of dental disease, including tooth decay, gum disease, and fungus infections.
Some people who have used this medicine had unusual changes in their behavior. Talk with your doctor if you start having problems with gambling or increased interest in sex while using this medicine.
Do not stop taking this medicine without first checking with your doctor. Your doctor may want you to reduce gradually the amount you are taking before stopping completely.
It is important that your doctor check your skin regularly for signs of a skin cancer called melanoma. If you notice any unusual red, brown, or black spots on your skin, talk to your doctor right away.
More common side effects:
- Twitching, twisting, uncontrolled repetitive movements of the tongue, lips, face, arms, or legs
Selegiline may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- dizziness
- lightheadedness
- fainting
- dry mouth
- nausea
- vomiting
- stomach pain
- difficulty swallowing
- heartburn
- diarrhea
- gas
- constipation
- difficulty falling asleep or staying asleep
- unusual dreams
- sleepiness
- depression
- pain, especially in the legs or back
- muscle pain or weakness
- purple blotches on the skin
- rash
- redness, irritation, or sores in the mouth (if you are taking the orally disintegrating tablets)
Less common
- blurred vision
- bruising
- chest pain
- convulsions
- decreased urine
- difficult or labored breathing
- difficulty with swallowing
- discouragement
- dizziness
- dry mouth
- feeling sad or empty
- headache
- increased thirst
- irregular heartbeat
- irritability
- large, flat, blue or purplish patches in the skin
- loss of appetite
- loss of interest or pleasure
- mood changes
- muscle pain or cramps
- nausea or vomiting
- nervousness
- numbness or tingling in the hands, feet, or lips
- pounding in the ears
- seeing, hearing, or feeling things that are not there
- shakiness and unsteady walk
- shakiness in the legs, arms, hands, or feet
- sleepiness or unusual drowsiness
- slow or fast heartbeat
- swelling or inflammation of the mouth
- tightness in the chest
- tiredness
- trouble concentrating
- trouble sleeping
- unsteadiness, trembling, or other problems with muscle control or coordination
- unusual tiredness or weakness
Incidence not known:
- agitation
- diarrhea
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fever
- overactive reflexes
- poor coordination
- restlessness
- shivering
- sweating
- talking or acting with excitement you cannot control
Some side effects can be serious. If you experience any of the following symptoms, call your doctor immediately:
- severe headache
- chest pain
- fast, irregular, or pounding heartbeat
- sweating
- sudden, severe nausea and vomiting
- confusion
- stiff or sore neck
- uncontrollable shaking of a part of your body
- unusual movements that are difficult to control
- hallucinations (seeing thing or hearing voices that do not exist)
- difficulty breathing
People who have Parkinson’s disease may have an increased risk of developing melanoma (a type of skin cancer). There is not enough information to tell whether selegiline or other medications for Parkinson’s disease increase the risk of melanoma. Talk to your doctor about the risks of taking selegiline and about whether you should have your skin examined during your treatment.
Selegiline may cause other side effects. Call your doctor if you have any unusual problems while you are taking this medication.
Selegiline patch side effects
Transdermal selegiline may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
- redness of the area where you applied the patch
- diarrhea
- heartburn
- dry mouth
- weight loss
- rash
Some side effects can be serious. If you experience any of these symptoms or those listed in the IMPORTANT WARNING section, call your doctor immediately:
- severe headache
- fast, slow, or pounding heartbeat
- chest pain
- stiff or sore neck
- nausea
- vomiting
- sweating
- confusion
- widened pupils (black circles in the middle of the eyes)
- sensitivity of the eyes to light
Transdermal selegiline may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
Selegiline overdose
In case of selegiline overdose, call the poison control helpline at 1-800-222-1222. Information is also available online at https://www.poisonhelp.org/help
If the victim has collapsed, had a seizure, has trouble breathing, or can’t be awakened, immediately call your emergency services number.
Symptoms of selegiline overdose may include:
- drowsiness
- dizziness
- faintness
- irritability
- hyperactivity
- agitation
- severe headache
- hallucinations (seeing things or hearing voices that do not exist)
- jaw tightness
- stiffness and arching of the back
- seizures
- coma (loss of consciousness for a period of time)
- fast and irregular pulse
- chest pain
- slowed breathing
- sweating
- fever
- cold, clammy skin