Silent sinus syndrome
Silent sinus syndrome is a rare disorder characterized by progressive enophthalmos, hypoglobus (inferior displacement of the globe in the orbit) and painless facial asymmetry due to a spontaneous, asymptomatic collapse of the maxillary sinus and orbital floor associated with chronic maxillary sinusitis and negative sinus pressures 1. As a result, secretions accumulate, and inflammation occurs, resulting in maxillary atelectasis and wall collapse 2. Silent sinus syndrome was first described by Montgomery in 1964 3, however, the term silent sinus syndrome was first described by Soparker in 1994 4.
In 1997 Kass et al. 5 suggested the name “chronic maxillary atelectasis”, as a term describing 22 patients with similar findings. Chronic maxillary atelectasis, however, may be diagnosed in patients with chronic rhinosinusitis symptoms while the criteria of silent sinus syndrome stipulate that affected patients must have the absence of these symptoms for diagnosis 6. Additionally, chronic maxillary atelectasis is divided into three stages, with stage 1 and 2 describing maxillary deformity in the absence of hypoglobus or enophthalmos 5.
While some strictly distinguish chronic maxillary atelectasis and silent sinus syndrome as separate clinical entities distinguished by presence or absence of chronic sinusitis symptoms, others suggest that silent sinus syndrome is actually part of the spectrum of chronic maxillary atelectasis 7. The tertiary stage of chronic maxillary atelectasis, manifest clinical deformity including enophthalmos and hypoglobus, closely overlays the definition of silent sinus syndrome 5.
More recently, Rose et al. 8 have suggested the term “imploding antrum syndrome” to clarify and describe the more acute and symptomatic event of sinus implosion that happens rapidly after long periods of chronic underlying atelectasis.
Silent sinus syndrome is usually diagnosed in patients in their 30s and 40s with a mean age of 39 and a range of 19 to 82 7. Most report an equal prevalence of silent sinus syndrome in men and women 9, although one large study of 84 patients suggests there may be a slightly higher rate in men 10. There is an equal reported incidence of right and left-sided disease 7. Silent sinus syndrome is almost exclusively a unilateral condition, although there are two case reports in the literature of bilateral disease 11.
Usually silent sinus syndrome diagnosis is suspected clinically, and it can be confirmed radiologically by characteristic imaging features that include maxillary sinus outlet obstruction, sinus opacification, and sinus volume loss caused by inward retraction of the sinus walls. Silent sinus syndrome treatment is surgical involving making an outlet for mucous drainage from the obstructed sinus, and despite controversies in the literature, simultaneous management of enophthalmos and sinus pathologies existing in the floor of the orbit, reconstruction, and endoscopic uncinectomy and antrostomy should be considered as some of the main options for treatment.
Silent sinus syndrome causes
In their early reports, Montgomery 12 named a mucocele as the cause of enophthalmos while Wilkins and Kulwin 13 noted a strong association with ipsilateral chronic maxillary sinus disease. When silent sinus syndrome was described in 1994 by Soparkeret al. 6, the disease process was initially though to be related to pre-existing sinus hypoplasia. This association, however, was disproven after a 1999 case report by Davidsonet al. 14 documented pre-disease imaging demonstrating normal maxillary sinus anatomy several years prior to the onset of symptoms and manifestations of silent sinus syndrome. This report thus strongly suggested that silent sinus syndrome occurs in patients with normal sinus size prior to disease development.
Silent sinus syndrome occurs due to hypoventilation of the maxillary sinus after osteomeatal complex obstruction 15. Obstruction of the natural sinus os may be secondary to multiple mechanisms including lateralized infundibular wall 5, lateralized middle turbinate 16, mucocele or polyp occluding the ostium 6, inflamed nasal mucosa, or presence of infraorbital ethmoid air cells that narrow maxillary ostium 17.
Occlusion and hypoventilation of the sinus leads to negative pressure development. This phenomenon was first demonstrated experimentally in rabbits in whom experimental occlusion of maxillary ostium resulted in measured subatmospheric pressure in the sinus 18. Kass et al. 19 then investigated intra-sinus pressure measurements in 5 patients with diagnosed maxillary atelectasis and compared them to pressures of 5 healthy control patients. The study utilized an 18-gauge needle placed into the sinus and attached to a pressure transducer. Results revealed subatmospheric intra-sinus pressures ranging from -13 to -6 cm H2O with a mean of −8.4 ± 2.6 cm H2O 19. Another case report employing the same measurement procedure documented negative pressure in the maxillary sinus of -23 mmHg (31.3 cm H2O) 14. This process of ostium occlusion followed by negative pressure development may be analogous to what occurs in the middle ear in patients with Eustachian tube obstruction 19.
Once the sinus becomes occluded and negative pressure develops, the sinus cavity is filled with a combination of mucus and acellular transudate 19 due to reabsorption of the aqueous component of the natural sinus mucosal secretions 9.
This process of aeration loss is hypothesized to create chronic, low-grade mucosal inflammation. Over time secondary demineralization of the bony orbital floor results, thus allowing the negative pressure of the sinus to implode these weakened areas 20.
Smoking
There has been a reported negative association between cigarette smoking and incidence of silent sinus syndrome. Observers of silent sinus syndrome have hypothesized that chronic inflammation and sinonasal disease caused by smoking may lead smokers to present with symptoms much earlier and therefore have treatment before development of the syndrome 9.
Orbital decompression
There has been an observed association of the late development of iatrogenic silent sinus syndrome after some bone-removing orbital decompressions for thyroid eye disease. One series reported 6 patients developing enophthalmos and hypoglobus months to years after ipsilateral orbital decompression for thyroid eye disease 21. Secondarily prolapsed fat into the ethmoidal infundibulum during the surgery occludes the maxillary sinus ostium. Development of silent sinus syndrome after orbital decompression may also be related to the removal of inferomedial bone strut important to maintaining the normal maxilla-ethmoidal interface and sinus aeration 21. With this consideration, it is recommend a concurrent prophylactic middle meatal antrostomy be performed with surgery for orbital decompression if the bone strut is to be removed to prevent future obstruction and imploding antrum 20.
Risk factors for silent sinus syndrome
Underlying aberrant nasal anatomy is thought to be the largest risk factor for silent sinus syndrome. Specifically, studies describe characteristic anatomical variations including ipsilateral nasal septum deviation, laterally deviated middle turbinate, and otherwise narrowed infundibular passage 16. Lateral deviation of middle turbinate was found in 62% of patients in a case series of 16 people 16.
These anatomical variations are hypothesized to predispose to a “flap-valve” occlusion of the natural maxillary sinus ostium wherein the sinus becomes completely occluded allowing gas resorption and development of negative pressure in the sinus antrum 19.
Silent sinus syndrome symptoms
Silent sinus syndrome presentation is typically with painless and usually relatively long-standing (months to years) facial asymmetry, enophthalmos of 2-5 mm, and hypoglobus 22. Symptoms of sinusitis are not always present 23. When there is significant deformity of the orbital floor, patients may develop diplopia. Diplopia is the most commonly occurring visual symptom, noted in 28% to 65% of cases in two large case series 7. In a series of 67 patients, however, ocular motility limitation was only noted in only 4 cases, each with significant hypoglobus 9. The proposed mechanism of diplopia is secondary to limitation of the superior and inferior oblique muscles, as their attachments to the bony orbit make them vulnerable to dysfunction when the globe becomes displaced in relationship to bony orbit 10. It has also been suggested that the inferior rectus muscle may develop fibrosis 24.
By strict criteria, silent sinus syndrome is not associated with exhibited sinus symptoms 10.
Signs of silent sinus syndrome
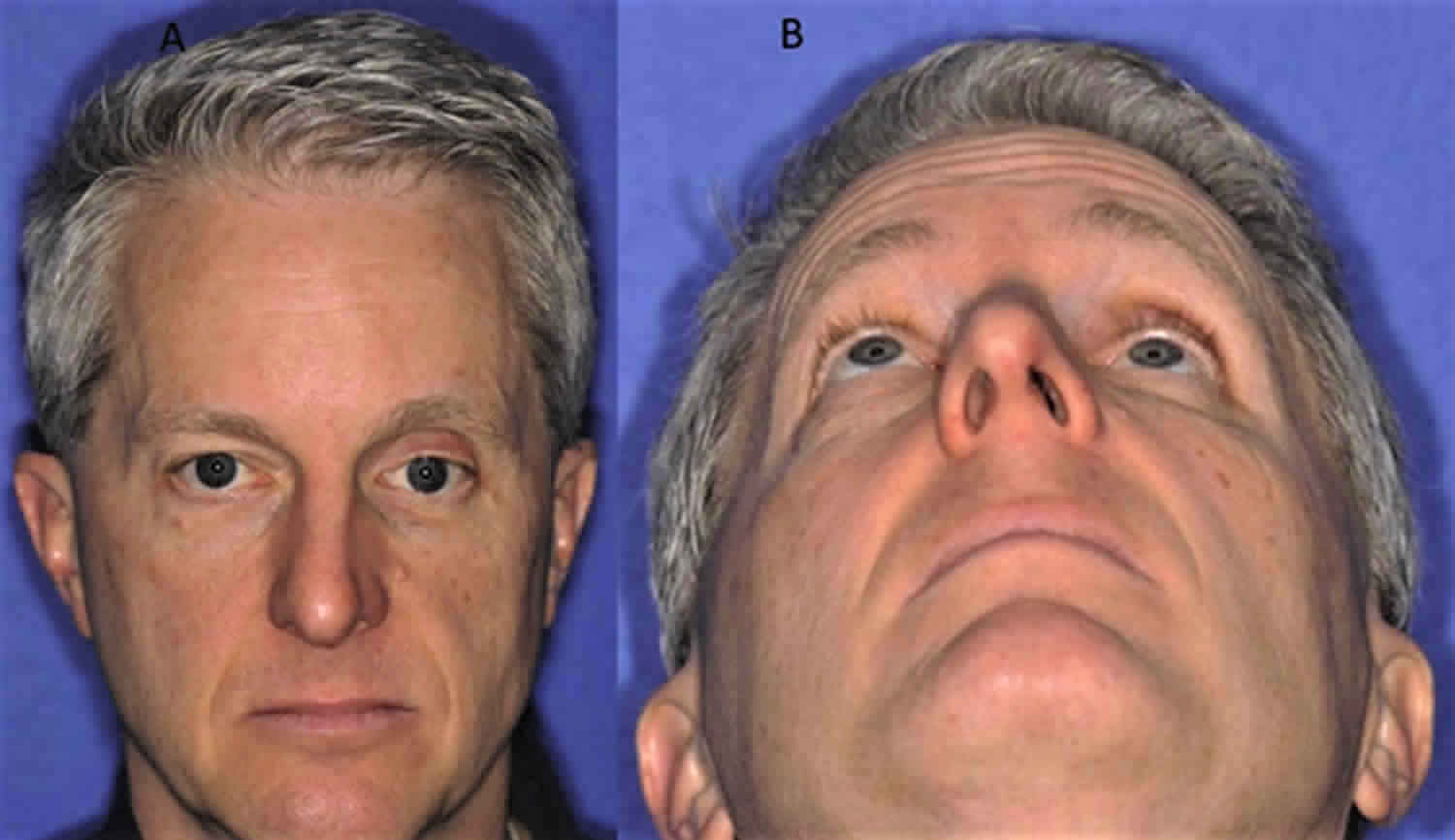
Enophthalmos and hypoglobus
Those diagnosed with silent sinus syndrome most commonly present complaining of changes in their facial appearance with enophthalmos and hypoglobus as the most common manifestations 7. Enophthalmos is present in 98% to 100% present of cases with the measurement of enophthalmos ranging from 2 mm to 6 mm 7 with a mean of 3.4 mm 9. Hypoglobus may be slightly less common than enophthalmos, documented in only 53% of patients in a review of 55 cases 7. The degree of hypoglobus ranges from 1-6mm with a mean of 3.2 mm 9.
Eyelid manifestations
The incidence of upper eyelid position change is high, reported in up to 88% of patients in one large case series 9. Pseudoretraction was seen in the large majority of these patients (90%) due to descent of globe, however the eyelid can also less commonly present with pseudoptotis due to deepening of superior sulcus and lower relative position of the upper eyelid 9. Narrowing of the vertical palpebral aperture has also been noted 8.
Time course
Silent sinus syndrome is most commonly a gradual and progressive disorder with a time course of weeks to months for sign and symptom development. Some reports, however, have documented rapid presentation overnight or over the course of a few days 9. The longest reported progression was observed over 2.5 years 9. The average duration of symptoms before presentation range from 4 to 8 months 9.
Rose et al. 8 depict a more acute underlying process whereby the chronic asymptomatic sinus disease precipitates an acute collapse of the bony orbital floor and sinus walls. In this manuscript, they describe the disease as non-progressive but later clarify that there is observed stability of the orbital signs of enophthalmos and hypoglobus only after re-establishment of free drainage from the maxillary sinus with endonasal sinus intervention 20.
Silent sinus syndrome diagnosis
Silent sinus syndrome diagnostic criteria
Silent sinus syndrome diagnostic criteria include 6:
- Spontaneous enophthalmos and/or hypoglobus
- Absence of symptoms of sinonasal inflammatory disease
- CT imaging showing contraction of maxillary sinus
- Absence of history of orbital trauma, absence of enophthalmos due to another etiology
- Absence of documented congenital deformity
Imaging
Radiographic findings are pathognomonic and required to make the diagnosis of silent sinus syndrome 8. CT imaging characteristically shows ipsilateral maxillary sinus shrinkage with areas of focal bone loss and increased radiolucency due to enlarged fat density in the pterygomaxillary fossa 7.
The orbital floor is typically inferiorly displaced and may be associated with concavity of the medial and posterolateral walls of the maxilla as well 7. The radiographic appearance of the orbital floor is the point of some debate. Most authors exclusively describe patchy demineralization 8 and decreased bone density 7 or dramatic thinning 6 of the bony orbital floor. In the Rose et al. 2003 series 8, however, 3 of 12 patients instead were noted to have thickened bone of the orbital floor. Dr. Rose later clarified this observation, explaining that one would expect hyperostosis and orbital floor thickening only in cases where mucosal inflammation had been very longstanding 20.
Other radiographic findings include nasal septum deviation to the affected side, noted in 32% to 83% of cases 16 and anomalous direction of middle turbinate 8. Rarely, concurrent collapse of a neighboring, ipsilateral ethmoid sinus has been documented 25.
Silent sinus syndrome differential diagnosis
The differential diagnosis of silent sinus syndrome includes chronic sinusitis, osteomyelitis, malignant sinus infiltration, orbital trauma, scleroderma, pseudo-enophthalmos, and atrophy of orbital contents. Orbital content atrophy or contraction may be secondary granulomatous polyangitis, irradiation, or sclerosing pseudotumor 26.
Burroughs et al. published a series of 19 cases referred with the incorrect diagnosis of silent sinus syndrome 26. The most frequent true underlying etiologies in order of prevalence were unrecognized orbital fractures, congenital facial asymmetry, contralateral exophthalmos from thyroid eye disease, and Parry-Romberg syndrome. They noted that those presenting with misdiagnosis often complained of facial pain and mucoprurulent discharge that predated their orbital manifestations. The criteria of silent sinus syndrome diagnosis mandate that patients must present with spontaneous enophthalmos or hypoglobus in the absence of these sinonasal symptoms 6. Additionally, other disease processes causing spontaneous enophthalmos such as Parry-Romberg syndrome are noted to have less hypoglobus and pseudoretraction of the upper lid than silent sinus syndrome 9.
Silent sinus syndrome treatment
Silent sinus syndrome is benign but may result in diplopia. Treatment involves the creation of a drainage route for the sinus. This can be with a nasal antral window or maxillary antrostomy.
Silent sinus syndrome surgery
Antrostomy
Historically, creation of a large naso-antral window via the Caldwell-Luc procedure was utilized to treat silent sinus syndrome 21. Blackwell et al. 27 in 1993 described an endoscopic approach to enlargement of the maxillary ostium in order to relieve the obstruction of the osteomeatal complex. This endoscopic antrostomy with or without uncinectomy is now the gold standard to re-establish normal sinus aeration 16. Great care must be taken during endoscopic approach near the lateral nasal wall in setting of altered uncinate process anatomy as penetration of lamina papyracea can occur 15.
Orbital floor repair
The repair of the orbital floor in conjunction with re-establishment of maxillary aeration is a subject of debate. Some propose that the inferior displacement of the orbital floor may be self-reversing by natural orbital floor and bony maxillary sinus remodeling after alleviation of the negative pressure in the maxillary sinus 16. Others argue that additional repair of the orbital floor should always be performed either in a concurrent or second-stage procedure 9.
A case series of 16 patients by Babar-Craig et al. 16 who underwent middle meatal antrostomy reported only small minority (2/16) needing a second stage floor repair. The authors advise waiting up to 6 months after aeration to observe for resolution of orbital signs prior to evaluating for the need of an orbital implant. Of 47 reported cases by Brandt et al. 34% did not reconstruct orbital floor 7. Thomas et al. 28 reported enophthalmos reduction of 1-2 mm after endoscopic maxillary antrostomy alone without further repair of the floor in a series of 4 patients.
A single-stage procedure in which endoscopic antrostomy is combined with orbital floor repair is preferable when severe enophthalmos is present 29. Advantages to a single-stage procedure include reduced morbidity, reduced patient discomfort, and less time of hospitalization 30. Risk of complications such as implant infection, post-operative diplopia, vision loss, or hematoma with a single stage procedure is low 30.
The most common materials of choice for silent sinus syndrome floor reconstruction include Medpore implants, silicone blocks, and Teflon sheets 31. Three patients repaired with silicone blocks in a case series of 67 developed further enophthalmos years later when the implant descended 9. Careful placement must be employed when using a silicone block, shaping the silicone to evenly distribute pressure onto neighboring healthy bone 20.
Non surgical treatment for silent sinus syndrome
In 2011, a case report of successful nonsurgical management using hyaluronic acid gel to reduce enophthalmos after middle-meatal antrostomy has been published 32. The gel was placed as a single bolus in the intra- and extraconal posterior orbit with a 21-gauge needle. Immediate improvement of the patient’s unresolved enophthalmos and superior sulcus deformity was described.
Silent sinus syndrome prognosis
Once drainage is established, no further volume loss will develop. However, any deformity at the time of surgery will be permanent and may require surgical correction, especially if diplopia is present.
References- Management of enophthalmos from silent sinus syndrome with a customized orbital implant. Otolaryngology Case Reports Volume 8, September 2018, Pages 17-19 https://doi.org/10.1016/j.xocr.2018.07.008
- D.J. Annino Jr., L.A. Goguen. Silent sinus syndrome. Curr Opin Otolaryngol Head Neck Surg, 16 (1) (2008), pp. 22-25
- W.W. Montgomery. Mucocele of the maxillary sinus causing enophthalmos. Eye Ear Nose Throat Mon, 43 (1964), pp. 41-44
- C.N. Soparkar, J.R. Patrinely, M.J. Cuaycong, et al. The silent sinus syndrome. A cause of spontaneous enophthalmos. Ophthalmology, 101 (1994), pp. 772-778
- Kass ES, Salman S, Rubin PA, Weber AL, Montgomery WW. Chronic maxillary atelectasis. Ann Otol Rhinol Laryngol. 1997;106(2):109-116.
- Soparkar CN, Patrinely JR, Cuaycong MJ, et al. The silent sinus syndrome. A cause of spontaneous enophthalmos. Ophthalmology. 1994;101(4):772-778.
- Brandt MG, Wright ED. The silent sinus syndrome is a form of chronic maxillary atelectasis: A systematic review of all reported cases. Am J Rhinol. 2008;22(1):68-73.
- Rose GE, Sandy C, Hallberg L, Moseley I. Clinical and radiologic characteristics of the imploding antrum, or “silent sinus,” syndrome. Ophthalmology. 2003;110(4):811-818.
- Soparkar CN, Patrinely JR, Davidson JK. Silent sinus syndrome-new perspectives?Ophthalmology. 2004;111(2):414-5; author reply 415-6.
- Numa WA, Desai U, Gold DR, Heher KL, Annino DJ. Silent sinus syndrome: A case presentation and comprehensive review of all 84 reported cases. Ann Otol Rhinol Laryngol. 2005;114(9):688-694.
- Suh JD, Ramakrishnan V, Lee JY, Chiu AG. Bilateral silent sinus syndrome. Ear Nose Throat J. 2012;91(12):E19-21.
- Montgomery WW. Mucocele of the maxillary sinus causing enophthalmos. Eye Ear Nose Throat Mon. 1964;43:41-44.
- Wilkins RB, Kulwin DR. Spontaneous enophthalmos associated with chronic maxillary sinusitis. Ophthalmology. 1981;88(9):981-985.
- Davidson JK, Soparkar CN, Williams JB, Patrinely JR. Negative sinus pressure and normal predisease imaging in silent sinus syndrome. Arch Ophthalmol. 1999;117(12):1653-1654.
- Hunt SM, Tami TA. Sinusitis-induced enophthalmos: The silent sinus syndrome. Ear Nose Throat J. 2000;79(8):576, 579-81, 584.
- Babar-Craig H, Kayhanian H, De Silva DJ, Rose GE, Lund VJ. Spontaneous silent sinus syndrome (imploding antrum syndrome): Case series of 16 patients. Rhinology. 2011;49(3):315-317.
- Vander Meer JB, Harris G, Toohill RJ, Smith TL. The silent sinus syndrome: A case series and literature review. Laryngoscope. 2001;111(6):975-978.
- Scharf KE, Lawson W, Shapiro JM, Gannon PJ. Pressure measurements in the normal and occluded rabbit maxillary sinus.Laryngoscope. 1995;105(6):570-574.
- Kass ES, Salman S, Montgomery WW. Manometric study of complete ostial occlusion in chronic maxillary atelectasis. Laryngoscope. 1996;106(10):1255-1258.
- Rose GE. Silent sinus syndrome — new perspectives? author reply. Ophthalmology (Rochester, Minn ). 2004;111(2):415-416.
- Rose GE, Lund VJ. Clinical features and treatment of late enophthalmos after orbital decompression: A condition suggesting cause for idiopathic “imploding antrum” (silent sinus) syndrome. Ophthalmology. 2003;110(4):819-826.
- Hobbs CG, Saunders MW, Potts MJ. “Imploding antrum” or silent sinus syndrome following naso-tracheal intubation. Br J Ophthalmol. 2004;88 (7): 974-5. doi:10.1136/bjo.2003.035386
- Illner A, Davidson HC, Harnsberger HR et-al. The silent sinus syndrome: clinical and radiographic findings. AJR Am J Roentgenol. 2002 Feb;178(2):503-6. https://www.ajronline.org/doi/full/10.2214/ajr.178.2.1780503
- Zhang C, Phamonvaechavan P, Christoff A, Guyton DL. Silent sinus syndrome causing cyclovertical diplopia masquerading as superior oblique paresis in the fellow eye. J AAPOS. 2010;14(5):450-452.
- Braganza A, Khooshabeh R. Ethmoidal involvement in “imploding” (silent) sinus syndrome. Ophthal Plast Reconstr Surg. 2005;21(4):305-307.
- Burroughs JR, Hernandez Cospin JR, Soparkar CN, Patrinely JR. Misdiagnosis of silent sinus syndrome. Ophthal Plast Reconstr Surg. 2003;19(6):449-454.
- Blackwell KE, Goldberg RA, Calcaterra TC. Atelectasis of the maxillary sinus with enophthalmos and midface depression. Ann Otol Rhinol Laryngol. 1993;102(6):429-432.
- Thomas RD, Graham SM, Carter KD, Nerad JA. Management of the orbital floor in silent sinus syndrome. Am J Rhinol. 2003;17(2):97-100.
- Cobb AR, Murthy R, Cousin GC, et al. Silent sinus syndrome. Br J Oral Maxillofac Surg. 2012;50(6):e81-5.
- Sesenna E, Oretti G, Anghinoni ML, Ferri A. Simultaneous management of the enophthalmos and sinus pathology in silent sinus syndrome: A report of three cases.J Craniomaxillofac Surg. 2010;38(6):469-472.
- Numa WA, Desai U, Gold DR, Heher KL, Annino DJ. Silent sinus syndrome: A case presentation and comprehensive review of all 84 reported cases. Ann Otol Rhinol Laryngol. 2005;114(9):688-694
- Mavrikakis I, Detorakis ET, Yiotakis I, Kandiloros D. Nonsurgical management of silent sinus syndrome with hyaluronic acid gel. Ophthal Plast Reconstr Surg. 2012;28(1):e6-7.