What is septic shock
Septic shock is a life-threatening medical emergency that happens when your blood pressure drops to a dangerously low level after an infection. This reduces the amount of blood and oxygen that reaches your body’s organs, stopping them working properly. Septic shock can occur as a complication of sepsis, a serious condition that happens when the body’s reaction to an infection damages its own tissues and organs.
Sepsis is caused by infection and can happen to anyone. Sepsis is most common and most dangerous in:
- Older adults
- Pregnant women
- Children younger than 1
- People who have chronic conditions, such as diabetes, kidney or lung disease, or cancer
- People who have weakened immune systems
Septic shock symptoms may include:
- Lightheadedness (dizziness)
- A change in mental state – such as confusion or disorientation
- Diarrhea
- Feeling sick and vomiting
- Low blood pressure, especially when standing
- Slurred speech
- Severe muscle pain
- Severe shortness of breath
- Producing less urine – for example, not peeing for a day
- Cold, clammy and pale or mottled skin
- Cool, pale arms and legs
- High or very low temperature, chills
- Loss of consciousness
- Palpitations
- Rapid heart rate
- Restlessness, agitation, lethargy, or confusion
- Shortness of breath
- Skin rash or discoloration
- Decreased mental status
- Drowsiness or fatigue
- Profuse sweating, moist skin
- Irritability
- Thirst
- Rapid, weak breathing
- Enlarged pupils
- Blue tinge to lips or fingernails (or gray in the case of dark-complexions)
Early treatment of sepsis, usually with antibiotics and large amounts of intravenous fluids, improves chances for survival.
Seek medical advice urgently from your medical professional if you’ve recently had an infection or injury and you have possible early signs of sepsis.
If sepsis is suspected, you’ll usually be referred to hospital for further diagnosis and treatment.
Severe sepsis and septic shock are medical emergencies. If you think you or someone in your care has one of these conditions, go straight to emergency department or call your local emergency services number for an ambulance.
If you suspect a person is in shock, call your local emergency number. Then immediately take the following steps:
- Lay the person down and elevate the legs and feet about 12 inches (unless there is a head, neck or back injury or if you suspect broken bones in the hips or legs), unless you think this may cause pain or further injury.Keep the person warm and comfortable, and loosen restrictive clothing.
- Do not give the person anything by mouth, including anything to eat or drink.
- Do not move the person unless he or she is in danger.
- Make sure the person is breathing and has a pulse. If the person is not breathing, and you are trained to do so, do rescue breathing.
- Continue to check breathing every five minutes until help arrives.
- Take measures to control any bleeding.
- Provide appropriate first aid for any injuries or illnesses.
- If the person vomits or bleeds from the mouth, turn the person on his or her side to prevent choking (provided there is no suspicion of spinal injury).
- Do not wait for mild shock symptoms to get worse before seeking emergency help.
Septic shock mortality rate
Septic shock has a high death rate. The death rate depends on the person’s age and overall health, the cause of the infection, how many organs have failed, and how quickly and aggressively medical therapy is started.
Septic shock is a clinical emergency that occurs in more than 230,000 US patients each year, with more than 40,000 US deaths annually (18% chance of dying) 1. However, observational studies report how mortality varies across combinations of shock features from 30% to 50% 2, 3.
Septic shock survival rate
While it can be treated, septic shock is a very serious condition that people can die from.
The chances of survival are better the earlier treatment is started.
Septic shock is a clinical emergency that occurs in more than 230,000 US patients each year, with more than 190,000 US survivors annually (82% chance of survival) 1. However, observational studies report how mortality varies across combinations of shock features from 30% to 50% 2, 3, depending on demographic factors such as age, race, sex, co-morbid conditions, and the presence of organ dysfunction 4. For example, in-patient mortality was predicted most by number and degree of organ injury with the strongest predictors being respiratory, cardiovascular, hepatic, and neurologic failure 5.
Many people who are successfully treated will eventually make a full recovery, but some have long-lasting physical and mental health problems.
These problems are known as post-sepsis syndrome.
Septic shock recovery
Post Sepsis Syndrome usually lasts between 6 and 18 months, sometimes longer.
Because you may look well, others (including your employer, doctor, or family) may be unaware of the problems and expect you to be better now. Don’t suffer in silence. Tell them about Post Sepsis Syndrome and how it’s affecting you.
Physical symptoms of Post Sepsis Syndrome:
- Lethargy/excessive tiredness
- Poor mobility / muscle weakness
- Breathlessness / chest pains
- Swollen limbs (excessive fluid in the tissues)
- Joint and muscle pains
- Insomnia
- Hair loss
- Dry / flaking skin and nails
- Taste changes
- Poor appetite
- Changes in vision
- Changes in sensation in limbs
- Repeated infections from the original site or a new infection
- Reduced kidney function
- Feeling cold
- Excessive sweating
Psychological and emotional symptoms of Post Sepsis Syndrome:
- Anxiety / fear of sepsis recurring
- Depression
- Flashbacks
- Nightmares
- Insomnia (due to stress or anxiety)
- PTSD (Post Traumatic Stress Disorder)
- Poor concentration
- Short term memory loss
- Mood swings
What treatment is available?
There is no specific treatment for Post Sepsis Syndrome, but most people will get better with time. In the meantime, it’s a case of managing the individual problems and looking after yourself while you are recovering.
Tell your family and friends about Post Sepsis Syndrome, explain how you feel and give them information to read so they can understand what you’re going through. It will help you all get through this difficult time.
Not all doctors know about Post Sepsis Syndrome, so it may be helpful to take one of our booklets with you or to print out this information. It is important that your doctor assesses your symptoms and excludes any other causes of the problems. Your doctor may refer you to a different professional to help manage individual Post Sepsis Syndrome problems, such as a pain specialist to manage your pain, a counselor or psychiatrist to manage mental health and emotional problems, or a physio or occupational therapist to manage fatigue.
If you are struggling with your recovery, you can call our helpline and speak to a member of our support team. These are trained nurses with an understanding of sepsis and the problems that can occur during recovery.
Above all, remind yourself that, horrible as Post Sepsis Syndrome is, you’re not alone, and these problems are part of the recovery process. Sometimes you have to look back to where you started to see how far you have come.
Recurring infections
Some survivors find that their immune system is not as effective in the year following their sepsis. As a result, they get one infection after another, whether it’s coughs and colds, repeated water infections or a recurring wound infection.
This can be worrying, as many people fear that they may get sepsis again. In most cases, early medical consultation and treatment with antibiotics treat the infection and it doesn’t progress to anything worse. But it’s important not to neglect any infections. Always make sure you, and those close to you, know the signs of sepsis and seek urgent medical attention if concerned.
Sepsis vs septic shock
Sepsis is a potentially life-threatening condition caused by the body’s response to an infection. The body normally releases chemicals into the bloodstream to fight an infection. Sepsis occurs when the body’s response to these chemicals is out of balance, triggering changes that can damage multiple organ systems.
If sepsis progresses to septic shock, blood pressure drops dramatically. This may lead to death.
Most often, sepsis occurs in people who are hospitalized or who have recently been hospitalized. People in the intensive care unit are especially vulnerable to developing infections, which can then lead to sepsis. If you develop signs and symptoms of sepsis after surgery or after being hospitalized, seek medical care immediately.
Risk factors for sepsis and septic shock
Sepsis and septic shock are more common if you:
- Are very young or very old
- Have a compromised immune system
- Have diabetes or cirrhosis
- Are already very sick, often in a hospital intensive care unit
- Have wounds or injuries, such as burns
- Have invasive devices, such as intravenous catheters or breathing tubes
- Have previously received antibiotics or corticosteroids
Causes of sepsis
Sepsis can be triggered by an infection in any part of the body. The most common sites of infection leading to sepsis are the lungs, urinary tract, tummy (abdomen) and pelvis.
Any type of infection — bacterial, viral or fungal — can lead to sepsis, the most likely varieties include:
- Pneumonia
- Infection of the digestive system (which includes organs such as the stomach and colon)
- Infection of the kidney, bladder and other parts of the urinary system
- Bloodstream infection (bacteremia)
Sepsis may develop when you’re already in hospital. For example, you’re more likely to develop sepsis if:
- you’ve recently had surgery
- you’ve had a urinary catheter fitted
- you have to stay in hospital for a long time
Sources of infection
Types of infection associated with sepsis include:
- lung infection (pneumonia)
- appendicitis
- an infection of the thin layer of tissue that lines the inside of the abdomen (peritonitis)
- an infection of the bladder, urethra or kidneys (urinary tract infection)
- an infection of the gallbladder (cholecystitis) or bile ducts (cholangitis)
- skin infections, such as cellulitis – this can be caused by an intravenous catheter that’s been inserted through the skin to give fluids or medication
- infections after surgery
- infections of the brain and nervous system – such as meningitis or encephalitis
- flu (in some cases)
- bone infection (osteomyelitis)
- heart infection (endocarditis)
Sometimes the specific infection and source of sepsis can’t be identified.
Who’s at risk of sepsis?
Everybody is potentially at risk of developing sepsis from minor infections. However, some people are more vulnerable, including people who:
- have a medical condition that weakens their immune system – such as HIV or leukemia
- are receiving medical treatment that weakens their immune system – such as chemotherapy or long-term steroids
- are very young or very old
- are pregnant
- have a long-term health condition – such as diabetes
- have just had surgery, or have wounds or injuries as a result of an accident
- are on mechanical ventilation – where a machine is used to help you breathe
- have drips or catheters attached to their skin
- are genetically prone to infections
Sepsis is a particular risk for people already in hospital because of another serious illness.
Bacterial infections that can be caught in hospital, such as MRSA (meticillin-resistant Staphylococcus aureus also called “superbug”), tend to be more serious, as these bacteria have often developed a resistance to many commonly used antibiotics.
What causes the symptoms of sepsis?
Usually, your immune system keeps an infection limited to one place. This is known as a localised infection.
Your body produces white blood cells, which travel to the site of the infection to destroy the germs causing infection.
A series of biological processes occur, such as tissue swelling, which helps fight the infection and prevents it spreading. This process is known as inflammation.
If your immune system is weak or an infection is particularly severe, it can quickly spread through the blood into other parts of the body. This causes the immune system to go into overdrive, and the inflammation affects the entire body.
This can cause more problems than the initial infection, as widespread inflammation damages tissue and interferes with blood flow.
The interruption in blood flow leads to a dangerous drop in blood pressure, which stops oxygen reaching your organs and tissues.
Tests to diagnose sepsis
Sepsis is often diagnosed based on simple measurements such as your temperature, heart rate and breathing rate. You may need to give a blood test.
Other tests can help determine the type of infection, where it’s located and which body functions have been affected. These include:
- urine or stool samples
- a wound culture – where a small sample of tissue, skin or fluid is taken from the affected area for testing
- respiratory secretion testing – taking a sample of saliva, phlegm or mucus
- blood pressure tests
- imaging studies – such as an X-ray, ultrasound scan or CT scan
Diagnostic criteria for sepsis 6
General variables
- Fever >100.9 °F (38.3 °C)
- Hypothermia (core temperature <96.8 °F [36 °C])
- Heart rate >90/min−1 or more than two SD above the normal value for age
- Tachypnea
- Altered mental status
- Significant edema or positive fluid balance (>20 mL/kg over 24 h)
- Hyperglycemia (plasma glucose >140 mg/dL or 7.7 mmol/L) in the absence of diabetes
Inflammatory variables
- Leukocytosis (white blood cells >12 000/μL)
- Leukopenia (white blood cells count <4000/μL)
- Normal white blood cells count with greater than 10% immature forms
- Plasma C-reactive protein more than two SD above the normal value
- Plasma procalcitonin more than 2 SD above the normal value
Hemodynamic variables
Arterial hypotension (systolic blood pressure <90 mmHg, mean arterial pressure <70 mmHG, or an systolic blood pressure decrease >40 mmHg in adults or less than 2 SD below normal for age)
Organ dysfunction variables
- Arterial hypoxemia (PaO2/FiO2 <300)
- Acute oliguria (urine output <0.5 mL/kg/h for at least 2 h despite adequate fluid resuscitation)
- Creatinine increase >0.5 mg/dL or 44.2 μmol/L
- Coagulation abnormalities (INR (international normalized ratio) >1.5 or activated partial thromboplastin time (aPTT) >60 s)
- Ileus (absent bowel sound)
- Thrombocytopenia (platelet count <100 000 μL−1)
- Hyperbilirubinemia (plasma total bilirubin >4 mg/dL or 70 μmol/L)
Tissue perfusion variables
- Hyperlactatemia (>1 mmol/L)
- Decreased capillary refill or mottling
Severe sepsis criteria
Severe sepsis definition = sepsis-induced tissue hypoperfusion or organ dysfunction (any of the following thought to be due to the infection).
- Sepsis-induced hypotension
- Lactate above upper limits laboratory normal
- Urine output <0.5 mL/kg/h for more than 2 h despite adequate fluid resuscitation
- Acute lung injury with PaO2/FiO2 <250 in the absence of pneumonia as infection source
- Acute lung injury with PaO2/FiO2 <200 in the presence of pneumonia as infection source
- Creatinine >2.0 mg/dL (176.8 μmol/L)
- Bilirubin >2 mg/dL (34.2 μmol/L)
- Platelet count <100 000 μL
- Coagulopathy (international normalized ratio >1.5)
Treatments for sepsis
If sepsis is detected early and hasn’t affected vital organs yet, it may be possible to treat the infection at home with antibiotics. Most people who have sepsis detected at this stage make a full recovery.
Almost all people with severe sepsis and septic shock require admission to hospital. Some people may require admission to an intensive care unit (ICU).
Because of problems with vital organs, people with severe sepsis are likely to be very ill and the condition can be fatal.
However, sepsis is treatable if it is identified and treated quickly, and in most cases leads to a full recovery with no lasting problems.
Sepsis recovery
Some people make a full recovery fairly quickly. The amount of time it takes to fully recover from sepsis varies, depending on:
- the severity of the sepsis
- the person’s overall health
- how much time was spent in hospital
- whether treatment was needed in an ICU
Some people experience long-term physical and/or psychological problems during their recovery period, such as:
- feeling lethargic or excessively tired
- muscle weakness
- swollen limbs or joint pain
- chest pain or breathlessness
These long-term problems are known as post-sepsis syndrome. Not everyone experiences these problems.
What causes septic shock
Septic shock occurs most often in the very old and the very young. It may also occur in people with weakened immune systems.
Any type of bacteria can cause septic shock. Fungi and (rarely) viruses may also cause the condition. Toxins released by the bacteria or fungi may cause tissue damage. This may lead to low blood pressure and poor organ function. Some researchers think that blood clots in small arteries cause the lack of blood flow and poor organ function.
The body has a strong inflammatory response to the toxins that may contribute to organ damage.
Risk factors for septic shock include:
- Diabetes
- Diseases of the genitourinary system, biliary system, or intestinal system
- Diseases that weaken the immune system, such as AIDS
- Indwelling catheters (those that remain in place for extended periods, especially intravenous lines and urinary catheters, and plastic and metal stents used
- for drainage)
- Leukemia
- Long-term use of antibiotics
- Lymphoma
- Recent infection
- Recent surgery or medical procedure
- Recent or current use of steroid medicines
- Solid organ or bone marrow transplantation
Who’s at risk of septic shock?
Anyone can develop septic shock, but it’s most common in people with a weak immune system, the body’s natural defences against illness and infection.
This includes:
- babies
- elderly people
- pregnant women and women who’ve recently given birth
- people with serious or long-term health conditions, such as diabetes, scarring of the liver (cirrhosis), kidney disease or cancer
- people with a condition that weakens the immune system, such as HIV or AIDS
- people having treatment that weakens the immune system, such as chemotherapy or long-term steroid treatment
Septic shock often occurs in people who are already in hospital for another reason.
Septic shock prevention
Prompt treatment of bacterial infections is helpful. However, many cases of septic shock cannot be prevented.
Stages of septic shock
Sepsis is a clinical state that falls along a continuum of pathophysiologic states, starting with a systemic inflammatory response syndrome and ending in multiorgan dysfunction syndrome before death.
The earliest signs of inflammation are heralded by the following:
- Fever (temperature higher than 38 C or hypothermia (temperature less than 36 C)
- Tachycardia (heart rate more than 90 beats per minute),
- Tachypnea (respiratory rate more than 20 breaths per minute)
- Leukocytosis (white blood cells greater than 12,000/mm³) / leukopenia (white blood cells less than 4,000/mm³) with or without bandemia (more than 10%).
The presence of two of these four clinical signs is necessary for the diagnosis of systemic inflammatory response syndrome. After that, systemic inflammatory response syndrome with an infectious source suffices the clinical definition for sepsis 7.
With the development of hypotension, tissue demands are not adequately met by tissue oxygenation, and the patient is now defined to be in severe sepsis 7. The decline in peripheral vascular perfusion and oxygenation leads to cellular and metabolic derangements, most notably a shift from aerobic respiration to anaerobic respiration with ensuing lactic acidosis. Tissue hypoperfusion may also be manifested by signs of end-organ damage, such as pre-renal azotemia or transaminitis. The difference in oxygen supply and demand can be monitored during resuscitation by trending the mixed venous oxygen saturation from a central line in the superior vena cava (SVC), when available 8.
When sepsis-induced hypotension remains refractory to initial management with fluid resuscitation, septic shock ensues 7. Septic shock is distinguished from other shock states as a distributive type of shock. The action of a combination of inflammatory mediators (histamine, serotonin, super-radicals, lysosomal enzymes) elaborated in response to bacterial endotoxins leads to a marked increase in capillary permeability and a concomitant reduction in peripheral vascular resistance. This translates not only into a reduction in afterload but also in preload from a decline in venous return from third-spacing. The resulting reduction in stroke volume is accommodated initially by an elevation in heart rate, i.e., compensated septic shock. As a result, the patient is in a hyperdynamic state that is characteristic of septic shock 8.
Clinically, patients, have a dynamic precordium with tachycardia and bounding peripheral pulses. They are warm to the touch and have a reduction in capillary refill (flash cap refill). This is described as warm shock. As shock progresses, elevated catecholamine production leads to an increase in peripheral vascular resistance as the body attempts to shunt blood away from non-vital tissues (gastrointestinal (GI) tract, kidneys, muscle, and skin) to the vital tissues (brain and heart). This is described as cold shock. Understanding the pathophysiology and continuum of septic shock is imperative in initiating appropriate treatment measures 8.
Functionally, septic shock is defined by persistent hypotension despite adequate fluid resuscitation from 60 ml/kg to 80 mL/kg of either crystalloid or colloid fluid. At this point, the initiation of appropriate vasoactive medications such as beta-adrenergic or alpha-adrenergic drugs is of utmost importance. The progression of organ dysfunction despite high-dose vasoactive administration defines the state of multi-organ dysfunction syndrome (MODS) which carries a mortality as high as 75%. While the exact circumstances predicting poor prognosis and death have been difficult to determine, immunologic dissonance (exaggerated proinflammatory response) versus immunologic paralysis (exaggerated anti-inflammatory response) have been purported to play a role 9.
Signs and symptoms of septic shock
Symptoms of sepsis may appear first.
Sepsis symptoms in children under five:
- looks mottled, bluish or pale
- is very lethargic or difficult to wake
- feels abnormally cold to touch
- is breathing very fast
- has a rash that does not fade when you press it
- has a fit or convulsion
Go straight to the emergency department or call your local emergency services number for an ambulance if your child has any of these symptoms.
Sepsis symptoms in older children and adults:
- a high temperature (fever) or low body temperature
- chills and shivering
- a fast heartbeat
- fast breathing
Many of the symptoms of sepsis are also associated with meningitis. The first symptoms of meningitis are often fever, vomiting, headache and feeling unwell.
Early signs and symptoms of sepsis
Earlier on in the presentation of sepsis, patients present with the following vital sign changes:
- Fever, temperature higher than 100.4 °F (38 °C), or hypothermia, temperature lower than 96.8 °F (36 °C)
- Tachycardia with a heart rate higher than 90 beats per minute in adult patients or less than two standard deviations for age in pediatric patients
- Tachypnea with respiratory rate greater than 20 breaths per minute in adult patients or more than two standard deviations for age in pediatric patients
Signs and symptoms of Severe Sepsis is defined as sepsis and end-organ dysfunction. At this stage, signs, and symptoms may include:
- Altered mental status
- Oliguria or anuria
- Hypoxia
- Cyanosis
- Ileus
Symptoms of septic shock may develop if sepsis is left untreated. In some cases, symptoms of more severe sepsis or septic shock (when your blood pressure drops to a dangerously low level) develop soon after. Septic shock can affect any part of the body, including the heart, brain, kidneys, liver, and intestines.
Septic shock symptoms may include:
- Lightheadedness (dizziness)
- A change in mental state – such as confusion or disorientation
- Diarrhea
- Feeling sick and vomiting
- Low blood pressure, especially when standing
- Slurred speech
- Severe muscle pain
- Severe shortness of breath
- Producing less urine – for example, not peeing for a day
- Cold, clammy and pale or mottled skin
- Cool, pale arms and legs
- High or very low temperature, chills
- Loss of consciousness
- Palpitations
- Rapid heart rate
- Restlessness, agitation, lethargy, or confusion
- Shortness of breath
- Skin rash or discoloration
- Decreased mental status
- Drowsiness or fatigue
- Profuse sweating, moist skin
- Irritability
- Thirst
- Rapid, weak breathing
- Enlarged pupils
- Blue tinge to lips or fingernails (or gray in the case of dark-complexions)
Patients progressing to septic shock will experience signs and symptoms of severe sepsis with hypotension. Of note, at an early “compensated” stage of shock, blood pressure may be maintained, and other signs of distributive shock might be present, for example, warm extremities, flash capillary refill (less than one second), and bounding pulses, also known as warm shock. This stage of shock, if managed aggressively with fluid resuscitation and vasoactive support, can be reversed. With the progression of septic shock into the uncompensated stage, hypotension ensues, and patients may present with cool extremities, delayed capillary refill (more than three seconds), and thready pulses, also known as cold shock. After that, with continued tissue hypoperfusion, shock may be irreversible, progressive rapidly into multiorgan dysfunction syndrome and death.
Septic shock possible complications
Respiratory failure, cardiac failure, or any other organ failure can occur. Gangrene may occur, possibly leading to amputation.
Septic shock diagnosis
Blood tests may be done to check for:
- Infection around the body
- Complete blood count (CBC) and blood chemistry
- Presence of bacteria or other organisms
- Low blood oxygen level
- Disturbances in the body’s acid-base balance
- Poor organ function or organ failure
Other tests may include:
- A chest x-ray to look for pneumonia or fluid in the lungs (pulmonary edema)
- A urine sample to look for infection
Additional studies, such as blood cultures, may not become positive for several days after the blood has been taken, or for several days after the shock has developed.
Laboratory Findings
Findings in sepsis, severe sepsis, and septic shock are as follows 10:
- Hyperglycemia (glucose more than 120 mg/dL)
- Leukocytosis (white blood cells more than 12,000/mm³) or leukopenia (white blood cells less than 4000/mm³)
- Bandemia (more than 10%)
- C-reactive protein or procalcitonin more than 2 SD above normal
- Mixed venous saturation more than 70%
- PaO2: FiO2 less than 300
- Pre-renal azotemia
- Coagulopathy, INR more than 1.5 or PTT more than 60 sec
- Thrombocytopenia (platelets less than 100,000/mL)
- Hyperbilirubinemia (total bilirubin more than 4 mg/dL)
- Lactic acidosis (more than 2 mmol/L)
Patients should be placed on continuous cardiopulmonary monitoring to allow close observation of vital signs. A thorough assessment of end-organ function and peripheral perfusion should be undertaken to determine where along the pathophysiologic continuum of sepsis they may fall. This should include a Glasgow Coma Scale (GCS) or mental status assessment, urine output measurement, or lactate/mixed venous saturation determination (with central lines). Regardless of where along the continuum patients are, all patients should have drawn a complete blood count with differential (CBC-d), source cultures (blood, urine, tracheal (if intubated), wound), and a urinalysis. Depending on the severity of presentation and age of the patient a lumbar puncture may be indicated, for example, patients with signs of encephalitis or meningitis or febrile pediatric patients under six weeks of age. The addition of C-reactive protein or procalcitonin, both acute phase proteins, may be helpful in distinguishing viral from bacterial sepsis, with the latter showing steeper elevations in these proteins. A complete chemistry panel with liver function test, disseminated intravascular coagulation (DIC) panel, and an arterial blood gas are additional labs that may provide important information on the severity of sepsis syndrome in a patient.
Septic shock criteria
| Septic shock diagnostic criteria | |
Clinical diagnosis is the criterion standard:
| Normotensive shock with isolated hyperlactemia needs clarity; Lactate and systolic blood pressure thresholds are uncertain; Biologic phenotyping may be promising but not yet feasible in real time or tested in randomized clinical trials |
| Pulmonary artery catheterization and continuous monitoring of central venous oxygen saturation not recommended for routine diagnosis | May have a role in right ventricular dysfunction, complex cases with diagnostic uncertainty |
| Focused ultrasonography is suggested if there is concern for overlapping hemodynamic manifestations of shock | Practical, easy to use, and recommended by expert consensus7 |
| Arterial pulse contour analysis | Awaiting randomized clinical trials for patient outcomes; Requires controlled mechanical ventilation and sinus rhythm |
Septic shock treatment
Septic shock is a medical emergency. In most cases, people are admitted to the intensive care unit of the hospital.
Below guidelines are derived from the 2012 Surviving Sepsis Campaign Guidelines 11:
Source Control
- Broad-spectrum antibiotics within one hour of diagnosis for all patients. Initial empiric anti-infective therapy should have activity against all likely pathogens and adequate penetration of source tissue.
- Removal of infected/necrotic tissue, if it is the source of septic shock, i.e. patients with cellulitis, abscess, infected devices, purulent wounds.
Management of Shock 12
- Measures most effective if achieved within the first six hours of diagnosis
- Restore central venous pressure (CVP) to 8 mmHg to 12 mmHg
- Restore mean arterial pressure (MAP) greater than 65 mmHg
- Restore superior vena cava saturation to 70% or mixed venous saturation to 65%
- Fluid resuscitation with crystalloid (NS or albumin) and colloid (blood products) up to 80 ml/kg
- Mechanical ventilation to reduce metabolic demand
- First line vasoactive agents (epinephrine in cold shock versus norepinephrine in warm shock) when fluid-refractory
- Note: dopamine as a first line agent has fallen out of favor given its inhibitory effect on the hypothalamic pituitary adrenal axis, namely prolactin and growth hormone, which can confer immunologic dysfunction 13
Enhancing Host Response
- Corticosteroids indicated in vasoactive-refractory shock and or in patients with low (unstimulated) basal cortisol levels less than 150 ug/L) 14
- Addition of vasopressin indicated in vasoactive-refractory shock
While central lines are not required for the resuscitation of patients with septic shock, they provide an accurate means of monitoring CVP and mixed venous saturations. Remember that CVP and MVO2 are most accurate from a central line that lies within the right atrium; lower extremity central lines do not provide the most accurate data for monitoring these indices of resuscitation. Regarding the need for central venous access for administration of vasoactive agents, a recent study showed that both dopamine, norepinephrine, and phenylephrine at high doses could be safely administered via peripheral venous access (Cardenas-Garcia et al., 2015).
Of note, early goal-directed therapy (EGDT) has not been shown to confer a survival benefit in more recent studies 15. All studies comparing early goal-directed therapy to standard practice have shown an increase in the administration of crystalloid and packed red blood cells in the first six hours and the placement of central lines. Furthermore, survival was influenced most by the maintenance of blood pressure independent of the type of fluid or vasoactive used and not CVP or MVO2 16. That said, the Surviving Sepsis Campaign guidelines continue to support early goal-directed therapy as the standard of practice for management of severe sepsis and septic shock.
The placement of an arterial line becomes important in the management of vasoactive-refractory shock for close monitoring of blood pressure and tissue oxygenation status via regular blood gasses with key attention to lactate levels and pO2.
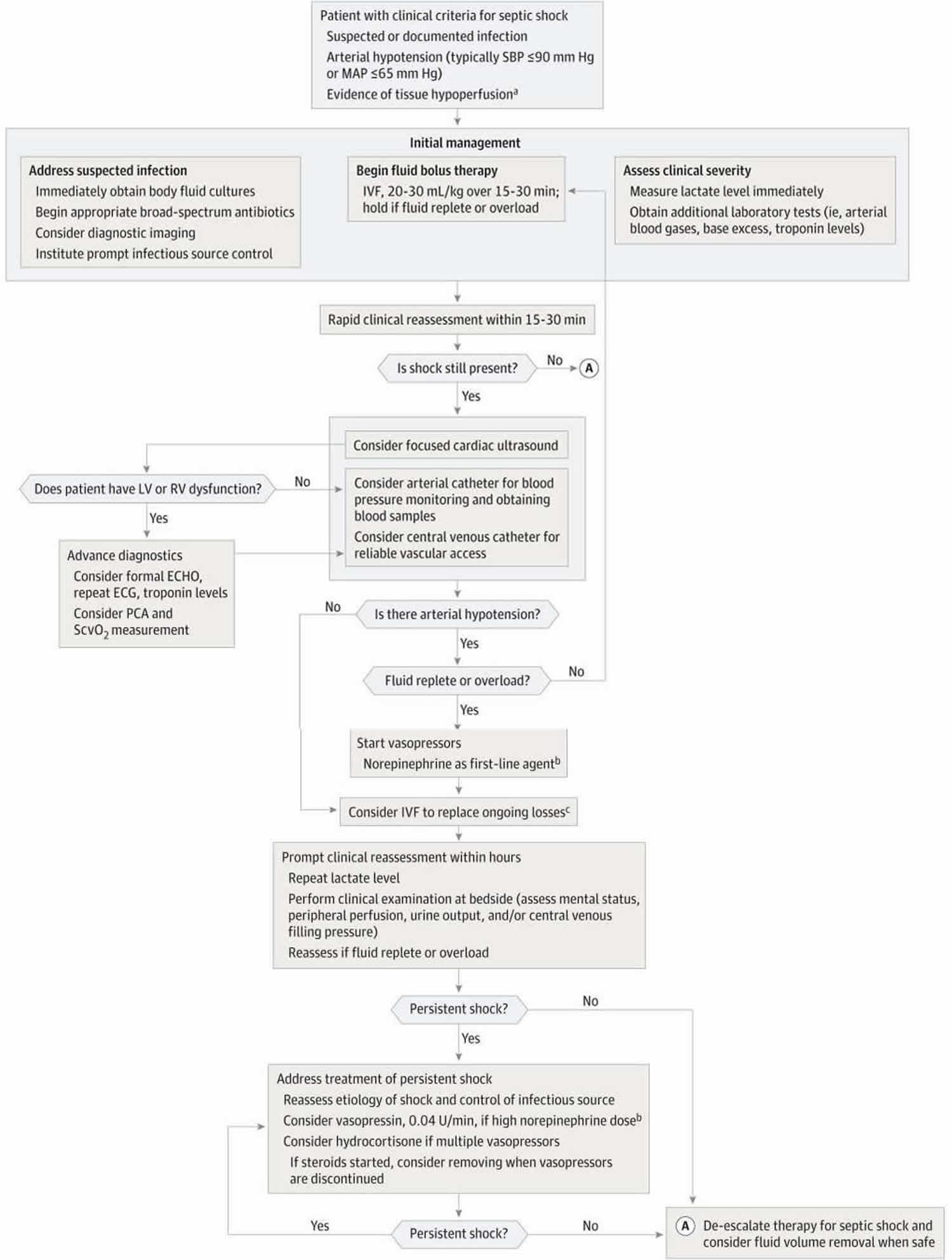
Figure 1. Proposed Algorithm for Treatment of Septic Shock
Footnote:
a) Tissue hypoperfusion typically manifests as altered mentation, low urinary output, poor peripheral perfusion, and/or hyperlactemia (≥2.0 mmol/L).
b) Norepinephrine may not always be the first choice in setting of tachycarrythmias or atrial fibrillation; consider adding vasopressin for norepinephrine rates that exceed 15 3g/kg/min.
c) The choice for fluid repletion and type will be refined by ongoing safety checks for pulmonary edema/fluid overload, metabolic derangements from unbalanced crystalloids, and ongoing losses.
Abbreviations: ECG = electrocardiogram; ECHO = echocardiogram; IVF = intravenous fluids; LV/RV = left ventricular/right ventricular; MAP = mean arterial pressure; PCA = pulse contour analysis; SBP = systolic blood pressure; ScvO2 = continuous central venous oxygen saturation.
[Source 1 ]Septic shock treatment may include:
- Breathing machine (mechanical ventilation)
- Dialysis
- Drugs to treat low blood pressure, infection, or blood clotting
- Norepinephrine is recommended as a first-line vasopressor
- Vasopressin may spare norepinephrine at higher doses
- Low-dose corticosteroids to be considered for vasopressor-dependent shock. Dosing regimen and timing of discontinuation remains controversial
- High volume of fluids given directly into a vein (intravenously)
- Prompt fluid bolus is recommended (500–1000 mL) with appropriate safety limits
- Fluid therapy with balanced crystalloids vs albumin is suggested based on meta-analyses 17, while specific fluid comparisons undergo additional randomized clinical trials
- Oxygen given through a face mask, a tube in the nose, or a tube passed down the throat
- Sedatives
- Surgery to drain infected areas and any tissue that has been badly damaged by the infection, if needed
- Antibiotics given into a vein
The pressure in the heart and lungs may be checked. This is called hemodynamic monitoring. This can only be done with special equipment and intensive care nursing.
It’s likely someone with septic shock will need to stay in hospital for several weeks.
References- Seymour CW, Rosengart MR. Septic Shock: Advances in Diagnosis and Treatment. JAMA. 2015;314(7):708-17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4646706/
- Liu V, Escobar GJ, Greene JD, Soule J, Whippy A, Angus DC, Iwashyna TJ. Hospital deaths in patients with sepsis from 2 independent cohorts. JAMA. 2014 Jul 02;312(1):90-2.
- Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010;36(2):222-31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2826633/
- Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005 Jan 1-7;365(9453):63-78.
- Elfeky S, Golabi P, Otgonsuren M, Djurkovic S, Schmidt ME, Younossi ZM. The epidemiologic characteristics, temporal trends, predictors of death, and discharge disposition in patients with a diagnosis of sepsis: A cross-sectional retrospective cohort study. J Crit Care. 2017 Jun;39:48-55.
- Schorr CA, Zanotti S, Dellinger RP. Severe sepsis and septic shock: management and performance improvement. Virulence. 2013;5(1):190-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3916373/
- Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992 Jun;101(6):1644-55.
- Nguyen HB, Rivers EP, Abrahamian FM, Moran GJ, Abraham E, Trzeciak S, Huang DT, Osborn T, Stevens D, Talan DA., Emergency Department Sepsis Education Program and Strategies to Improve Survival (ED-SEPSIS) Working Group. Severe sepsis and septic shock: review of the literature and emergency department management guidelines. Ann Emerg Med. 2006 Jul;48(1):28-54.
- Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N. Engl. J. Med. 2003 Jan 09;348(2):138-50.
- Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G., International Sepsis Definitions Conference. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med. 2003 Apr;29(4):530-8.
- Mahapatra S, Heffner AC. Shock, Septic (Sepsis) [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430939
- Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M., Early Goal-Directed Therapy Collaborative Group. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N. Engl. J. Med. 2001 Nov 08;345(19):1368-77.
- Ventura AM, Shieh HH, Bousso A, Góes PF, de Cássia F O Fernandes I, de Souza DC, Paulo RL, Chagas F, Gilio AE. Double-Blind Prospective Randomized Controlled Trial of Dopamine Versus Epinephrine as First-Line Vasoactive Drugs in Pediatric Septic Shock. Crit. Care Med. 2015 Nov;43(11):2292-302.
- Annane D, Aegerter P, Jars-Guincestre MC, Guidet B., CUB-Réa Network. Current epidemiology of septic shock: the CUB-Réa Network. Am. J. Respir. Crit. Care Med. 2003 Jul 15;168(2):165-72.
- ProCESS Investigators. Yealy DM, Kellum JA, Huang DT, Barnato AE, Weissfeld LA, Pike F, Terndrup T, Wang HE, Hou PC, LoVecchio F, Filbin MR, Shapiro NI, Angus DC. A randomized trial of protocol-based care for early septic shock. N. Engl. J. Med. 2014 May 01;370(18):1683-93.
- Osborn TM. Severe Sepsis and Septic Shock Trials (ProCESS, ARISE, ProMISe): What is Optimal Resuscitation? Crit Care Clin. 2017 Apr;33(2):323-344.
- Rochwerg B, Alhazzani W, Gibson A, et al. FISSH Group (Fluids in Sepsis and Septic Shock) Fluid type and the use of renal replacement therapy in sepsis: a systematic review and network meta-analysis [published online April 23, 2015] Intensive Care Med. doi: 10.1007/s00134-015-3794-1.